Abstract
Objectives
Mindfulness training for smoking cessation may work by lessening the association between craving and smoking. However, no studies have tested whether baseline craving may be an indicator of individual smokers who might benefit more from receiving mindfulness training.
Methods
This study evaluated baseline craving strength and frequency as treatment moderators in a randomized controlled trial for smoking cessation comparing mobile (smartphone-based) mindfulness training plus ecological momentary assessment (MMT-EMA) to ecological momentary assessment (EMA). Participants included 325 adult smokers (71.7% female; 81.4% White; mean age = 41.27). Craving strength and frequency were assessed with the Craving Experiences Questionnaire. Smoking was measured as cigarettes per day (CPD) at baseline and six-month follow-up. Moderated regression models were conducted.
Results
There was a significant interaction between treatment group and craving strength, but not craving frequency, in the prediction of smoking. Follow-up analyses indicated that baseline craving strength predicted benefit from receiving MMT-EMA, such that higher craving strength at baseline was significantly associated with greater reductions in CPD from baseline to six months in the MMT-EMA group, but not in the EMA group.
Conclusions
Findings suggest that baseline craving strength may be a prognostic marker of benefit from smartphone app-delivered mindfulness training for smoking cessation. Future work is warranted for understanding baseline craving as a moderator of mindfulness training for smoking cessation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
One in ten deaths is attributed to tobacco use worldwide (Reitsma et al. 2017). In the USA, 15.1% of the population or 36.5 million people are current cigarette smokers, with 75.7% or 27.6 million of these being daily smokers (Jamal et al. 2018). Finding strategies to help smokers quit remains of critical importance.
Several meta-analytic reviews indicate that mindfulness-based programs (MBPs) may be promising for smoking cessation (Goldberg et al. 2017; Li et al. 2017; Maglione et al. 2017; Oikonomou et al. 2017). Mindfulness is commonly defined as the process of bringing non-judgmental awareness to present-moment experience (Kabat-Zinn 2005). MBPs for smoking cessation emphasize formal training in mindfulness meditation to enhance one’s ability to notice and accept challenging internal experiences, such as negative affect and craving (Bowen et al. 2010; Bowen and Marlatt 2009; Brewer et al. 2011).
Standard behavioral treatments for smoking cessation focus on helping smokers avoid situations that trigger craving and practice distraction or substitution when cravings occur. MBPs, on the other hand, focus on helping smokers experience and attend to craving without smoking, which is theorized to disrupt the core underlying associative learning processes that initiate and perpetuate smoking behavior. For example, mindfulness training is intended to foster new associative learning related to craving experiences, such as learning that cravings can be felt and experienced as they are without engaging in smoking. This new learning can then compete with existing associations (i.e., this craving will not go away or will get worse unless I smoke or distract myself). While avoiding cues and using substitute behaviors may reduce the frequency of craving and prevent smoking in response to cravings, these strategies may not foster new core learning about cravings and may leave an individual prone to relapse when they have a craving in the future and an adequate substitution or distracting activity is not immediately available. Hence, because MBPs focus on helping smokers experience and attend to craving without smoking, MBPs for smoking cessation are hypothesized to work by lessening the association between craving and smoking (Brewer et al. 2013; Levin et al. 2015).
Preliminary studies from our group provide support for the reduced association between craving and smoking as a mechanism of change in MBPs for reduced smoking. In one recent study, we found that smartphone app-based mindfulness training for smoking cessation (the Craving to Quit app) lessened the association between craving and smoking to a greater extent than a control app (Garrison et al. 2018). Although this did not lead to a reduction in smoking with smartphone app-based mindfulness training as compared to control, it may support smoking cessation in the longer term. This finding was in line with an earlier study of in-person mindfulness training for smoking cessation, in which we found that increased engagement in daily mindfulness practice lessened the association between craving and smoking following mindfulness training (Elwafi et al. 2013). Furthermore, in that trial, in-person mindfulness training was found to significantly reduce smoking compared with control (Brewer et al. 2011). Moreover, there is evidence that mindfulness practice attenuates the link between craving and substance use among individuals receiving MBPs for alcohol and other drug use disorders (Enkema and Bowen 2017).
Importantly, understanding the mechanisms underlying MBPs can assist in the identification of individuals who might benefit most from receiving MBPs. Given the hypothesized mechanism underlying MBPs for smoking cessation, it stands to reason that smokers who experience higher levels of craving may benefit more from MBPs. In addition, our recent trial of smartphone app-based mindfulness training for smoking cessation found that completing a greater number of modules in the mindfulness training program lessened the positive association between craving strength and smoking, but not between craving frequency and smoking (Garrison et al. 2018). These findings also suggest that MBPs for smoking cessation might be particularly effective for smokers who experience strong craving.
To date, there is limited empirical knowledge on which types of smokers may benefit more or less from MBPs. To our knowledge, no studies have evaluated whether baseline craving moderates the efficacy of MBPs for smoking cessation. In the current study, we tested baseline craving strength and frequency as treatment moderators in our recent trial of the Craving to Quit app for smoking cessation (Garrison et al. 2018). In that trial, there were no significant group differences in smoking outcomes between those who received the Craving to Quit app versus the control app (Garrison et al. 2018). However, greater mindfulness training module completion was associated with a reduced association between craving strength and smoking among those receiving Craving to Quit. Therefore, the current study tested the a priori hypothesis that baseline craving strength would moderate the effect of Craving to Quit on smoking, such that smokers with higher baseline craving strength would benefit more relative to smokers with lower baseline craving strength.
Method
Participants
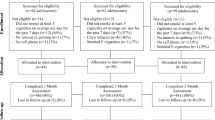
Participants included 325 adult smokers who were a part of the modified intent-to-treat (ITT) sample in the parent study (Garrison et al. 2018) defined by completing at least 1 day of treatment. Eligibility criteria included 18–65 years of age, smoking > 5 cigarettes per day, < 3 months of abstinence from smoking in the past year, own a iPhone/Android smartphone, and motivated to quit as evidenced by at least 8/10 on the Contemplation Ladder (Biener and Abrams 1991) and at least 4/5 on the Action item of the Readiness to Change Questionnaire (Rollnick et al. 1992). Table 1 provides a summary of demographic and treatment-related variables for the modified ITT sample used in the current secondary data analysis study. A power analysis was previously reported for the clinical trial (Garrison et al. 2015, 2018).
Procedures
The parent trial was a pragmatic randomized controlled trial (RCT) conducted entirely via smartphone. Participants provided online informed consent and were directed to complete all study assessments via smartphone. This included their smartphone app and links to study surveys hosted on Yale Qualtrics Survey Tool, an online survey platform optimized for mobile.
Enrolled participants were randomized to receive either an app for mobile mindfulness training with ecological momentary assessment (MMT-EMA; i.e., the Craving to Quit app) or an app delivering ecological momentary assessment only (EMA; control app). The MMT-EMA group received a 22 day treatment program via the Craving to Quit app, which includes mindfulness for smoking cessation training modules, including formal meditation practices (i.e., body scan, breath awareness, and loving-kindness) and an informal (on-the-go) mindfulness practice for responding to craving. Both the MMT-EMA and EMA groups completed EMA procedures in which they responded to multiple daily app-based “check-ins” regarding smoking behavior, craving, and other smoking-related factors. Following the 22-day treatment, participants completed follow-up surveys one, three, and six months from treatment initiation. For further details regarding the parent trial, please refer to the main outcome paper (Garrison et al. 2018) and protocol paper (Garrison et al. 2015).
Measures
Measures for the current study included smoking, craving strength, and craving frequency, collected at baseline and six months post-treatment-initiation. At these time points, subjects were e-mailed a link to the study survey hosted on Yale Qualtrics Survey Tool, optimized for mobile. Additional measures not analyzed here were described previously (Garrison et al. 2015, 2018). Smoking was measured as self-reported cigarettes per day (CPD). Craving strength and craving frequency were measured using the Craving Experience Questionnaire (CEQ) (May et al. 2014), a 22-item self-report questionnaire. The CEQ was developed based on elaborated intrusion theory, which conceptualizes craving as a cognitive-affective phenomenon that begins as an intrusive thought in response to an external or internal cue and is elaborated into an embodied (i.e., multi-sensory) cognition (May et al. 2014). The scale was developed based on studies of multiple consummatory behaviors (cigarettes, alcohol, chocolate, food) on multiple time scales (“now” to “past week”). Craving strength and frequency are measured in terms of craving intensity, imagery vividness, and cognitive intrusiveness. Internal consistency was good for the craving strength subscale (Cronbach’s alpha = 0.87) and the craving frequency subscale (Cronbach’s alpha = 0.89).
Data Analyses
Moderated regression models (Aiken and West 1991) were conducted to evaluate the interaction of craving strength and treatment group, as well as craving frequency and treatment group (in a separate model), in the prediction of CPD at 6 months. Interaction models included the treatment group variable, the craving variable, the interaction term, and the baseline CPD as predictors of CPD at 6 months. Additionally, in the omnibus interaction model, we controlled for craving strength when testing craving frequency by treatment group and vice versa. In regard to missing data, 62 participants or 19.1% of the sample were missing data on CPD at 6 months. Attrition analyses revealed that treatment group, baseline craving strength and frequency, gender, age, and race were not related to having missing data on CPD at six months. For all models, all available data were utilized, and maximum likelihood estimation was used to estimate model parameters (Witkiewitz et al. 2014b). We explored the nature of the interaction effect with two follow-up analyses. First, we tested the association between the baseline craving variable and change in CPD from baseline to 6 months within each treatment group separately (e.g., association between baseline craving and change in CPD in the MMT-EMA group). Second, we compared mean changes from baseline to 6 months in CPD by treatment group among those with low (1 standard deviation [SD] or more below mean), moderate (score was in a range that did not exceed 1 SD above/below mean), and high (1 SD or more above the mean) baseline scores for the craving variables.
Results
Table 2 provides the bivariate correlations and descriptive statistics for study variables. There were no significant differences in baseline craving strength or frequency between the treatment groups. Moderated regression analyses revealed a significant interaction between treatment group and baseline craving strength in the prediction of CPD at 6 months (B = − 0.079, SE = 0.038, p = 0.042). On the other hand, there was no significant interaction between treatment group and baseline craving frequency in the prediction of CPD at six months (B = − 0.46, SE = 0.038, p = 0.238).
Follow-up analyses to probe the nature of the craving strength by treatment group interaction indicated that among those who received MMT-EMA, higher baseline craving strength was significantly associated with greater reductions in CPD from baseline to six months (B = − 0.07; SE = 0.028; β = − 0.215; p = 0.018; R2 = 0.05), as seen in Fig. 1. Among those who received EMA-only, baseline craving strength was not significantly associated with changes in CPD from baseline to six months (B = 0.004; SE = 0.033; β = 0.01; p = 0.909; R2 = 0.001).
Further follow-up analyses showed that among individuals with “high baseline craving strength” (n = 50), those who received MMT-EMA reduced their CPD by approximately nine (mean = 8.66, SD = 5.99) cigarettes on average from baseline to six months, whereas those who received EMA-only reduced their CPD by approximately 6 (mean = 5.68, SD = 7.88) cigarettes on average. Although demonstrating a small-to-medium effect size (Cohen’s d = 0.41), this mean difference did not reach statistical significance (p = 0.197). Among individuals with “moderate baseline craving strength” (n = 224), those who received MMT-EMA reduced their CPD by approximately six (mean = 6.39, SD = 7.34) cigarettes on average, whereas those who received EMA-only reduced their CPD by approximately seven (mean = 7.19, SD = 6.05) cigarettes on average. This mean difference was not significant (Cohen’s d = 0.11; p = 0.492). Finally, among individuals with “low baseline craving strength” (n = 51), those who received MMT-EMA reduced their CPD by approximately six (mean = 5.72, SD = 7.20) cigarettes on average, whereas those who received EMA-only reduced their CPD by approximately 6 (mean = 6.3, SD = 6.05) cigarettes on average. This mean difference was not significant (Cohen’s d = 0.08; p = 0.781).
Discussion
The current study evaluated baseline craving strength and frequency as treatment moderators in a RCT comparing mobile mindfulness training plus ecological momentary assessment to ecological momentary assessment only (Garrison et al. 2018). We found a significant interaction effect for craving strength, but not craving frequency. That is, there was a significant interaction between treatment group and baseline craving strength in the prediction of CPD at 6 months following treatment initiation. Follow-up analyses to describe the nature of the interaction indicated that higher baseline craving strength was significantly associated with greater reductions in CPD from baseline to 6 months in the MMT-EMA group, but there was no significant association in the EMA group.
These findings are in line with our a priori hypothesis that smokers with higher craving strength, in particular, might benefit most from MMT-EMA. Our hypothesis was based on findings from our parent RCT in which, despite a reduction in both craving strength and frequency (and smoking) across treatment in both groups, only the relationship between craving strength and smoking was reduced and only for MMT-EMA (Garrison et al. 2018). Our findings are also consistent with prior theoretical (Brewer et al. 2013; Witkiewitz et al. 2014a) and empirical work (Elwafi et al. 2013; Enkema and Bowen 2017), suggesting that one specific mechanism of action in MBPs is helping smokers work mindfully with craving experiences. MBPs teach smokers how to practice mindful observation of craving, to learn to work mindfully with cravings rather than smoke, in order to weaken the conditioned association between craving and smoking (Witkiewitz et al. 2014a). Targeting the core learning processes that maintains smoking is intended to help smokers manage cravings that will very likely continue to arise in both the short and long term (Brewer et al. 2013). Our work suggests that cravings continue to arise for smokers, as evident by a similar level of craving (strength and frequency) between groups, yet the positive association between craving and smoking was reduced with mindfulness training. Despite a high correlation between craving strength and craving frequency, we found differential interaction effects with treatment group on CPD. We note that the omnibus interaction model controlled for craving strength when testing craving frequency by treatment group and vice versa. Therefore, when holding craving frequency constant, there was a significant interaction between craving strength and treatment condition on smoking outcomes. Additionally, the internal consistencies of both the craving strength and craving frequency scores were high, lending support to examining these factors separately. These findings suggest that MBPs may be particularly well-suited for smokers who report high baseline craving strength. Future work is needed to fully differentiate the effects of MBPs on craving strength and frequency, their interaction, and effects on smoking.
Moreover, our findings support the hypothesis that MBPs for smoking cessation may work by reducing the association between craving strength and smoking, but not by reducing the strength or frequency of cravings alone. This is in line with the approach in MBPs to work mindfully with cravings rather than avoid them.
Our finding indicated that baseline craving strength was associated with greater reductions in smoking for those who received MMT-EMA, among whom baseline craving strength accounted for 5% of the variance in change in CPD (R2 = 0.05). Although the magnitude of this association is low, it is in line with the magnitude of associations between psychological and behavioral variables reported in research on the topics of smoking, mindfulness, and addictive behaviors (for meta-analyses see: Gass et al. 2014; Karyadi et al. 2014). One possibility is that the heterogeneity of the current sample of smokers contributed to the low effect size. In particular, the current sample had a wide range of smoking, with some reporting five cigarettes per day, and others reporting > 30 cigarettes per day. Future work is needed with larger samples to test the strength of the association in homogeneous subgroups (e.g., one pack/day smokers) and to test whether craving strength predicts mindfulness treatment outcomes beyond other baseline factors.
In order to better understand the interaction effect between baseline craving strength and treatment group on smoking, we compared CPD at baseline and 6 months among those with high, medium, and low baseline craving strengths and found no significant differences. However, the parent clinical trial was powered to test efficacy (Garrison et al. 2015, 2018) and may not be sufficiently powered for such subgroup analyses. Future studies with larger samples of craving level subgroups could help to determine whether MBPs for smoking cessation are more efficacious among smokers with high baseline craving. It would also be useful for future research to validate cutoffs for high, medium, and low craving strengths from multiple samples. The cutoffs in this study were based on the mean scores in just one sample. It is also possible that group differences in smoking would emerge with extended training (beyond the 22-day treatment in the current trial) or with longer-term follow-up (beyond six months), which can be tested in future studies.
Limitations and Future Research
The current study has several possible limitations. First, the parent trial was conducted entirely via smartphone including online surveys optimized for mobile; therefore, it is possible that some participants did not pay careful attention to assessments. Future studies should include “attention checks” (e.g., “answer “a” to this question”) to ensure attentiveness to online surveys. Second, as noted in the main outcome paper, the number of treatment starters in each treatment group was imbalanced (MMT-EMA, n = 143; EMA, n = 182), potentially due to the extra step of being directed to the Craving to Quit website to complete questionnaires before downloading the app for the MMT-EMA group. It is possible that individuals who experience strong craving may have been less likely to start treatment and engage with the app. However, baseline craving strength was not significantly correlated with being a treatment starter (r = − 0.037, p = 0.404). Third, the measure of baseline craving (CEQ) was a retrospective self-report of craving experiences “in the last week.” While the parent RCT employed intensive EMA during treatment, EMA was not conducted prior to treatment initiation. Baseline craving experiences assessed via EMA rather than retrospective self-report could have resulted in different findings. Finally, the sample in this study was predominantly white and female (58% participants were white and female); therefore, the findings may not generalize to other populations, and studies with more representative samples are needed, as well as studies that appropriately survey sex/gender identity, as that information was not obtained for this trial.
Despite these limitations, this study was informed by a theoretical framework about how and why mindfulness training helps people reduce smoking (Brewer et al. 2013). Furthermore, this study tested a priori hypotheses stated in the parent trial protocol paper (Garrison et al. 2015) and outcome paper (Garrison et al. 2018), in which mindfulness training might work in part by lessening the association between craving and smoking. Overall, our study provides novel preliminary evidence that self-reported baseline craving strength was associated with changes in self-reported smoking among those receiving mindfulness training. Future studies, included several suggested above, are warranted for a more complete understanding of craving strength and frequency as mechanisms and moderators of mindfulness-based programs for smoking cessation.
References
Aiken, L. S., & West, S. G. (1991). Multiple regression: testing and interpreting interactions. Thousand Oaks: Sage Publications, Inc.
Biener, L., & Abrams, D. (1991). The contemplation ladder: validation of a measure of readiness to consider smoking session. Health Psychology, 10, 360–365.
Bowen, S., & Marlatt, A. (2009). Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behaviors, 23(4), 666. https://doi.org/10.1037/a0017127.
Bowen, S., Chawla, N., & Marlatt, G. A. (2010). Mindfulness-based relapse prevention for the treatment of substance use disorders: a clinician’s guide. New York: Guilford Press.
Brewer, J. A., Mallik, S., Babuscio, T. A., Nich, C., Johnson, H. E., Deleone, C. M., Minnix-Cotton, C. A., Byrne, S. A., Kober, H., & Weinstein, A. J. (2011). Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug and Alcohol Dependence, 119(1–2), 72–80. https://doi.org/10.1016/j.drugalcdep.2011.05.027.
Brewer, J. A., Elwafi, H. M., & Davis, J. H. (2013). Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychology of Addictive Behaviors, 27(2), 366–379. https://doi.org/10.1037/a0028490.
Elwafi, H. M., Witkiewitz, K., Mallik, S., Thornhill, T. A., 4th, & Brewer, J. A. (2013). Mindfulness training for smoking cessation: moderation of the relationship between craving and cigarette use. Drug and Alcohol Dependence, 130(1–3), 222–229. https://doi.org/10.1016/j.drugalcdep.2012.11.015.
Enkema, M. C., & Bowen, S. (2017). Mindfulness practice moderates the relationship between craving and substance use in a clinical sample. Drug and Alcohol Dependence, 179, 1–7. https://doi.org/10.1016/j.drugalcdep.2017.05.036.
Garrison, K. A., Pal, P., Rojiani, R., Dallery, J., O’Malley, S. S., & Brewer, J. A. (2015). A randomized controlled trial of smartphone-based mindfulness training for smoking cessation: a study protocol. BMC Psychiatry, 15(1), 83. https://doi.org/10.1186/s12888-015-0468-z.
Garrison, K. A., Pal, P., O’Malley, S. S., Pittman, B. P., Gueorguieva, R., Rojiani, R., Scheinost, D., Dallery, J., & Brewer, J. A. (2018). Craving to quit: a randomized controlled trial of smartphone app-based mindfulness training for smoking cessation. Nicotine & Tobacco Research. https://doi.org/10.1093/ntr/nty126.
Gass, J. C., Motschman, C. A., & Tiffany, S. T. (2014). The relationship between craving and tobacco use behavior in laboratory studies: a meta-analysis. Psychology of Addictive Behaviors, 28(4), 1162. https://doi.org/10.1037/a0036879.
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2017). Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. https://doi.org/10.1016/j.cpr.2017.10.011.
Jamal, A., Phillips, E., Gentzke, A. S., Homa, D. M., Babb, S. D., King, B. A., & Neff, L. J. (2018). Current cigarette smoking among adults — United States, 2016. MMWR. Morbidity and Mortality Weekly Report, 67, 53–59. https://doi.org/10.15585/mmwr.mm6702a1.
Kabat-Zinn, J. (2005). Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York: Delta Trade Paperback/Bantam Dell.
Karyadi, K. A., VanderVeen, J. D., & Cyders, M. A. (2014). A meta-analysis of the relationship between trait mindfulness and substance use behaviors. Drug and Alcohol Dependence, 143, 1–10. https://doi.org/10.1016/j.drugalcdep.2014.07.014.
Levin, M. E., Luoma, J. B., & Haeger, J. A. (2015). Decoupling as a mechanism of change in mindfulness and acceptance: a literature review. Behavior Modification, 39(6), 870–911. https://doi.org/10.1177/0145445515603707.
Li, W., Howard, M. O., Garland, E. L., McGovern, P., & Lazar, M. (2017). Mindfulness treatment for substance misuse: a systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96. https://doi.org/10.1016/j.jsat.2017.01.008.
Maglione, M. A., Maher, A. R., Ewing, B., Colaiaco, B., Newberry, S., Kandrack, R., Shanman, R. M., Sorbero, M. E., & Hempel, S. (2017). Efficacy of mindfulness meditation for smoking cessation: a systematic review and meta-analysis. Addictive Behaviors, 69, 27–34. https://doi.org/10.1016/j.addbeh.2017.01.022.
May, J., Andrade, J., Kavanagh, D. J., Feeney, G. F., Gullo, M. J., Statham, D. J., Skorka-Brown, J., Connolly, J. M., Cassimatis, M., Young, R. M., & Connor, J. P. (2014). The Craving Experience Questionnaire: a brief, theory-based measure of consummatory desire and craving. Addiction, 109(5), 728–735. https://doi.org/10.1111/add.12472.
Oikonomou, M. T., Arvanitis, M., & Sokolove, R. L. (2017). Mindfulness training for smoking cessation: a meta-analysis of randomized-controlled trials. Journal of Health Psychology, 22(14), 1841–1850. https://doi.org/10.1177/1359105316637667.
Reitsma, M. B., Fullman, N., Ng, M., Salama, J. S., Abajobir, A., Abate, K. H., Abbafati, C., Abera, S. F., Abraham, B., & Abyu, G. Y. (2017). Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the global burden of disease study 2015. The Lancet, 389(10082), 1885–1906. https://doi.org/10.1016/S0140-6736(17)30819-X.
Rollnick, S., Heather, N., Gold, R., & Hall, W. (1992). Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. British Journal of Addiction, 87, 743–754.
Witkiewitz, K., Bowen, S., Harrop, E. N., Douglas, H., Enkema, M., & Sedgwick, C. (2014a). Mindfulness-based treatment to prevent addictive behavior relapse: theoretical models and hypothesized mechanisms of change. Substance Use and Misuse, 49(5), 513–524. https://doi.org/10.3109/10826084.2014.891845.
Witkiewitz, K., Falk, D. E., Kranzler, H. R., Litten, R. Z., Hallgren, K. A., O’Malley, S. S., & Anton, R. F. (2014b). Methods to analyze treatment effects in the presence of missing data for a continuous heavy drinking outcome measure when participants drop out from treatment in alcohol clinical trials. Alcoholism, Clinical and Experimental Research, 38(11), 2826–2834. https://doi.org/10.1111/acer.12543.
Acknowledgments
The authors wish to thank Prasanta Pal and Rahil Rojiani for their contributions to app development. We thank Jesse Dallery, Brian P. Pittman, Ralitza Gueorguieva, and Dustin Scheinost for their contributions to the parent clinical trial. We thank all participants who contributed to this work.
Funding
This study was funded by the American Heart Association (grant number 14CRP18200010) and the National Institute on Drug Abuse (grant number K12DA00167).
Author information
Authors and Affiliations
Contributions
CRR designed and conducted the data analyses and wrote the paper. KAG designed and led the parent clinical trial; contributed to the conceptualization of the paper, data analysis, and interpretation; and helped to write and edit the final manuscript. SSO and JAB collaborated on the parent clinical trial and helped to write and edit final manuscript. JAB additionally developed the mindfulness app used in this study.
Corresponding author
Ethics declarations
The study was approved by the Yale University Institutional Review Board. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All participants enrolled in the study gave their informed consent prior to their inclusion in the study.
Disclaimer
The views presented in the manuscript are not necessarily those of the funding agencies who did not have input into the content of the manuscript outside of funding the proposed research.
Conflict of Interest
Dr. Brewer owns stock in MindSciences, the company that developed the mindfulness app used in this study. This financial interest has been disclosed to and is being managed by Brown University, in accordance with its Conflict of Interest and Conflict of Commitment policies. All other authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roos, C.R., Brewer, J.A., O’Malley, S.S. et al. Baseline Craving Strength as a Prognostic Marker of Benefit from Smartphone App-Based Mindfulness Training for Smoking Cessation. Mindfulness 10, 2165–2171 (2019). https://doi.org/10.1007/s12671-019-01188-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-019-01188-6