Abstract
Objectives
A burgeoning literature demonstrates that self-compassion has widespread implications for numerous mental health problems, with recent research highlighting the role of self-compassion in body dissatisfaction and eating pathology. The primary purpose of this study was to investigate the relations between self-compassion, psychological distress, and eating pathology in a clinical sample of female adolescents. In addition, this study examined whether psychological distress emerged as a cross-sectional mediator of the relation between self-compassion and eating pathology.
Methods
Fifty-eight female adolescents with eating disorders (Mage = 15.45; SD = 1.49) completed the Self-Compassion Scale (SCS), Hopkins Symptom Checklist (SCL-5), and Eating Disorder Examination Questionnaire - Adolescent Version (EDE-Q).
Results
The SCS positive items (referred to as self-compassion) were negatively associated with psychological distress and eating pathology. The SCS negative items (referred to as self-criticism) were positively associated with psychological distress and eating pathology (all ps < .001). Notably, psychological distress mediated the link between self-compassion and eating pathology (ab = − 0.39, 95% percentile bootstrap confidence interval (PB CI): −0.78 to −0.09). Psychological distress also mediated the relation between self-criticism and eating pathology (ab = 0.30, 95% PB CI: 0.05 to 0.68).
Conclusions
This study supports the notion that interventions focused on increasing self-compassion and decreasing psychological distress may have important implications for eating disorder recovery in youth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Eating disorders affect adolescents’ social, emotional, cognitive, and physiological developmental processes in a detrimental manner (Quine 2012). In particular, elevated psychological distress and severe social and functional impairment have been consistently documented across all subtypes of eating disorders in youth (Swanson et al. 2011). Given that disordered eating behaviors typically develop in adolescence and have been linked with nearly every psychiatric disorder, early intervention is crucial (American Psychiatric Association 2013; Swanson et al. 2011). While family-based therapy is currently considered the first-line intervention for adolescents, data suggests that only 40–50% of youth experience full remission and that eating disorder symptoms often persist into adulthood (Rienecke 2017). As such, there is clearly a need for novel approaches that can be widely disseminated to improve treatment effectiveness.
A rapidly accumulating body of research underscores the pertinent role of self-compassion in the development and treatment of psychopathology (MacBeth and Gumley 2012), with recent research indicating the impact of self-compassion throughout the developmental spectrum (Marsh, Chan, & MacBeth, 2017; Pullmer et al. 2019a). Developmental stage theories in conjunction with extant research further highlight how self-compassion is highly relevant in adolescence, given that identity formation is a principal process during this stage of life (Erikson 1968; Neff and McGehee 2010). It is also likely the period in which self-compassion is especially needed, as adolescents are constantly evaluating and comparing themselves to others (Brown and Lohr 1987; Harter 1990). This social comparison process can contribute to continuous negative self-judgments and body dissatisfaction, which are strongly implicated in the onset and maintenance of mental health problems, including eating disorders (Neff and McGehee 2010; Neumark-Sztainer et al. 2006). Indeed, age is positively associated with self-compassion and lower levels of self-compassion have been found in adolescents when compared with young adults (Neff and McGehee 2010; Neff and Vonk 2009). Self-compassion may therefore serve to help adolescents cope with pain and suffering that can arise throughout the eating disorder recovery process as they attempt to re-establish their identities (Kelly et al. 2017; McNamara and Parsons 2016).
Compassion for others turned inward is the essence of self-compassion, which is operationally defined by three factors that interact to produce a self-compassionate mindset (Neff 2003). Each continuous factor is portrayed on positive and negative poles that exemplify compassionate and uncompassionate responses in the face of failure: self-kindness versus self-judgment, common humanity versus isolation, and mindfulness versus over-identification. Self-kindness involves treating oneself in a gentle and supportive manner. Rather than engaging in harsh self-criticism, people with higher levels of self-kindness may be more likely to accept their flaws and mistakes in a nonjudgmental manner. Common humanity entails acknowledging that imperfection, failure, and suffering are an inherent part of the human condition. People higher on this component will be more likely to view themselves as connected with others and less likely to feel isolated when considering personal shortcomings. Finally, mindfulness involves acknowledgement of distressing experiences without rumination. A mindful person may be more likely to hold difficult thoughts and emotions in objective awareness and less likely to over-identify with them or push them away (Neff and Dahm 2015).
While the components of self-compassion can be viewed as conceptually distinct, it is important to note that they mutually influence one another (Neff and Dahm 2015; Neff 2016). Take the example of a highly motivated treatment-seeking individual with anorexia nervosa-binge-eating/purging type, a disorder characterized by intense body dissatisfaction, fear of weight gain, and dietary restraint coupled with recurrent binge-eating and/or purging behavior (American Psychiatric Association 2013). Following a binge-purge episode, this individual may feel as though they have “failed” treatment. Being aware of the notion that “failure” is an inherent part of being human (e.g., “It is normal to have a slip”) reduces feelings of isolation from others (e.g., “I am not alone in this”) and increases mindfulness (e.g., “I see the slip clearly”). Practicing self-kindness (e.g., “It is okay to have a slip”) can induce less self-judgment (e.g., “No one is perfect”) and increase feelings of common humanity (e.g., “Other people are struggling with this too”). As exemplified, the components of self-compassion represent a dynamic system, which together constitute various capabilities that enable people to respond effectively to distress and disappointment (Neff and Dahm 2015; Neff 2016).
Although self-compassion and self-esteem are moderately correlated, research indicates that self-compassion promotes self-acceptance and positive psychological outcomes above and beyond self-esteem (Neff and Dahm 2015; Neff and Vonk 2009). Self-esteem can be defined as the degree to which people positively evaluate themselves (Neff and Dahm 2015). Unlike self-compassion, self-esteem has been linked with numerous maladaptive qualities (e.g., narcissism and bullying) and can fluctuate in accordance with performance outcomes (Baumeister, Bushman, & Campbell, 2000; Crocker and Park 2004). Research therefore highlights the various pitfalls of attempting to foster self-esteem. Given that self-compassion is less contingent on external circumstances, it has been deemed a more stable predictor of self-worth (Neff and Vonk 2009).
While research on self-compassion in the domain of eating pathology is nascent, studies indicate that adult females with eating disorders have lower levels of self-compassion than females without eating disorders (Ferreira et al. 2013; Kelly, Vimalakanthan, & Carter, 2014) and that self-compassion may facilitate eating disorder remission (Gale et al. 2014; Kelly and Tasca 2016). More recently, advances have been made to understand the processes through which self-compassion exerts its effect across the lifespan (Ferrari et al. 2019). A meta-analysis established a strong inverse relation between self-compassion and psychological distress in adolescents (Marsh et al., 2017). Explanatory models for the development of eating pathology provide support for the notion that psychological distress predicts body dissatisfaction and eating pathology in youth (Stice et al. 2017). Furthermore, psychological distress was identified as a potential mechanism of action for the impact of self-compassion on eating pathology in a non-clinical pediatric sample (Pullmer, Coelho, & Zaitsoff, 2019b). Overall, this research underscores the relevance of investigating self-compassion and psychological distress in adolescents with eating disorders.
It is important to note that the vast majority of studies utilized the total score of the Self-Compassion Scale (SCS; Neff 2003). The SCS total score is calculated by adding the scores of six subscales, three of which represent a compassionate or “positive” approach to suffering (i.e., self-kindness, common humanity, and mindfulness) versus a self-critical or “negative” response (i.e., self-judgment, isolation, and over-identification). Recent research provides support for a two-factor SCS model, which suggests that the “positive” and “negative” components of the SCS (hereby referred to as self-compassion and self-criticism) may be differentially related to psychopathology, particularly among clinical populations (Costa et al. 2016; Muris and Petrocchi 2017).
The primary aim of this study was to elucidate the relations between self-compassion, psychological distress, and eating pathology. We hypothesized that (1) self-compassion would be negatively associated with psychological distress and eating pathology in female adolescents with eating disorders and (2) self-criticism would be positively associated with psychological distress and eating pathology. We also explored whether, as demonstrated in a school-based sample of adolescents (Pullmer et al., 2019b), psychological distress mediated the relation between self-compassion and eating pathology, as well as the relation between self-criticism and eating pathology.
Method
Participants
Participants were 58 female adolescents (M = 15.45, SD = 1.49, range = 12–18) who were receiving specialized eating disorder treatment. With respect to ethnic-cultural background, 62.1% (n = 36) of participants self-identified as Caucasian, 20.7% (n = 12) as Asian, 13.8% (n = 8) with more than one ethnic-cultural background, and 3.4% (n = 2) as First Nations or Hispanic. Regarding gender, 100% of the sample who reported sex and gender identity (n = 57) self-identified with their assigned sex at birth. The majority of adolescents reported living with their mother and father (69%, n = 40), 27.6% (n = 16) reported living primarily with their mother, and 3.4% (n = 2) reported other living situations (e.g., living with their grandparents or adult caregiver(s)).
Participants had a mean percent median body mass index (BMI) of 91.3% (SD = 13.60). All participants met Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association 2013) criteria for an eating disorder (70.7%; n = 41 anorexia nervosa (AN)-restricting type; 10.3%; n = 6 unspecified feeding or eating disorder; 6.9%; n = 4 AN-binge-eating/purging type; 6.9% n = 4 bulimia nervosa; 3.4%; n = 2 other specified feeding or eating disorder, and 1.7%; n = 1 avoidant/restrictive food intake disorder). With respect to treatment modality, 46.6% (n = 27) were outpatients, 37.9% (n = 22) were inpatients, and 15.5% (n = 9) were day program patients (mean duration of treatment = 65.07 days; SD = 81.71; range = 0–372).
The majority of participants (63.8%, n = 37) reported engaging in compensatory behaviors over the past 28 days. Reported behaviors included excessive exercise (48.3%, n = 28), self-induced vomiting (22.4%, n = 13), laxative/diuretic use (13.8%, n = 8), and diet pill use (5.2%, n = 3). Of the sample, 22.4% (n = 13) reported binge-eating episodes over the past 28 days.
Procedure
All procedures were approved by the Research Ethics Boards at Simon Fraser University and The University of British Columbia (BC)/Children’s and Women’s Health Centre of BC. Data were collected as part of a larger study investigating the role of body checking on eating pathology (Zaitsoff, Pullmer, & Coelho, submitted). Youth were invited to participate if they were at least 10 years of age (i.e., early adolescence as defined by the World Health Organization, 2014), receiving treatment at an eating disorders program, proficient in English, able to understand and answer study-related forms and questionnaires, and not part of an ongoing study.
Eligible and interested youth met with their parent(s)/guardian(s) and a research assistant to obtain study information. Participants completed questionnaires assessing socio-demographic variables, self-compassion, psychological distress, and eating pathology. Study data were collected and managed on paper and via Research Electronic Data Capture (REDCap) tools hosted at the hospital where the study took place. REDCap is a secure, web-based application designed to support data capture for research studies (Harris et al. 2009). Written assent and parental consent were obtained from 59 adolescents to administer questionnaires and access medical records; however, one parent subsequently withdrew consent yielding a total of 58 participants.
Measures
Participant Characteristics
Participants completed a demographic questionnaire designed for this study assessing sex, gender identity, ethnic-racial background, and living situation. The following data were extracted from patient medical records: age, eating disorder diagnosis, current treatment duration, and weight and height, which were recorded as close as possible to the time of study participation (i.e., within 2 weeks). Percent median BMI values were examined in relation to the World Health Organization values for the 50th BMI percentile, with values under 100 indicating a lower than median BMI for age and sex (Onis et al. 2007).
Self-Compassion
The Self-Compassion Scale was used to measure trait self-compassion (SCS; Neff 2003). In accordance with the two-factor structure of the SCS (Costa et al. 2016; Muris and Petrocchi 2017), this measure contains 13 positively worded items representing self-compassion (e.g., “I am kind to myself when I am experiencing suffering”) and 13 negatively worded items representing self-criticism (e.g., “I am disapproving and judgmental about my own flaws and adequacies”). All items are rated on a 5-point Likert scale, with higher scores indicating higher self-compassion and self-criticism, respectively. The SCS yields excellent psychometric properties in adolescents (e.g., Cunha, Xavier, & Castilho, 2016). Internal consistency (α) in the current study was 0.90 for self-compassion and 0.92 for self-criticism.
Psychological Distress
The Hopkins Symptom Checklist (SCL-5; Aasheim et al. 2012) was used to measure psychological distress (i.e., depressive and anxiety symptoms). Participants were asked whether they had been bothered by any of the following during the past 2 weeks: (1) feeling fearful, (2) nervousness or shakiness inside, (3) feeling hopeless about the future, (4) feeling blue, and (5) worrying too much about things. Items are rated on a 4-point Likert scale, with higher scores indicating higher psychological distress. This measure is widely used in adolescents (Skrove, Romundstad, & Indredavik, 2013). Internal consistency in the current sample was 0.83.
Eating Pathology
The Eating Disorder Examination Questionnaire (EDE-Q) - Adolescent Version was used to assess eating pathology (Mond et al. 2014). This measure contains 36 items and assesses the severity and frequency of eating disorder symptoms over the past 28 days on a 7-point scale (e.g., “On how many days, out of the past 28 days, have you been deliberately trying to limit the amount of food you eat to influence your shape or weight?”). A global score was calculated utilizing the average of 22 subscale items (Aardoom et al. 2012), with higher scores representing more severe eating pathology. Internal consistency in the current sample was 0.96.
Data Analyses
As reported by Fritz and Mackinnon (2007), 59 participants are indicated for simple mediation analyses (power = 0.80, expected R2 = 0.39–0.59). Complete case analysis was utilized given the low proportion of item-level missingness across all participants and measures (i.e., 0.26%). Participants (n = 3) were excluded from simple mediation analyses if they were missing > 10% of items on a specific questionnaire (Graham 2012).
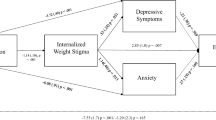
Descriptive statistics were calculated for socio-demographic variables, anthropometric measurements, self-compassion, self-criticism, psychological distress, and eating pathology. Pearson’s correlations were computed to investigate associations between main study variables. Given the utility of cross-sectional mediation models to determine direct and indirect relations between variables, simple mediation analyses were conducted via PROCESS Model 4 to examine whether self-compassion (Model 1) and self-criticism (Model 2) were related to eating pathology through psychological distress (Hayes 2017; Fig. 1). PROCESS uses an HC3 estimator to account for heteroscedasticity. Indirect effects were considered significant when the 95% percentile bootstrap confidence interval (PB CI) did not contain zero (bootstrap N = 10,000).
Results
Relations Between Self-Compassion, Self-Criticism, Psychological Distress, and Eating Pathology
Self-compassion was negatively associated with psychological distress and eating pathology, and self-criticism was positively associated with psychological distress and eating pathology (Table 1). Simple mediation analyses for Model 1 (Table 2) indicated that self-compassion was indirectly related to eating pathology through psychological distress. Participants who were more self-compassionate were less likely to be psychologically distressed (a = − 0.48), and participants who were less psychologically distressed were less likely to endorse severe eating pathology (b = 0.81). A bootstrap confidence interval for the indirect effect (ab = − 0.39; SE = 0.18) was entirely below zero (− 0.78 to − 0.09). There was also evidence that self-compassion was negatively related to eating pathology independent of its effect on psychological distress (c′ = − 1.10, p < .001).
Simple mediation analyses for Model 2 (Table 3) revealed that self-criticism was indirectly related to eating pathology through psychological distress. Participants who were more self-critical were more likely to be psychologically distressed (a = 0.47), and those who were more psychologically distressed were more likely to endorse severe eating pathology (b = 0.63). A bootstrap confidence interval for the indirect effect (ab = 0.30; SE = 0.16) did not encapsulate zero (0.05 to 0.68). Self-criticism was also positively related to eating pathology independent of its effect on psychological distress (c′ = 1.00, p < .001).
Discussion
The current study examined the relations between self-compassion, psychological distress, and eating pathology in female adolescents with eating disorders. As hypothesized, self-compassion was negatively associated with psychological distress and eating pathology. In addition, self-criticism was positively associated with psychological distress and eating pathology. Exploratory analyses revealed that psychological distress mediated the relation between self-compassion and eating pathology and between self-criticism and eating pathology.
Overall, the results are concordant with research demonstrating a strong negative link between self-compassion and eating pathology in adults (Braun, Park, & Gorin, 2016). Our findings are also compatible with research highlighting the role of self-compassion in adolescent body image (Rodgers et al. 2018) and emotional eating in adolescents who were overweight/obese without eating disorders (Gouveia, Canavarro, & Moreira, 2018). It is therefore not surprising that self-compassion and self-criticism were directly related to eating pathology in the current study, particularly given that eating disorders are characterized by harsh self-judgment and related cognitions. The finding that both self-compassion and self-criticism are indirectly related to eating pathology through psychological distress is novel and corroborates recent research identifying this mechanism of action in adolescents without eating disorders (Pullmer et al., 2019b). It may be that employing a self-compassionate mindset evokes adaptive emotion regulation strategies, which serves to reduce psychological distress and the impact of perceived stress on eating pathology and treatment-related outcomes (Gouveia et al. 2018).
With respect to the self-compassion literature at large, research suggests that the positive and negative poles of self-compassion may be differentially related to psychopathology (Muris and Petrocchi 2017), with a recently conducted study underscoring this disparate relationship in a large sample of adults with depressive symptoms (Lopez, Sanderman, & Schroevers, 2018). Given that both self-compassion and self-criticism were directly and indirectly related to eating pathology, results from the current study do not provide support for this notion in female adolescents with eating disorders, suggesting that findings may differ depending on the disorder in question. It may also be that other variables interact with self-compassion and self-criticism to influence disordered eating. Specifically, research implicates both shame and fear of self-compassion as pertinent constructs to consider over the course of treatment. From a theoretical standpoint, Goss and Allan (2009) indicate that shame contributes to the maintenance of eating pathology. It is further posited that while self-compassion is the antidote to shame, individuals differ in the extent to which they fear self-compassion, which may impact their ability to build self-compassion and experience improved health outcomes (Gilbert 2005). Upon establishing the protective role of self-compassion in adults, research demonstrates not only that shame and eating pathology mutually influence one another (Kelly and Tasca 2016), but also that high fear of self-compassion in conjunction with low trait self-compassion predicts eating pathology and associated shame over time (Kelly, Carter, & Borairi, 2013). Although the current study did not measure shame or fear of self-compassion, research in adults insinuates the potential relevance of both of these constructs in adolescents.
Limitations and Future Research
With respect to study limitations, the cross-sectional design and sample composition (i.e., females only) precludes our ability to determine causality and generalize findings across the gender spectrum. Additionally, self-report questionnaires administered at the same timepoint are subject to the common method bias. As well, the current sample size was just shy of the minimum sample size required for simple mediation. Furthermore, while diagnoses were provided by a psychiatrist or psychologist specialized in eating disorders as part of a multidisciplinary team assessment, structured and validated clinical interviews were not utilized. It is also important to note that adolescents in this study presented with different diagnostic classifications and were at various stages of treatment. Although we did not have an adequate sample size to conduct between-group analyses, it is possible that self-compassion and self-criticism have distinctive roles at varying stages of treatment and across eating disorder diagnoses. Indeed, research in adults indicates that increases in self-compassion early in treatment predict improved treatment outcomes (Kelly et al. 2013) and that individuals with anorexia nervosa are less likely to experience increases in self-compassion when compared to those with bulimia nervosa or other specified feeding or eating disorder (Gale et al. 2014). Thus, while our study provides support for the role of self-compassion in female adolescents with eating disorders, longitudinal research is needed to elucidate between-group differences and identify barriers to the development of self-compassion.
Finally, this study examined between-person predictors of outcome. Recent research in adults demonstrates the within-persons effects of self-compassion in the realms of body image and eating pathology by employing ecological momentary assessment or daily diary methodologies (Kelly and Tasca 2016; Thogersen-Ntoumani et al. 2017). Research in adult females with eating disorders provides further evidence for the utility of examining within-person variance by implicating that increased self-compassion may help break the cyclical relation between eating pathology and shame within patient trajectories (Kelly and Tasca 2016). Empirical examinations of within-persons effects therefore highlight a promising avenue for future research in adolescents.
The current study adds to a growing body of research implicating the role of self-compassion in eating disorders and related pathology. This study further demonstrates how self-compassion and self-criticism are related to eating pathology by underscoring psychological distress as a potentially important pathway for youth with and without eating disorders (Pullmer et al., 2019b). Results suggest that attending to self-compassion and psychological distress might ultimately help enhance effective elements of treatment and develop more targeted interventions to maximize health outcomes.
References
Aardoom, J. J., Dingemans, A. E., Slof Op’t Landt, M. C., & Van Furth, E. F. (2012). Norms and discriminative validity of the Eating Disorder Examination Questionnaire (EDE-Q). Eating Behaviors, 13, 305–309.
Aasheim, V., Waldenstrom, U., Hjelmstedt, A., Rasmussen, S., Pettersson, H., & Schytt, E. (2012). Associations between advanced maternal age and psychological distress in primiparous women, from early pregnancy to 18 months postpartum. An International Journal of Obstetrics and Gynaecology, 119, 1108–1116.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Baumeister, R. F., Bushman, J., & Campbell, W. K. (2000). Self-esteem, narcissism, and aggression: does violence result from low self-esteem from threatened egotism. Current Directions in Psychological Science, 9, 26–29.
Braun, T. D., Park, C. L., & Gorin, A. (2016). Self-compassion, body image, and disordered eating: A review of the literature. Body Image, 17, 117–131.
Brown, B., & Lohr, M. J. (1987). Peer-group affiliation and adolescent self-esteem: an integration of ego-identity and symbolic-interaction theories. Journal of Personality and Social Psychology, 52, 47–55.
Costa, J., Maroco, J., Pinto-Gouveia, J., Ferreira, C., & Castilho, P. (2016). Validation of the psychometric properties of the Self-Compassion Scale. Testing the factorial validity and factorial invariance of the measure among borderline personality disorder, anxiety disorder, eating disorder and general populations. Clinical Psychology & Psychotherapy, 23, 460–468.
Crocker, J., & Park, L. E. (2004). The costly pursuit of self-esteem. Psychological Bulletin, 130, 392–414.
Cunha, M., Xavier, A., & Castilho, P. (2016). Understanding self-compassion in adolescents: validation study of the Self-Compassion Scale. Personality and Individual Differences, 93, 56–62.
Erikson, E. (1968). Identity: youth and crisis. New York: Norton.
Ferreira, C., Pinto-Gouveia, J., & Duarte, C. (2013). Self-compassion in the face of shame and body image dissatisfaction: Implications for eating disorders. Eating Behaviours, 14, 207–210.
Ferrari, M., Hunt, C., Harrysunker, A., Abbott, M. J., Beath, A. P., & Einstein, D. A. (2019). Self-compassion interventions and psychosocial outcomes: a meta-analysis of RCTs. Mindfulness, 10, 1455–1473.
Fritz, M. S., & MacKinnon, D. P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18, 233–239.
Gale, C., Gilbert, P., Read, N., & Goss, K. (2014). An evaluation of the impact of introducing compassion focused therapy to a standard treatment programme for people with eating disorders. Clinical Psychology & Psychotherapy, 21, 1–12.
Graham, J. W. (2012). Missing data: Analysis and design. New York, NY: Springer.
Gilbert, P. (2005). Compassion: conceptualizations, research and use in psychotherapy. London: Routledge.
Goss, K., & Allan, S. (2009). Shame, pride and eating disorders. Clinical Psychology & Psychotherapy, 16, 303–316.
Gouveia, M. J., Canavarro, M. C., & Moreira, H. (2018). Associations between mindfulness, self-compassion, difficulties in emotion regulation, and emotional eating among adolescents with overweight/obesity. Journal of Child and Family Studies, 28, 273–285.
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Information, 42, 377–381.
Harter, S. (1990). Self and identity development. In S. S. Feldman & G. R. Elliot (Eds.), At the threshold: the developing adolescent (pp. 352–387). Cambridge: Harvard University Press.
Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford Press.
Kelly, A. C., & Tasca, G. A. (2016). Within-persons predictors of change during eating disorders treatment: an examination of self-compassion, self-criticism, shame, and eating disorder symptoms. International Journal of Eating Disorders, 49, 716–722.
Kelly, A. C., Carter, J. C., & Borairi, S. (2013). Are improvements in shame and self-compassion early in eating disorders treatment associated with better patient outcomes? International Journal of Eating Disorders, 47, 54–64.
Kelly, A. C., Vimalakanthan, K., & Carter, J. C. (2014). Understanding the roles of self-esteem, self-compassion and fear of self-compassion in eating disorder pathology: an examination of female students and eating disorder patients. Eating Behaviours, 15, 388–391.
Kelly, A. C., Wisniewski, L., Martin-Wagar, C., & Hoffman, E. (2017). Group-based compassion-focused therapy as an adjunct to outpatient treatment for eating disorders: a pilot randomized controlled trial. Clinical Psychology & Psychotherapy, 24, 475–482.
Lopez, A., Sanderman, R., & Schroevers, M. J. (2018). A close examination of the relationship between self-compassion and depressive symptoms. Mindfulness, 9, 1470–1478.
MacBeth, A., & Gumley, A. (2012). Exploring compassion: a meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32, 545–552.
Marsh, I. C., Chan, S. W., & MacBeth, A. (2017). Self-compassion and psychological distress in adolescents – a meta-analysis. Mindfulness, 9, 1011–1027.
McNamara, N., & Parsons, H. (2016). ‘Everyone here wants everyone else to get better’: the role of social identity in eating disorder recovery. British Journal of Social Psychology, 4, 662–680.
Mond, J., Hall, A., Bentley, C., Harrison, C., Gratwick-Sarll, K., & Lewis, V. (2014). Eating-disordered behaviour in adolescent boys: Eating Disorders Examination Questionnaire norms. International Journal of Eating Disorders, 47, 335–341.
Muris, P., & Petrocchi, N. (2017). Protection or vulnerability? A meta-analysis of the relations between the positive and negative components of self-compassion and psychopathology. Clinical Psychology & Psychotherapy, 24, 373–383.
Neff, K. D. (2003). The development and validation of a scale to measure self-compassion. Self and Identity, 2, 223–250.
Neff, K. D. (2016). The Self-Compassion Scale is a valid and theoretically coherent measure of self-compassion. Mindfulness, 7, 264–274.
Neff, K. D., & Dahm, K. A. (2015). Self-compassion: What it is, what it does, and how it relates to mindfulness. In B. Ostafin, M. Robinson, & B. Meier (Eds.), Handbook of mindfulness and self-regulation. New York: Springer.
Neff, K. D., & McGehee, P. (2010). Self-compassion and psychological resilience among adolescents and young adults. Self and Identity, 9, 225–240.
Neff, K. D., & Vonk, R. (2009). Self-compassion versus global self-esteem: two different ways of relating to oneself. Journal of Personality, 77, 23–50.
Neumark-Sztainer, D., Paxton, S. J., Hannan, P. J., Haines, J., & Story, M. (2006). Does body satisfaction matter? Five-year longitudinal associations between body satisfaction and health behaviours in adolescent females and males. Journal of Adolescent Health, 39, 244–251.
Onis, M., Onyango, A., Borghi, E., Siyam, A., Nishida, C., & Siekmann, J. (2007). Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization, 85, 660–667.
Pullmer, R., Chung, J., Samson, L., Balanji, S., & Zaitsoff, S. L. (2019a). A systematic review of the relation between self-compassion and depressive symptoms in adolescents. Journal of Adolescence, 74, 210–220.
Pullmer, R., Coelho, J. S., & Zaitsoff, S. L. (2019b). Kindness begins with yourself: the role of self-compassion in adolescent body satisfaction and eating pathology. International Journal of Eating Disorders, 52, 809–816.
Quine, D. (2012). Eating disorders in childhood and adolescence: Assessment and treatment issues. In J. R. Fox & K. P. Goss (Eds.), Eating and its Disorders (pp. 442–466). Hoboken: Wiley-Blackwell.
Rienecke, R. D. (2017). Family-based treatment of eating disorders in adolescence: current insights. Adolescent Health, Medicine and Therapeutics, 8, 69–79.
Rodgers, R. F., Donovan, E., Cousineau, T., Yates, K., McGowan, K., Cook, E., et al. (2018). BodiMojo: efficacy of a mobile-based intervention in improving body image and self-compassion among adolescents. Journal of Youth and Adolescence, 47, 1363–1372.
Skrove, M., Romundstad, P., & Indredavik, M. S. (2013). Resilience, lifestyle and symptoms of anxiety and depression in adolescence: the Young-HUNT study. Social Psychiatry and Psychiatric Epidemiology, 48, 407–416.
Stice, E., Gau, J. M., Rohde, P., & Shaw, H. (2017). Risk factors that predict future onset of each DSM-5 eating disorder: predictive specificity in high-risk adolescent females. Journal of Abnormal Psychology, 126, 38–51.
Swanson, S. A., Crow, S. J., Le Grange, D., Swendsen, J., & Merikangas, K. R. (2011). Prevalence and correlates of eating disorders in adolescents: results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry, 68, 714–723.
Thogersen-Ntoumani, C., Dodos, L., Chatzisarantis, N., & Ntoumanis, N. (2017). A diary study of self-compassion, upward social comparisons, and body image-related outcomes. Applied Psychology. Health and Well-Being, 9, 242–258.
World Health Organization (2014). Adolescence: A period needing special attention. Geneva: Author.
Zaitsoff, S. L., Pullmer, R., & Coelho, J. S. (submitted). A longitudinal examination of body checking behaviours and eating disorder pathology in community sample of adolescent males and females.
Acknowledgments
We would like to thank Dr. Alexander Chapman, Dr. Allison Kelly, and Dr. Brent McFerran for their involvement and feedback on Rachelle Pullmer’s dissertation. Thanks are also due to Sarah Anderson, Avarna Fernandes, and Janet Suen for their role in recruitment and data collection, as well as to the patients who participated in this study.
Funding
This paper is based, in part, on Rachelle Pullmer’s doctoral dissertation and was conducted in the context of a larger study funded by the Mental Health and Concurrent Disorders Clinical and Translational Research Seed Grant from the Provincial Health Services Authority/British Columbia Children’s Hospital Research Institute (Principal Investigators: Dr. Shannon Zaitsoff and Dr. Jennifer Coelho; Clinical Trainee: Rachelle Pullmer) and Dr. Shannon Zaitsoff’s Departmental Research Grant (Simon Fraser University). The Vanier Canada Graduate Scholarship, awarded to Rachelle Pullmer from the Canadian Institutes of Health Research, also supported this project.
Author information
Authors and Affiliations
Contributions
RP: designed the study, conducted data analyses, and wrote the paper. SLZ: collaborated with the design and editing of the final manuscript. JSC: oversaw execution of the study, and collaborated with the design and editing of the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by Simon Fraser University and The University of British Columbia/Children’s and Women’s Health Centre of BC, and was therefore performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Statement of Informed Consent
Informed consent was obtained for all participants prior to their inclusion in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pullmer, R., Zaitsoff, S.L. & Coelho, J.S. Self-Compassion and Eating Pathology in Female Adolescents with Eating Disorders: The Mediating Role of Psychological Distress. Mindfulness 10, 2716–2723 (2019). https://doi.org/10.1007/s12671-019-01254-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-019-01254-z