Abstract
Objectives
Self-compassion is a healthy way of relating to one’s self motivated by a desire to help rather than harm. Novel self-compassion-based interventions have targeted diverse populations and outcomes. This meta-analysis identified randomized controlled trials of self-compassion interventions and measured their effects on psychosocial outcomes.
Methods
This meta-analysis included a systematic search of six databases and hand-searches of the included study’s reference lists. Twenty-seven randomized controlled trials that examined validated psychosocial measures for self-compassion-based interventions met inclusion criteria. Baseline, post and follow-up data was extracted for the intervention and control groups, and study quality was assessed using the PRISMA checklist.
Results
Self-compassion interventions led to a significant improvement across 11 diverse psychosocial outcomes compared with controls. Notably, the aggregate effect size Hedge’s g was large for measures of eating behavior (g = 1.76) and rumination (g = 1.37). Effects were moderate for self-compassion (g = 0.75), stress (g = 0.67), depression (g = 0.66), mindfulness (g = 0.62), self-criticism (g = 0.56), and anxiety (g = 0.57) outcomes. Further moderation analyses found that the improvements in depression symptoms continued to increase at follow-up, and self-compassion gains were maintained. Results differed across population type and were stronger for the group over individual delivery methods. Intervention type was too diverse to analyze specific categories, and publication bias may be present.
Conclusions
This review supports the efficacy of self-compassion-based interventions across a range of outcomes and diverse populations. Future research should consider the mechanisms of change.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Self-compassion refers to the ability to be kind and helpful to one’s self at times of error or despair. This healthy way of relating to oneself effectively internalizes the compassion and support we may typically extend to a friend in times of need. Self-compassion has recently emerged as a construct of interest in clinical psychology, yet Eastern philosophies such as Buddhism have long recognized its importance (Brach 2003; Harris 1997; Kabat-Zinn 2009). Recent interest has been driven by the recognition of the link between a tendency to be self-compassionate and a plethora of mental health benefits. Neff (2003a) propagated the construct self-compassion as comprised of three core and interrelated components: self-kindness, connection, and mindfulness. Self-kindness is the tendency to extend kindness and support to oneself rather than engaging in harsh self-criticism or judgment. Connection encourages the recognition that imperfection is part of the human condition and discourages isolation and withdrawal. Mindfulness involves acknowledging and approaching negative thoughts or emotions with equanimity rather than over-identifying or wallowing in such patterns. An evolutionary perspective posits, in a complementary fashion, that self-compassion stimulates caregiving hormones (i.e., oxytocin) and physiological reactions (i.e., decreased heart rate) which enable feelings of safeness, connection, and compassionate motivation (Gilbert 2014; Kirby et al. 2017a). Thus, through the activation of the parasympathetic nervous system, it is proposed that self-compassion practice leads to physiological, psychological, and physical health benefits (Gilbert 2014).
The widespread use of the self-report 26-item self-compassion scale (SCS; Neff 2003a) and a shorter 12-itemed version (SCS-s; Raes et al. 2011) has contributed to the unification of a growing body of research. Both scales include six subscales: self-kindness versus self-judgment, mindfulness versus over-identification, and common humanity versus isolation. The SCS-s displays a near perfect correlation with the SCS long form (Raes et al. 2011). The recent controversy regarding the SCS includes an argument for a two-factor solution of positive and negatively orientated items (Muris and Petrocchi 2017) and questioning whether “self-compassion” is merely an absence of neuroticism rather than a new unique construct (Pfattheicher et al. 2017). In response, Neff argues that whilst self-compassion correlates with neuroticism, it is a distinct construct with meaningful incremental validity in predicting life satisfaction and is capable of identifying subtle treatment effects (Neff et al. 2018a). Neff et al. (2018a) also insist on the use of a total score or six-subscale score, based on factor analyses across international samples (N = 11,685). Overall self-compassion appears to offer a new theoretical framework for understanding adaptive ways of responding to personal suffering beyond what can be offered by neuroticism (Neff et al. 2018a).
A tendency to be self-compassionate has been linked with a diverse range of psychological and physical health outcomes. Dispositional self-compassion appears to predict the lack of typical markers of psychological disturbance such as neurotic perfectionism (Mehr and Adams 2016) and thought rumination (Svendsen et al. 2017). Perhaps, as a result, a lack of self-compassion appears to be a vulnerability factor for later depression (Krieger et al. 2016). A meta-analysis found lower self-compassion levels significantly predicted psychopathology including depression, anxiety, and stress symptoms (MacBeth and Gumley 2012). In addition to an absence of psychopathology, self-compassion has also been linked with greater self-reported psychological well-being (r = 0.47; Zessin et al. 2015). Finlay-Jones (2017) suggested that being self-compassionate may protect against poor clinical psychological outcomes by enabling adaptive emotion-regulation strategies such as healthy reappraisals, emotional acceptance, and self-soothing. Relatedly, self-compassion has also been linked with improved stress management in both controlled lab settings (Arch et al. 2016) and diverse real-world populations such as the elderly (Perez-Blasco et al. 2016), adolescents (Galla 2016), women managing infertility (Cunha et al. 2016), medical trainees (Richardson et al. 2016), and psychologist trainees (Finlay-Jones et al. 2015). Health psychology research suggests that self-compassion relates to better psychological and medical outcomes in the context of chronic illnesses including HIV (Yang and Mak 2017), diabetes (Ferrari et al. 2017a; Friis et al. 2016) and chronic pain (Wren et al. 2012). This extensive body of research suggests self-compassion may be a parsimonious and efficacious target for psychological treatment and intervention.
Although much of the literature conceptualizes self-compassion as a personality disposition or tendency, experimental studies have demonstrated that self-compassion is also a skill that can be acquired. Several interventions specifically focused on cultivating self-compassion have been developed and empirically assessed by different research groups. Two of the earliest self-compassion-based interventions are the Mindful Self-Compassion (MSC) program (Neff and Germer 2013) and compassion-focused therapy (CFT; Gilbert 2014). MSC is a structured program developed for non-clinical populations and run by two facilitators in either an eight-week or five-day intensive format. Topics covered included self-compassion, mindfulness, applying self-compassion to everyday life, and developing a compassionate inner voice, as well as living with core values, managing difficult emotions and relationships, and cultivating appreciation. The protocol also includes a four-hour silent retreat with yoga, meditation, and mindful eating (Neff and Germer 2013). In comparison, CFT is a group-therapy program designed for clinical populations. Gilbert (2014) describes a number of phases within CFT including psychoeducation seeking to reduce blame and shame and a formulation process to understand how early life experiences shaped “threat”, “doing” and “soothing systems”. These phases are followed by a focus on building compassion with imagery and breathing exercises and moving toward a self-compassionate identity and application of self-compassion to specific problems such as anxiety or depression. Although both approaches converge to target the development of a self-compassionate identity and application of self-compassion to manage difficulties, the treatments seeking to develop these skills do differ. Thus, a review of these current self-compassion-based interventions is timely, given the rapid growth of research and clinical work in this area.
Several existing literature reviews have examined compassion interventions, which are more broadly focused on increasing individuals’ general capacity for compassion, as opposed to specifically self-compassion. Such reviews linked compassion-based interventions with psychological improvements in a diverse range of populations including participants with brain injuries, eating disorders, personality disorders, and schizophrenia-spectrum disorders (Beaumont and Hollins 2015), and for people who are highly self-critical (Leaviss and Uttley 2015). More recently, a meta-analysis found compassion-based interventions led to benefits for both self-reported compassion (Cohen’s d = 0.55) and self-compassion (d = 0.70) and mental health outcomes such as depression (d = 0.64), anxiety (d = 0.49), and well-being (d = 0.51) (Kirby et al. 2017b).
The primary question addressed by this meta-analysis is to quantify the degree to which self-compassion, using a validated measure such as the SCS, can be increased through a psychological self-compassion intervention. This meta-analysis was also interested in the effect of such interventions on other psychosocial outcomes and, if reported, the long-term effects. This meta-analysis also sought to investigate the effect of intervention type, population type, and duration of intervention on the relationship between intervention and outcome. This meta-analysis sought to provide a useful summary of the diverse applications of self-compassion interventions to-date, and suggest directions for future research and clinical practice in this area.
Method
Protocol
The meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Hutton et al. 2015; Moher et al. 2010) and registered with Ferrari et al. (2017b :CRD42017069182).
Eligibility Criteria
Eligibility criteria required publications to be peer-reviewed, published in English, and report a randomized controlled trial (RCT) design which assessed the effectiveness of a self-compassion-based intervention (see Table 1 for full inclusion and exclusion criteria). Papers were excluded if they were unpublished, including submitted dissertations given if they had not yet undergone evaluation in a peer-review process.
Types of Participants
No limits were placed on the type of participants. Both clinical and non-clinical human populations were included, of all ages across the lifespan.
Types of Interventions
Included publications were required to refer to self-compassion theory and literature in the introduction, report the provision of an explicit explanation of self-compassion to participants, and include all three components of self-compassion: self-kindness, mindfulness, and connection (Neff 2003b). Other therapeutic interventions, such as CBT or ACT, which investigated the effects of alternative approaches on self-compassion as an outcome, were excluded (e.g., Yadavaia et al. 2014). Although there is a conceptual overlap, mindfulness-based interventions including the loving-kindness meditation were not the focus of the current review and are reviewed elsewhere (i.e., Galante et al. 2014; Zeng et al. 2015). Interventions which only briefly mentioned self-compassion (Ritzert et al. 2016) or involved solely meditation practice were excluded (e.g., Albertson et al. 2015).
Types of Comparisons
Data from all forms of active and passive control groups were extracted and included in the current review. For studies with multiple comparison groups, active controls were included to enable a more conservative comparison with reduced risk of type-I error (Borenstein et al. 2009).
Types of Outcomes
In addition to a self-compassion measure, psychosocial outcomes were included in the current review if they were measured using a validated scale in at least three independent studies (Rosenthal 1995).
Information Sources and Search Strategy
The literature search was conducted using PsycINFO, CINAHL, OVID Medline, Embase, Scopus, Web of Science, and PubMed databases using an identical search strategy. The final database search was conducted on 30 August 2017. Keyword searches were kept broad: (compassion* or compassionate or self-compassion or self compassion) AND (program or intervention* or treatment* or counselling or exposure or therap$). Limiters included peer-reviewed articles written in English. No time restriction was placed on included publications. The reference list of the identified empirical studies and previous reviews of self-compassion interventions was hand searched for additional studies.
Study Selection, Data Collection, and Synthesis of Results
Study eligibility was assessed in a standardized, non-blinded manner by the first author (MF) and checked by the second and third authors (CH, AH). All articles examined in the full-text screening (N = 269) were independently screened by two authors (MF, AH). Any discrepancies were documented and resolved via discussion. In instances where reporting of the data was incomplete (for example, Neff 2003a, b), authors were contacted and invited to share their data. Seven authors whose papers did not report data required for the current analysis were contacted. Of these, six replied and two were able to provide the requested data (Friis et al. 2016; Johnson and O'Brien 2013).
Data Extraction
A pilot data extraction database was tested against ten randomly selected included publications. Adjustments were made accordingly. The data extracted included publication details (authors, year, and country), participant demographics and recruitment details, intervention descriptions, outcomes measures, and relevant statistical data. Where available, outcome data for the longest reported follow-up time point was extracted for relevant outcomes. This follow-up data was classified as short (< 6 months), medium (6–12 months inclusive), or long (> 12 months).
Risk of Bias
The risk of bias was assessed at the study level. The Cochrane Collaboration’s tool for assessing risk of bias (Higgins et al. 2011) was adapted to assess the validity of the included psychological interventions (see Supplementary Material A for a full description of the adaptions made to the original tool). With respect to attrition rates, the mean participant dropout across all studies was 12.3% (ranging between 0 and 69.9%) between randomization and those who were included in the reported analysis. Four studies reported reasons for dropout beyond the participants being non-responsive. Friis et al. (2016) reported that during the intervention, one participant withdrew due to reasons related to the content of the intervention, another due to life stress. Koszycki et al. (2016) reported four dropouts from the intervention group due to finding a job (n = 2), illness, and family issues. Palmeira et al. (2017) reported that nine participants in their intervention group were excluded, four did not attend any treatment sessions, three dropped out after the first treatment session, one had bariatric surgery, and one experienced a severe depressive episode. Przezdziecki and Sherman (2016) reported that three participants in the intervention group discontinued as the content was not relevant, 16 failed to respond, and two did not receive the hardcopy intervention via in the post and therefore could not complete the intervention.
Results
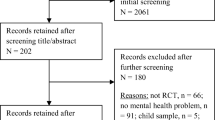
Initially, 21,934 titles were retrieved from the database searches, from which duplicates were removed (n = 10,520 removed, see Fig. 1). During title and abstract screening, 11,154 articles were excluded for violation of the inclusion criteria. During full-text screening, 240 articles were excluded, the most common reason for exclusion being the lack of an RCT design (n = 113). In total, 27 studies met the inclusion criteria and were included in the review. The interrater reliability for the independent full-text screening of two authors was strong (Kappa = 0.85, p < .001; Landis and Koch 1977). Across the 27 included studies, 1480 participants were involved. The participants were most likely to be in their 30s (Mage = 35.8) and female (M = 76.7%). Notably, no studies included in the current review examined the effects of self-compassion-based interventions for children or adolescents. Twenty-five (86%) of the included studies had been published in the last 5 years (since 2013), with seven published in 2016 and eight in 2017. Most were conducted in the Western countries including the USA (k = 6), UK (k = 5), and Canada (k = 4) (see Table 2 for the full list of study characteristics).
Risk of Bias Within Studies
Table 3 presents an assessment of the risk of bias for each study. Overall, the risk of detection bias was low given the frequent use of validated and often computerized self-report measures. In relation to selection bias, many studies failed to explicitly report the method of randomization used. In addition, many studies failed to report adequate allocation concealment for participant and investigator. Most studies did explicitly report attrition rates and reasons for participant dropouts. One study reported preregistration as an RCT in an online database (Palmeira et al. 2017). In this instance, all measures listed on the trial registry were reported in the final publication.
Study Results
In addition to self-compassion, ten primary outcomes were reported in the included studies including anxiety, depression, eating behavior, life satisfaction, mindfulness, negative affect, positive affect, rumination, self-criticism, and stress. Each effect-size analysis for these outcomes used Hedges’ g, a variation of Cohen’s d that corrects for biases due to small sample sizes (Hedges and Olkin 2014). Cohen has described effect sizes ≥ 0.2, 0.5, and 0.8 as small, moderate, and large, respectively (Cohen 1977). A random effects model acknowledged that the studies were not exact replicates of each other and that included samples that were not drawn from the same population (Borenstein et al. 2009). In instances when the same study reported on several measures for the same outcome, a CMA-calculated mean of the elected outcomes was used to prevent attributing greater weight to studies with multiple outcomes and avoid the bias of selecting one measure over another.
Self-Compassion Outcomes
Hedges’ g with 95% confidence intervals, significance testing, and heterogeneity statistics for all outcomes are presented in Table 4. Self-compassion-based interventions produced a medium and significant effect for the outcome self-compassion (g = 0.75; 95% CI 0.53–0.97) (Fig. 2). There is likely substantial heterogeneity in self-compassion effects as the Q-statistic was significant and I2 suggests that 84% of observed variance reflects true effect sizes rather than sampling error (Q(26) = 167.50, p < .001, I2 = 84.48, see Table 4).
Given the current debate about the utility of the self-compassion measure and the validity of a one-, two-, or six-factor solution (see Muris and Petrocchi 2017; Neff et al. 2018a, b; Pfattheicher et al. 2017), where available the subscale data as well as the SCS total score were analyzed. Fifteen studies used the SCS, and eight studies used the short version of the scale, the SCS-s. Self-compassion-based interventions had a stronger effect on the 26-item SCS (g = 0.85; 95% CI 0.53–1.18) than the 12-itemed SCS-s (g = 0.73; 95% CI 0.54–0.92). The SCS may represent moderate heterogeneity whereas the SCS-s heterogeneity effects were not significant (see heterogeneity statistics reported in Table 4). In relation to the subscale data, self-compassion-based interventions led to a large effect for over-identification (g = 0.84; 95% CI 0.49–1.20), a moderate effect for common humanity (g = 0.66; 95% CI 0.06–1.25), self-judgment (g = 0.63; 95% CI 0.30–0.96), self-kindness (g = 0.58; 95% CI 0.12–1.05), and isolation (g = 0.56; 95% CI 0.24–0.89), and a small effect for mindfulness (g = 0.40; 95% CI 0.09–0.70). Heterogeneity was not significant for the negative subscales of over-identification, self-judgment, and isolation; however, results suggested moderate heterogeneity for the positive subscales: common humanity, self-kindness, and mindfulness.
Clinical Outcomes
Self-compassion-based interventions led to a large and significant effect on eating behaviors (g = 1.76; 95% CI 0.53–2.99). A moderate and significant effect was found for stress (g = 0.67; 95% CI 0.37–0.96), depression (g = 0.66; 95% CI 0.45–0.87), and anxiety (g = 0.57; 95% CI 0.33–0.82). Comparatively, a small yet still significant effect was found for negative affect (g = 0.33; 95% CI 0.11–0.56). Heterogeneity statistics suggest there may be substantial heterogeneity for eating behavior and moderate heterogeneity for depression and anxiety, whereas heterogeneity was not significant for stress and negative affect (see Table 4).
Well-being Outcomes
Self-compassion-based interventions led to a small and significant effect on positive affect (g = 0.48; 95% CI 0.19–0.77) and life satisfaction (g = 0.40; 95% CI 0.05–0.75). Tests of heterogeneity were not significant, and there was low variation in effect sizes for both outcomes.
Psychological Process Outcomes
Self-compassion-based interventions led to a large and significant effect on rumination outcomes (g = 1.37; 95% CI 0.09–2.64). A moderate and significant effect was found for mindfulness (g = 0.62; 95% CI 0.44–0.80), and self-criticism (g = 0.56; 95% CI 0.30–0.82). Tests of heterogeneity were significant and indicated substantial variation in effect sizes for rumination and moderate variation for mindfulness, whereas the test of heterogeneity was not significant for self-criticism (see Table 4).
Outcomes at Follow-up Time Points
Depression and self-compassion were the only outcomes measured at a follow-up time point across at least three studies. Depression was measured at 1-month (Ivtzan et al. 2016), 2-month (Wong and Mak 2016), and 3-month (Arimitsu 2016; Friis et al. 2016) follow-up time points. Self-compassion was measured at 1-month (Ivtzan et al. 2016; Mosewich et al. 2013), 2-month (Wong and Mak 2016), and 3-month (Arimitsu 2016; Friis et al. 2016) follow-up time points. A small yet significant effect at follow-up was found for depression symptoms (g = 0.33; 95% CI: 0.09–0.58) while the effect for self-compassion was too small to be meaningful (g = 0.19; 95% CI 0.03–0.36). These effects suggest that intervention groups maintained improvements in both depressive and self-compassion scores from post-intervention to respective follow-up time points, and a slight continued improvement in depression symptoms.
Pre-Post Effects of Self-Compassion-Based Interventions Across Populations
There were no child RCT studies which met inclusion criteria for the current review; all included studies investigated adults with the lowest reported mean age being 19.7 years (Johnson and O'Brien 2013). The populations examined could be categorized broadly into four groups: community samples; clinical samples; clinical health samples (e.g., adults diagnosed with diabetes (Friis et al. 2016) and survivors of breast cancer (Przezdziecki and Sherman 2016)); or university samples (see “Population” column in Table 2). Effects for the self-compassion outcome were significant and large for community samples (k = 8, g = 0.83; 95% CI 0.61–1.05) and clinical samples (k = 9, g = 0.82; 95% CI 0.28–1.36). Effects were moderate and significant for clinical health samples (k = 3; g = 0.56; 95% CI 0.20–0.92) and small for university populations (k = 7, g = 0.47; 95% CI 0.20–0.74). The between-group heterogeneity tests comparing the four populations were not significant (see Table 4).
Pre-Post Effects of Self-Compassion-Based Interventions Across Different Comparison Groups
Across all studies, there was considerable variation in the type of control group used (see “Control” column in Table 2). Several outcomes were measured across enough studies to enable a comparison of effects between waitlist and active control groups. Of these, effects for depression outcomes were consistently significant and moderate when comparing self-compassion-based interventions to both waitlists (g = 0.67, 95% CI 0.51–0.83) and active control groups (g = 0.79, 95% CI 0.07–1.50; see Table 4). In comparison, improvements in self-compassion and mindfulness remained significant but appeared to be less pronounced when comparing self-compassion interventions to a more conservative active control group (see effect sizes, 95% confidence intervals, and tests of heterogeneity in Table 4). For example, there was a significant and large effect for the outcome self-compassion in studies reporting a waitlist control (g = 0.87; 95% CI 0.63–1.12), while studies reporting an active control comparison showed a significant and small effect (g = 0.42; 95% CI 0.20–0.64). In studies reporting a waitlist comparison group, improvements in anxiety (g = 0.70; 95% CI 0.44–0.96) and self-criticism (g = 0.67; 95% CI 0.35–0.98) outcomes were significant; however, these effects were non-significant in studies reporting an active control group comparison (anxiety g = 0.28; 95% CI − 0.03–0.59; self-criticism g = 0.37; 95% CI − 0.09–0.82). The test of between-groups heterogeneity was not significant for depression or rumination outcomes and was significant for anxiety, mindfulness, and self-compassion outcomes (see Table 4).
Clinical Significance of Self-Compassion-Based Interventions According to Treatment Approach
Given the diversity of self-compassion interventions included, any attempt to cluster specific intervention approaches would be subjective. There were, however, enough studies reporting on a group versus an individual delivery method to facilitate a comparison. Group-based delivery had a significant and large effect on self-compassion (g = 0.81; 95% CI 0.59–1.04) whereas an individual delivery produced a significant yet small effect (g = 0.37; 95% CI 0.14–0.56). There was a moderate and significant amount of between-group heterogeneity in treatment approach (see Table 4). There was great variability in reported treatment intensity (see Table 2). Interventions ranged from one session (Ascone et al. 2017; Mosewich et al. 2013) to 12 1.5-h sessions across 12 weeks (Koszycki et al. 2016). Across all interventions, the mean number of sessions was six.
Risk of Bias Across Studies
The risk of publication bias is pertinent in an emerging area of research such as self-compassion. Visual inspection of the funnel plot suggested a slight trend toward asymmetry with more studies on the right toward the bottom of the plot (see Fig. 3). This may indicate a slight risk of publication bias wherein there is an increased likelihood for published studies to contain significant results. The failsafe N for self-compassion outcomes was 1589. This was deemed to be a substantial number of unpublished studies with no effect that would need to exist to turn the p value to be non-significant. The trim and fill analysis, when looking for missing studies to the left side of the mean effect (favoring control), suggests no studies are missing. Under the random effects model, the point estimate for the combined studies is g = 0.60 (95% CI 0.52–0.68). Taken together, the risk of publication bias appears to be small.
Discussion
The current meta-analysis found that a broad range of existing self-compassion-based interventions have been recently assessed using RCTs, indicative of a growing area of clinical practice and research. The current systematic search identified 27 RCT studies that met inclusion criteria, involving 1480 participants. In addition to the primary outcome, self-compassion, nine other psychosocial outcomes were measured across enough studies to be included in the analysis. Overall, self-compassion-based interventions produced a moderate and significant improvement in self-compassion scores, supporting the conceptualization of self-compassion as a malleable construct which can be cultivated. Self-compassion-based interventions also produced significant improvements across all other identified outcomes compared with control interventions, although the size of these effects differed. Large effect sizes were found for eating behavior and rumination outcomes. This suggests that cultivating one’s self-compassion may be protective when treating eating difficulties, including binge-eating disorder (Duarte et al. 2017; Kelly and Carter 2015; Kelly et al. 2017) and weight loss (Palmeira et al. 2017). The improvement in ruminative thought patterns may suggest that self-compassion cultivates a healthier and adaptive style of thinking. This shift in cognitive patterns may be the mechanism through which self-compassion treats multiple psychopathologies including depression (Ferrari et al. 2018; Krieger et al. 2016) and anxiety (MacBeth and Gumley 2012). Moderate effect sizes were found for stress, depression, mindfulness, self-criticism, and anxiety outcomes. Comparatively, small yet still significant effects were found for positive affect, life satisfaction, and negative affect outcomes. Taken together, self-compassion-based interventions appear to foster improvement across a range of both clinical symptoms and indicators of wellbeing.
At follow-up time points, self-compassion intervention groups continued to make small improvements in depression symptoms, and self-compassion scores were maintained. Although follow-up data were only reported by a small number of studies (depression k = 4; self-compassion k = 5), these promising findings suggest that improvements in self-compassion are enduring. Thus teaching individuals a kinder, more self-compassionate way of responding to times of distress appears to be a skill which can generalize to long-term functioning. Furthermore, practicing self-compassion may continue to have a compound effect on depression symptoms, further reducing their prevalence over time. This supports prior research which argues self-compassion has a buffering effect against the manifestation of depression symptoms (Ferrari et al. 2018).
Across the included studies, the most common measure of self-compassion was the SCS (k = 23; Neff 2003a). Other scales included the Fears of Compassion Scale (FCS), the Compassionate Attributes and Actions Scales (CAAS), and an adapted Self-Compassionate Attitude scale (SCA; Przezdziecki and Sherman 2016). In the current meta-analysis, the SCS (long form) produced a similar effect size to the analysis of all self-compassion measures combined. Theoretically, these scales measure different aspects of compassion including the motivation to engage in difficult feelings (CEAS engagement subscale) and the ability to focus on what is helpful (CEAS action subscale); fears of experiencing compassion for self, others, and from others (FCS); and self-compassion in relation to body image (SCA).
The results of the current meta-analysis contribute to a growing body of literature which supports the efficacy of self-compassion-based interventions targeting a broad range of populations and outcomes (Beaumont and Hollins 2015). A prior systematic review by Leaviss and Uttley (2015) found compassion interventions improved self-criticism compared with treatment as usual. The current review converges with this finding and specifies a moderate effect size for this outcome. The aggregate effect sizes in the current meta-analysis are generally consistent with effect sizes found in the recent meta-analysis of compassion-based interventions conducted by Kirby (2017b). Both reviews found large effect sizes for self-compassion as an outcome and moderate effect sizes for anxiety and depression. Kirby (2017b) also measured the outcome well-being (d = 0.51), upon which self-compassion interventions enacted a similar sized effect to the construct life satisfaction in the current review (g = 0.40). The current review extends on this research by finding that self-compassion-based interventions, compared with control conditions, are associated with significant improvement across eight additional diverse psychosocial outcomes.
Further moderation analyses examined whether the effects of self-compassion-based interventions differed when examining studies that utilized a waitlist versus an active control comparison. The intervention effects on depression outcomes were consistent and moderate across all control group types, indicating a robust effect. This also suggests that for depression symptoms, self-compassion-based interventions may have an effect comparable to more established interventions such as CBT (Beaumont et al. 2012) and mindfulness practice (Feliu-Soler et al. 2017). Although further research is required to establish the strength of self-compassion-based interventions relative to current evidence-based practice, the current results are promising. Aggregate effects for self-compassion and mindfulness outcomes were smaller yet still significant for studies containing active controls compared with waitlist, suggesting that whilst not as robust as changes in depression scores, self-compassion-based interventions are also beneficial for these outcomes. In contrast, effects for anxiety and self-criticism were moderate and significant in studies using a waitlist control group, but became non-significant when compared with active control groups. This trend may indicate that self-compassion-based interventions are less effective for anxiety outcomes than approaches such as CBT-based programs (Armstrong and Rimes 2016; Beaumont et al. 2012), or imagery work (Ascone et al. 2017; Campbell et al. 2017). Self-compassion-based interventions may also be less effective for self-criticism outcomes than attention control (Mosewich et al. 2013), mindfulness (Feliu-Soler et al. 2017), or imagery work (Ascone et al. 2017). Taken together, these results suggest self-compassion-based interventions demonstrate the most robust effects on depression outcomes, strong effects for mindfulness and self-compassion outcomes, and potentially weaker effects for anxiety and self-criticism outcomes. Eating behavior, stress, and rumination outcomes also demonstrated moderate to large effects as a result of self-compassion interventions; however, not enough studies examined different control groups to compare this effect across active versus waitlist control groups.
It is a marker of the exponential growth of research in the self-compassion field that many RCTs, despite intensive resource and time costs associated with this research methodology, were available for the current meta-analysis. Across the 27 included RCT studies, the 1480 participants who were involved tended to be aged in their 30s and are female. The majority of the included studies were conducted in Western countries and published in the last 5 years (86%). Although the uptake of self-compassion-based approaches seems to be high in individualistic societies, a growing number of studies have demonstrated efficacy in other cultural contexts (Arimitsu 2016; Dundas et al. 2017; Feliu-Soler et al. 2017; Lee and Bang 2010; Wong and Mak 2016). This may lend support to the universality of self-compassion; whether individuals respond to pain and distress with self-compassion and kindness or self-criticism seems to be important across different cultural contexts.
When examining the populations in which self-compassion interventions have been assessed, a significant and measurable benefit was found in the clinical, community, and clinical health populations, with smaller but still significant effects in university populations. Self-compassion-based interventions demonstrated benefit across all four types of populations, suggesting that self-compassion approaches have high acceptability in broader society compared with other evidence-based treatments, such as CBT, which are typically reserved for clinical samples and less frequently delivered in non-clinical community samples. The large effect on self-compassion outcomes for clinical samples suggests that self-compassion interventions are a viable option for more severe clinical presentations. A clinical presentation commonly targeted with self-compassion-based interventions in the current meta-analysis was disordered eating (Duarte et al. 2017; Kelly and Carter 2015; Kelly et al. 2017). Theoretically, this is cogent given that self-compassion approaches may directly target the high levels of perfectionism and self-criticism that underpin this psychopathology. Seeking to better understand the influence of self-compassion within the context of physical health conditions or health-related behaviors, such as eating, is an area for further study. Although this meta-analysis found large effects for improvements in eating behaviors, Mantzios and Egan (2017) argue self-compassion may be confabulated with self-kindness and lead to poor decision-making in the context of some health behaviors such as eating. For example, prioritizing positive affect may encourage eating high-sugar-content foods and subvert long-term weight management goals with short-term hedonistic goals. Although self-compassion overall appears to be beneficial in enhancing self-reported eating behaviors, further nuanced studies could examine potential pitfalls in practicing a self-compassionate response.
Community samples appeared to benefit from self-compassion-based interventions, potentially indicating that practicing self-compassion leads to improvements in psychological functioning within healthy populations. Overall effects were moderate for the three health populations including adults with brain injury (Campbell et al. 2017), adults with diabetes (Friis et al. 2016), and breast cancer survivors (Przezdziecki and Sherman 2016). The benefits of self-compassion within the context of chronic illness may be pertinent given high demands of self-management treatment regimens and the relative lack of control over symptoms that accompany such presentations. Though still significant, the smallest effects for self-compassion outcomes were found in university populations. University samples may be prone to perfectionistic tendencies and self-criticism in the context of academic pressure (Harvey et al. 2015). Such vulnerabilities would theoretically benefit from self-compassion interventions; however, in the current meta-analysis this effect seems to be small.
This meta-analysis also examined the influence of group and individual modes of delivery on self-compassion outcomes, finding a stronger effect for group-based delivery. A potential explanation for this trend may be that group delivery enables an experiential lived experience of connection (as opposed to isolation), which aligns with the core theoretical framework for self-compassion. Group-based delivery may also encourage sharing and discussing the personal relevance of intervention concepts, reinforcing common humanity and acceptance of flaws, as seen in other mindfulness-based trials (i.e., Mantzios and Giannou 2014). Future research would make a valuable contribution to self-compassion literature by directly comparing the effects of different approaches to identify which is most successful at increasing self-compassion and other psychosocial outcomes.
The original protocol of this meta-analysis had intended to compare different approaches to teaching or implementing a self-compassion intervention. The vast diversity across the studies prevented this analysis. Overall, most studies implemented an intervention that was eclectic and combined self-compassion concepts and practices with other approaches including acceptance and commitment therapy (ACT; Palmeira et al. 2017), mindfulness or meditation practice (Feliu-Soler et al. 2017; Ivtzan et al. 2016), or compassion-focused therapy (Ascone et al. 2017; Campbell et al. 2017; Duarte et al. 2017). A potential direction for future research may be to consider whether self-compassion is most effective as a stand-alone intervention or as an adjunct to other evidence-based therapies. The intensity of the included interventions also varied from experimental mood manipulations conducted with writing prompts (for example, Johnson and O'Brien 2013; Przezdziecki and Sherman 2016) to manualized therapy interventions (for example, Friis et al. 2016; Neff and Germer 2013).
Limitations and Directions for Future Research
This meta-analysis may be subject to a number of potential limitations and biases, including, common to many meta-analytic reviews, the risk of publication bias. As discussed above, the failsafe N and funnel plot analyses suggest that publication bias is unlikely to be a significant threat to the current findings. Of greater concern is that only one of the included studies had registered their trial with an online database prior to commencing data collection. This simple process can significantly increase confidence in the future development of self-compassion literature. Based on the current quality assessment, further methodological recommendations to improve the quality of self-compassion studies include conducting RCTs with active controls using evidence-based treatment, collecting follow-up data, and complying with CONSORT guidelines. These recommendations are similar to those of Kirby (2017b) on the basis of their compassion meta-analysis. Kirby (2017b) also call for experience-sampling approaches to measure self-compassion, greater detail when describing intervention content to facilitate an understanding of mechanisms of change, consideration of dosage effects, and an assessment of the acceptability of such interventions.
No studies that met inclusion criteria for the current meta-analysis investigated child or adolescent populations. This trend suggests a lack of RCT studies assessing the relevance of self-compassion for younger populations. This represents a notable gap in the literature considering the increasing body of research in adolescent samples linking self-compassion to health outcomes such as emotional well-being (Bluth and Blanton 2014; Galla 2016), and resilience against low self-esteem (Marshall et al. 2015; Neff and McGehee 2010). Kirby et al. (2017a, b) have also previously noted this gap in research involving children or adolescents.
An important question that this meta-analysis was unable to answer is how self-compassion has an effect on such a diverse range of psychosocial outcomes. In other words, what is the mechanism of change through which self-compassion has an effect? After analyzing the effect of self-compassion-based interventions on the SCS subscales, the effect sizes were consistent across most subscales, but slightly larger for over-identification. This supports Neff’s suggestion (Neff 2003b) that all three facets of self-compassion (self-kindness, mindfulness, and connection) overlap and work together to form a generally healthy way of relating to oneself. Given that the unified construct of “self-compassion” is supported by the current meta-analysis, future research should consider measuring potential mechanisms of change through which self-compassion has an effect on psychological and health outcomes. Such mechanisms may include the practice of meditation (Zeng et al. 2015), increased emotion-regulation skill (Finlay-Jones 2017), greater self-regulation (Kelly et al. 2010), physiological changes such as regulated heart rate (Kirby et al. 2017a, b), enhanced social connection (Kok et al. 2013), or perhaps a more cognitive mechanism such as advanced reappraisal skills that are core to CBT approaches.
Overall, the results of the current meta-analysis indicate that self-compassion-based interventions are a promising area of intervention for a diverse range of psychosocial outcomes across a wide range of populations. There is currently strong uniformity in the self-compassion literature in relation to the measurement of self-compassion because of the widespread use of the validated SCS measure. Although there are several self-compassion-based interventions that are well established with clear training pathways and manualized protocols (for example, MSC and CFT), this meta-analysis identified a diverse range of other approaches that show promise. This paper aims to provide some organization and synthesis to a rapidly growing area of research, and encourage further development of evidence-based approaches teaching and practicing self-compassion.
References
Albertson, E. R., Neff, K. D., & Dill-Shackleford, K. E. (2015). Self-compassion and body dissatisfaction in women: a randomized controlled trial of a brief meditation intervention. Mindfulness, 6(3), 444–454. https://doi.org/10.1007/s12671-014-0277-3.
Arch, J. J., Landy, L. N., & Brown, K. W. (2016). Predictors and moderators of biopsychological social stress responses following brief self-compassion meditation training. Psychoneuroendocrinology, 69, 35–40. https://doi.org/10.1016/j.psyneuen.2016.03.009.
Arimitsu, K. (2016). The effects of a program to enhance self-compassion in Japanese individuals: a randomized controlled pilot study. Journal of Positive Psychology, 11(6), 559–571. https://doi.org/10.1080/17439760.2016.1152593.
Armstrong, L., & Rimes, K. A. (2016). Mindfulness-based cognitive therapy for neuroticism (stress vulnerability): a pilot randomized study. Behavior Therapy, 47(3), 287–298. https://doi.org/10.1016/j.beth.2015.12.005.
Ascone, L., Sundag, J., Schlier, B., & Lincoln, T. M. (2017). Feasibility and effects of a brief compassion-focused imagery intervention in psychotic patients with paranoid ideation: a randomized experimental pilot study. Clinical Psychology & Psychotherapy, 24(2), 348–358. https://doi.org/10.1002/cpp.2003.
Beaumont, E., & Hollins, M. C. (2015). A narrative review exploring the effectiveness of compassion-focused therapy. Counselling Psychology Review, 30(1), 21–32.
Beaumont, E., Galpin, A., & Jenkins, P. (2012). ‘Being kinder to myself’: a prospective comparative study, exploring post-trauma therapy outcome measures, for two groups of clients, receiving either cognitive behavior therapy or cognitive behavior therapy and compassionate mind training. Counselling Psychology Review, 27(1), 31–43 Retrieved from: http://usir.salford.ac.uk/id/eprint/39206.
Bluth, K., & Blanton, P. W. (2014). Mindfulness and self-compassion: exploring pathways to adolescent emotional well-being. Journal of Child and Family Studies, 23(7), 1298–1309. https://doi.org/10.1007/s10826-013-9830-2.
Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2009). Introduction to meta-analysis (vol. 10). Chichester: John Wiley & Sons, Ltd..
Brach, T. (2003). Radical acceptance: Awakening the love that heals fear and shame within us. Random House.
Campbell, I. N., Gallagher, M., McLeod, H. J., O'Neill, B., & McMillan, T. M. (2017). Brief compassion focused imagery for treatment of severe head injury. Neuropsychological Rehabilitation, 1–11. https://doi.org/10.1080/09602011.2017.1342663.
Cohen, J. (1977). Statistical power analysis for the behavioral sciences (rev. ed.). Hillsdale: Lawrence Erlbaum Associates, Inc..
Cornish, M. A., & Wade, N. G. (2015). Working through past wrongdoing: examination of a self-forgiveness counseling intervention. Journal of Counseling Psychology, 62(3), 521–528. https://doi.org/10.1037/cou0000080.supp.
Cunha, M., Galhardo, A., & Pinto-Gouveia, J. (2016). Experiential avoidance, self-compassion, self-judgment and coping styles in infertility. Sexual & Reproductive Healthcare, 10, 41–47. https://doi.org/10.1016/j.srhc.2016.04.001.
Duarte, C., Pinto-Gouveia, J., & Stubbs, R. J. (2017). Compassionate attention and regulation of eating behavior: a pilot study of a brief low-intensity intervention for binge eating. Clinical Psychological Psychotherapy., 14(6). https://doi.org/10.1002/cpp.2094.
Dundas, I., Binder, P.-E., Hansen, T. G. B., & Stige, S. H. (2017). Does a short self-compassion intervention for students increase healthy self-regulation? A randomized control trial. Scandinavian Journal of Psychology, 58(5), 443–450. https://doi.org/10.1111/sjop.12385.
Feliu-Soler, A., Pascual, J. C., Elices, M., Martin-Blanco, A., Carmona, C., Cebolla, A., et al. (2017). Fostering self-compassion and loving-kindness in patients with borderline personality disorder: a randomized pilot study. Clinical Psychological Psychotherapy, 24(1), 278–286. https://doi.org/10.1002/cpp.2000.
Ferrari, M., Dal Cin, M., & Steele, M. (2017a). Self-compassion is associated with optimum self-care behavior, medical outcomes and psychological well-being in a cross-sectional sample of adults with diabetes. Diabetic Medicine, 34(11), 1546–1553. https://doi.org/10.1111/dme.13451.
Ferrari, M., Harrysunker, A., Hunt, C., Abbott, M., & Einstein, D. (2017b). The skill of self-kindness: a metaanalysis of randomized controlled trials investigating self-compassion-based interventions [Protocol]. PROSPERO 2017 CRD42017069182. Retrieved from: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017069182. Accessed 5 Apr 2019.
Ferrari, M., Yap, K., Scott, N., Einstein, D. A., & Ciarrochi, J. (2018). Self-compassion moderates the perfectionism and depression link in both adolescence and adulthood. PLoS One, 13(2), e0192022.
Finlay-Jones, A. L. (2017). The relevance of self-compassion as an intervention target in mood and anxiety disorders: a narrative review based on an emotion regulation framework. Clinical Psychologist, 21(2), 90–103. https://doi.org/10.1111/cp.12131.
Finlay-Jones, A. L., Rees, C. S., & Kane, R. T. (2015). Self-compassion, emotion regulation and stress among Australian psychologists: testing an emotion regulation model of self-compassion using structural equation modeling. PLoS One, 10(7). https://doi.org/10.1371/journal.pone.0133481.
Friis, A. M., Johnson, M. H., Cutfield, R. G., & Consedine, N. S. (2016). Kindness matters: a randomized controlled trial of a mindful self-compassion intervention improves depression, distress, and HbA1c among patients with diabetes. Diabetes Care, 39(11), 1963–1971. https://doi.org/10.2337/dc16-0416.
Galante, J., Galante, I., Bekkers, M.-J., & Gallacher, J. (2014). Effect of kindness-based meditation on health and well-being: a systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 82(6), 1101. https://doi.org/10.1037/a0037249.
Galla, B. M. (2016). Within-person changes in mindfulness and self-compassion predict enhanced emotional well-being in healthy, but stressed adolescents. Journal of Adolescence, 49, 204–217. https://doi.org/10.1016/j.adolescence.2016.03.016.
Gilbert, P. (2014). The origins and nature of compassion focused therapy. British Journal of Clinical Psychology, 53(1), 6–41. https://doi.org/10.1111/bjc.12043.
Gilbert, P., & Procter, S. (2006). Compassionate mind training for people with high shame and selfcriticism: overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 13(6), 353–379.
Harris, E. J. (1997). Detachment and compassion in early Buddhism. Buddhist Publication Society.
Harvey, B., Milyavskaya, M., Hope, N., Powers, T. A., Saffran, M., & Koestner, R. (2015). Affect variation across days of the week: influences of perfectionism and academic motivation. Motivation and Emotion, 39(4), 521–530.
Hedges, L. V., & Olkin, I. (2014). Statistical method for meta-analysis. Academic press.
Held, P., & Owens, G. P. (2015). Effects of self-compassion workbook training on trauma-related guilt in a sample of homeless veterans: a pilot study. Journal of Clinical Psychology, 71(6), 513–526. https://doi.org/10.1002/jclp.22170.
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. British Medical Journal, 343, d5928. https://doi.org/10.1136/bmj.d5928.
Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmid, C. H., Cameron, C., et al. (2015). The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Annals of Internal Medicine, 162(11), 777–784. https://doi.org/10.7326/M14-2385.
Ivtzan, I., Young, T., Martman, J., Jeffrey, A., Lomas, T., Hart, R., & Eiroa-Orosa, F. J. (2016). Integrating mindfulness into positive psychology: a randomised controlled trial of an online positive mindfulness program. Mindfulness, 7, 1396–1407. https://doi.org/10.1007/s12671-016-0581-1.
Jazaieri, H., Jinpa, G. T., McGonigal, K., Rosenberg, E. L., Finkelstein, J., Simon-Thomas, E., … & Goldin, P. R. (2013). Enhancing compassion: a randomized controlled trial of a compassion cultivation training program. Journal of Happiness Studies, 14(4), 1113–1126. https://doi.org/10.1007/s10902-012-9373-z.
Johnson, E. A., & O'Brien, K. A. (2013). Self-compassion soothes the savage EGO-threat system: effects on negative affect, shame, rumination, and depressive symptoms. Journal of Social and Clinical Psychology, 32(9), 939–963. https://doi.org/10.1521/jscp2013329939.
Kabat-Zinn, J. (2009). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delta.
Kelly, A. C., & Carter, J. C. (2015). Self-compassion training for binge eating disorder: a pilot randomized controlled trial. Psychology and Psychotherapy: Theory, Research and Practice, 88(3), 285–303. https://doi.org/10.1111/papt.12044.
Kelly, A. C., Zuroff, D., Foa, C., & Gilbert, P. (2010). Who benefits from training in self-compassionate self-regulation? A study of smoking reduction. Journal of Social and Clinical Psychology, 29(7), 727–755. https://doi.org/10.1002/cpp.2018.
Kelly, A. C., Wisniewski, L., Martin-Wagar, C., & Hoffman, E. (2017). Group-based compassion-focused therapy as an adjunct to outpatient treatment for eating disorders: a pilot randomized controlled trial. Clinical Psychological Psychotherapy, 24(2), 475–487. https://doi.org/10.1002/cpp.2018.
Kirby, J. N., Doty, J. R., Petrocchi, N., & Gilbert, P. (2017a). The current and future role of heart rate variability for assessing and training compassion. Frontiers in Public Health, 5. https://doi.org/10.3389/fpubh.2017.00040.
Kirby, J. N., Tellegen, C. L., & Steindl, S. R. (2017b). A meta-analysis of compassion-based interventions: current state of knowledge and future directions. Behavior Therapy, 48(6), 778–792. https://doi.org/10.1016/j.beth.2017.06.003.
Kok, B. E., Coffey, K. A., Cohn, M. A., Catalino, L. I., Vacharkulksemsuk, T., Algoe, S. B., … & Fredrickson, B. L. (2013). How positive emotions build physical health: perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychological Science, 24(7), 1123–1132. https://doi.org/10.1177/0956797612470827.
Koszycki, D., Thake, J., Mavounza, C., Daoust, J. P., Taljaard, M., & Bradwejn, J. (2016). Preliminary investigation of a mindfulness-based intervention for social anxiety disorder that integrates compassion meditation and mindful exposure. Journal of Alternative and Complementary Medicine, 22(5), 363–374. https://doi.org/10.1089/acm.2015.0108.
Krieger, T., Berger, T., & Grosse, M. H. (2016). The relationship of self-compassion and depression: cross-lagged panel analyses in depressed patients after outpatient therapy. Journal of Affective Disorders, 202, 39–45. https://doi.org/10.1016/j.jad.2016.05.032.
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 159–174. https://doi.org/10.2307/2529310.
Leaviss, J., & Uttley, L. (2015). Psychotherapeutic benefits of compassion-focused therapy: an early systematic review. Psychological Medicine, 45(5), 927–945. https://doi.org/10.1017/S0033291714002141.
Lee, W. K., & Bang, H. J. (2010). The effects of mindfulness-based group intervention on the mental health of middle-aged Korean women in community. Stress and Health, 26(4), 341–348. https://doi.org/10.1002/smi.1303.
MacBeth, A., & Gumley, A. (2012). Exploring compassion: a meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32(6), 545–552. https://doi.org/10.1016/j.cpr.2012.06.003.
Mantzios, M., & Egan, H. H. (2017). On the role of self-compassion and self-kindness in weight regulation and health behavior change. Frontiers in Psychology, 8, 229. https://doi.org/10.3389/fpsyg.2017.00229.
Mantzios, M., & Giannou, K. (2014). Group vs. single mindfulness meditation: exploring avoidance, impulsivity, and weight management in two separate mindfulness meditation settings. Applied Psychology: Health and Well‐Being, 6(2), 173–191.
Mantzios, M., & Wilson, J. C. (2014). Making concrete construals mindful: a novel approach for developing mindfulness and self-compassion to assist weight loss. Psychology & Health, 29(4), 422–441. https://doi.org/10.1080/08870446.2013.863883.
Marshall, S. L., Parker, P. D., Ciarrochi, J., Sahdra, B., Jackson, C. J., & Heaven, P. C. (2015). Self-compassion protects against the negative effects of low self-esteem: a longitudinal study in a large adolescent sample. Personality and Individual Differences, 74, 116–121. https://doi.org/10.1016/j.paid.2014.09.013.
Matos, M., Duarte, C., Duarte, J., Pinto-Gouveia, J., Petrocchi, N., Basran, J., & Gilbert, P. (2017). Psychological and physiological effects of compassionate mind training: a pilot randomised controlled study. Mindfulness, 1–14. https://doi.org/10.1007/s12671-017-0745-7.
Mehr, K. E., & Adams, A. C. (2016). Self-compassion as a mediator of maladaptive perfectionism and depressive symptoms in college students. Journal of College Student Psychotherapy, 30(2), 132–145. https://doi.org/10.1080/87568225.2016.1140991.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Group, P. (2010). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International Journal of Surgery, 8(5), 336–341. https://doi.org/10.1016/j.ijsu.2010.02.007.
Mosewich, A. D., Crocker, P. R., Kowalski, K. C., & DeLongis, A. (2013). Applying self-compassion in sport: an intervention with women athletes. Journal of Sport and Exercise Psychology, 35(5), 514–524. https://doi.org/10.1123/jsep.35.5.514.
Muris, P., & Petrocchi, N. (2017). Protection or vulnerability? A meta-analysis of the relations between the positive and negative components of self-compassion and psychopathology. Clinical Psychology Psychotherapy, 24(2), 373–383. https://doi.org/10.1002/cpp.2005.
Neff, K. D. (2003a). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860309027.
Neff, K. D. (2003b). Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(2), 85–101. https://doi.org/10.1080/15298860309032.
Neff, K. D., & Germer, C. K. (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology, 69(1), 28–44. https://doi.org/10.1002/jclp.21923.
Neff, K. D., & McGehee, P. (2010). Self-compassion and psychological resilience among adolescents and young adults. Self and Identity, 9(3), 225–240. https://doi.org/10.1080/15298860902979307.
Neff, K. D., Tóth-Király, I., & Colosimo, K. (2018a). Self-compassion is best measured as a global construct and is overlapping with but distinct from neuroticism: a response to Pfattheicher, Geiger, Hartung, Weiss, and Schindler (2017). European Journal of Personality, 32(4), 371–392. https://doi.org/10.1002/per.2148.
Neff, K. D., Tóth-Király, I., Yarnell, L., Arimitsu, K., Castilho, P., Ghorbani, N., & Mantios, M. (2018b). Examining the factor structure of the self-compassion scale using exploratory SEM bifactor analysis in 20 diverse samples: support for use of a total score and six subscale scores. Psychological Assessment, 99, 596–607. https://doi.org/10.1080/00223891.2016.1269334.
Palmeira, L., Cunha, M., & Pinto-Gouveia, J. (2017). Processes of change in quality of life, weight self-stigma, body mass index and emotional eating after an acceptance-, mindfulness- and compassion-based group intervention (kg-free) for women with overweight and obesity. Journal of Health Psychology, 1–14. https://doi.org/10.1177/1359105316686668.
Park, S. H. (2006). Development of the mindfulness scale. Doctoral dissertation, Catholic University, Korea.
Perez-Blasco, J., Viguer, P., & Rodrigo, M. (2013). Effects of a mindfulness-based intervention on psychological distress, well-being, and maternal self-efficacy in breast-feeding mothers: results of a pilot study. Archives of Women's Mental Health, 16(3), 227–236. https://doi.org/10.1007/s00737-013-0337-z.
Perez-Blasco, J., Sales, A., Meléndez, J. C., & Mayordomo, T. (2016). The effects of mindfulness and self-compassion on improving the capacity to adapt to stress situations in elderly people living in the community. Clinical Gerontologist, 39(2), 90–103. https://doi.org/10.1080/07317115.2015.1120253.
Pfattheicher, S., Geiger, M., Hartung, J., Weiss, S., & Schindler, S. (2017). Old wine in new bottles? The case of self-compassion and neuroticism. European Journal of Personality, 31(2), 160–169. https://doi.org/10.1002/per.2097.
Przezdziecki, A., & Sherman, K. A. (2016). Modifying affective and cognitive responses regarding body image difficulties in breast cancer survivors using a self-compassion-based writing intervention. Mindfulness, 7(5), 1142–1155. https://doi.org/10.1007/s12671-016-0557-1.
Puterman, E., DeLongis, A., & Pomaki, G. (2010). Protecting us from ourselves: social support as a buffer of trait and state rumination. Journal of Social and Clinical Psychology, 29(7), 797–820.
Raes, F., Pommier, E., Neff, K. D., & Van Gucht, D. (2011). Construction and factorial validation of a short form of the self-compassion scale. Clinical Psychology and Psychotherapy, 18(3), 250–255. https://doi.org/10.1002/cpp.702.
Richardson, D. A., Jaber, S., Chan, S., Jesse, M. T., Kaur, H., & Sangha, R. (2016). Self-compassion and empathy: impact on burnout and secondary traumatic stress in medical training. Open Journal of Epidemiology, 6(03), 167. https://doi.org/10.4236/ojepi.2016.63017.
Ritzert, T. R., Forsyth, J. P., Sheppard, S. C., Boswell, J. F., Berghoff, C. R., & Eifert, G. H. (2016). Evaluating the effectiveness of ACT for anxiety disorders in a self-help context: outcomes from a randomized wait-list controlled trial. Behavior Therapy, 47(4), 444–459. https://doi.org/10.1016/j.beth.2016.03.001.
Rosenthal, R. (1995). Writing meta-analytic reviews. Psychological Bulletin, 118(2), 183. https://doi.org/10.1037/0033-2909.118.2.183.
Smeets, E., Neff, K., Alberts, H., & Peters, M. (2014). Meeting suffering with kindness: effects of a brief self-compassion intervention for female college students. Journal of Clinical Psychology, 70(9), 794–807. https://doi.org/10.1002/jclp.22076.
Svendsen, J. L., Kvernenes, K. V., Wiker, A. S., & Dundas, I. (2017). Mechanisms of mindfulness: rumination and self-compassion. Nordic Psychology, 69(2), 71–82. https://doi.org/10.1080/19012276.2016.1171730.
Wong, C. C., & Mak, W. W. (2016). Writing can heal: effects of self-compassion writing among Hong Kong Chinese college students. Asian American Journal of Psychology, 7(1), 74–82. https://doi.org/10.1037/aap0000041.
Wren, A. A., Somers, T. J., Wright, M. A., Goetz, M. C., Leary, M. R., Fras, A. M., et al. (2012). Self-compassion in patients with persistent musculoskeletal pain: relationship of self-compassion to adjustment to persistent pain. Journal of Pain and Symptom Management, 43(4), 759–770. https://doi.org/10.1016/j.jpainsymman.2011.04.014.
Yadavaia, J. E., Hayes, S. C., & Vilardaga, R. (2014). Using acceptance and commitment therapy to increase self-compassion: a randomized controlled trial. Journal of Contextual Behavioral Science, 3(4), 248–257. https://doi.org/10.1016/j.jcbs.2014.09.002.
Yang, X., & Mak, W. W. (2017). The differential moderating roles of self-compassion and mindfulness in self-stigma and well-being among people living with mental illness or HIV. Mindfulness, 8(3), 595–602. https://doi.org/10.1007/s12671-016-0635-4.
Zeng, X., Chiu, C. P., Wang, R., Oei, T. P., & Leung, F. Y. (2015). The effect of loving-kindness meditation on positive emotions: a meta-analytic review. Frontiers in Psychology, 6. https://doi.org/10.3389/fpsyg.2015.01693.
Zessin, U., Dickhäuser, O., & Garbade, S. (2015). The relationship between self-compassion and well-being: a meta-analysis. Applied Psychology: Health and Well-Being, 7(3), 340–364. https://doi.org/10.1111/aphw.12051.
Author information
Authors and Affiliations
Contributions
MF designed and executed the study, conducted the analyses and interpretation and wrote the manuscript. CH collaborated with the design and proof editing of the paper. AH contributed to literature searches and data extraction and management. MA contributed to proof editing of the paper. AB contributed to statistical analyses interpretation and proof editing the paper. DE collaborated with the design and proof editing of the paper.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics
The research reported here was conducted in an ethical and responsible manner. As a meta-analysis, approval from a human research ethics committee was not required.
Data Availability Statement
The data file is made available in the supplementary materials for this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ferrari, M., Hunt, C., Harrysunker, A. et al. Self-Compassion Interventions and Psychosocial Outcomes: a Meta-Analysis of RCTs. Mindfulness 10, 1455–1473 (2019). https://doi.org/10.1007/s12671-019-01134-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-019-01134-6