Abstract
Objectives
Deep breathing (DB) is known to elicit positive changes to the heart rate variability (HRV) measurement and improve the quality of well-being. However, literature reporting on the effects of the mindful DB duration is scant. This study investigated the HRV indices and its correlation with the mental health scores of three different mindful DB durations.
Methods
Fifty participants were recruited and assigned to the control (Con, n = 13), mindful DB for 5 min (DB5, n = 14), 7 min (DB7, n = 11), or 9 min (DB9, n = 12) group. The HRV was measured during the baseline, mindful DB intervention, post-intervention, and a follow-up session after 7 days of practicing the DB daily. The mental health state was screened during the baseline and follow-up session.
Results
During the intervention, all three DB groups had a significantly larger standard deviation of the normal-to-normal interval and normalized low frequency power whereas the normalized high frequency power (nHF) was significantly smaller than the control group. The depression score for the DB7 and DB9 participants was significantly smaller than the control group (p = 0.024 and p = 0.021, respectively). A significant negative correlation was obtained for the depression score and nHF of the DB9 group (r = − 0.673, p = 0.016).
Conclusions
The mindful DB duration plays a role in the shifting of the autonomic nervous system such that only the reduction in depression for the DB9 group was associated with the greater activation of the parasympathetic nervous system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The variation in the time interval between heartbeats is known as the heart rate variability (HRV) and it is modulated by the autonomic nervous system (ANS) which consists of the sympathetic and parasympathetic branches (McCorry 2007). In normal conditions, the two branches are balanced but a greater activation of the sympathetic side can occur under certain pathological conditions such as myocardial infarction (Buccelletti et al. 2009; Carney et al. 2001; Katz et al. 1999), congested heart failure (Isler and Kuntalp 2007; Patel et al. 2017; Ponikowski et al. 1997), and diabetic neuropathy (Chessa et al. 2002; Sridhar et al. 2010). This sympathovagal imbalance can be inferred from the time domain HRV parameters such as the standard deviation of the normal-to-normal (NN) intervals (SDNN) and the square root of the mean of the squares of the successive differences between adjacent NN intervals (RMSSD) (Stein et al. 1994). Aside from the time domain, the parameters in the frequency domain also provide information on the autonomic system, especially in the low-frequency (0.04–0.15 Hz; LF) and high-frequency range (0.15–0.40 Hz; HF) (Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology 1996). The LF power is reflecting on the baroceptor-mediated sympathetic and parasympathetic nervous systems whereas the HF power is related to the parasympathetic nervous system. The ratio of the LF power to the HF power (LF/HF) has been proposed to reflect the sympathovagal balance, but recent research into this variable had failed to provide any evidence for this claim (Billman 2011; Milicevic 2005).
Apart from pathological reasons, the changes in the HRV can also be brought voluntarily through alteration in the respiration rate and rhythm. Respiration and the heart rate are connected via the respiration sinus arrhythmia (RSA) such that the heart rate increases during inhalation and the heart rate decreases during exhalation (Billman 2011). Song and Lehrer (2003) had investigated the effects of breathing for 5 min at specific respiratory rates of 3, 4, 6, 8, 10, 12, and 14 breaths per minute on the HRV indices. Their outcome reported non-significant changes in the mean heart rate between each respiratory rate but a significant difference was observed for the LF and HF power. The general trend was when the respiratory rate was lower, the LF power was greater and the inverse relationship was seen in the HF power. A similar study by Guzik et al. (2007) who had set a total 5 min breathing time for different cycles of breath per minute indicated that at the respiratory rate of 6 breaths per minute, the SDNN, LF, and HF power were significantly different from 9, 12, and 15 breaths per minute. Additionally, the RMSSD indicated no difference between each respiratory rate. On the other hand, the carry-over effects of mindful deep breathing on the HRV measurement have been studied as well by Prinsloo et al. (2013a) who used a HRV biofeedback-induced deep breathing intervention. They had evaluated the changes in the HRV indices during the baseline, intervention, and a post-intervention period and reported that during the intervention (lasting for 10 min), both the SDNN, total power, and LF power of the intervention group were significantly larger than that of the control group whereas during the post-intervention period, the inter-group differences disappeared. Another report by Tharion et al. (2012) had investigated the changes in the HRV measurement after 1 month of practicing deep breathing at 6 breaths per minute, once every day for 30 min. As compared to the control group with no exercise on video-aided mindful deep breathing, there was a significant increase in the HF and total power, but a decrease was observed for the mean arterial pressure and the respiration rate in the intervention group after 1 month of practicing. Overall, the effect of the breathing frequency on the HRV indices, mainly the SDNN, LF, and HF power, has been extensively investigated in prior literature. However, one long-standing question that has yet to be answered is how the deep breathing durations affect HRV indices. From the above-cited studies, it can be seen that there is no consensus on the breathing duration, which can range from 5 to 30 min.
Besides the issue of the deep breathing duration, the use of deep breathing as an intervention to improve one’s mental state is still an active research area. It is believed that deep breathing, HRV, and the mental health are inherently linked together such that mindful deep breathing has the potential to enhance the parasympathetic activity that may lead to the correction of sympathovagal imbalance seen in psychological diseases (Agelink et al. 2002; Veith et al. 1994; Whooley and Wong 2013), and hence achieving a better mental health state (Brown and Gerbarg 2005). The efficacy of mindful deep breathing for improving the mental health in patients with depression, anxiety, and stress for patients with coronary heart disease (Chung et al. 2010), post-traumatic stress disorder (Kim et al. 2013), cancer (Hayama and Inoue 2012; Jacobsen et al. 2002; Kim et al. 2005), burn care (Park et al. 2013), and pregnancy (Yu and Song 2010) has been demonstrated previously. These results show that mindful deep breathing may provide an alternative to psychotropic medications (van Schaik et al. 2004). However, the results have been mixed in people with good health. Busch et al. (2012) reported there was a reduction in anxiety and depression after performing repeated blocks of 5-min duration mindful deep breathing at a rate of 7 breaths per minute whereas Lin et al. (2014) had reported that there was no effect on the anxiety level when mindful deep breath at 6 or 5.5 breaths per minute for 12 min with a 5:5 or 4:6 inhalation-to-exhalation ratio. Notably, the deep breathing duration is not consistent across different studies and this may have impacted the results.
In this pilot study, the effects of the mindful deep breathing duration of 5, 7, and 9 min on the HRV indices and its correlation to mental health state were investigated in a nonclinical, young adult population. It was hypothesized that longer mindful deep breathing durations would produce greater change in the HRV indices during the intervention, post-intervention, and follow-up session as compared to the control group. For the mental health in terms of depression, anxiety, and stress, it was hypothesized that the scoring of the mindful deep breathing (DB) groups would be smaller than that of the control group. Lastly, a negative correlation between the mental health score and the nHF was expected in the DB groups.
Method
Participants
The required sample size of 52 was determined based on the rule of thumb proposed by Julious (2005) such that for a pilot study, the recommended sample size per group should be 12, as well as considering a dropout rate of 10% (1.1 × 12 × 4 ≈ 52). The inclusion criteria of this study were (i) being students enrolled in the university (regardless of the education level), (ii) age ranging from 18 to 30, and (iii) have no prior knowledge about the deep breathing exercise. As for the exclusion criteria, there was three: (i) those who were sick for the past 2 weeks before the experiment, (ii) those who were having any medical prescriptions, and (iii) those who could not perform deep breathing for 5 min or more. A total of 56 eligible young adults (23% female) with an age range from 20 to 27 were recruited from the university through the distribution of flyers and also through word of mouth advertising. All the recruited participants had a normal or corrected-to-normal vision and no respiratory or psychiatric diseases as confirmed by a self-reported questionnaire. There were five participants who did not come for the follow-up session, and hence were removed from the final analysis. One more participant was excluded from the final analysis due to equipment malfunction during the follow-up session. Consequently, a total of 50 participants were able to complete the protocol and the demographic information along with the baseline HRV variables and mental health scores are shown in Table 1. Among the 50 participants, 49 (98%) were enrolled in a bachelor degree program whereas only 1 (2%) was enrolled in a foundation program. In terms of the ethnic composition, 1 (2%) was Aryan, 1 (2%) was Sino-Kadazan, 2 (4%) were Malaysian Indian, and 46 (92%) were Malaysian Chinese. There were no differences in terms of the demographic information, baseline HRV indices, and baseline mental health scores among the four groups.
Procedure
The research procedures were approved by the local university scientific and ethical review committee (Reference no.: U/SERC/04/2017), and therefore been performed in accordance with the Declaration of Helsinki. All the participants understood the procedures and informed consent was obtained all individual participants included in the study prior to the experiment.
The experimental procedure is summarized in Fig. 1b. Based on the participants’ chosen time slot for the experiment, they were randomized to one of the four groups: Control group (Con), mindful deep breathing for 5 min (DB5), mindful deep breathing for 7 min (DB7), and mindful deep breathing for 9 min (DB9). Among the final 50 participants who managed to complete the protocol, there were 13, 11, 14, and 12 participants in the Con, DB5, DB7, and DB9 groups, respectively.
a Screenshots from the mindful deep breathing guiding video and the b flowchart of the participants and experimental procedure which consisted of 7 main parts: baseline (R1), first Go/NoGo task (T1), intervention (INT), post-intervention (R2), second Go/NoGo task (T2), follow-up baseline (R3), and third Go/NoGo task (T3)
The experiment was carried out in a laboratory room with sufficient lighting provided by two fluorescent lamps. On arrival to the experiment room, the participants first rested for 15 min sitting upright on a chair to ensure the physiological state returned to a stable condition. During the same time, the HRV recording equipment was applied to the participants for data acquisition. After 15 min was up, a baseline reading of 5 min (R1) was taken followed by the administration of a Go/NoGo task (T1) that lasts about 10 min. Next, the participants underwent the intervention (INT). For the participants in the three DB groups, they were required to follow the video and perform the mindful deep breathing for their assigned breathing duration of either 5, 7, or 9 min. As for the control group, the participants were requested to stay at rest for 9 min without being shown the mindful deep breathing video or any other instructions. After the intervention period, all the participants rested for 5 min (R2) and was later carried on with the next Go/NoGo task (T2). The HRV measurement was recorded at R1, INT, and R2.
The follow-up session was 1 week after the first session at the same timeslot for each participant. The mindful deep breathing video guide was sent to each participant in the DB groups and they were instructed to perform the exercise once per day at any time for the 7 days period (the first day was the first session). Messages were sent to remind the participants and a confirmation was sent to the researcher every time after the mindful deep breathing was done. As for the control group, no such instructions were given and they did not know about the mindful deep breathing video. During the follow-up session, all the participants rested for 15 min again while the HRV recording equipment was being applied. Next, a follow-up baseline reading of 5 min (R3) was obtained followed by a third Go/NoGo task (T3). Again, the HRV was only obtained during R3 but not T3.
The three Go/NoGo tasks (T1, T2, and T3) were employed to investigate how mindful deep breathing of various durations might modulate cognitive control. The corresponding results have been published elsewhere (Cheng et al. 2017), and thus, only the HRV variables and mental health scores are the main focus of this study.
Video-Aided Mindful Deep Breathing Intervention
The mindful deep breathing intervention in this study was guided by a video as shown in Fig. 1a The mindful deep breathing technique employed here was a short-duration, video-aided mindful deep breathing that has been previously shown to induce an increment conflict monitoring ability (Cheng et al. 2017). The respiratory rate was set to 6 breaths per minute with 5 s of inhalation and 5 s of exhalation. This particular rate was chosen because it would create a resonance effect between the respiration and the heartbeat and produce the greatest change in HRV (Vaschillo et al. 2006). In the video, there was a smiley face in the middle and petals were appearing and disappearing around it. The appearing of the petals signaled the inhalation process whereas the disappearing of the petals signaled the exhalation process. This video guide was created to standardize the breathing rate of the participants. The participants were instructed to keep their attention on following tightly to the video guided mindful deep breathing video guide, as well as to feel the air flowing in and out from their body throughout the 5, 7, or 9 min of mindful deep breathing duration. Any longer duration was not considered to avoid the risk of hyperventilation (Prinsloo et al. 2013b). The links to the three videos are provided in the Supplementary Materials.
HRV Data Acquisition and Analysis
A photoplethysmograph (PPG) was obtained using a KYTO Mobile Heart Rate Monitor (Model no: HRM-2935; http://kytofitness.com) which transmitted the raw interbeat interval data to a smartphone app named Elite HRV (https://www.elitehrv.com). Prior to the actual recording, the PPG signal was visually examined for several minutes to ensure a stable signal was obtained. The data recording lasted for 5 min for each mindful deep breathing duration during INT. For the DB5 group, the reading was taken from the 0th minute to the 5th minute; DB7 group was from 2nd minute to the 7th minute; DB9 group was from 4th minute to the 9th minute. These recording periods provided the recommended 5 min reading for HRV as proposed by the Task Force of the European Society of Cardiology and The North American Society of Pacing and Electrophysiology (1996). Throughout the three recording periods (INT, R2, and R3), the participants were instructed to sit still and abstain from any physical movement including eye blinks in order to reduce the motion and EMG-related noise. In the Elite HRV app, the raw R-R interval data was exported and analyzed using HRVAS (Ramshur 2010), which is an open source software designed to perform HRV analysis by using MATLAB.
First, the raw R-R interval data were visually inspected for significant missing data and were discarded from the final analysis if there was a significant missing of data. Next, the raw R-R interval data was checked for ectopic beats. Two filters were used to detect the ectopic beats: when an interval was 20% more than the previous interval and also intervals that lay beyond 3 standard deviations from the mean interbeat interval. Following that, a wavelet detrending method was used to detrend the data. In the time domain analysis, the mean heart rate (HR), SDNN, and RMSSD were obtained whereas in the frequency domain, the normalized power in the LF (nLF; 0.04–0.15 Hz) and HF (nHF; 0.15–0.4 Hz) bands was obtained. A Lomb-Scargle Periodogram that uses the least squares fit of sinusoids to the data was used as this method do not need the waveform to be stationary (Van Dongen et al. 1999).
Measures
21-Item Depression, Anxiety, and Stress Scale
In order to do a brief screening on the mental health state of the participants, the 21-item Depression, Anxiety and Stress Scale (DASS-21) questionnaire was used. The DASS-21, which is the short form of the DASS that has 42 items, was used to measure the range of severity for depression, anxiety, and stress. It comprised of a 4-point Likert scale like items which range from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time), where the participants were required to indicate the presence of the description over the past week. To calculate the total score for each category (depression, anxiety, and stress), the score for each item in the same category was summed together and then multiplied by two. The DASS-21 has been found to be reliable when using on nonclinical samples given that the Cronbach alphas of the depression, anxiety, and stress scale were 0.88, 0.82, and 0.90, respectively (Henry and Crawford 2005).
Data Analyses
The statistical analysis was performed using SPSS version 24.0 (SPSS, Inc.) and G*Power version 3.1.9.2 (Faul et al. 2007). For the demographic information, as well as the baseline HRV variables (mean HR, SDNN, RMSSD, nLF, and nHF) and mental health score from DASS-21 of each category (depression, anxiety, and stress), one-way ANOVA was used to analyze the difference between the four groups (Con, DB5, DB7, and DB9) in order to assess the randomization procedure. For the mental health score at R3, a univariate ANCOVA with the respective baseline reading at R1 as the covariate was used to analyze the differences between the group (Con, DB5, DB7, and DB9). For the HRV measurements, they were analyzed using a 4 × 3 repeated measure ANCOVA with the group (Con, DB5, DB7, and DB9) as the between-subject factor, time (INT, R2, and R3) as the within-subject factor, and the baseline reading at R1 as the covariate. Whenever the sphericity condition was violated, the Greenhouse-Geisser (when ε < 0.75) or Huynh-Feldt (when ε > 0.75) correction was applied depending on the epsilon. A planned contrast was carried for any significant group difference such that the Con group was compared to each of the DB groups with Bonferroni correction (corrected p = 0.0167) but no comparisons were done among the DB groups as these do not address the hypotheses. For the time variable, a pairwise comparison with Bonferroni correction (corrected p = 0.0167) was used to find the specific change. Further, the Pearson correlation between the percentage change (between R3 and R1) of the depression, anxiety, and stress score and the nHF was obtained for each group. The Cohen’s d effect sizes of the HRV variables and mental health scores within and between the four groups for all three time points were calculated (Becker 1988; Farnia et al. 2018). The interpretation of the effect size by Cohen (1992) was adopted. This study focused on the five HRV indices during the follow-up session (R3) as the co-primary dependent variables (Offen et al. 2007) whereas the HRV indices of other time points and the mental health scores were the secondary dependent variables. A two-sided p value of < 0.05 was considered as statistically significant. Values are reported in mean and standard error in parenthesis.
Result
Heart Rate Variability
The adjusted mean and the standard error for each parameter is shown in Table 3. For the mean heart rate, there was a significant time main effect (Table 2), indicating the mean heart rate during the intervention (INT) was larger than the period of rest immediately after the deep breathing (R2) (p < 0.001, d = 0.88). For the SDNN, there was a significant time main effect and a significant time × group interaction. Post-hoc analysis with Bonferroni correction revealed that during the intervention (INT), the SDNN of the Con group was smaller than that of the DB5, DB7, and DB9 groups (p = 0.012, d = 1.25, p = 0.033, d = 1.01 and p = 0.033, d = 1.06, respectively). Furthermore, the SDNN value during the intervention (INT) was larger than both the rest period immediately after the intervention and also during the follow-up session (R2 and R3) for the DB5 group (p < 0.001, d = 0.65 and p = 0.001, d = 0.57, respectively). The same result was observed in both DB7 and DB9 groups as well (DB7: p < 0.001, d = 0.64 and p = 0.004, 0.48; DB9: p = 0.002, d = 0.51 and p = 0.016, d = 0.59), as shown in Fig. 2a. For the RMSSD, there was only a significant time main effect, indicating the RMSSD was larger during the intervention (INT) than the resting period immediately post deep breathing (R2) (p = 0.003, d = 0.50). These results are summarized in Fig. 2a, b, Tables 2, 3, and 4.
The adjusted mean of a SDNN, b RMSSD, c nLF, and d nHF for each group (Con, DB5, DB7, and DB9) during each time (INT, R2, and R3). Error bars represent the standard error. #, p < 0.05 as compared to the Con group; ###, p < 0.001 as compared to the Con group; *, p < 0.05; **, p < 0.01; ***, p < 0.001
For the nLF, there was a significant time main effect, a significant group main effect, and a significant time × group interaction (Table 2). Post-hoc analysis with Bonferroni correction showed that during the intervention (INT), the nLF of the Con group was smaller than that of DB5, DB7, and DB9 (p < 0.001, d = 2.31, p < 0.001, d = 2.39 and p < 0.001, d = 1.87, respectively). Within the DB5 group, the magnitude of the nLF during the intervention (INT) was larger than both the resting periods (R2 and R3) (p < 0.001, d = 0.64 and p < 0.001, d = 0.94, respectively). Further, the nHF during the resting period immediately after the deep breathing (R2) was larger than that of the follow-up session (R3) (p = 0.007, d = 0.46). For DB7 and DB9, the nLF during the deep breathing (INT) was larger than both the resting periods (R2 and R3) (DB7: p < 0.001, d = 0.81 and p < 0.001, d = 0.98, respectively; DB9: p < 0.001, d = 0.72 and p < 0.001, d = 0.87, respectively). Focusing on the nHF, there was a significant time main effect, a significant group main effect, and a significant time × group interaction (Table 2). Post-hoc analysis revealed that during the intervention (INT), the nHF of the Con group was larger than all three DB groups (DB5: p < 0.001, d = 2.31; DB7: p < 0.001, d = 2.39; DB9: p < 0.001, d = 1.87, respectively). Within the DB5 group alone, the magnitude of the nHF during deep breathing (INT) was smaller than both resting periods of R2 and R3 (p < 0.001, d = 0.64 and p < 0.001, d = 0.94, respectively). During the post-intervention resting period R2, the nHF was smaller than that of the follow-up resting period R3 (p = 0.007, d = 0.46). For the DB7 and DB9 groups, the nHF during the intervention (INT) was smaller than both the resting periods R2 and R3 (DB7: p < 0.001, d = 0.81 and p < 0.001, d = 0.98, respectively; DB9: p < 0.001, d = 0.72 and p < 0.001, d = 0.87, respectively). These results are summarized in Fig. 2c, d, Tables 2, 3, and 4.
When the participants in the three deep breathing groups were pooled into one single deep breathing group (DB), the results obtained for the HRV indices were similar as above (Table S1, Table S2, and Table S3). This indicates that the mindful deep breathing had a similar effect on the HRV indices regardless of the deep breathing duration.
Mental Health
For the mental state obtained from the DASS-21, there was only a significant group main effect observed for the depression category. Post-hoc analysis revealed that the depression score for the Con group (13.268 (1.037)) was larger than that of DB7 (9.240 (1.010)) and DB9 (9.059 (0.021)) during R3 (p = 0.024, d = 0.94 and p = 0.021, d = 0.99, respectively) as shown in Fig. 3a, Tables 2 and 4. There was no effect on the anxiety or stress category. Similarly, when analyzing the deep breathing participants as a whole, there was no effect on the anxiety and stress category as well. On the other hand, there was a significant reduction in the depression score for the DB group as compared to the Con group (Table S1 and Table S3).
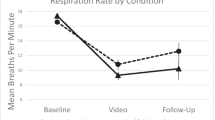
a The adjusted mean score for depression, anxiety, and stress during R3 obtained from DASS-21 for each group. b A significant negative correlation between the percentage change of the depression score and the percentage change of the nHF was obtained for the DB9 group. The error bars represent the standard errors. *, p < 0.05
Correlation Between HRV and Mental Health
There was only one significant correlation between the percentage change of the DASS scores and the nHF of each group. For the DB9 group, there was a significant negative correlation between the depression score and the nHF (r = − 0.673, p = 0.016) as shown in Fig. 3b. Since a majority of the percentage change in depression score was in the negative range, this negative correlation could be seen as an increased in the nHF had led to a decrease in the depression score. Interestingly, when pooled into the DB group, no significant correlation was found between the nHF and the depression score for the DB group. This indicates that the mindful deep breathing duration is an important factor to consider as more information can be revealed by analyzing the individual breathing durations.
Discussion
This pilot study had investigated the effects of different mindful deep breathing durations on the HRV indices in both the time domain (mean heart rate, SDNN, and RMSSD) and the frequency domain (nLF and nHF) along with the mental health in terms of depression, anxiety, and stress. During the mindful deep breathing at 6 breaths per minute (INT), a significant increase in the SDNN and nLF was observed for all three breathing durations of 5, 7, and 9 min when compared to the control group, with a large effect size for all three groups. The magnitude of the nHF for all three DB groups was significantly smaller than that of the control group during the intervention as well. There was no difference between the control and DB groups during the post-intervention period as well as the follow-up session after 7 days. Besides that, the self-reported depression score from the DASS-21 questionnaire was found to be significantly smaller in two of the three DB groups (DB7 and DB9) as compared to the control group, again achieving a large effect size of greater than 0.90. The rationale of choosing a 1-week period of daily practicing was such that it would be long enough to have an effect on the HRV measurements and mental health scores, yet brief enough to maximize protocol adherence for participants with busy lifestyles. We note that the study had a high adherence rate (91%).
Deep breathing is a fundamental exercise in most mindfulness practices (Brown and Gerbarg 2009), although the form of the deep breathing exercise may differ in terms of the breathing frequency and duration. Following the operational definition of mindfulness by (Bishop et al. 2004), mindfulness comprises of two facets that include the self-regulation of attention and orientation of one’s experience in the present moment. In this study, we had instructed the participants to keep their attention on following tightly to the video as well as to feel the air flowing in and out from their body and these two actions falls within the two facets of mindfulness. The participants would need to regulate their attention and placed it onto the video in order to follow the pre-set breathing frequency of 6 breaths per minute for either 5, 7, or 9 min, along with the need to bring their consciousness or experience to the present moment of deep breathing. Not only that these instructions are similar to the instruction given by coaches of various mindfulness practices (Cheng et al. 2017), the chosen deep breathing durations of 5, 7, and 9 min are also in line with the required daily practice time of 5 to 15 min of many mindfulness practices (Baer 2015; Bower et al. 2015). Further, the use of visual cues for attention regulation has the potential to reduce mind wandering as well as to help those who are unable to focus while deep breathing with their eyes closed. Taken together, the mindful deep breathing exercise in this study differs from conventional deep breathing that does not require one to modulate his or her attention and experience.
Breathing at 6 breaths per minute for either 5, 7, or 9 min had resulted in a higher HRV measurement compared to the control group during the mindful deep breathing intervention. In terms of the time domain variables, the increase in the SDNN but not the mean HR and RMSSD is consistent with previous reported literature (Kim et al. 2016; Lin et al. 2014; Prinsloo et al. 2013a; Wang et al. 2010). From Fig. 2b, it can be seen that the RMSSD value for the DB groups was larger than that of Con although they were not statistically different. These results provide evidence that mindful deep breathing at a rate of 6 breaths per minute caused an incline of the ANS towards the parasympathetic side, consistent with the relaxation feeling obtained during mindful deep breathing (Kjellgren et al. 2007; Lin et al. 2014; Prinsloo et al. 2011). Further, it was also shown that the mindful deep breathing technique employed here modulated the ANS with a considerable effect with the effect sizes being in the range of medium to large.
Regarding the frequency domain, the huge difference observed in the nLF and the nHF between the DB groups and the Con group was due to the breathing frequency of 0.1 Hz (6 breaths per minute), indicating that the participants had followed the breathing video guide. The power spectrum density of the HRV is modulated by the breathing frequency such that the peaks will shift towards and centered around the breathing frequency (Sanderson et al. 1996). In this study, the breathing frequency of 0.1 Hz led to a huge peak at around 0.1 Hz, which lies in the LF range (0.04 to 0.15 Hz) and caused a mixture of the LF and HF power. Even though the nLF and nHF are associated with the sympathetic and parasympathetic activation, respectively, this explanation could not be applied here as the LF and HF components are indissociable (Malliani 2005). However, this problem was solved by Aysin and Aysin (2006) who had utilized an enhanced HRV (eHRV) analysis that takes into account the breathing frequency for the frequency domain analysis. Using this enhanced method, they had successfully isolated the LF and HF regions when the participants were breathing at 6 breaths per minute and had found that the HF power was larger than the LF power. Although not reproduced here, their results provided further evidence that the three different mindful deep breathing durations employed here did induce a greater activation of the parasympathetic nervous system.
Regarding the mindful deep breathing duration, from the results here, it suggested that mindful deep breathing for 5 min was the optimum duration as it produced the largest change in HRV as compared to the control group and this is contrary to the hypothesis. During the post-intervention period and also the follow-up session, there was no significant difference between the DB groups and the Con group, which was in agreement with several studies that reported a similar result (Prinsloo et al. 2013a; Tharion et al. 2012). Overall, mindful deep breathing for either 5, 7, or 9 min had produced similar result of a greater activation of the parasympathetic nervous system as compared to the control group. Among the three respiration rates, 5 breaths per minutes seems to be best given that it produced the greatest change in the HRV indices.
Viewing from the mental health state, the result obtained in this study has shown that by mindful deep breathing for at least 7 min per day for 7 days, the depression score was smaller when compared to the control group (Fig. 3). This is in line with various literature exploring the usage of mindful deep breathing as an alternative method to reduce depression in patients with coronary heart disease (Chung et al. 2010; Gellis and Kang-Yi 2012), patients on haemodialysis (Tsai et al. 2015), and even for normal healthy people (Brown and Gerbarg 2005; Busch et al. 2012). The study conducted by Busch et al. (2012) had investigated the effect of two different types of mindful deep breathing, namely the relaxing mindful deep breathing and attentive mindful deep breathing on pain perception, autonomic activity, and mood processing in healthy undergraduate students. They have reported that by undergoing either one of the mindful deep breathing training for 6 weeks, the depression score obtained from the Profile of Mood States (POMS) was significantly reduced as compared to the baseline score. From the current result, it seems that 1 week of training in mindful deep breathing can lead to the same effect. It was also revealed that the notion of “the longer the better” seems to be supported as the 9 min mindful deep breathing had resulted in a greater reduction (larger effect size) in the depression score as compared to the DB7 group.
Besides that, the percentage change of the depression score was found to be having a negative correlation with the percentage change of the nHF in the DB9 group. The increase in the nHF indicates a greater activation of the parasympathetic over the sympathetic nervous system (Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology 1996). Given the negative correlation here, the shifting towards the vagal tone had led to a reduction in the depression score and this is consistent with the studies done by Agelink et al. (2002) and Udupa et al. (2007). One particular interesting point is that the correlation between the depression score and nHF was only significant for the DB9 group and not for DB5 or DB7. It may be possible that the breathing duration plays a role in the shifting of the ANS such that only DB9’s reduction in depression was associated with the parasympathetic activation while the other two groups were not.
Limitations and Future Research
There are few limitations in this study. The first one would be the relatively small sample size in each group and larger sample size would inevitably lead to a more accurate result. Nonetheless, the majority of the effect sizes obtained in this study fell within the medium and large range (i.e., d > 0.50) and this shows the potential of this mindful deep breathing exercise as a behavioral intervention for depression symptoms. One cautionary note is that the effect sizes estimated may be inflated due to the winner’s curse phenomenon (Button et al. 2013). The second limitation is that the results for both males and females were combined and analyzed together. It is known that HRV measurement differs for both of the genders (Umetani et al. 1998) and by separating them, more information can be known about the relationship between the mindful deep breathing duration and the HRV indices. In this study, the number of females in each group was too small to make a statistically valid comparison. Further, one can extend the scope of this study by recruiting both nonclinical and clinical participants in the children, adolescent, and senior population. It seems possible that mindful deep breathing will have different effects on the HRV of different age population given that the HRV decreases with age (Jensen-Urstad et al. 1997; Zhang 2007).
Lastly, it was observed that only the depression score was decreased after the mindful deep breathing but not the anxiety nor stress scores. The reason for this phenomenon is not known, but one possibility is that the observed result was due to the 1-week study period adopted in this study. There is a temporal dependence between depression and anxiety such that the depressive symptoms are able to predict later anxiety symptoms and vice versa (Jacobson and Newman 2017). It may be possible that with a practice duration of longer than 1 week, the anxiety and/or stress score will decrease as well and this will be an interesting future research to elucidate the mechanism for the comorbidity of depression, anxiety, and stress.
References
Agelink, M. W., Boz, C., Ullrich, H., & Andrich, J. (2002). Relationship between major depression and heart rate variability. Clinical consequences and implications for antidepressive treatment. Psychiatry Research, 113(1–2), 139–149.
Aysin, B., & Aysin, E. (2006). Effect of respiration in heart rate variability (HRV) analysis. Conference proceeding: Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 1, 1776–1779. https://doi.org/10.1109/IEMBS.2006.260773.
Baer, R. A. (2015). Mindfulness-based treatment approaches: clinician's guide to evidence base and applications. New York, NY: Elsevier.
Becker, B. J. (1988). Synthesizing standardized mean-change measures. British Journal of Mathematical and Statistical Psychology, 41(2), 257–278.
Billman, G. E. (2011). Heart rate variability—a historical perspective. Frontiers in Physiology, 2, 86. https://doi.org/10.3389/fphys.2011.00086.
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., et al. (2004). Mindfulness: a proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241. https://doi.org/10.1093/clipsy.bph077.
Bower, J. E., Crosswell, A. D., Stanton, A. L., Crespi, C. M., Winston, D., Arevalo, J., et al. (2015). Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer, 121(8), 1231–1240. https://doi.org/10.1002/cncr.29194.
Brown, R. P., & Gerbarg, P. L. (2005). Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression. Part II—clinical applications and guidelines. Journal of Alternative and Complementary Medicine, 11(4), 711–717. https://doi.org/10.1089/acm.2005.11.711.
Brown, R. P., & Gerbarg, P. L. (2009). Yoga breathing, meditation, and longevity. Annals of the New York Academy of Sciences, 1172, 54–62. https://doi.org/10.1111/j.1749-6632.2009.04394.x.
Buccelletti, E., Gilardi, E., Scaini, E., Galiuto, L., Persiani, R., Biondi, A., et al. (2009). Heart rate variability and myocardial infarction: systematic literature review and metanalysis. European Review for Medical and Pharmacological Sciences, 13(4), 299–307.
Busch, V., Magerl, W., Kern, U., Haas, J., Hajak, G., & Eichhammer, P. (2012). The effect of deep and slow breathing on pain perception, autonomic activity, and mood processing—an experimental study. Pain Medicine (Malden, Mass), 13(2), 215–228.
Button, K. S., Ioannidis, J. P., Mokrysz, C., Nosek, B. A., Flint, J., Robinson, E. S., et al. (2013). Power failure: why small sample size undermines the reliability of neuroscience. Nature Review Neuroscience, 14(5), 365–376. https://doi.org/10.1038/nrn3475.
Carney, R. M., Blumenthal, J. A., Stein, P. K., Watkins, L., Catellier, D., Berkman, L. F., et al. (2001). Depression, heart rate variability, and acute myocardial infarction. Circulation, 104(17), 2024–2028.
Cheng, K. S., Chang, Y. F., Han, R. P. S., & Lee, P. F. (2017). Enhanced conflict monitoring via a short-duration, video-assisted deep breathing in healthy young adults: an event-related potential approach through the Go/NoGo paradigm. PeerJ, 5, e3857. https://doi.org/10.7717/peerj.3857.
Chessa, M., Butera, G., Lanza, G. A., Bossone, E., Delogu, A., De Rosa, G., et al. (2002). Role of heart rate variability in the early diagnosis of diabetic autonomic neuropathy in children. Herz, 27(8), 785–790. https://doi.org/10.1007/s00059-002-2340-4.
Chung, L. J., Tsai, P. S., Liu, B. Y., Chou, K. R., Lin, W. H., Shyu, Y. K., et al. (2010). Home-based deep breathing for depression in patients with coronary heart disease: a randomised controlled trial. International Journal of Nursing Studies, 47(11), 1346–1353. https://doi.org/10.1016/j.ijnurstu.2010.03.007.
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159.
Farnia, V., Gharehbaghi, H., Alikhani, M., Almasi, A., Golshani, S., Tatari, F., et al. (2018). Efficacy and tolerability of adjunctive gabapentin and memantine in obsessive compulsive disorder: double-blind, randomized, placebo-controlled trial. Journal of Psychiatric Research, 104, 137–143. https://doi.org/10.1016/j.jpsychires.2018.07.008.
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191.
Gellis, Z. D., & Kang-Yi, C. (2012). Meta-analysis of the effect of cardiac rehabilitation interventions on depression outcomes in adults 64 years of age and older. American Journal of Cardiology, 110(9), 1219–1224. https://doi.org/10.1016/j.amjcard.2012.06.021.
Guzik, P., Piskorski, J., Krauze, T., Schneider, R., Wesseling, K. H., Wykretowicz, A., et al. (2007). Correlations between the Poincare plot and conventional heart rate variability parameters assessed during paced breathing. The Journal of Physiological Sciences, 57(1), 63–71. https://doi.org/10.2170/physiolsci.RP005506.
Hayama, Y., & Inoue, T. (2012). The effects of deep breathing on ‘tension-anxiety’ and fatigue in cancer patients undergoing adjuvant chemotherapy. Complementary Therapies in Clinical Practice, 18(2), 94–98. https://doi.org/10.1016/j.ctcp.2011.10.001.
Henry, J. D., & Crawford, J. R. (2005). The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 44(Pt 2, 227–239. https://doi.org/10.1348/014466505X29657.
Isler, Y., & Kuntalp, M. (2007). Combining classical HRV indices with wavelet entropy measures improves to performance in diagnosing congestive heart failure. Computers in Biology and Medicine, 37(10), 1502–1510. https://doi.org/10.1016/j.compbiomed.2007.01.012.
Jacobsen, P. B., Meade, C. D., Stein, K. D., Chirikos, T. N., Small, B. J., & Ruckdeschel, J. C. (2002). Efficacy and costs of two forms of stress management training for cancer patients undergoing chemotherapy. Journal of Clinical Oncology, 20(12), 2851–2862. https://doi.org/10.1200/JCO.2002.08.301.
Jacobson, N. C., & Newman, M. G. (2017). Anxiety and depression as bidirectional risk factors for one another: a meta-analysis of longitudinal studies. Psychological Bulletin, 143(11), 1155–1200. https://doi.org/10.1037/bul0000111.
Jensen-Urstad, K., Storck, N., Bouvier, F., Ericson, M., Linbland, L. E., & Jensen-Urstad, M. (1997). Heart rate variability in healthy subjects is related to age and gender. Acta Physiologica Scandinavica, 160(3), 235–241. https://doi.org/10.1046/j.1365-201X.1997.00142.x.
Julious, S. A. (2005). Sample size of 12 per group rule of thumb for a pilot study. Pharmaceutical Statistics, 4(4), 287–291. https://doi.org/10.1002/pst.185.
Katz, A., Liberty, I. F., Porath, A., Ovsyshcher, I., & Prystowsky, E. N. (1999). A simple bedside test of 1-minute heart rate variability during deep breathing as a prognostic index after myocardial infarction. American Heart Journal, 138(1 Pt 1), 32–38.
Kim, K. S., Lee, S. W., Choe, M. A., Yi, M. S., Choi, S., & Kwon, S.-H. (2005). Effects of abdominal breathing training using biofeedback on stress, immune response and quality of life in patients with a mastectomy for breast cancer. Taehan Kanho Hakhoe Chi, 35(7), 1295–1303.
Kim, S. H., Schneider, S. M., Bevans, M., Kravitz, L., Mermier, C., Qualls, C., et al. (2013). PTSD symptom reduction with mindfulness-based stretching and deep breathing exercise: randomized controlled clinical trial of efficacy. The Journal of Clinical Endocrinology & Metabolism, 98(7), 2984–2992. https://doi.org/10.1210/jc.2012-3742.
Kim, J.-H., Bae, H.-S., & Park, S.-S. (2016). The effects of breath-counting meditation and deep breathing on heart rate variability. Journal of Korean Medicine, 37(2), 36–44.
Kjellgren, A., Bood, S. A., Axelsson, K., Norlander, T., & Saatcioglu, F. (2007). Wellness through a comprehensive yogic breathing program—a controlled pilot trial. BMC Complementary and Alternnative Medicine, 7, 43. https://doi.org/10.1186/1472-6882-7-43.
Lin, I. M., Tai, L. Y., & Fan, S. Y. (2014). Breathing at a rate of 5.5 breaths per minute with equal inhalation-to-exhalation ratio increases heart rate variability. International Journal of Psychophysiology, 91(3), 206–211.
Malliani, A. (2005). Heart rate variability: from bench to bedside. European Journal of Internal Medicine, 16(1), 12–20. https://doi.org/10.1016/j.ejim.2004.06.016.
McCorry, L. K. (2007). Physiology of the autonomic nervous system. American Journal of Pharmaceutical Education, 71(4), 78.
Milicevic, G. (2005). Low to high frequency ratio of heart rate variability spectra fails to describe sympatho-vagal balance in cardiac patients. Collegium Antropologicum, 29(1), 295–300.
Offen, W., Chuang-Stein, C., Dmitrienko, A., Littman, G., Maca, J., Meyerson, L., et al. (2007). Multiple co-primary endpoints: medical and statistical solutions: a report from the multiple endpoints expert team of the Pharmaceutical Research and Manufacturers of America. Drug Information Journal, 41(1), 31–46. https://doi.org/10.1177/009286150704100105.
Park, E., Oh, H., & Kim, T. (2013). The effects of relaxation breathing on procedural pain and anxiety during burn care. Burns, 39(6), 1101–1106. https://doi.org/10.1016/j.burns.2013.01.006.
Patel, V. N., Pierce, B. R., Bodapati, R. K., Brown, D. L., Ives, D. G., & Stein, P. K. (2017). Association of holter-derived heart rate variability parameters with the development of congestive heart failure in the Cardiovascular Health Study. JACC: Heart Failure, 5(6), 423–431. https://doi.org/10.1016/j.jchf.2016.12.015.
Ponikowski, P., Anker, S. D., Chua, T. P., Szelemej, R., Piepoli, M., Adamopoulos, S., et al. (1997). Depressed heart rate variability as an independent predictor of death in chronic congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. The American Journal of Cardiology, 79(12), 1645–1650.
Prinsloo, G. E., Rauch, H. G. L., Lambert, M. I., Muench, F., Noakes, T. D., & Derman, W. E. (2011). The effect of short duration heart rate variability (HRV) biofeedback on cognitive performance during laboratory induced cognitive stress. Applied Cognitive Psychology, 25(5), 792–801. https://doi.org/10.1002/acp.1750.
Prinsloo, G. E., Derman, W. E., Lambert, M. I., & Laurie Rauch, H. G. (2013a). The effect of a single session of short duration biofeedback-induced deep breathing on measures of heart rate variability during laboratory-induced cognitive stress: a pilot study. Applied Psychophysiology and Biofeedback, 38(2), 81–90.
Prinsloo, G. E., Rauch, H. G. L., Karpul, D., & Derman, W. E. (2013b). The effect of a single session of short duration heart rate variability biofeedback on EEG: a pilot study. Applied Psychophysiology and Biofeedback, 38(1), 45–56.
Ramshur, J. (2010). Design, evaluation, and application of heart rate variability analysis software (HRVAS). Memphis, TN: University of Memphis.
Sanderson, J. E., Yeung, L. Y., Yeung, D. T., Kay, R. L., Tomlinson, B., Critchley, J. A., et al. (1996). Impact of changes in respiratory frequency and posture on power spectral analysis of heart rate and systolic blood pressure variability in normal subjects and patients with heart failure. Clinical Science (London), 91(1), 35–43.
Song, H.-S., & Lehrer, P. M. (2003). The effects of specific respiratory rates on heart rate and heart rate variability. Applied Psychophysiology and Biofeedback, 28(1), 13–23.
Sridhar, B., Haleagrahara, N., Bhat, R., Kulur, A. B., Avabratha, S., & Adhikary, P. (2010). Increase in the heart rate variability with deep breathing in diabetic patients after 12-month exercise training. The Tohoku Journal of Experimental Medicine, 220(2), 107–113. https://doi.org/10.1620/tjem.220.107.
Stein, P. K., Bosner, M. S., Kleiger, R. E., & Conger, B. M. (1994). Heart rate variability: a measure of cardiac autonomic tone. American Heart Journal, 127(5), 1376–1381.
Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology. (1996). Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. European Heart Journal, 17(3), 354–381. https://doi.org/10.1161/01.CIR.93.5.1043.
Tharion, E., Samuel, P., Rajalakshmi, R., Gnanasenthil, G., & Subramanian, R. K. (2012). Influence of deep breathing exercise on spontaneous respiratory rate and heart rate variability: a randomised controlled trial in healthy subjects. Indian Journal of Physiology and Pharmacology, 56(1), 80–87.
Tsai, S. H., Wang, M. Y., Miao, N. F., Chian, P. C., Chen, T. H., & Tsai, P. S. (2015). The efficacy of a nurse-led breathing training program in reducing depressive symptoms in patients on hemodialysis: a randomized controlled trial. American Journal of Nursing, 115(4), 24–32; quiz 33, 42. https://doi.org/10.1097/01.NAJ.0000463023.48226.16.
Udupa, K., Sathyaprabha, T. N., Thirthalli, J., Kishore, K. R., Lavekar, G. S., Raju, T. R., et al. (2007). Alteration of cardiac autonomic functions in patients with major depression: a study using heart rate variability measures. Journal of Affective Disorders, 100(1–3), 137–141. https://doi.org/10.1016/j.jad.2006.10.007.
Umetani, K., Singer, D. H., McCraty, R., & Atkinson, M. (1998). Twenty-four hour time domain heart rate variability and heart rate: relations to age and gender over nine decades. Journal of the American College of Cardiology, 31(3), 593–601. https://doi.org/10.1016/s0735-1097(97)00554-8.
Van Dongen, H. P., Olofsen, E., Van Hartevelt, J. H., & Kruyt, E. W. (1999). Searching for biological rhythms: peak detection in the periodogram of unqueally spaced data. Biological Rhythm Research, 30(2), 149–177.
van Schaik, D. J., Klijn, A. F., van Hout, H. P., van Marwijk, H. W., Beekman, A. T., de Haan, M., et al. (2004). Patients’ preferences in the treatment of depressive disorder in primary care. General Hospital Psychiatry, 26(3), 184–189. https://doi.org/10.1016/j.genhosppsych.2003.12.001.
Vaschillo, E. G., Vaschillo, B., & Lehrer, P. M. (2006). Characteristics of resonance in heart rate variability stimulated by biofeedback. Applied Psychophysiology and Biofeedback, 31(2), 129–142. https://doi.org/10.1007/s10484-006-9009-3.
Veith, R. C., Lewis, N., Linares, O. A., Barnes, R. F., Raskind, M. A., Villacres, E. C., et al. (1994). Sympathetic nervous system activity in major depression. Basal and desipramine-induced alterations in plasma norepinephrine kinetics. Archives of General Psychiatry, 51(5), 411–422.
Wang, S. Z., Li, S., Xu, X. Y., Lin, G. P., Shao, L., Zhao, Y., et al. (2010). Effect of slow abdominal breathing combined with biofeedback on blood pressure and heart rate variability in prehypertension. Journal of Alternative and Complementary Medicine, 16(10), 1039–1045. https://doi.org/10.1089/acm.2009.0577.
Whooley, M. A., & Wong, J. M. (2013). Depression and cardiovascular disorders. Annual Review of Clinical Psychology, 9, 327–354. https://doi.org/10.1146/annurev-clinpsy-050212-185526.
Yu, W. J., & Song, J. E. (2010). Effects of abdominal breathing on state anxiety, stress, and tocolytic dosage for pregnant women in preterm labor. Journal of Korean Academy of Nursing, 40(3), 442–452. https://doi.org/10.4040/jkan.2010.40.3.442.
Zhang, J. (2007). Effect of age and sex on heart rate variability in healthy subjects. Journal of Manipulative Physiological Therapeutics, 30(5), 374–379. https://doi.org/10.1016/j.jmpt.2007.04.001.
Acknowledgments
Special thanks to ICaterpillar Sdn. Bhd. for sponsoring the HRV device. We also wish to thank all the of the study participants.
Author information
Authors and Affiliations
Contributions
KSC assisted in the designing of the study, executed the study, analyzed the data, and wrote the paper. PEC collaborated in the writing and editing of the final manuscript. PFL formulated the research question, designed the study, and provided expert knowledge for the interpretation of the results. All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee of University of Tunku Abdul Rahman and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 26 kb)
Rights and permissions
About this article
Cite this article
Cheng, K.S., Croarkin, P.E. & Lee, P.F. Heart Rate Variability of Various Video-Aided Mindful Deep Breathing Durations and Its Impact on Depression, Anxiety, and Stress Symptom Severity. Mindfulness 10, 2082–2094 (2019). https://doi.org/10.1007/s12671-019-01178-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-019-01178-8