Abstract
A key challenge for people who struggle with major depressive disorder (MDD) is the prevention of recurrence, given that the risk of recurrence increases significantly with each episode. Recently, it has been suggested that low levels of self-compassion may be an enduring risk factor for depression recurrence; however, surprisingly little research has examined the pathways through which self-compassion and recurrent depressive symptoms are linked. Thus, our study examined how self-compassion may be protective in the recurrence of depressive symptoms through four emotion regulation strategies associated with depression: brooding rumination, experiential avoidance, cognitive reappraisal, and acceptance. A sample of 100 participants with a history of recurrent depression were recruited using Amazon’s Mechanical Turk (MTurk). Simple and multiple mediation analyses were conducted. Results from the simple mediation models indicated that higher levels of self-compassion were associated with lower depressive symptoms through brooding rumination, experiential avoidance, and acceptance, while cognitive reappraisal did not mediate the relation. The multiple mediation model revealed that brooding rumination was the only significant mediator, when controlling for other emotion regulation strategy variables. Theoretical implications are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A crucial challenge in the treatment of major depressive disorder (MDD) is depression recurrence (Bockting et al. 2015). Estimates indicate that 40 to 60% of people who experience a major depressive episode (MDE) will suffer another episode. Furthermore, with each successive episode, the chance of recurrence increases significantly (Bockting et al. 2015; Bulloch et al. 2014); it has been suggested that among people with three or more episodes, 90% will experience recurrent episodes (Monroe and Harkness 2011). Given the significance of MDD, and specifically its recurrent nature, better understanding of what protects against depression recurrence is important for informing and improving targeted interventions for depression (Bockting et al. 2015).
Self-compassion has received substantial attention among researchers and clinicians due to its potential function as a protective factor against depression, with robust associations between these constructs (Finlay-Jones 2017; MacBeth and Gumley 2012). Given that self-compassion involves how a person relates to oneself during times of distress, it has been suggested that emotion regulation may be a potential mechanism through which self-compassion operates (Finlay-Jones 2017).
Self-compassion has been described as a way of relating with kindness to oneself in times of suffering or failure (Neff 2003a) and consists of three inter-related components (Neff 2011; Neff 2016; Neff et al. 2007). Each element has a positive and negative pole, characterizing compassionate and uncompassionate responses towards oneself in times of suffering or difficulty: (a) self-kindness versus self-judgment, (b) common humanity versus isolation, and (c) mindfulness versus over-identification (Neff 2003a; Neff 2016). While mindfulness is a key component of self-compassion, in the context of self-compassion, mindfulness relates more specifically to an awareness of negative experiences, rather than awareness of all experiences (see Neff and Dahm 2015). As such, mindfulness is narrower in scope in the context of self-compassion. Furthermore, the construct of self-compassion includes the elements of kindness towards the self and relating experiences to part of being human, which differs from mindfulness alone.
Self-compassion appears to be a robust protective factor against depressive symptoms, with strong empirical support for a negative association between self-compassion and depressive symptoms found in both cross-sectional and longitudinal studies (e.g., MacBeth and Gumley 2012; Neff 2003a; Neff et al. 2007; Raes 2010; Raes 2011; Wong and Mak 2012). Recently, researchers have begun to examine self-compassion and its relationship to clinical depression. Research with clinical samples is in its infancy, but research has shown that patients with MDD have lower levels of self-compassion than those who have never experienced depression (Diedrich et al. 2016b; Krieger et al. 2013; Krieger et al. 2016). Importantly, a recent longitudinal study used a cross-lagged panel analysis to demonstrate that depressive symptoms were predicted by decreased levels of self-compassion, while depressive symptoms did not predict lower levels of self-compassion, at 6 months and 12 months in a group of outpatients who had previously been treated for clinical depression (Krieger et al. 2016). These findings indicate that low levels of self-compassion may place people at higher risk for depression, rather than being the result of depressive symptomatology.
Developing self-compassion may be especially important for those who are vulnerable to recurrent depressive symptoms (Ehret et al. 2014). Research has indicated that there is a change that results from an initial episode of depression, which is long-lasting, and puts people at risk for subsequent recurrent episodes (Burcusa and Iacono 2007; Teasdale 1988). Cognitive scar theories suggest that there are changes at both cognitive and neuronal levels that result from an initial episode of depression. With repeated MDEs, there is a stronger association between low mood and negative thinking patterns (Segal et al. 2012; Teasdale 1988; Teasdale et al. 2000). This association leads to the development of MDEs more easily with each episode, as mild stress or negative mood states trigger depressogenic cognitive processes (e.g., rumination); thus, there is a lower threshold to the progression of a full MDE (Elgersma et al. 2015). As such, understanding how self-compassion operates in people with recurrent depression and how it influences depression’s cyclical pattern, is important.
Self-compassion may protect against recurrent depression by attenuating negative thinking patterns and low moods. Being self-compassionate may facilitate breaking the lowered threshold of depressogenic responses to distress that are typical of recurrent depression. Recently, low self-compassion has been identified as a possible enduring risk factor for depression recurrence (Ehret et al. 2014). Lower levels of self-compassion have been observed in people with remitted depression when compared to never-depressed control groups. In addition, self-criticism, which may be indicative of low levels of self-compassion, has been identified as an enduring vulnerability factor in depression relapse and recurrence (Ehret et al. 2014; Joeng and Turner 2015). Having decreased self-compassion may be an ongoing risk factor in the development of further episodes of depression once people are in remission, and therefore bolstering the capacity to be self-compassionate could be important in the prevention of recurrent depressive symptoms (Ehret et al. 2014; Raes 2011).
While self-compassion has consistently been linked with depression, there is surprisingly little understanding of the pathways (i.e., mediators) through which they are linked. One suggested pathway is emotion regulation (Finlay-Jones 2017). Emotion regulation has been defined as the use of automatic and strategic processes to modify the occurrence, intensity, duration, or expression of an emotional response (Gross 2014). Difficulty with emotion regulation has been identified as a predictive and maintaining factor in depression (Aldao et al. 2010; Berking et al. 2014; Ehring et al. 2008). Emotion regulation deficits, specifically related to down regulating negative affect, have been posited to be at the core of mood disorders (Hofmann et al. 2012). Being unable to effectively regulate emotional responses to everyday events or emotional experiences may lead to more persistent and severe periods of distress, which can evolve into negative mood states or MDD (Berking and Whitley 2014; Nolen-Hoeksema et al. 2008).
Given that self-compassion involves a shift in how one relates to painful experiences and negative emotion (Neff 2003a), it would seem to follow that people who are higher in self-compassion may be able to regulate these emotions more effectively, leading to less depressive symptoms. Self-compassion may operate by impacting specific emotion regulation strategies that those who are vulnerable to depression recurrence tend to over- or under-utilize (Finlay-Jones 2017), such as by decreasing the tendency to use maladaptive emotion regulation strategies and/or bolstering the use of adaptive ones. Self-compassion has been found to be inversely related to difficulty with emotion regulation, resulting in decreased depressive symptoms (Finlay-Jones et al. 2015; Finlay-Jones 2017; Krieger et al. 2013; Raes 2010). Meta-analytic evidence has indicated which emotion regulation strategies—rumination, experiential avoidance, cognitive reappraisal, and acceptance—have been most strongly associated with depression (Aldao et al. 2010). In sum, these four emotion regulation strategies may explain the association between self-compassion and recurrent depressive symptoms, and as such warrant further exploration.
One way that self-compassion may protect against recurrent depressive symptoms is by reducing the tendency to ruminate in response to negative affect. Brooding rumination, the tendency to have repetitive and frequent negative thoughts, which are often self-critical in nature, is the type of rumination most frequently associated with depressive symptoms (Treynor et al. 2003). It involves over-engagement with negative thought patterns in an attempt to reduce or control unwanted emotions (Desrosiers et al. 2013). Rumination exacerbates distress by increasing the impact of negative moods on thoughts used to understand current circumstances, creating cyclical depressogenic thinking patterns that can develop into an MDE (see Aldao and Nolen-Hoeksema 2010; Nolen-Hoeksema et al. 2008). Self-compassion helps people to hold negative thoughts and emotions in mindful and non-judgmental awareness, and not fixate on them (Neff 2011). Additionally, self-compassion likely facilitates having a compassionate and soothing response to suffering, instead of having a self-critical or blaming response, which is common with rumination (Nolen-Hoeksema et al. 2008). Thus, being more self-compassionate may impede the cycle of rumination and worsening depressive symptoms.
A second way that self-compassion may protect against recurrent depressive symptoms is by changing people’s tendency to engage in experiential avoidance. Experiential avoidance is an unwillingness or aversion to experiencing difficult or negatively evaluated emotions, thoughts, or physical sensations (Hayes et al. 2006; Hofmann et al. 2012). Avoidance of negative emotions or distress, which is often related to fear of experiencing unwanted emotions, can lead to further negative affect, anhedonia, and depressive symptoms (Beblo et al. 2012). While avoidance may be initially protective or adaptive in that people do not experience immediate pain or distress, over time avoidance can become maladaptive, leading to worsening symptoms (Hayes et al. 2006) and long-term emotional difficulties (Gámez et al. 2011; Hofmann et al. 2012). One effective approach that has been found to counter experiential avoidance is mindfulness. Mindfulness facilitates de-identifying with painful thoughts (Hofmann et al. 2012) and is one of the facets of self-compassion that encourages people to turn towards, instead of avoid, distress. In this way, self-compassion may foster an ability to adopt a new perspective of distress, one of self-kindness and non-judgment, and may increase people’s willingness to face unwanted thoughts, experiences, and emotions, instead of avoiding them. Because experiential avoidance relates to people’s relationship with distress (Gámez et al. 2011), shifting this through self-compassion may foster a more adaptive relationship to negative emotions.
A third way that self-compassion may protect against recurrent depression is by bolstering people’s capacity to use cognitive reappraisal. Cognitive reappraisal is reframing an experience to regulate emotional distress (Desrosiers et al. 2013) and to change the emotional impact of distressing events by shifting negative cognitive biases (Gross and John 2003). Cognitive reappraisal is an adaptive emotion regulation strategy and has been associated with reductions in depressive symptoms (Aldao et al. 2010). Self-compassion involves being able to view negative emotions or experiences as part of being human (i.e., common humanity), which is a change in perspective that is hypothesized to reduce feelings of disconnection and isolation (Finlay-Jones et al. 2015). The concept of self-compassion also involves a shifting or reframing of people’s relationship to an emotional experience, with increased mindfulness and self-kindness, and it could be that this non-judgmental reappraisal or reframing leads to reductions in depressive symptoms (Desrosiers et al. 2013; Neff 2003b). Some research has indicated that those who are more self-compassionate use more accurate appraisals of their self-evaluations (Leary et al. 2007). It has been proposed that those with high self-compassion think about distressing events in a way that reduces their negative impact (Allen and Leary 2010; Leary et al. 2007). A recent experimental study demonstrated that using explicit self-compassion prior to utilizing cognitive reappraisal was more effective in reducing depressive symptoms than cognitive reappraisal alone in a sample of people with depression (Diedrich et al. 2016a).
Lastly, self-compassion may be protective for recurrent depressive symptoms by enhancing acceptance of distress. Acceptance is the willingness to experience emotions or other sensations without a need to alter or suppress them (Bond et al. 2011; Hayes et al. 2006). Having more acceptance of emotions when faced with distress allows people to acknowledge unwanted feelings or thoughts, instead of reverting to automatic or habitual patterns that may perpetuate depressive symptoms (Segal et al. 2012). This presents the choice of different skillful responses to situations, feelings, or thoughts. Acceptance of emotions has been negatively associated with the development of depressive symptoms (Berking et al. 2014). Furthermore, research has suggested that people who have experienced clinical depression and are vulnerable to depression recurrence have less acceptance of negative emotions (Ehring et al. 2008). Within mindfulness approaches to treating depression, one key target is the non-judgmental acceptance of emotional experiences (Aldao and Nolen-Hoeksema 2010), and self-compassion may foster a more mindful and accepting approach to negative emotions.
In the present study, we investigated whether four emotion regulation strategies that have been linked with depression mediated the association between self-compassion and depressive symptoms in a sample of adults with recurrent depression. This study explored two maladaptive emotion regulation strategies—rumination and experiential avoidance—and two adaptive emotion regulation strategies —acceptance and cognitive reappraisal—as possible mediators. These relations were investigated through both simple mediation and parallel multiple mediation analyses. Overall, we expected that higher levels of self-compassion would be associated with lower levels of depressive symptoms. We hypothesized that: (H1) brooding rumination, (H2) experiential avoidance, (H3) cognitive reappraisal, and (H4) acceptance would mediate the relation between self-compassion and depressive symptoms. Lastly, we hypothesized that (H5) in a parallel multiple mediation model, each of the four above emotion regulation strategies would mediate the relation between self-compassion and depressive symptoms, while controlling for the other emotion regulation strategies.
Method
Participants
A total of 887 people completed the initial screening questionnaire, and 105 met the inclusion and exclusion criteria. Of those who met the criteria, five chose not to participate. Participants (N = 100) were 70% women, 29% men, and 1% transgender; the mean age was 38.55 years (SD = 12.06), with a range of 21 to 66 years, and were mostly Caucasian (80%), Hispanic (7%), and East Asian (7%). The reported number of lifetime depressive episodes ranged from 2 to greater than 10, with 50% of participants reporting 2 to 3 lifetime episodes, 17% reporting 4 to 5 episodes, and 33% reporting over 6 episodes.
Procedure
Participants were recruited from Amazon’s Mechanical Turk (MTurk; https://www.mturk.com), an online crowdsourcing service through which people complete Human Intelligence Tasks (HITs) in exchange for monetary stipends. A benefit of using MTurk includes access to hard-to-reach populations, including people with psychological concerns who may not have sought support from mental health professionals (Shapiro et al. 2013). Research has indicated that studying clinical populations via MTurk is useful and efficient (Chandler and Shapiro 2016; Shapiro et al. 2013). Following recommendations for clinical research using MTurk (e.g., Chandler and Shapiro 2016), participants were recruited through a posting on MTurk with a vague description of the study, to avoid misrepresentation or malingering. To participate, MTurk worker qualifications requirements were set to the following: US location, HIT approval rate greater than 95%, and number of HITs approved greater than 1000.
Ethics approval was obtained prior to conducting the study. Upon completion of the informed consent, participants were invited to complete the screening measures. Once completed, surveys were reviewed to determine if participants met the inclusion and exclusion criteria. Criteria for inclusion were as follows: 19 years of age or older (the legal age of adulthood where the study was conducted), at least two previous reported MDEs with a remission period of at least 2 months, and fluency in English. Exclusion criteria included the following: any indication of a previous episode of mania or hypomania, and/or any symptoms of psychosis. All participants who met these criteria were invited to participate in the full study on MTurk, and again completed informed consent prior to completing the measures online. A debriefing page was provided at the end of the survey, containing resources for participants who felt that they needed additional support, information, or crisis intervention. To assess for consistent reporting and truthfulness, participants were asked to report their location, and this information was cross-referenced with their IP address. Additionally, participants completed a simple mathematical problem to discourage spamming and check attention (Mason and Suri 2012). The screening and full study were matched and checked to ensure that the reported location, age, and MTurk ID matched.
Measures
Recurrent Depression
The Patient Health Questionnaire-9 (PHQ-9; Spitzer et al. 1999) was used to determine whether the worst reported lifetime depressive episode met criteria for an MDE. The PHQ-9 is a self-report tool that measures the presence and severity of the nine DSM-5 criterion A symptoms for an MDE. These symptoms include depressed mood, loss of interest or pleasure (anhedonia), significant appetite or weight changes, sleep disturbances, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness or guilt, difficulty concentrating, and suicidal ideation or attempt (APA 2013). The PHQ-9 has been validated for use as a brief assessment of lifetime major depression (Cannon et al. 2007). The instructions were changed to read: “For the 2 weeks in your life that you were the most blue, sad, or depressed, how often were you bothered by any of the following problems?” Each of the nine items were rated on a scale from 0 (not at all) to 4 (nearly every day). There was also a question to assess for criterion B: clinically significant impairment (i.e., “How difficult have these problems made it for you to do your work, take care of the things at home, or get along with other people?”). For items 1–8, we used a threshold for a positive symptom of 2 (more than half the days) instead of 3 (nearly every day), which has been found to significantly raise the sensitivity of the measure, while preserving a high specificity (Kroenke et al. 2001). Item 9 relates to suicidal ideation, and a score of 1 was categorized as a positive symptom (Cannon et al. 2007). These guidelines for scoring were used to determine if the participant met the cutoff criteria of at least five symptoms, including one of the two required symptoms for a DSM-5 diagnosis of an MDE (depressed mood or anhedonia). Cronbach’s alpha in the current study was 0.85.
Three additional questions were included to assess the MDE criteria not measured by the PHQ-9 for lifetime depression: criteria C, D, and E. These screening questions were drawn from the Composite International Diagnostic Interview (CIDI) and DSM-5 criteria. DSM-5 criterion C, which necessitates that the episode is not caused by a medical condition or substance use, was screened for using the question: “Was the episode you just described due to the influence of medication, drugs, or alcohol, or another medical condition?” Criterion D, which stipulates that the possibility of psychosis or a psychotic disorder must be ruled out, was screened for using three questions (e.g., “Did you ever have a time when you felt that your mind was being taken over by others?”). Three questions assessed for the possibility of a previous hypomanic/manic episode (e.g., “Have there been times, lasting at least a few days, when you felt the opposite of depressed, when you were very cheerful or happy and this felt different from your normal self?”), and addressed criterion E (that there has never been an episode of hypomania or mania). Lastly, one question assessed whether the episode was related to grief: “At the time of that episode, were you grieving for a person, or a pet, who had died in the past 2 months?”
The screening question for recurrence of depression, as well as lifetime number of episodes, was based upon the DSM-5 criteria requiring a period of at least 2 months with no significant signs or symptoms of depression: “How many SEPARATE times (with at least 2 months in between with no significant signs and symptoms) in your life have you felt sad, empty, or depressed most of the day, nearly every day, for at least 2 weeks?”
Current Depressive Symptoms
The Beck Depression Inventory-II (BDI-II; Beck et al. 1996) is a 21-item self-report measure used to measure current depressive symptom severity. Items (e.g., sadness) were rated from 0 (I do not feel sad) to 3 (I am so sad or unhappy that I cannot stand it), to indicate how respondents had been feeling during the previous 2 weeks. Higher scores indicated greater depressive symptom severity. Cronbach’s alpha for the present study was 0.92.
Self-Compassion
The Self-Compassion Scale (SCS; Neff 2003b) is a 26-item self-report measure of how self-compassionately respondents act towards themselves in times of difficulty. The SCS measures six dimensions of self-compassion, which encompass the compassionate versus uncompassionate ways that people respond along three elements, and which synergistically interact to provide a measure of overall self-compassion (Neff et al. 2017). These include self-kindness (e.g., “When I’m going through a very hard time, I give myself the caring and tenderness I need”), common humanity (e.g., “When I’m down and out, I remind myself that there are lots of other people in the world feeling like I am”), mindfulness (e.g., “When I’m feeling down I try to approach my feelings with curiosity and openness”), self-judgment (e.g., “I’m disapproving and judgmental about my own flaws and inadequacies”), isolation (e.g., “When I think about my inadequacies, it tends to make me feel more separate and cut off from the rest of the world”), and over-identification (e.g., “When I’m feeling down I tend to obsess and fixate on everything that’s wrong”). Items were rated on a 5-point scale from 1 (almost never) to 5 (almost always), and negatively worded items were reverse scored (Neff 2003b). We used the total SCS score and higher scores indicated more self-compassion. Recent empirical work examining the factor structure of the SCS indicated that utilizing a total SCS score is both theoretically and psychometrically supported as a measure of self-compassion (see Neff 2016; Neff et al. 2017). Strong psychometric support for the SCS total score has been found across several other studies (Joeng and Turner 2015; Krieger et al. 2013; Neff et al. 2007). Cronbach’s alpha in the present study was 0.95.
Brooding Rumination
The Ruminative Responses Scale (RRS; Treynor et al. 2003) is a self-report measure of rumination. In the current study, we used the brooding rumination subscale, which measures the tendency to have repetitive negative thoughts. This subscale has five items to which respondents indicated how often they think or do things when they feel depressed (e.g., “Think: Why do I have problems other people don’t have?”), with responses ranging from 1 (never) to 4 (always). Higher scores reflected higher levels of brooding rumination. The Cronbach’s alpha for the present sample was 0.77.
Experiential Avoidance
The Brief Experiential Avoidance Questionnaire (BEAQ; Gámez et al. 2013) is a 15-item self-report measure of experiential avoidance, which is the tendency to avoid distressing emotions, thoughts, or physical sensations (e.g., “I work hard to keep out upsetting feelings”). Items are rated by respondents from 1 (strongly disagree) to 6 (strongly agree), with higher scores indicating greater experiential avoidance. The Cronbach’s alpha in the present sample was 0.83.
Cognitive Reappraisal
The cognitive reappraisal subscale of the Emotion Regulation Questionnaire (ERQ; Gross and John 2003) was used to measure cognitive reappraisal or the ability to reframe distressing emotional experiences in a more positive way. This subscale consists of six items (e.g., “I control my emotions by changing the way I think about the situation I’m in”). Respondents indicated their agreement with each statement from 1 (strongly disagree) to 7 (strongly agree) to denote how much they used a specific strategy to manage their emotions. A higher score reflected greater use of cognitive reappraisal. Cronbach’s alpha in the present sample was 0.90.
Acceptance
The six-item non-acceptance of emotional responses subscale of the Difficulties in Emotion Regulation Scale (DERS; Gratz and Roemer 2004) was used to measure how accepting respondents were of their negative emotions. The items (e.g., “When I’m upset, I feel ashamed at myself for feeling that way”) were measured on a scale from 1 (almost never) to 5 (almost always). Items were reverse scored and higher scores indicated greater emotional acceptance. Cronbach’s alpha in the present sample was 0.93.
Data Analyses
The statistical method described by Preacher and Hayes (2008) was used to investigate the mediating effects of rumination, experiential avoidance, cognitive reappraisal, and acceptance on the relationship between self-compassion and depressive symptoms. Data analyses were conducted using SPSS version 24.0, and the PROCESS macro for SPSS (Hayes 2013), model number 4. Bootstrapping was utilized in the mediation analyses, which is a resampling procedure that does not force the assumption of normality for the sampling distribution of the indirect (i.e., mediating) effect (Preacher and Hayes 2008). Instead, the distribution is constructed empirically. From this generated sampling distribution, 95% confidence intervals are constructed to test the indirect effects, which are considered significant if zero does not fall between the upper and lower confidence intervals (Preacher and Hayes 2008). In this study, the bootstrapped confidence intervals for the indirect effects were based on 10,000 resamples. The percent mediation was calculated for each indirect effect, which indicated what percentage of the association between self-compassion and depressive symptoms was accounted for by the mediator.
First, we conducted four simple mediation analyses to test the indirect effects between self-compassion and depressive symptoms through each mediating variable (i.e., rumination, experiential avoidance, acceptance, and cognitive reappraisal). Second, we tested a parallel multiple mediation model to examine the indirect effects of each mediating variable, while controlling for the other mediators (Hayes 2013). The direct and indirect effects were standardized, using z-scores, to facilitate comparisons within and between the models.
Results
Preliminary Analyses
First, data were screened for missingness. Twenty-eight (0.35%) item responses were missing and imputed using the expectation maximization algorithm (Tabachnick and Fidell 2013). Next, the data were screened for univariate and multivariate outliers using boxplots, scatterplots, and Mahalanobis distance. No meaningful outliers were noted. All distributions of scales demonstrated normality. Descriptive statistics and correlations for all study variables were explored and are presented in Table 1. All study variables significantly correlated with each other in the expected directions. Self-compassion showed a moderate negative association with depressive symptoms (r = − 0.57, p < 0.001), as expected.
Simple Mediation Models
To examine if the four emotion regulation strategies mediated the association between self-compassion and depressive symptoms without controlling for the other emotion regulation strategies, we ran four simple mediation models (see Table 2). Supporting our first hypothesis, brooding rumination significantly mediated the link between self-compassion and depressive symptoms, b = − 0.16, 95% CI [− 0.30, − 0.07]. Brooding rumination accounted for 28% of the relation between self-compassion and depressive symptoms. Supporting hypothesis two, experiential avoidance significantly mediated the association between self-compassion and depressive symptoms, b = − 0.10, 95% CI [− 0.22, − 0.03]. Experiential avoidance accounted for 18% of the link between self-compassion and depressive symptoms. Inconsistent with hypothesis three, cognitive reappraisal did not significantly mediate the relation between self-compassion and depressive symptoms, b = − 0.07, 95% CI [− 0.21, 0.03]. Lastly, consistent with hypothesis four, acceptance significantly mediated the link between self-compassion and depressive symptoms, b = − 0.09, 95% CI [− 0.20, − 0.02]. Acceptance accounted for 20% of the association between self-compassion and depressive symptoms.
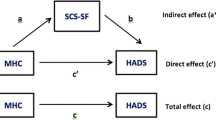
Multiple Mediation Model
To examine the mediating effects of each of the emotion regulation strategies, while controlling for the other emotion regulation strategies, we used a multiple mediation model. Because cognitive reappraisal did not mediate the relation between self-compassion and depressive symptoms in the simple mediation model, cognitive reappraisal was not included in the multiple mediation model (see Fig. 1). When brooding rumination, experiential avoidance, and acceptance were included, only brooding rumination significantly mediated the link between self-compassion and depressive symptoms, b = − 0.12, 95% CI [− 0.24, − 0.03] (see Table 3). Brooding rumination accounted for 21% of the association between self-compassion and depressive symptoms. This was only partially consistent with hypothesis five, in that only one of the maladaptive emotion regulation strategies was a significant mediator.
Next, we re-ran our multiple mediation model using only the positive subscales on the SCS (i.e., self-kindness, mindfulness, and common humanity). Some have argued (e.g., Muris et al. 2016; Muris et al. 2018) that the SCS negative scales conceptually overlap with psychopathology and related constructs (e.g., rumination). By running the same multiple mediation model without the negative SCS scales, we can evaluate if our findings maintained without potentially conceptually overlapping scales. The overall association between self-compassion and depressive symptoms was slightly weaker, however remained moderately negatively correlated (r = − 0.47, p < 0.001). Importantly, consistent with our initial multiple-mediation model, brooding rumination significantly mediated the link between self-compassion (as measured by the three positive subscales) and depressive symptoms, b = − 0.07, 95% CI [− 0.19, − 0.01], while experiential avoidance, b = − 0.04, 95% CI [− 0.13, 0.01] and acceptance, b = − 0.04, 95% CI [− 0.11, 0.01] did not. Brooding rumination accounted for 16% of the association between self-compassion (positive scales) and depressive symptoms. These results indicate that whether the total SCS score or the score of solely the positive subscales were used, brooding rumination was the strongest mediator between self-compassion and depressive symptoms in our sample. In keeping with our initial study operationalization of self-compassion, we elected to retain Neff’s conceptualization of an overall level of self-compassion, utilizing the total SCS score (see Neff et al. 2017; Neff 2018) in our interpretation of the results.
Discussion
Given the heightened vulnerability to recurrence of depression in those who have experienced previous MDEs, understanding the processes through which recurrence occurs, and how it can be prevented, is important for helping this population. The current research was undertaken to add to our understanding of how self-compassion may operate as a protective factor for people at risk for depression recurrence. The overall aim of this study was to investigate whether four emotion regulation strategies (two adaptive and two maladaptive) mediated the relations between self-compassion and depressive symptoms in a sample with recurrent depression. Each potential mediator was first explored as an individual mechanism through simple mediation analyses. Subsequently, significant mediators were examined in a multiple mediation model in which the influence of the other mediating variables was controlled.
The simple mediation analyses revealed that brooding rumination, experiential avoidance, and acceptance each mediated the relation between self-compassion and depressive symptoms. Cognitive reappraisal did not mediate this relation. Subsequently, the parallel multiple mediation model revealed that only the indirect effect of self-compassion on depressive symptoms via brooding rumination was significant when controlling for the other mediators. Taken together, in adults with recurrent depression, while self-compassion appears to reduce depressive symptoms by lessening the tendency to ruminate in the face of negative affect or difficulty, by decreasing avoidance of emotional experiences, and by bolstering an acceptance of negative emotions, our findings suggest that the main emotion regulation pathway through which self-compassion may operate is through its influence on brooding rumination.
Results from the current study provide support for self-compassion being a protective factor for depressive symptom recurrence in people with a history of recurrent depression. Consistent with previous studies that have examined the relation between self-compassion and depressive symptoms in clinical samples (e.g., Diedrich et al. 2016b; Ehret et al. 2014; Krieger et al. 2013; Krieger et al. 2016), self-compassion was negatively associated with depressive symptoms (r = − 0.57). While prior research has pointed to decreased self-compassion in those with remitted depression (Ehret et al. 2014), the present study extends the literature by demonstrating that low levels of self-compassion are associated with greater depressive symptomatology in people with recurrent depression. It is important to note that our sample of people with recurrent depression likely included both people in remission as well as people who met criteria for a current major depressive episode. Although the current findings are cross-sectional, previous work has supported the proposed temporal order (Diedrich et al. 2016b; Krieger et al. 2016). It is still possible, however, that depression itself further impacts people’s ability to be self-compassionate, which subsequently puts them at increased risk for recurrent depression, similar to scar theories of recurrent depression. As such, future longitudinal research would be beneficial in unpacking this relation. Nevertheless, it seems clear that self-compassion plays a role in impacting depressive symptomatology (MacBeth and Gumley 2012), and our findings support this in recurrent depression.
Our findings extend the literature by demonstrating that an overall pathway through which self-compassion may impact depressive symptomatology in people with recurrent depression is through its influence on emotion regulation strategies. Our findings build on the limited, but emerging, clinical research, which suggests that having higher levels of self-compassion is protective in depression through its influence on people’s ability to regulate negative affect (Diedrich et al. 2016b; Finlay-Jones 2017; Krieger et al. 2013). The key pathway that emerged in our study was brooding rumination, which was found to be the only significant mediator when controlling others in a parallel multiple mediation model. Thus, it seems that high levels of self-compassion may reduce the tendency to engage in repetitive, self-critical thought, which is typical of brooding rumination. This, in turn, may lessen depressive symptomatology. When someone experiences stress or difficult emotions, self-compassion may serve as a way of relating to these experiences that interrupts the problematic loop of cyclical negative thoughts and emotions. This is important because rumination is a particularly problematic emotion regulation strategy that puts people at higher risk of developing subsequent episodes of depression (Joormann and Siemer 2014). Our findings are line with previous research in a non-clinical sample examining brooding rumination as a mediator between self-compassion and depressive symptoms (Raes 2010), as well as with a prior study of clinically depressed outpatients that identified symptom-focused rumination as a significant mediator (Krieger et al. 2013). Other studies have also found that self-compassion attenuates cyclical thinking patterns that result in other negative mental health outcomes (Fresnics and Borders 2017; Neff et al. 2007).
It is important to note that there is substantial debate surrounding the operationalization and measurement of self-compassion (e.g., Muris et al. 2016; Muris et al. 2018; Neff et al. 2017; Neff 2018). In particular, there is concern regarding the possible overlap between items on the SCS and aspects of psychopathology such as rumination, which could overinflate or blur these relations (Muris et al. 2016). In our study, brooding rumination remained a significant meditator even when we removed the possibly overlapping self-critical SCS items. While our findings did not substantially change with or without the self-critical items, it is important to be aware of the possible overlap between items on the SCS and aspects of psychopathology. Further examination of subscales on the SCS was beyond the scope of this particular study, however may elucidate important nuances in future research.
It is also important to note that, while not the dominant pathways in our multiple mediation model, experiential avoidance and acceptance significantly mediated the relation between self-compassion and depressive symptoms when tested individually. Our study demonstrated these relations in people with recurrent depression. These findings offer some novel insight into ways in which self-compassion impacts people’s ability to regulate their emotions, albeit less strongly than brooding rumination. Self-compassion seems to foster a more accepting approach to negative affect, as well as decrease the propensity to avoid uncomfortable emotions. By shifting these acceptance or avoidance tendencies, negative emotions are likely not propagated further. These findings fit with previous work which showed that cognitive and behavioral avoidance was a mechanism through which self-compassion influenced depressive symptoms (Krieger et al. 2013). However, our findings differed slightly from a previous study that showed that, while overall adaptive emotion regulation mediated the relation between self-compassion and depressive symptoms in a sample of patients with clinical depression, acceptance, when tested alone, did not (Diedrich et al. 2016b). It has been suggested that a lack of acceptance of emotions is a vulnerability to depression (Aldao et al. 2010; Ehring et al. 2008), and many acceptance or mindfulness-based interventions stem from the idea that non-judgmentally accepting one’s emotions shifts the power that emotions can have. Self-compassion comes from this same theoretical underpinning, and our findings fit within this theoretical paradigm of mental health and well-being.
An unexpected finding in our study was that cognitive reappraisal was not a significant mediator in the relation between self-compassion and depressive symptoms. This is inconsistent with recent experimental findings, which have demonstrated that the precursory use of self-compassion enhanced the explicit use of cognitive reappraisal to significantly reduce depressed mood in a clinically depressed sample (Diedrich et al. 2016a). In our study, the pathway between self-compassion and cognitive reappraisal was significant in the mediation model, indicating that high self-compassion may be associated with a greater ability to cognitively reappraise situations. However, the effect of cognitive reappraisal on depressive symptoms was not significant. This aligns with a number of previous studies, which have suggested that compared to other emotion regulation strategies, cognitive reappraisal is more inconsistently linked to depressive symptoms (Aldao et al. 2010; Joormann and Siemer 2014; Nezlek and Kuppens 2008). Findings from our study indicate that cognitive reappraisal may not play a large role in how self-compassion impacts depressive symptomatology in those with recurrent depressive symptoms. This may be because there are times when it is more adaptive to change the relationship towards inner experiences, including emotions, thoughts and physical sensations, as opposed to more traditional cognitive modification strategies (Ehring et al. 2008; Hayes et al. 2006; Teasdale 1999). So, it may be that this changing of the relationship to one’s experiences, through self-compassion, does not actually occur through cognitive reappraisal, and that it is more of a shift in how one relates to the experience (e.g., through acceptance) that impacts depressive symptoms. However, given the strong correlation in the present study between cognitive reappraisal and self-compassion, as well as recent experimental findings suggesting that self-compassion facilitates the use of cognitive reappraisal to decrease depressed mood (Diedrich et al. 2016a), clarification through future research is warranted.
Limitations and Future Directions
A number of limitations should be considered in our study. As mentioned, the data collected were cross-sectional and obtained through self-report measures. Additionally, our design did not include a control group. Given that we used self-report measures, it is possible that common method biases may have influenced the results (Podsakoff et al. 2003). Future research that uses other assessment methods such as clinical interviews or significant other reports would reduce some of the biases inherent to self-report measures. While our findings do fit with other longitudinal work that supports our model’s temporal order (Diedrich et al. 2016b; Krieger et al. 2016), we cannot definitively know the temporal sequence. Our model was hypothesized and tested based on theory and recent empirical findings; however, it is important to consider the possibility that self-compassion may mediate the relation between emotion regulation (e.g., brooding rumination) and depressive symptoms. Due to the cross-sectional nature of this study, the results may not accurately reflect mediation between the variables over time (Cole and Maxwell 2003). Given the possible biases in cross-sectional mediation analyses (Maxwell and Cole 2007), future research testing our model longitudinally is warranted and would provide a more nuanced understanding of these processes over time.
Another possible limitation may be related to the online assessment of participants. There is the possibility for careless or distracted responding, misunderstanding or misinterpreting questions, and malingering when completing studies online. In addition, we were not able to utilize a clinician-administered structured clinical diagnostic interview to verify that participants were accurately interpreting the screening questions for recurrent depression. That being said, recent research has suggested that MTurk participants are typically as honest as those recruited using other methods (Chandler and Shapiro 2016), and MTurk has been used effectively for research with clinical populations. Further, while we had a relatively large age range in our sample, participants did not include older adults and were predominantly female, Caucasian, and limited to residents of the USA; therefore, these demographics should be kept in mind when considering the results. Our research sheds light onto the relations among self-compassion, emotion regulation strategies, and depressive symptoms in this particular group, but future research would be necessary to determine whether the relations are similar in other groups.
Despite some of its limitations, the present research highlights some of the possible ways that self-compassion may operate in people with recurrent depressive symptoms. Future research can build upon this work and yield important information in considering clinical interventions that bolster self-compassion for the prevention and treatment of recurrent MDD. For example, existing programs related to self-compassion, such as Mindful Self-Compassion (Neff and Germer 2013) and Compassion Focused Therapy (Gilbert 2014), could be tested in samples with recurrent MDD. Furthermore, given the impact of self-compassion on emotion regulation, future research is warranted that examines other emotion regulation strategies that may account for the mental health benefits of self-compassion and their relations with other psychological disorders associated with emotion regulation difficulties. Ultimately, it seems that self-compassion is an important component of mental health in clinical populations, and research that continues to uncover its use in addressing psychological disorders, including recurrent depression, will be of great benefit.
References
Aldao, A., & Nolen-Hoeksema, S. (2010). Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research and Therapy, 48(10), 974–983. https://doi.org/10.1016/j.brat.2010.06.002.
Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. https://doi.org/10.1016/j.cpr.2009.11.004.
Allen, A. B., & Leary, M. R. (2010). Self-compassion, stress, and coping. Social and Personality Psychology Compass, 4(2), 107–118. https://doi.org/10.1111/j.1751-9004.2009.00246.x.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association.
Beblo, T., Fernando, S., Klocke, S., Griepenstroh, J., Aschenbrenner, S., & Driessen, M. (2012). Increased suppression of negative and positive emotions in major depression. Journal of Affective Disorders, 141(2–3), 474–479. https://doi.org/10.1016/j.jad.2012.03.019.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation.
Berking, M., & Whitley, B. (2014). Affect regulation training: A practitioners’ manual. New York: Springer.
Berking, M., Wirtz, C. M., Svaldi, J., & Hofmann, S. G. (2014). Emotion regulation predicts symptoms of depression over five years. Behaviour Research and Therapy, 57(1), 13–20. https://doi.org/10.1016/j.brat.2014.03.003.
Bockting, C., Hollon, S. D., Jarrett, R. B., Kuyken, W., & Dobson, K. (2015). A lifetime approach to major depressive disorder: The contributions of psychological interventions in preventing relapse and recurrence. Clinical Psychology Review, 41, 16–26. https://doi.org/10.1016/j.cpr.2015.02.003.
Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., Orcutt, H. K., et al. (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676–688. https://doi.org/10.1016/j.beth.2011.03.007.
Bulloch, A., Williams, J., Lavorato, D., & Patten, S. (2014). Recurrence of major depressive episodes is strongly dependent on the number of previous episodes. Depression and Anxiety, 31(1), 72–76. https://doi.org/10.1002/da.22173.
Burcusa, S. L., & Iacono, W. G. (2007). Risk for recurrence in depression. Clinical Psychology Review, 27(8), 959–985. https://doi.org/10.1016/j.cpr.2007.02.005.
Cannon, D. S., Tiffany, S. T., Coon, H., Scholand, M. B., McMahon, W. M., & Leppert, M. F. (2007). The PHQ-9 as a brief assessment of lifetime major depression. Psychological Assessment, 19(2), 247–251. https://doi.org/10.1037/1040-3590.19.2.247.
Chandler, J., & Shapiro, D. (2016). Conducting clinical research using crowdsourced convenience samples. Annual Review of Clinical Psychology, 12(1), 53–81. https://doi.org/10.1146/annurev-clinpsy-021815-093623.
Cole, D. A., & Maxwell, S. E. (2003). Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology, 112(4), 558 577. https://doi.org/10.1037/0021-843X.112.4.558.
Desrosiers, A., Vine, V., Klemanski, D. H., & Nolen-Hoeksema, S. (2013). Mindfulness and emotion regulation in depression and anxiety: Common and distinct mechanisms of action. Depression and Anxiety, 30(7), 654–661. https://doi.org/10.1002/da.22124.
Diedrich, A., Hofmann, S. G., Cuijpers, P., & Berking, M. (2016a). Self-compassion enhances the efficacy of explicit cognitive reappraisal as an emotion regulation strategy in individuals with major depressive disorder. Behaviour Research and Therapy, 82, 1–10. https://doi.org/10.1016/j.brat.2016.04.003.
Diedrich, A., Burger, J., Kirchner, M., & Berking, M. (2016b). Adaptive emotion regulation mediates the relationship between self-compassion and depression in individuals with unipolar depression. Psychology and Psychotherapy: Theory, Research and Practice, 1–17. https://doi.org/10.1111/papt.12107
Ehret, A. M., Joormann, J., & Berking, M. (2014). Examining risk and resilience factors for depression: The role of self-criticism and self-compassion. Cognition and Emotion, 29(8), 1496–1504. https://doi.org/10.1080/02699931.2014.992394.
Ehring, T., Fischer, S., Schnülle, J., Bösterling, A., & Tuschen-Caffier, B. (2008). Characteristics of emotion regulation in recovered depressed versus never depressed individuals. Personality and Individual Differences, 44(7), 1574–1584. https://doi.org/10.1016/j.paid.2008.01.013.
Elgersma, H. J., de Jong, P. J., van Rijsbergen, G. D., Kok, G. D., Burger, H., van der Does, W., et al. (2015). Cognitive reactivity, self-depressed associations, and the recurrence of depression. Journal of Affective Disorders, 183, 300–309. https://doi.org/10.1016/j.jad.2015.05.018.
Finlay-Jones, A. L. (2017). The relevance of self-compassion as an intervention target in mood and anxiety disorders: A narrative review based on an emotion regulation framework. Clinical Psychologist, 21(2), 90–103. https://doi.org/10.1111/cp.12131.
Finlay-Jones, A. L., Rees, C. S., & Kane, R. T. (2015). Self-compassion, emotion regulation and stress among Australian psychologists: Testing an emotion regulation model of self-compassion using structural equation modeling. PLoS One, 10(7), e0133481. https://doi.org/10.1371/journal.pone.0133481.
Fresnics, A., & Borders, A. (2017). Angry rumination mediates the unique associations between self-compassion and anger and aggression. Mindfulness, 8(3), 554–564. https://doi.org/10.1007/s12671-016-0629-2.
Gámez, W., Chmielewski, M., Kotov, R., Ruggero, C., & Watson, D. (2011). Development of a measure of experiential avoidance: The Multidimensional Experiential Avoidance Questionnaire. Psychological Assessment, 23(3), 692–713. https://doi.org/10.1037/a0023242.
Gámez, W., Chmielewski, M., Kotov, R., Ruggero, C., Suzuki, N., & Watson, D. (2013). The Brief Experiential Avoidance Questionnaire: Development and initial validation. Psychological Assessment, 26(1), 35–45. https://doi.org/10.1037/a0034473.
Gilbert, P. (2014). The origins and nature of compassion focused therapy. British Journal of Clinical Psychology, 53(1), 6–41. https://doi.org/10.1111/bjc.12043.
Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 1–54. https://doi.org/10.1023/B:JOBA.0000007455.08539.94.
Gross, J. (Ed.). (2014). Handbook of emotion regulation (Second ed.). New York: The Guilford Press.
Gross, J. J., & John, O. P. (2003). Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85(2), 348–362. https://doi.org/10.1037/0022-3514.85.2.348.
Hayes, A. F. (2013). The PROCESS macro for SPSS and SAS (version 2.13) [Software].
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. https://doi.org/10.1016/j.brat.2005.06.006.
Hofmann, S. G., Sawyer, A. T., Fang, A., & Asnaani, A. (2012). Emotion dysregulation model of mood and anxiety disorders. Depression and Anxiety, 29(5), 409–416. https://doi.org/10.1002/da.21888.
Joeng, J. R., & Turner, S. L. (2015). Mediators between self-criticism and depression: Fear of compassion, self-compassion, and importance to others. Journal of Counseling Psychology, 62(3), 453–463. https://doi.org/10.1037/cou0000071.
Joormann, J., & Siemer, M. (2014). Emotion regulation in mood disorders. In J. Gross (Ed.), Handbook of emotion regulation (pp. 413–427). New York: The Guilford Press.
Krieger, T., Altenstein, D., Baettig, I., Doerig, N., & Holtforth, M. G. (2013). Self-compassion in depression: Associations with depressive symptoms, rumination, and avoidance in depressed outpatients. Behavior Therapy, 44(3), 501–513. https://doi.org/10.1016/j.beth.2013.04.004.
Krieger, T., Berger, T., & Holtforth, M. (2016). The relationship of self-compassion and depression: Cross-lagged panel analyses in depressed patients after outpatient therapy. Journal of Affective Disorders, 202, 39–45. https://doi.org/10.1016/j.jad.2016.05.032.
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Leary, M. R., Tate, E. B., Adams, C. E., Batts Allen, A., & Hancock, J. (2007). Self-compassion and reactions to unpleasant self-relevant events: The implications of treating oneself kindly. Journal of Personality and Social Psychology, 92(5), 887–904. https://doi.org/10.1037/0022-3514.92.5.887.
MacBeth, A., & Gumley, A. (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32(6), 545–552. https://doi.org/10.1016/j.cpr.2012.06.003.
Mason, W., & Suri, S. (2012). Conducting behavioral research on Amazon’s mechanical Turk. Behavior Research Methods, 44(1), 1–23. https://doi.org/10.3758/s13428-011-0124-6.
Maxwell, S. E., & Cole, D. A. (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods, 12(1), 23–44. https://doi.org/10.1037/1082-989X.12.1.23.
Monroe, S. M., & Harkness, K. L. (2011). Recurrence in major depression: A conceptual analysis. Psychological Review, 118(4), 655–674. https://doi.org/10.1037/a0025190.
Muris, P., Otgaar, H., & Petrocchi, N. (2016). Protection as the mirror image of psychopathology: Further critical notes on the self-compassion scale. Mindfulness, 7, 787–790. https://doi.org/10.1007/s12671-016-0509-9.
Muris, P., Otgaar, H., & Pfattheicher, S. (2018). Stripping the forest from the rotten trees: Compassionate self-responding is a way of coping, but reduced uncompassionate self-responding mainly reflects psychopathology [Letter to the editor]. Mindfulness, 1–4. https://doi.org/10.1007/s12671-018-1030-0
Neff, K. D. (2003a). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(2), 85–101. https://doi.org/10.1080/15298860309032.
Neff, K. D. (2003b). The development and validation of a scale to measure self-compassion. Self and Identity, 2, 223–250. https://doi.org/10.1080/15298860309027.
Neff, K. D. (2011). Self-compassion, self-esteem, and well-being. Social and Personality Psychology Compass, 5(1), 1–12. https://doi.org/10.1111/j.1751-9004.2010.00330.x.
Neff, K. D. (2016). The Self-Compassion Scale is a valid and theoretically coherent measure of self-compassion. Mindfulness, 7(1), 264–274. https://doi.org/10.1007/s12671-015-0479-3.
Neff, K. D. (2018). Setting the record straight about the Self-Compassion Scale [Letter to the editor]. Mindfulness, 1–3. https://doi.org/10.1007/s12671-018-1061-6
Neff, K. D., & Dahm, K. A. (2015). Self-compassion: What it is, what it does, and how it relates to mindfulness. In B. Ostafin, M. Robinson, & B. Meier (Eds.), Handbook of mindfulness and self- regulation (pp. 121–137). New York: Springer. https://doi.org/10.1007/978-1-4939-2263-5_10.
Neff, K. D., & Germer, C. K. (2013). A pilot study and randomized controlled trial of the Mindful Self Compassion program. Journal of Clinical Psychology, 69(1), 28–44. https://doi.org/10.1002/jclp.21923.
Neff, K. D., Rude, S. S., & Kirkpatrick, K. L. (2007). An examination of self-compassion in relation to positive psychological functioning and personality traits. Journal of Research in Personality, 41(4), 908–916. https://doi.org/10.1016/j.jrp.2006.08.002.
Neff, K. D., Whittaker, T. A., & Karl, A. (2017). Examining the factor structure of the self-compassion scale in four distinct populations: Is the use of a total scale score justified? Journal of Personality Assessment, 99(6), 596–607. https://doi.org/10.1080/00223891.2016.1269334.
Nezlek, J. B., & Kuppens, P. (2008). Regulating positive and negative emotions in daily life. Journal of Personality, 76(3), 561–580. https://doi.org/10.1111/j.1467-6494.2008.00496.x.
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3(5), 400–424. https://doi.org/10.1111/j.1745-6924.2008.00088.x.
Podsakoff, P. M., MacKenzie, S. B., Lee, J. Y., & Podsakoff, N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88(5), 879–903. https://doi.org/10.1037/0021-9010.88.5.879.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. https://doi.org/10.3758/BRM.40.3.879.
Raes, F. (2010). Rumination and worry as mediators of the relationship between self-compassion and depression and anxiety. Personality and Individual Differences, 48(6), 757–761. https://doi.org/10.1016/j.paid.2010.01.023.
Raes, F. (2011). The effect of self-compassion on the development of depression symptoms in a non- clinical sample. Mindfulness, 2(1), 33–36. https://doi.org/10.1007/s12671-011-0040-y.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2012). Mindfulness-based cognitive therapy for depression (2nd ed.). New York: Guilford Press.
Shapiro, D. N., Chandler, J., & Mueller, P. A. (2013). Using Mechanical Turk to study clinical populations. Clinical Psychological Science, 1(2), 213–220. https://doi.org/10.1177/2167702612469015.
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & the Patient Health Questionnaire Primary Care Study Group. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA, 282(18), 1737–1744. https://doi.org/10.1001/jama.282.18.1737.
Tabachnick, B. G., & Fidell, L. S. (2013). Using multivariate statistics (6th ed.). Boston: Pearson Education.
Teasdale, J. D. (1988). Cognitive vulnerability to persistent depression. Cognition & Emotion, 2(3), 247–274. https://doi.org/10.1080/02699938808410927.
Teasdale, J. D. (1999). Emotional processing, three modes of mind and the prevention of relapse in depression. Behaviour Research and Therapy, 37(7), S53–S77. https://doi.org/10.1016/S0005-7967(99)00050-9.
Teasdale, J. D., Segal, Z. V., Williams, J. M., Ridgeway, V. A., Soulsby, J. M., & Lau, M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623. https://doi.org/10.1037/0022-006X.68.4.615.
Treynor, W., Gonzalez, R., & Nolen-Hoeksema, S. (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research, 27(3), 247–259. https://doi.org/10.1023/A:1023910315561.
Wong, C. C. Y., & Mak, W. W. S. (2012). Differentiating the role of three self-compassion components in buffering cognitive-personality vulnerability to depression among Chinese in Hong Kong. Journal of Counseling Psychology, 60(1), 162–169. https://doi.org/10.1037/a0030451.
Funding
This study was supported by the Canadian Institutes of Health Research (CIHR) in the form of a CGS-M Master’s Award awarded to the first author.
Author information
Authors and Affiliations
Contributions
AMB designed and executed the study, collected and analyzed the data, and wrote the paper. DWC collaborated with the design and writing of the study. AMH and RLW collaborated on the design of the study and edited the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Behavioural Research Ethics Board at the University of British Columbia and/or the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was obtained prior to conducting the study.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bakker, A.M., Cox, D.W., Hubley, A.M. et al. Emotion Regulation as a Mediator of Self-Compassion and Depressive Symptoms in Recurrent Depression. Mindfulness 10, 1169–1180 (2019). https://doi.org/10.1007/s12671-018-1072-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-018-1072-3