Abstract
Objective
The present study was conducted to examine the effects of the Mindfulness-Based Stress Reduction (MBSR) Program on stress, anxiety, and prenatal attachment of the high-risk pregnant women.
Method
This randomized controlled study was conducted with 94 high-risk pregnant women (48 participants in the experimental group, 46 participants in the control group). In the study, the experimental group underwent an eight-session MBSR program, consisting of two sessions per week for a total duration of 1 month. Data of the study were collected with the Prenatal Distress Questionnaire-Revised (NuPDQ), Pregnancy-Related Anxiety Questionnaire-Revised 2 (PRAQR2), and Prenatal Attachment Inventory (PAI).
Results
After the intervention, the PRAQR2 total mean score in the experimental group was significantly lower than that in the control group (p < 0.05). In addition, the PAI total mean score in the experimental group was significantly higher than that in the control group (p < 0.05). However, there was no significant difference between the groups in the NuPDQ total mean score (p > 0.05).
Conclusions
It was determined that the MBSR program applied to high-risk pregnant women decreased anxiety levels, increased prenatal attachment levels, and did not affect stress levels of the pregnant women. Health professionals may consider the MBSR program for high-risk pregnant women as a means by which to improve their pregnancy outcomes.
Preregistration
NCT05317065.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although most pregnancies and births occur without problems, it is reported that all pregnant women are at risk, and approximately 15% of pregnant women may develop a life-threatening complication (World Health Organization, 2017). High-risk pregnancies refer to any situation that situates the mother, fetus, or newborn at increased risk for morbidity or mortality during pregnancy or childbirth (Nesro et al., 2021; Zaidan et al., 2018). The presence of risky situations during pregnancy also has a negative effect on psychological health (Bahadır Yılmaz & Şahin, 2019; Çağlar & Yeşiltepe Oskay, 2019; Dagklis et al., 2016). It is known that the distress (Gözüyeşil & Ariöz Düzgün, 2021) and anxiety (Pisoni et al., 2016; Rodrigues et al., 2016; Smorti et al., 2023) levels of high-risk pregnant women, especially those who are hospitalized, are high. Gözüyeşil and Ariöz Düzgün (2021) reported in their study with high-risk pregnant women that more than half of the participants (63.5%) experienced distress (Gözüyeşil & Ariöz Düzgün, 2021). Furthermore, it is stated that 68% of high-risk pregnant women experience moderate to high levels of anxiety (Paz et al., 2022). It has been reported that the prevalence of pregnancy-related anxiety (26.5%) is higher than the prevalence of general anxiety (16.4%) in pregnant women (Naja et al., 2020). Pregnancy-related anxiety differs from general anxiety and depression symptoms, and refers to fears and worries specific to pregnancy, including the health of the fetus, childbirth, and future parenting concerns (Huizink et al., 2004). Pregnancy-related anxiety and distress are associated with adverse birth outcomes (Faramarzi et al., 2019; Madhavanprabhakaran et al., 2015). Moreover, it is stated that health problems experienced during pregnancy can increase the level of anxiety and affect mother-baby attachment (Yeşilçınar et al., 2023).
Prenatal attachment is a multidimensional emotional bond that includes the mother’s thoughts, behaviors, and attitudes towards her unborn child (Bakır et al., 2014; Filippetti et al., 2022). This bond begins with the woman’s desire to become pregnant and strengthens as she feels fetal movement and embraces her maternal roles (Topaç Tuncel & Kahyaoğlu Süt, 2019). A risky situation that may occur during pregnancy negatively affects the woman’s adaptation to pregnancy and the process of gaining the maternal role that begins with pregnancy, and at the same time, it causes confusion in maternal roles by feeling guilty and can reveal sources of stress (Baltacı & Başer, 2020; Deliktaş et al., 2015). Eswi and Khalil (2012) found in their study that the attachment level of high-risk pregnant women was lower than low-risk pregnant women (Eswi & Khalil, 2012). Pisoni et al. (2016) similarly reported in their study that parents who are at risk of premature birth and are hospitalized and expecting a baby have higher anxiety and depression levels and lower attachment levels than the physiological pregnant group (Pisoni et al., 2016). Medical risks and maternal risks both increase the risk of pregnancy and adverse obstetric outcomes (Kuppusamy et al., 2023).
It is extremely important to implement psychological interventions to reduce the psychological distress of pregnant women and increase mother-baby well-being (Zhang et al., 2023). Although there is no consensus on the definition of mindfulness, it is generally defined as a mental state that involves focusing on the present moment in a non-judgmental manner, with an attitude of openness and acceptance of experiences (Lucena et al., 2020). Mindfulness-Based Stress Reduction (MBSR) program is designed in 8-week sessions and is one of the most well-known mindfulness intervention. The MBSR program includes body scans, gentle stretching, and yoga mindfulness exercises, as well as a wide range of holistic techniques and therapies to apply mindfulness to daily life experiences, including coping with stress (Creswell, 2017). Studies have also emphasized that mindfulness interventions reduce the stress and anxiety levels of high-risk pregnant women and are effective on prenatal attachment in pregnant women (Gheibi et al., 2020; Güney et al., 2022; Shreffler et al., 2019; Woolhouse et al., 2014). Additionally, Dhillon et al. (2017), in a systematic review and meta-analysis of mindfulness-based interventions in pregnancy, have stated that the MBSR program can be used to solve problems such as anxiety, depression, and perceived stress and that the practice increases the awareness levels of pregnant women, reduces prenatal anxiety, and can be used as an effective method to cope with maternal distress (Dhillon et al., 2017). Although the MBSR has been used in many areas recently, no study has been found in which the effects of the MBSR program on stress, anxiety, and prenatal attachment of high-risk pregnant women are examined together. It was aimed that the results of this study, which was conducted to examine the effect of the MBSR program on stress, anxiety, and prenatal attachment of the high-risk pregnant women, will provide important contributions to health professionals who provide care services in the antenatal period regarding the effectiveness of MBSR program. We hypothesized that the MBSR program provided to high-risk pregnant women affects prenatal distress levels, pregnancy-related anxiety levels, and prenatal attachment levels.
Method
Participants
The current study was carried out between the dates of June and August 2022 at the 15th Family Health Center (FHC) of a city center located in the Southeastern Anatolia Region of Turkey. Seven healthcare professionals, including three physicians, three midwives, and one nurse, were working at the FHC. The total population of FHC was around 9000 on average. The working hours of FHC were between 08:00–12:00 and 13:00–17:00. Pregnant women who were diagnosed with high-risk pregnancies registered to the FHC were referred to the Healthy Living Center (HLC) in the city center and the high-risk pregnancies were reported. The population of the study consisted of pregnant women who were registered to the 15th FHC in a city center located in the Southeastern Anatolia Region of Turkey at the relevant dates and diagnosed with high-risk pregnancies and reported to the HLC. The minimum number of individuals to be included in the sample of the study was determined by power analysis. In the literature review, it was determined the mean pregnancy-related anxiety score in the high-risk pregnant women, was previously reported as 30.53 (SD = 6.49) (Duman et al., 2021). The information in the literature shows that an approximately 4- or 5-point difference in scale scores can be clinically and statistically significant in a different intervention study conducted with pregnant women using same measurement tools (Aksoy Derya et al., 2021). The sample size was calculated as 84 pregnant women (42 participants for the experimental group, 42 participants for the control group) assuming that the method applied with a 5% error level, 95% confidence interval, and 80% ability to represent the universe would reduce the anxiety mean score (30.53, SD = 6.49) by 4 points. Considering possible case losses (20%), a total of 100 pregnant women were planned to be included in the study. The final sample consisted of 94 high-risk pregnant women. The pregnant women were 18–44 years old, in a romantic relationship, then nearly half of the participants had similar income perception, and at the time of recruitment participants had a gestational age between 12 and 27.
Inclusion criteria were as follows: pregnant women who were between the 10th and 28th week of gestation, diagnosed with high-risk pregnancies, able to understand Turkish, used smartphones, had Internet network and access, had headset accessories that they could use in the interviews, and voluntarily accepted to participate in the study were included in the study.
Exclusion criteria were as follows: pregnant women who had participated in mind–body practices or any other types of prenatal classes/programs during the study period. Other exclusion criteria included unwillingness to continue to participate in the study, having a psychological problem. Psychiatric health problems were determined according to the declaration and medical history of the pregnant women.
The high-risk pregnant women were randomly assigned to two groups, namely experimental and control group. Columns between 1 and 100 were created using the “Random Integer Generator” method, which is located in the “Numbers” sub-heading of the “random.org” site for the women who met the sample selection criteria. The numbers 1 and 2 for the experimental and control groups were observed in the column. Which number would represent the experimental or control group was determined by drawing lots at the beginning of the research. The women who matched the number 1 as a result of the lottery were assigned to the experimental group, and the women who matched the number 2 were assigned to the control group (Random.org). The randomization process was conducted by a non-involved person in the sampling and analysis.
Procedure
The data of the study were collected from pregnant women who were registered to the 15th FHC in a city center in the Southeastern Anatolia Region of Turkey between the dates of June and August 2022, diagnosed with the high-risk pregnancies, and reported to the HLC. Pregnant women were invited to participate in the study by contacting them by phone. The pregnant women who accepted to participate in the study, met the inclusion criteria, and were assigned to the experimental and control groups were informed (Whatsapp) by the researcher and asked to fill in web-based online questionnaires prepared through Google Forms. The informed consent form was presented on the first page of the online questionnaire. As a pre-test, the Personal Information Form, Prenatal Distress Questionnaire-Revised (NuPDQ), Pregnancy-Related Anxiety Questionnaire-Revised 2 (PRAQR2), and Prenatal Attachment Inventory (PAI) were applied to the high-risk pregnant women in the experimental and control groups. After the MBSR program (assignments, exercises, and applications of breathing and body) was applied online by the researcher to the experimental group for 1 month, two sessions each week, a total of eight sessions, post-test data was obtained by re-applying the the NuPDQ, PRAQR2, and PAI to the experimental group and simultaneously to the control group.
Intervention
In order to evaluate the effect of the MBSR program on stress, anxiety, and prenatal attachment of the high-risk pregnant women, the MBSR was applied to the high-risk pregnant women in the experimental group for four weeks (two sessions per week for a total of eight sessions). The intervention protocol of this study covers the entire MBSR program, which consists of two sessions per week for 1 month and home assignments given throughout the program. In all sessions, mindfulness exercises such as 3-min breathing, body and breathing exercises, body scanning meditation, sitting meditation, mountain meditation, and compassion meditation were applied to the participants under the guidance of the researcher (S.O.C.), who was trained and has a certificate in the field of MBSR. It was done in sessions and individual applications in an environment where pregnant women were not disturbed at any time of the day. The sessions of the MBSR program were based on the meditation techniques of Mindfulness Therapy (Kabat-Zinn, 1990). The live online MBSR program was provided via mobile communication tools. Sessions were conducted as individual or group sessions according to choice of high-risk pregnant women by determining the days and time when they were available online. Each session lasted an average of 40–60 min. The pregnant women in the control group received usual hospital care and they were applied no intervention. After the collection of the posttest data, the participants in the control group were offered mindfulness training at no cost.
Measures
Personal Information Form
This is a form consisting of 16 questions developed by the researchers in line with the literature, with the aim of determining the women’s socio-demographic (age, spouse’s age, educational level, employment status, spouse’s employment status, perceived income level) and obstetric (week of gestation, number of pregnancies, number of abortions/curettage, number of births, number of living children, the status of having a planned pregnancy, method of previously terminated pregnancy, the time period between the present pregnancy and the previous delivery, the status of getting pregnant with treatment, the risk status of pregnancy) characteristics (Bakır et al., 2014; Dereli Yılmaz & Kızılkaya Beji, 2010; Duman et al., 2021; Yüksel et al., 2020).
Prenatal Distress Questionnaire-Revised
Prenatal distress was measured using the validated 17-item NuPDQ. The NuPDQ assesses pregnant women’s concerns about social relationships, physical and emotional symptoms, themselves, and their baby. The Turkish validity and reliability study of the questionnaire was conducted by Yüksel et al. (2011). The questionnaire is in the form of 3-point Likert type. Each item in the questionnaire was scored as 0 = Not at all, 1 = A little, and 2 = A lot. A minimum of 0 and a maximum of 34 points can be obtained from the questionnaire. An increase in the scores obtained from the questionnaire is interpreted as an increase in prenatal distress (Ibrahim & Lobel, 2020; Lobel et al., 2008; Yali & Lobel, 1999; Yüksel et al., 2011). In the Turkish validity and reliability study of the scale, Cronbach’s alpha coefficient was reported as 0.85 (Yüksel et al., 2011). In the present study, the Cronbach’s alpha coefficient and McDonald’s omega were calculated as 0.94 for the NupDQ.
The Pregnancy-Related Anxiety Questionnaire-Revised 2
The PRAQR2 was developed by Van der Bergh (1990), and Huizink et al. (2016) revised it. The PRAQR2 was developed to question the level of anxiety experienced by women about their pregnancies. The Turkish adaptation of the questionnaire was made by Aksoy Derya et al. (2018). The Turkish version of the questionnaire consists of 10 items for multiparas and 11 items for primiparas, and the questionnaire is in the format of a 5-point Likert type. There are 3 subscales in the questionnaire: Fear of giving birth, Worries about bearing a handicapped child, and Concern about one’s own appearance. The 8th item in the questionnaire is applied only to primiparous women. Items are scored between 1 and 5, where 1 = Absolutely not relevant and 5 = Very relevant. A minimum of 11 and a maximum of 55 points can be obtained from primiparas, and a minimum of 10 and a maximum of 50 points can be obtained from multiparas. As the score obtained from the questionnaire increases, the level of anxiety during pregnancy also increases (Aksoy Derya et al., 2018; Huizink et al., 2016; Van der Bergh, 1990). In the Turkish validity and reliability study of the questionnaire, Cronbach’s alpha coefficient was reported as 0.93 in multiparas and 0.94 in nulliparas (Aksoy Derya et al., 2018). In the current study, the Cronbach’s alpha coefficient was determined to be 0.94 and McDonald’s omega was calculated as 0.95 for the PRAQR2.
Prenatal Attachment Inventory
The PAI was developed by Muller (1993) to explain the thoughts, feelings, and situations experienced by women during their pregnancies and to determine the level of attachment to their babies in the prenatal period. Turkish validity and reliability study was carried out by Dereli Yılmaz & Kızılkaya Beji, (2013). Each item is evaluated between 1 and 4 points, and the inventory is in the 4-point Likert type. There are 21 items in total in the inventory, and the items are scored as 1 = Never, 2 = Sometimes, 3 = Often, and 4 = Always. A minimum of 21 and a maximum of 84 points can be obtained from the inventory. As the scores obtained from the inventory increase, the level of attachment also enhances (Dereli Yılmaz & Kızılkaya Beji, 2013; Muller, 1993). In the Turkish validity and reliability study of the inventory, Cronbach’s alpha coefficient was reported as 0.84 (Dereli Yılmaz & Kızılkaya Beji, 2013). In this study, the Cronbach’s alpha coefficient and McDonald’s omega was calculated as 0.94 for the PAI.
Data Analyses
The obtained data were analyzed using the program Statistical Package for the Social Sciences (SPSS) for Windows 25.0. Kolmogorov–Smirnov test was used to determine whether the data presented a normal distribution. It was seen that the data were normally distributed. Descriptive statistics included numbers, percentage distribution, mean, standard deviation, and min–max values. The descriptive and obstetric characteristics were compared through chi-square test, and independent samples t-test. The mean scores of stress, anxiety, and prenatal attachment were compared before intervention using the independent samples t-test. To test for the intervention effects, ANCOVA test with controlling the baseline scores were conducted. Effect sizes were reported as partial η2. The level of significance was accepted as p < 0.05.
Results
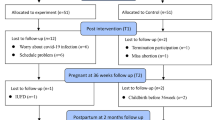
Due to the fact that two pregnant women in the experimental group could not be reached during the post-test application, and four pregnant women in the control group did not complete the post-test voluntarily, the study was completed with a total of 94 high-risk pregnant women (48 participants for the experimental group, 46 participants for the control group). In addition, 16 pregnant women did not accept to participate in the study, and 4 pregnant women could not be included in the study because they did not have smartphones/or Internet access (Fig. 1; CONSORT Research Flowchart). Dropped out and excluded participants did not differ from the final sample on any descriptive and obstetric characteristics.
When the high-risk pregnant women in the experimental and control groups were compared in terms of descriptive characteristics, it was determined that there was no statistically significant difference between the two groups in terms of descriptive characteristics such as age, spouse’s age, educational level, employment status, spouse’s employment status, and income level (p > 0.05) (Table 1).
When the high-risk pregnant women in the experimental and control groups were compared in terms of obstetric characteristics, the status of having a planned pregnancy, how the previous pregnancy terminated, the time period between the current pregnancy and the previous delivery, the status of conception with treatment, gestational week, number of pregnancies, number of miscarriages/curettages, number of deliveries, and number of living children, there was no statistically significant difference in terms of obstetric characteristics (p > 0.05) (Table 2). Both groups had similar descriptive and obstetric characteristics.
When the pregnancy-related risk status of high-risk pregnant women regarding their pregnancies was examined, it was seen that 33% of them were having pregnancies at early/advanced age, 21.3% of them had frequent interbirth intervals and anemia, 19.1% of them had obesity, 17% of them had blood incompatibility, 16% of them had consanguineous marriages, 5.3% of them had gestational diabetes and pre-existing diabetes, and 42.6% of them had other risk factors (risk of premature birth, multiple pregnancies, history of anomalous baby, preeclampsia, smoking, presence of infection, risk of miscarriage, heart diseases, endocrine diseases) (Table 3).
When the pre-test and post-test NuPDQ total, PAI total, PRAQR2 total, and its subscales’ mean scores of the high-risk pregnant women were examined, it was found that the pre-test NuPDQ total mean score of the high-risk pregnant women was 25.74 (SD = 3.45), and the post-test NuPDQ total mean score was 15.56 (SD = 8.61).
It was determined that the pre-test PRAQR2 total mean score of the high-risk pregnant women was 39.33 (SD = 5.05), and the post-test PRAQR2 total mean score was 29.88 (SD = 10.0). In addition, the PRAQR2’s subscale of fear of giving birth total mean score was 14.94 (SD = 1.90) in the pre-test, 11.78 (SD = 3.87) in the post-test; the PRAQR2’s subscale of worries about bearing a handicapped child total mean score was 13.71 (SD = 2.76) in the pre-test and 9.86 (SD = 3.73) in the post-test; the PRAQR2’s subscale of concern about one’s own appearance total mean score was 10.67 (SD = 1.89) in the pre-test and 8.24 (SD = 3.13) in the post-test.
It was determined that the pre-test PAI total mean score of the high-risk pregnant women was 42.16 (SD = 7.33), and the post-test PAI total mean score was 49.35 (SD = 9.66) (Table 4).
The inter-group comparisons of the pre-test and post-test total mean scores of the high-risk pregnant women in the experimental and control groups from the NuPDQ, PRAQR2, and PAI were analyzed. When the pre-test NuPDQ and PAI total mean scores of the high-risk pregnant women in the experimental and control groups were compared, it was determined that the differences between the groups were not statistically significant and that the high-risk pregnant women in the experimental and control groups had similar distress and attachment levels before the implementation of MBSR program (p > 0.05). When the pre-test PRAQR2 total mean scores of the high-risk pregnant women in the experimental and control groups were compared, it was determined that the difference between the groups was statistically significant and the anxiety levels of the high-risk pregnant women in the control group before the implementation of MBSR program were lower than those in the experimental group (p < 0.05) (Table 5).
After the intervention, a comparison of the mean score of the stress indicated no statistically significant difference between the groups after adjusting the effect of baseline score (adjusted mean difference, AMD: − 12.571; 95% CI (confidence interval): − 15.0 to − 10.1; p > 0.05). However, the mean score of the anxiety significantly decreased in the experimental group, compared to the control group (AMD: − 14.917; 95% CI: − 17.8 to − 11.9; p < 0.001), with large effect size (η2 = 0.528). Furthermore, the mean score of the prenatal attachment significantly increased in the experimental group, compared to the control group (AMD: 11.554; 95% CI: 8.3 to 14.7; p < 0.001), with large effect size (η2 = 0.357) (Table 5).
Discussion
High-risk pregnancy is a physiological and psychosocial condition that threatens the life and health of the mother, fetus, or newborn. High-risk pregnant women often experience stress and anxiety as a result of risk factors during pregnancy and as a result of hospitalization. Well-being in psychosocial health ensures that both the maternal role and maternal attachment are healthy. This study aimed to assess the impact of the MBSR program on stress, anxiety, and prenatal attachment among high-risk pregnant women. The results showed a decrease in anxiety levels and an increase in attachment levels among the high-risk pregnant women in the experimental group, while stress levels remained unchanged after the MBSR program.
In the study, it was determined that there was no statistically significant difference between the descriptive and obstetric characteristics of the pregnant women in the experimental and control groups. In line with these results, it can be said that the study groups were homogeneously distributed. When the NuPDQ and PAI total mean scores of the high-risk pregnant women in the experimental and control groups were compared, it was determined that the differences between the groups were not statistically significant, while the pre-test measurement of the PRAQR2 total mean score of the high-risk pregnant women in the control group was lower than those of the experimental group. Therefore, it was seen that the high-risk pregnant women in the experimental and control groups had similar distress and attachment levels before the implementation of the MBSR program. On the other hand, it was seen that the anxiety levels of the pregnant women in the control group were lower, and the pregnant women in the experimental group were more disadvantaged in terms of anxiety. These results may be due to the fact that individuals’ situations and risk perceptions are different and that there are many factors from effecting anxiety.
Pregnancy, which is a physiological process, is also a complex process in which anxiety and stress can occur intensely. In fact, this situation is even more evident when pregnancy is risky (Dağlar & Nur, 2014; Gümüşdaş et al., 2014). Because pregnant women with high-risk pregnancies may experience anxiety and stress due to many factors such as health problems, uncertainty, hospitalization, and separation from the family (Baltacı & Başer, 2020). A study evaluating psychosocial health status in the literature has also stated that those with high-risk pregnancies are more likely to develop distress, anxiety, and depression compared to others, and their psycho-social health status is affected more negatively (Gümüşdaş et al., 2014). It is known that mindfulness interventions have positive effects on the distress (Pan et al., 2019; Woolhouse et al., 2014) and anxiety (İbici Akca et al., 2023; Mohamed et al., 2017; Vieten & Astin, 2008; Woolhouse et al., 2014) levels of pregnant women. Our study results show that, although the MBSR program in high-risk pregnant women does not affect the stress experienced, it is an effective method for coping with anxiety. Güney et al. (2022) reported in their study that the MBSR program was effective in reducing the distress and anxiety levels of pregnant women diagnosed with COVID-19 (Güney et al., 2022). Goetz et al. (2020) similarly found in their study that electronic mindfulness-based intervention reduced the anxiety scores of hospitalized high-risk pregnant women (Goetz et al., 2020). Zhang et al. (2023) reported in their study that the Digital Guided Self-help Mindfulness Training reduced the anxiety levels of pregnant women with psychological distress (Zhang et al., 2023). Hulsbosch et al. (2023) reported in their study that the online mindfulness-based intervention was not effective in reducing the distress levels of pregnant women with pregnancy distress (Hulsbosch et al., 2023). Our research results show that the MBSR program applied to high-risk pregnant women effectively reduces anxiety levels and supports the literature. However, there are differences between study findings regarding the effects of mindfulness practices on the distress levels in pregnant women. In line with these results, it can be said that there is a need for further controlled studies that reveal the relationship between mindfulness and distress.
Danger symptoms and fears of losing the fetus in high-risk pregnant women can negatively affect mother-infant attachment (Baltacı & Başer, 2020; Røhder et al., 2020). In the literature, it has been stated that the prenatal attachment level of high-risk pregnant women is lower than that of non-risky pregnant women (Eswi & Khalil, 2012; Pisoni et al., 2016), and that anxiety and stress that occur during hospitalization and discomfort that cause risky situations negatively affect prenatal attachment (Pisoni et al., 2014). Although it has long been accepted that mindfulness-based practices are a factor that significantly contributes to the health of the mother and child (Golmakani et al., 2021), studies examining the effects of these practices on prenatal attachment are quite limited. Limited studies have reported that mindfulness interventions increase the prenatal attachment levels of pregnant populations (Gheibi et al., 2020; Haghighat et al., 2015; Malhotra et al., 2021; Shreffler et al., 2019). In this study, similarly, it was determined that the prenatal attachment levels of the high-risk pregnant women who received the MBSR program were significantly higher than those who did not receive the MBSR program. Muzik et al. (2012) smilarly reported that mindfulness yoga significantly increased maternal–fetal attachment of pregnant women at high risk for psychopathology (Muzik et al., 2012). According to these results, it is possible to say that the MBSR program is an effective application that increases the prenatal attachment of high-risk pregnant women and based on the available evidence, MBSR can also be used among non-medical methods for high-risk pregnant women.
Limitations and Future Research
The limitations of the study are that pregnant women who did not have a smartphone or Internet access could not be included in the study due to the online conduct of the study. We included all high-risk pregnant women in our study, regardless of risk factor rather than a specific risky condition associated with pregnancy. Anxiety and stress levels may vary depending on the severity of the risk situation during pregnancy and the risk perception of the pregnant woman. Therefore, it may be recommended to consider a specific risky situation associated with pregnancy for future studies. This way, the relationship between MBSR program and anxiety and distress can be understood more clearly in this population. Additionally, more studies focusing on low-cost psychological interventions are needed. Future research should include face-to-face practices as an alternative to improve the efficacy and persistence of the intervention, including self-administration at home, and include sample groups of pregnant women experiencing high levels of distress in pregnancy. Other limitations include the relatively small number of participants and the fact that all were selected from only a single health center. Multicenter studies that allow high-risk pregnant women with different socio-cultural characteristics to be included in the research will help generalize the findings. In addition, verifying our results with more sample groups in terms of generalizability of the findings will be important.
According to the results of the study, the MBSR program applied to high-risk pregnant women decreased anxiety, increased prenatal attachment levels, but did not affect stress levels of the pregnant women. Pregnancy is a period in which some important physical and psychological changes are seen, and the addition of risks related to pregnancy to these changes can make the process more difficult and complex, causing it to become inextricable for the woman and her family. For this reason, it is extremely important to manage the changes that occur in women who have a high-risk pregnancy in order to protect and increase the health of the mother and baby. Further research is necessary to validate these findings and explore the full potential of such interventions. Although the literature is limited, studies, like ours, on some populations, have shown that a mindfulness program may help to increase prenatal attachment and reduce anxiety. For this reason, it is recommended that health professionals integrate this program into the care they offer in order to reveal the positive effects of the MBSR program.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Aksoy Derya, Y., Timur Taşhan, S., Duman, M., & Durgun Ozan, Y. (2018). Turkish adaptation of the pregnancy-related anxiety questionnaire-revised 2: Validity and reliability study in multiparous and primiparous pregnancy. Midwifery, 62, 61–68. https://doi.org/10.1016/j.midw.2018.03.006
Aksoy Derya, Y., Altıparmak, S., Akça, E., Gökbulut, N., & Yılmaz, A. N. (2021). Pregnancy and birth planning during COVID-19: The effects of tele-education offered to pregnant women on prenatal distress and pregnancy-related anxiety. Midwifery, 92, 102877. https://doi.org/10.1016/j.midw.2020.102877
Bahadır Yılmaz, E., & Şahin, E. (2019). Factors associated with prenatal distress levels of pregnant women. Journal of Psychiatric Nursing, 10(3), 197–203. https://doi.org/10.14744/phd.2019.17363
Bakır, N., Ölçer, Z., & Oskay, Ü. (2014). The levels and affecting factors of prenatal attachment in high risk pregnant. International Refereed Journal of Gynaecological Diseases and Maternal Child Health, 1(1), 25–37. https://doi.org/10.17367/JACSD.2014019296
Baltacı, N., & Başer, M. (2020). Anxiety, prenatal attachment and nurses’ role in risky pregnancies. E-Journal of Dokuz Eylul University Nursing Faculty, 13(3), 206–212. https://doi.org/10.46483/deuhfed.565338
Creswell, J. D. (2017). Mindfulness interventions. Annual Review of Psychology, 68, 491–516. https://doi.org/10.1146/annurev-psych-042716-051139
Çağlar, M., & Yeşiltepe Oskay, Ü. (2019). Assesment of prenatal distress and depressive symptoms in women with gestational diabetes. Turkish Journal of Diabetes and Obesity, 2, 73–78. https://doi.org/10.25048/tjdo.2019.43
Dagklis, T., Papazisis, G., Tsakiridis, I., Chouliara, F., Mamopoulos, A., & Rousso, D. (2016). Prevalence of antenatal depression and associated factors among pregnant women hospitalized in a high-risk pregnancy unit in Greece. Social Psychiatry and Psychiatric Epidemiology, 51, 1025–1031. https://doi.org/10.1007/s00127-016-1230-7
Dağlar, G., & Nur, N. (2014). The relationship between anxiety and depression level and coping styles with stress of pregnant women. Cumhuriyet Medical Journal, 36, 429–441. https://doi.org/10.7197/1305-0028.76793
Deliktaş, A., Körükcü, Ö., & Kukulu, K. (2015). Motherhood experience in different groups. Journal of Marmara University Institute of Health Sciences, 5(4), 274–283. https://doi.org/10.5455/musbed.20150831014409
Dereli Yılmaz, S., & Kızılkaya Beji, N. (2010). Levels of coping with stres, depression and prenatal attachment and affecting factors of pregnant women. Journal of General Medicine, 20(3), 99–108.
Dereli Yılmaz, S., & Kızılkaya Beji, N. (2013). Turkish version of prenatal attachment inventory: A study of reliability and validity. Journal of Anatolia Nursing and Health Sciences, 16(2), 103–109.
Dhillon, A., Sparkes, E., & Duarte, R. V. (2017). Mindfulness-based interventions during pregnancy: A systematic review and meta-analysis. Mindfulness, 8(6), 1421–1437. https://doi.org/10.1007/s12671-017-0726-x
Duman, M., Doğan Yüksekol, Ö., & Durgun Ozan, Y. (2021). The effect of pregnancy-related anxiety on prenatal attachment in pregnant women with preeclampsia. The Journal of Gynecology-Obstetrics and Neonatology, 18(3), 907–915. https://doi.org/10.38136/jgon.795735
Eswi, A., & Khalil, A. (2012). Prenatal attachment and fetal health locus of control among low risk and high risk pregnant women. World Applied Sciences Journal, 18(4), 462–471. https://doi.org/10.5829/idosi.wasj.2012.18.04.6491
Faramarzi, M., Hassanjanzadeh, P., & Khafri, S. (2019). Maternal mid- and late-pregnancy distress and birth outcome: A causal model of the mediatory role of pregnancy-specific distress. International Journal of Reproductive Biomedicine, 17, 585–590. https://doi.org/10.18502/ijrm.v17i8.4824
Filippetti, M. L., Clarke, A. D. F., & Rigato, S. (2022). The mental health crisis of expectant women in the UK: Effects of the COVID-19 pandemic on prenatal mental health, antenatal attachment and social support. BMC Pregnancy and Childbirth, 22, 68. https://doi.org/10.1186/s12884-022-04387-7
Gheibi, Z., Abbaspour, Z., Haghighyzadeh, M. H., & Javadifar, N. (2020). Effects of a mindfulness-based childbirth and parenting program on maternal-fetal attachment: A randomized controlled trial among Iranian pregnant women. Complementary Therapies in Clinical Practice, 41, 101226. https://doi.org/10.1016/j.ctcp.2020.101226
Goetz, M., Schiele, C., Müller, M., Matthies, L. M., Deutsch, T. M., Spano, C., Graf, J., Zipfel, S., Bauer, A., Brucker, S. Y., Wallwiener, M., & Wallwiener, S. (2020). Effects of a brief electronic mindfulness-based intervention on relieving prenatal depression and anxiety in hospitalized high-risk pregnant women: Exploratory pilot study. Journal of Medical Internet Research, 22(8), 93. https://doi.org/10.2196/17593
Golmakani, N., Shaghaghi, F., Ahmadi, Z., Gholami, M., Kamali, Z., & Mohebbi-Dehnavi, Z. (2021). Investigating the relationship between the dimensions of mindfulness and maternal attachment to the fetus during pregnancy. Journal of Education and Health Promotion, 10, 433. https://doi.org/10.4103/jehp.jehp_1513_20
Gözüyeşil, E., & Ariöz Düzgün, A. (2021). Prenatal distress and the contributing factors in high-risk pregnant women. Journal of Education and Research in Nursing, 18(2), 123–129. https://doi.org/10.5152/jern.2021.16870
Gümüşdaş, M., Ejder Apay, S., & Özorhan, E. Y. (2014). Comparison of psycho-social health in pregnant women with and without risk. Journal of Health Science and Profession, 1(2), 32–42. https://doi.org/10.17681/hsp.80013
Güney, E., Cengizhan, S. Ö., Karataş Okyay, E., Bal, Z., & Uçar, T. (2022). Effect of the mindfulness-based stress reduction program on stress, anxiety, and childbirth fear in pregnant women diagnosed with COVID-19. Complementary Therapies in Clinical Practice, 47, 101566. https://doi.org/10.1016/j.ctcp.2022.101566
Haghighat, F., Moradi, A.-R., Mazaheri, M. A., Hantoushzade, Z., Allahyari, A. A., & Pasandide, A. (2015). The effect of Iranian-Islamic mindful motherhood training on maternal fetal attachment. Iran Journal of Nursing, 27(92), 33–43. https://doi.org/10.29252/ijn.27.92.33
Huizink, A. C., Mulder, E. J. H., Robles de Medina, P. G., Visser, G. H. A., & Buitelaar, J. K. (2004). Is pregnancy anxiety a distinctive syndrome? Early Human Development, 79, 81–91. https://doi.org/10.1016/j.earlhumdev.2004.04.014
Huizink, A. C., Delforterie, M. J., Scheinin, N. M., Tolvanen, M., Karlsson, L., & Karlsson, H. (2016). Adaption of pregnancy anxiety questionnaire–revised for all pregnant women regardless of parity: PRAQ-R2. Archives of Women’s Mental Health, 19(1), 125–132. https://doi.org/10.1007/s00737-015-0531-2
Hulsbosch, L. P., Potharst, E. S., Schwabe, I., Boekhorst, M. G. B. M., Pop, V. J. M., & Nyklíček, I. (2023). Online mindfulness-based intervention for women with pregnancy distress: A randomized controlled trial. Journal of Affective Disorders, 332, 262–272. https://doi.org/10.1016/j.jad.2023.04.009
Ibrahim, S. M., & Lobel, M. (2020). Conceptualization, measurement, and effects of pregnancy-specific stress: Review of research using the original and revised prenatal distress questionnaire. Journal of Behavioral Medicine, 43(1), 16–33. https://doi.org/10.1007/s10865-019-00068-7
İbici Akca, E., Gökbulut, N. & Cengizhan, S. O. (2023). The effects of MBSR programme on prenatal comfort and fetal health anxiety in pregnant women. Journal of Reproductive and Infant Psychology. https://doi.org/10.1080/02646838.2023.2227219
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and ilness. Delacourt.
Kuppusamy, P., Prusty, R. K., & Kale, D. P. (2023). High-risk pregnancy in India: Prevalence and contributing risk factors - a national survey-based analysis. Journal of Global Health, 13, 04116. https://doi.org/10.7189/jogh.13.04116
Lobel, M., Cannella, D. L., DeVincent, C., Schneider, J., Graham, J. E., & Meyer, B. A. (2008). Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychology, 27(5), 604–615. https://doi.org/10.1037/a0013242
Lucena, L., Frange, C., Pinto, A. C. A., Andersen, M. L., Tufik, S., & Hachul, H. (2020). Mindfulness interventions during pregnancy: A narrative review. Journal of Integrative Medicine, 18, 470–477. https://doi.org/10.1016/j.joim.2020.07.007
Madhavanprabhakaran, G. K., D’Souza, M. S., & Nairy, K. S. (2015). Prevalence of pregnancy anxiety and associated factors. International Journal of Africa Nursing Sciences, 3, 1–7. https://doi.org/10.1016/j.ijans.2015.06.002
Malhotra, J., Malhotra, N., Patil, M., Malhotra, N., & Garg, R. (2021). Mindful digital program–based interventions and their role in pregnancy and fetal outcomes. Journal of South Asian Federation of Obstetrics and Gynaecology, 13(3), 170–175. https://doi.org/10.5005/jp-journals-10006-1909
Mohamed, M. S., Elsharkawy, N. B., & Awad, M. H. (2017). Mindfulness based intervention program on anxiety and depressive symptoms among pregnant women. American Journal of Nursing Science, 6(3), 232–239. https://doi.org/10.11648/j.ajns.20170603.21
Muller, M. E. (1993). Development of the prenatal attachment inventory. Western Journal of Nursing Research, 15(2), 199–215. https://doi.org/10.1177/019394599301500205
Muzik, M., Hamilton, S. E., Rosenblum, K. L., Waxler, E., & Hadi, Z. (2012). Mindfulness yoga during pregnancy for psychiatrically at-risk women: Preliminary results from a pilot feasibility study. Complementary Therapies in Clinical Practice, 18, 235–240. https://doi.org/10.1016/j.ctcp.2012.06.006
Naja, S., Al Kubaisi, N., Singh, R., & Bougmiza, I. (2020). Generalized and pregnancy-related anxiety prevalence and predictors among pregnant women attending primary health care in Qatar, 2018–2019. Heliyon, 6, e05264. https://doi.org/10.1016/j.heliyon.2020.e05264
Nesro, J., Dhinsa, M., & Gelan, M. (2021). Prevalence of high risk pregnant women who attend antenatal care and associated factors in Jimma Medical Center, Jimma Town, South Western Ethiopia. International Journal Women’s Health and Wellness, 7(133), 1–9. https://doi.org/10.23937/2474-1353/1510133
Pan, W.-L., Gau, M.-L., Lee, T.-Y., Jou, H.-J., Liu, C.-Y., & Wen, T.-K. (2019). Mindfulness-based programme on the psychological health of pregnant women. Women and Birth, 32, e102–e109. https://doi.org/10.1016/j.wombi.2018.04.018
da Paz, M. M. S., de Diniz, M. C. R., de Almeida, M. O., Cabral, N. O., de Assis, T. J. C. F., de Sena, M. F., de Pontes, V. A., da Borges, N. M. S., & Mendes, C. K. T. T. (2022). Analysis of the anxiety level in high risk pregnancy based on the Beck Anxiety Inventory. Revista Brasileira de Saúde Materno Infantil, 22(4), 1015–1023. https://doi.org/10.1590/1806-9304202200040016
Pisoni, C., Garofoli, F., Tzialla, C., Orcesi, S., Spinillo, A., Politi, P., Balottin, U., Manzoni, P., & Stronati, M. (2014). Risk and protective factors in maternal-fetal attachment development. Early Human Development, 90S2, 45–46. https://doi.org/10.1016/S0378-3782(14)50012-6
Pisoni, C., Garofoli, F., Tzialla, C., Orcesi, S., Spinillo, A., Politi, P., Balottin, U., Tinelli, C., & Stronati, M. (2016). Complexity of parental prenatal attachment during pregnancy at risk for preterm delivery. The Journal of Maternal-Fetal & Neonatal Medicine, 29(5), 771–776. https://doi.org/10.3109/14767058.2015.1017813
Random.Org. Random Integer Generator. Retrieved May 15, 2022, from https://www.random.org/integers/?num=100&min=1&max=2&col=5&base=10&format=html&rnd=new.
Rodrigues, P. B., Zambaldi, C. F., Cantilino, A., & Sougey, E. B. (2016). Special features of high-risk pregnancies as factors in development of mental distress: A review. Trends in Psychiatry and Psychotherapy, 38(3), 136–140. https://doi.org/10.1590/2237-6089-2015-0067
Røhder, K., Væver, M. S., Aarestrup, A. K., Jacobsen, R. K., Smith-Nielsen, J., & Schiøtz, M. L. (2020). Maternal-fetal bonding among pregnant women at psychosocial risk: The roles of adult attachment style, prenatal parental reflective functioning, and depressive symptoms. PLoS ONE, 15(9), e0239208. https://doi.org/10.1371/journal.pone.0239208
Shreffler, K. M., Tiemeyer, S., Ciciolla, L., & Croff, J. M. (2019). Effect of a mindfulness-based pilot intervention on maternal-fetal bonding. International Journal of Women’s Health, 11, 377–380. https://doi.org/10.2147/IJWH.S203836
Smorti, M., Ginobbi, F., Simoncini, T., Pancetti, F., Carducci, A., Mauri, G., & Gemignani, A. (2023). Anxiety and depression in women hospitalized due to high-risk pregnancy: An integrative quantitative and qualitative study. Current Psychology, 42, 5570–5579. https://doi.org/10.1007/s12144-021-01902-5
Topaç Tuncel, N., & Kahyaoğlu Süt, H. (2019). The effect of anxiety, depression and prenatal distress levels in pregnancy on prenatal attachment. The Journal of Gynecology - Obstetrics and Neonatology, 16(1), 9–17.
Van der Bergh, B. R. H. (1990). The influence of maternal emotions during pregnancy on fetal and neonatal behavior. Pre- and Peri-Natal Psychology, 5(2), 119–130.
Vieten, C., & Astin, J. (2008). Effects of a mindfulness-based intervention during pregnancy on prenatal stres and mood: Results of a pilot study. Archives of Women’s Mental Health, 11, 67–74. https://doi.org/10.1007/s00737-008-0214-3
Woolhouse, H., Mercuri, K., Judd, F., & Brown, S. J. (2014). Antenatal mindfulness intervention to reduce depression, anxiety and stress: A pilot randomised controlled trial of the MindBabyBody program in an Australian tertiary maternity hospital. BMC Pregnancy and Childbirth, 14(369), 1–16. https://doi.org/10.1186/s12884-014-0369-z
World Health Organization. (2017). Managing complications in pregnancy and childbirth: A guide for midwives and doctors. Retrieved October 1, 2023, from https://www.who.int/publications/i/item/9789241565493
Yali, A. M., & Lobel, M. (1999). Coping and distress in pregnancy: An investigation of medically high risk women. Journal of Psychosomatic Obstetrics & Gynecology, 20(1), 39–52. https://doi.org/10.3109/01674829909075575
Yeşilçınar, İ, Kıncı, M. F., Ünver, H. C., & Sivaslıoğlu, A. A. (2023). Pregnancy-related anxiety and prenatal attachment in pregnant women with preeclampsia and/or gestational diabetes mellitus: A cross-sectional study. Journal of Clinical Obstetrics & Gynecology, 33(1), 27–35. https://doi.org/10.5336/jcog.2022-93264
Yüksel, A., Dabanlı, Z., & Bahadır Yılmaz, E. (2020). Determining of the relationship between conscious awareness, depression, anxiety and stress in pregnancy. Journal of Academic Research in Nursing, 6(2), 195–202. https://doi.org/10.5222/jaren.2020.55707
Yüksel, F., Akın, S., & Durna, Z. (2011). The Turkish adaptation of the “Revised Prenatal Distress Questionnaire”: A reliability/validity and factor analysis study. Journal of Education and Research in Nursing, 8(3), 43–51.
Zaidan, A. A., Al-Gburi, R. K., & Alhilli, H. M. (2018). The prevalence of high risk pregnancy among pregnant women attending primary health care center in Baghdad Al-Karkh health directorate. Iraqi Journal of Community Medicine, 31(4), 143–147.
Zhang, X., Li, Y., Wang, J., Mao, F., Wu, L., Huang, Y., Sun, J., & Cao, F. (2023). Effectiveness of digital guided self-help mindfulness training during pregnancy on maternal psychological distress and infant neuropsychological development: Randomized controlled trial. Journal of Medical Internet Research, 25, e41298. https://doi.org/10.2196/41298
Acknowledgements
We extend our gratitude to all pregnant women for their participation, and the Coordinatorship of Scientific Research Projects at Amasya University for providing financial support.
Funding
This study was funded by Amasya University’s Coordinatorship of Scientific Research Project with the number of FMB-BAP 22–0546.
Author information
Authors and Affiliations
Contributions
E.I.A.: conceptualization; data curation; formal analysis; investigation; methodology; supervision; visualization; validation; writing—original draft; writing—review and editing. S.O.C.: data curation; investigation; methodology; validation; writing—original draft; writing—review and editing. N.G.: investigation; methodology; validation; writing—original draft; writing—review and editing.
Corresponding author
Ethics declarations
Ethics Statement
Approval was obtained from the Scientific Research and Publication Ethics Committee of Inonu University (Decision Number: 2022/3280). In addition, necessary permissions were obtained from the relevant institution in order to conduct the research. The high-risk pregnant women who participated in the study were informed that they were free to participate in the study or not and that they could leave the study at any time.
Informed Consent
Informed consent and consent to publish were obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Use of Artificial Intelligence
Artificial Intelligence was not used.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ibıcı Akca, E., Cengızhan, S.O. & Gokbulut, N. Effectiveness of a Mindfulness-Based Stress Reduction (MBSR) Program on Stress, Anxiety, and Prenatal Attachment for High-Risk Pregnant Women: A Randomized Controlled Trial. Mindfulness 14, 2963–2974 (2023). https://doi.org/10.1007/s12671-023-02247-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-023-02247-9