Abstract
Adults over the age of 65 years are now the fastest growing segment of the Canadian population. Although individual differences exist, aging is commonly associated with impairments in executive function and episodic memory. Previous studies have shown that mindfulness-based stress reduction (MBSR) can improve cognitive function in healthy younger adults, but no studies have yet examined this effect in older adults. The present study investigated the effectiveness of MBSR on improving executive function and episodic memory in older adult as well as its effectiveness in improving perceived stress and well-being. Ninety-seven healthy older adults were randomly assigned to either MBSR (n = 57) or an active control group (n = 40). It was hypothesized that compared with the control group, the MBSR group would display significant improvements in measures of executive function, episodic memory, mindfulness, mood, self-esteem, and quality of life. No clinically meaningful changes were found on any variable. In light of these results, the value of MBSR for this population is discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most significant consequences of aging is cognitive decline, with decays most often seen in memory, executive functions, processing speed, and reasoning (Deary et al. 2009). A decline in cognitive function is associated with reductions in functional status, independence, and overall quality of life (QOL). Executive functioning in particular is important in maintaining QOL because it enables individuals to successfully engage in independent, purposive, and self-serving behavior (Lezak et al. 2004). as long as executive functioning is intact, individuals with substantial cognitive impairment can still continue to be independent and productive (Lezak et al. 2004).
Declines in executive function in late life may have a number of detrimental effects. For instance, cross-sectional studies suggest that healthy community-dwelling older adults who perform poorly on tests of executive function have more difficulty completing instrumental activities of daily living than do older adults without executive impairment (Cahn-Weiner et al. 2000; Carlson et al. 1999; Grigsby et al. 1998). Longitudinal studies have corroborated these results, reporting that impairment in executive function is a reliable predictor of functional decline (Royall et al. 2004; Wang et al. 2002). The ability to perform instrumental daily activities is integral to one’s independence and quality of life (Cahn-Weiner et al. 2000). Thus, in order to ensure maintenance of executive function in late life, prevention is key.
Mindfulness-based stress reduction (MBSR), originally developed by Kabat-Zinn (1990). may contribute to healthy cognitive and psychological functioning in older adults. Mindfulness is defined as “moment-to-moment awareness” (Kabat-Zinn 1990, p. 2). It is cultivated by purposefully becoming aware of one’s thoughts and feelings in the present moment without judgment. MBSR is a program based on accepting thoughts, feelings, and behaviors that are difficult or impossible to change and encouraging metacognitive processes that emphasize experience of the present moment (Kabat-Zinn 1990). The standard MBSR program is an 8-week program that teaches participants to suppress the habitual tendency to automatically engage in, and respond to, evaluative and negative mental states (Kabat-Zinn 1990). Participants are encouraged to become aware of their emotions, cognitions, and behaviors with an interested, accepting, and nonjudgmental attitude (Segal et al. 2002). Eventually, this practice is believed to not only lead to change in actual thoughts and behaviors but also in the attitudes toward those thoughts and behaviors (Kabat-Zinn 1990). The cognitive mechanisms involved in mindfulness are hypothesized to be sustained attention (to maintain awareness of current experience), attention switching (to bring attention back to the present moment when it wanders), attentional inhibition (to avoid cognitive rumination), and non-directed attention (to enhance awareness of present experience, without assumptions or expectations; Bishop et al. 2004).
The efficacy of MBSR as a cost-effective stress management technique has been evaluated for over two decades in a variety of populations, including patients with chronic pain (Kabat-Zinn 1982), medical/premedical school students (Shapiro et al. 1998). cancer outpatients (Carlson et al. 2003; Speca et al. 2000). and healthy younger adults (Astin 1997; Klatt et al. 2008; Shapiro et al. 2007). Overall, these studies have shown MBSR to be efficacious in improving psychological well-being and various stress-related health outcomes in both clinical and healthy populations (Kabat-Zinn 1990). Specifically, beneficial effects have been reported for symptoms of general distress (Astin 1997; Carlson et al. 2003; Speca et al. 2000). worry, rumination, anxiety (Jain et al. 2007; Kabat-Zinn et al. 1992), depressive symptoms (Astin 1997; Shapiro et al. 1998; Speca et al. 2000). and quality of life (Brown and Ryan 2003; Carlson et al. 2003). Chiesa and Serretti (2009) conducted a literature review and meta-analysis of studies examining the relationship between MBSR and psychosocial outcomes in healthy populations. Only ten, mainly low-quality, studies were found. Results showed that relative to a waitlist control, MBSR was related to a significant reduction in stress and a significant enhancement in spirituality. Comparing MBSR to a relaxation-based control group, both treatments were equivalent in their ability to reduce stress; however, MBSR was associated with significant reductions in rumination and anxiety and improvements in empathy and self-compassion. Of note, the authors state that participants in the studies reviewed were most often undergraduate students, thus limiting the generalizability of results to healthy older adults. They urged future studies to focus on including representative samples (Chiesa and Serretti 2009). a review of mindfulness-based interventions reported that the mean age in mindfulness studies ranges from 38 to 51 years of age (Baer 2003).
Although only a handful of studies have examined the benefits of MBSR in older adults, they have yielded promising results. Findings indicate that MBSR training in older adults can improve emotional well-being by reducing loneliness, general emotional distress, and symptoms of depression and anxiety (Young and Baime 2010). MBSR has also been found to improve physical health parameters, including reduced blood pressure (Palta et al. 2012). reduced pain (Morone et al. 2008). and improved immune functioning (Moynihan et al. 2010).
The reported results of MBSR on cognitive function have been promising in young and middle-aged adults. Jain et al. (2007) examined attentional performance before and after either an 8-week MBSR course administered to meditation-naïve participants, a 1-month intensive mindfulness retreat administered to participants with previous meditation experience, or an 8-week no treatment control group. They concluded that meditation training (either additional or newly learned) improved voluntary top-down attentional control as measured by the Attention Network Test (Fan et al. 2002). Wenk-Sormaz (2005) examined the effects of brief mindfulness training on performance on the Stroop task (Stroop 1935). a measure of executive function, using healthy young meditation-naïve participants. Relative to the attentional control condition, three 20-min sessions of mindfulness meditation was associated with less Stroop interference and more flexible word production, suggesting that even brief exposure to mindfulness practice can improve attentional control.
In another study by Jha et al. (2010). the effects of an MBSR program on working memory ability were explored in two military cohorts as they went through a pre-deployment process. When compared with a civilian control group, the military personnel who did not receive mindfulness training experienced a degradation of working memory. Among the military personnel who were given mindfulness training, not only did they see memory improvement when compared with the cohort who did not receive training, but they also reported a dose–response effect of amount of time practiced, that is, working memory capacity increased with an increase in the number of minutes participants engaged in formal meditation practices (Jha et al. 2010).
In contrast, a number of studies have reported no effect of MBSR on cognitive function in healthy adults. For instance, Lykins et al. (2012) found that adults with long-term mindfulness meditation practice (average duration of 6 years) were no better than matched non-meditators on tasks measuring sustained attention, attentional switching, inhibition, or working memory. Similarly, Anderson et al. (2007) found that compared with an 8-week waitlist control group, an 8-week MBSR course for healthy adults resulted in no differences in sustained attention, attentional switching, inhibition, or non-directed attention, suggesting that the cognitive outcomes of mindfulness in healthy populations warrant further clarification.
More recently, Lenze et al. (2014) examined the effects of MBSR on cognitive function in a sample of 34 older adults with clinically significant anxiety-related distress and co-occurring cognitive dysfunction. Participants were assigned to either a traditional eight-session MBSR group or a modified 12-session MBSR group and were asked to complete a cognitive battery pre- and post-intervention. Participants showed statistically significant improvements on measures of immediate and delayed recall and executive function, regardless of which group they participated in. Furthermore, the authors found that the intervention reduced worry severity and that participants were highly satisfied with the intervention. Moynihan et al. (2013) found that compared with a waitlist control group, MBSR was able to produce small but significant changes in executive functioning in a sample of healthy older adults.
The MBSR literature contains several gaps, in part resulting from a failure to adhere to a standard intervention protocol. As reviewed previously, some researchers reported findings from studies comparing long-term mindfulness meditation practitioners with meditation-naïve participants (Lykins et al. 2012). while others used brief 20-min practices (Wenk-Sormaz 2005), and others made extreme alterations to the standard protocol (Jha et al. 2010). This lack of standardization makes it difficult, if not impossible, to compare findings across studies and determine the utility of an MBSR program through replication. It is thus imperative that the standard Kabat-Zinn (1990) guidelines are followed across studies to establish a foundation for its utility before drastic modifications are made.
Another limitation of the literature is that studies have failed to incorporate a control group or have used waitlist control groups rather than active control groups. Although waitlist control groups are useful as a group comparison, active control groups have several benefits. For instance, they allow researchers to draw conclusions about whether the experimental intervention is efficacious over and above the effects of participation in a research group and its related nonspecific factors.
Despite these limitations, in a review of 23 controlled, case–control, or randomized controlled studies examining the effect of mindfulness-based training on cognitive function among participants ranging in age from 18–75 years old, Chiesa et al. (2011) concluded that mindfulness-based practices “could provide significant benefits on several measures of cognition” (p. 462). The authors noted that executive function in particular deserves further investigation given that the substantial psychological benefits following mindfulness training are thought to depend, at least partly, on executive function (Baer 2003). These authors suggest that high quality studies using standardized mindfulness programs are needed in order to address the aforementioned discrepancies in the literature.
Given the robust association between aging and cognitive decline, the current exploratory study aimed to address a large gap in the literature and assess the effects of a standardized MBSR program on cognitive function in healthy older adults. Furthermore, the current study aimed to replicate previous findings on psychological well-being. Specifically, we hypothesized that compared with the control group, MBSR would be associated with significant improvements in executive function and episodic memory and improvements in mindfulness, mood, and quality of life. Given that Bishop et al. (2004) proposed that one of the most significant cognitive mechanisms involved in mindfulness is attention switching, our primary outcome variable was a measure of divided attention. The current study also aimed to assess the acceptability of the interventions and assess recruitment potential and retention rates.
Method
Participants
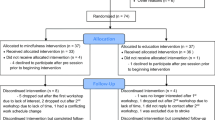
A total of 304 older adults were contacted and 196 individuals were excluded at the point of screening. The most common reason for exclusion from the study was being unable to make the time commitment, followed by not meeting inclusion criteria (described below), and lastly, declining to participate upon hearing the study details. The 97 remaining participants were assigned to either the MBSR or control condition. Figure 1 contains a CONSORT chart of participant flow from initial recruitment, pre-test, randomization, treatment completion, follow-up testing, and analysis. All participants were blinded to our study hypotheses. To ensure participants were unaware of the study hypotheses, they were only informed that the aims of the study were to assess whether an 8-week stress management program could affect psychological well-being and cognitive function. Group allocation was not disclosed until the eligible participant signed the informed consent form and completed baseline assessment.
Procedure
The present study was conducted between June 2013 and March 2015 and was approved by the Ryerson University Research Ethics Board. Participants were recruited through a combination of online recruitment advertisements, educational community talks/events, and through the Ryerson Senior Participant Pool, which is a Ryerson University-maintained database of older adult participants. Eligible individuals were required to be at least 60 years of age and living independently in the community. Furthermore, they were required to have English-language proficiency, have normal or corrected-to-normal hearing and vision, and be able to attend eight weekly sessions on Ryerson campus. Participants were excluded if they endorsed any medical or psychiatric conditions that might significantly affect cognitive performance, such as a neurodegenerative disorder, recently diagnosed psychopathology, stroke, or diabetes. Participants who endorsed regular, active participation in any mindfulness-based activities such as yoga, meditation, or tai chi were also excluded. Further, individuals were excluded if they had undergone neuropsychological testing in the past year (using a similar cognitive battery) due to potential learning effects.
Eligible participants were asked for their availability to attend the 8-week group. The intervention and control groups were held concurrently, each taking place during the same 8-week period, at the same time of day on different days (e.g., the intervention group was held on Thursdays at 10 am and the control group was held on Fridays at 10 am over the same 8-week period). At the time of screening, eligible participants were informed of the two weekdays when the interventions would take place (e.g., Thursdays or Fridays) but were not informed as to which intervention was to be held on each day. Group allocation was first based on randomization using a list randomizer if the eligible participant indicated that they were available on both weekdays for 8 weeks. However, for logistical reasons, participants who were only available on one of the 2 days were allocated to the group that they could attend. It is important to emphasize that participants were not aware of the group that they were allocated to until the end of their first testing session.
Eligible participants were asked to undergo a 1-h pre-intervention testing session 1 to 2 weeks prior to commencement of the intervention. A trained research assistant facilitated the testing session and was naïve to the participants’ group allocation until testing was complete. Following consent, participants completed a battery of cognitive tests and a series of psychological questionnaires. After the battery was complete, the participants were told whether they were assigned to MBSR or the reading and relaxation (R&R) control group. After the 8-week intervention phase, all participants were asked to meet with the same research assistant at the same time of day and complete a post-intervention testing session in which a comparable battery of cognitive tests was administered.
Interventions
MBSR
The MBSR intervention consisted of eight weekly group sessions lasting 2.5 h each. MBSR was administered according to the guidelines created by Kabat-Zinn (1990). with two minor modifications made to cater to the older adult population (i.e., slightly shortening daily practice time by 15 min to avoid physical discomfort associated with sitting for long periods of time, and eliminating the full-day retreat due to financial constraints and previous research suggesting that the retreat is too strenuous for older adults; Lenze et al. 2014). Kabat-Zinn (1990) encourages MBSR facilitators to make minor alterations to the protocol in order to accommodate the needs of their specific group of participants, so we are confident that these modifications did not affect the fidelity of the program.
A fixed facilitator protocol was followed. The protocol detailed the specific poems to be read, the exercises to be introduced, the discussion topics, the weekly homework, and the general duration for each in-session activity. Participants were taught various meditation practices that were applied in the course and also assigned for homework. Participants engaged in the body scan, sitting meditation, and light hatha yoga. Participants were required to complete 30 min of homework per day, which consisted of practicing the techniques learned in each week’s class. The MBSR groups were led by trained MBSR practitioners who maintained an ongoing personal practice and who had experience facilitating MBSR groups and working with older adults.
R&R
The R&R control group was made up of two components: (a) a reading component and (b) a relaxation component (i.e., progressive muscle relaxation (PMR)) and was designed to control for the nonspecific aspects of the MBSR program. As with the MBSR group, the R&R group met once per week for 2.5 h over 8 weeks at the same time of day. In the first half of each weekly session, the researcher led participants in a discussion about their thoughts on a short story, similar to a book club. The PMR component of the group took place in the second half of each weekly session and followed a modified protocol established by Bernstein et al. (2000). The reading component of the group controlled for cognitive and social engagement and the PMR component controlled for the meditation aspects of MBSR. The protocol used in this group detailed the specific exercises to be introduced, the discussion topics, the weekly homework, and the general duration for each in-session activity. To control for the time spent completing homework, participants were required to read a short story and engage in 30 min of daily PMR exercises each week. The R&R group was led by a trained graduate student.
Participants in both groups received audio compact discs to facilitate their at-home mindfulness or PMR practice and were asked to log their daily practices. Although controlling for the effects of group facilitator across the MBSR groups and between MBSR and R&R was not possible, a facilitator feedback questionnaire was administered to participants at the end of the intervention to measure whether the facilitators were comparable on a variety of nonspecific therapist characteristics. Facilitators in both groups completed an intervention fidelity checklist at the end of each session to ensure self-adherence to the standardized protocol. Participants who either dropped out of the intervention or declined to complete the cognitive assessment were contacted in order to document their reason(s) for discontinuing their participation in the project.
Measures
Participants completed a cognitive battery and a set of self-report questionnaires within 1 to 2 weeks before (pre-testing) and after (post-testing) the intervention. These measures consisted of cognitive and self-report measures of well-being.
Cognitive Measures
Global Cognitive Function
The Mini-Mental State Examination (MMSE; Folstein et al. 1975) is a brief cognitive screening tool of global cognitive function rated on a 30-point scale. It consists of 11 items representing several cognitive domains, including orientation to time and place, verbal memory, attention, language comprehension and production, and visual construction. Scores of 27 and above are associated with normal cognitive function. The MMSE has been judged to have satisfactory sensitivity and construct validity to cognitive impairment (Tombaugh and McIntyre 1992) and is sensitive to change (Roselli et al. 2009).
Executive Function
Trail Making Tests A and B (TMT; Reitan and Wolfson 1993) were used to evaluate information processing speed, visual scanning ability, integration of visual and motor functions, mental flexibility, and set shifting. TMT-A requires participants to connect 25 consecutively numbered circles using straight lines. TMT-B requires subjects to connect consecutive numbers and letters, alternating between the two sequences (i.e., 1-A-2-B-3-C). TMT-B is a timed task, and faster time-to-complete is associated with better functioning. It is sensitive to age-related decline in executive functioning (Rasmusson et al. 1998). Previous research indicates that TMT scores are sensitive to change after an MBSR intervention (Johansson et al. 2012).
The Controlled Oral Word Association Task (COWAT; Eslinger et al. 1984) was used to measure verbal fluency and has been found to be a sensitive indicator of executive dysfunction. The COWAT consists of three word-naming trials, and participants are asked to verbally generate as many words as they can think of when prompted with a letter of the alphabet (F, A, and S) and a category (Animals). This task not only requires participants to demonstrate semantic knowledge using phonological or categorical rules, but it also requires them to use executive functions to track prior responses and block intrusions (i.e., words that do not fit the rule; Kemper and McDowd 2008). This measure is sensitive to age-related decline in verbal fluency (Steinberg et al. 2005) and has been used previously with older adults (Anderson-Hanley et al. 2012).
An alternate version of the TMT was administered and counterbalanced to minimize learning effects. The alternate version of the TMT is comparable to the original version; Franzen et al. (1996) found no significant differences in overall level of performance between TMT Part A and its alternate form, and between TMT part B and its alternate form, in a sample of closed head injury patients. These authors found reliability estimates of r = 0.70 for TMT-A and its alternate form and r = 0.78 for TMT-B and its alternate form. Their results indicate adequate reliability of the alternate forms for TMT. However, the alternate version of the COWAT was not used, as previous research indicates a difference in difficulty between the alternate and original forms (Barry et al. 2008).
Psychosocial Questionnaires
Mindfulness
The Mindful Attention Awareness Scale (MAAS; Brown and Ryan 2003) was used as a dispositional measure of mindfulness. It is a 15-item scale that measures the frequency of mindful states in day-to-day life in both general and situation-specific statements. Higher scores are indicative of greater mindfulness. It has been used previously to measure mindfulness in older adults and has a Cronbach’s alpha level of 0.87 among the general adult population in the USA (Morone et al. 2009). It has demonstrated sensitivity to change after an MBSR intervention (Shapiro et al. 2007).
Perceived Stress
The Perceived Stress Scale (PSS; Cohen et al. 1983) measures the degree to which situations in one’s life are appraised as stressful. The scale includes items designed to measure how often individuals find their lives unpredictable, uncontrollable, and overloaded during the last month. Internal consistency is good (α = 0.85), and the stability of the test-retest coefficients ranges from 0.75 to 0.86 (Cohen et al. 1983). This scale has been used among older adult populations (Hamarat et al. 2001) and has been shown to be sensitive to change with a MBSR intervention (Shapiro et al. 2007).
Depression
The Geriatric Depression Scale (GDS; Yesavage et al. 1983) was used to measure depression in the elderly. It is a 30-item scale with clinical cutoff points at 5 ± 4 (normal), 15 ± 6 (mildly depressed), and 23 ± 5 (very depressed). It has demonstrated good capacity for discriminating between depressed and non-depressed elderly people (Montorio and Izal 1996) and additionally shows sensitivity to change following a psychological intervention (Thompson et al. 1987).
Quality of Life
The Quality of Life Scale (QOLS; Flanagan 1978) measures satisfaction with needs met. It contains 16 items representing six domains of quality of life: physical and material well-being, relationships with other people, social and civic activities, personal development, and independence. Cronbach’s alpha coefficient has been documented at 0.87 for the general adult population (Burckhardt et al. 1989). This scale has demonstrated sensitivity to change following an MBSR intervention (Azulay et al. 2012).
Self-esteem
The Rosenberg Self-Esteem Scale (RSES; Rosenberg, 1965) is a ten-item measure that assesses global self-esteem. The RSES contains an equal number of positively and negatively worded items and responses are coded on a four-point scale. It is considered to be an appropriate measure of self-esteem in the elderly (Breytspraak and George 1979) and a powerful predictor of increased reactivity to stress (Pruessner et al. 2005). This scale has previously demonstrated sensitivity to change following an MBSR intervention (Goldin and Gross 2010).
Feedback Questionnaire
At the end of the follow-up testing session, all participants were asked to complete a feedback questionnaire, consisting of a facilitator component and an intervention component. The facilitator feedback component instructed participants to rate their group facilitator on a variety of domains in order to determine whether the facilitators of each intervention were comparable in terms of therapist effects (adapted from the Cognitive Processing Therapy: Therapist Adherence and Competence protocol; Wiltsey-Stirman et al. 2013).
Statistical Analyses
Using the Outlier Labeling Rule (Hoaglin et al. 1986). outliers were discovered. Three participants were deemed outliers due to significantly slower time to complete the TMT-B task, two participants showed significantly higher scores on the GDS, and one participant showed significantly lower QOL than the rest of the participants. Given that exclusion of outliers did not significantly change statistical outcomes, all reported analyses contain the outlier data points.
One-way analysis of variance (ANOVA) and χ 2 analyses were used to analyze between-group differences at baseline. In order to test the stated hypotheses, mixed 2 × 2 analyses of covariance (ANCOVAs) were performed, using time (pre- and post-intervention) as the within groups factor and group assignment (MBSR, R&R) as the between groups factor. A priori variables (sex, education, and age) were entered as covariates in all analyses (Brayne and Calloway 1990; Deary et al., 2009; Tombaugh 2004).
Data were first analyzed using intention-to-treat (ITT) principles (Fisher et al. 1990). The ITT analyses included all participants enrolled in the group sessions, regardless of whether they completed the sessions or not. Then, “per protocol treatment” (PPT or completer) analyses were conducted on the subsample of participants that attended at least six of the eight sessions (i.e., intervention completers). The PPT analyses excluded participants who did not complete at least six (75 %) of the sessions. Analyses were conducted using SPSS version 21.0. All analyses were considered significant at p < 0.05.
Results
Baseline characteristics of the two groups are shown in Table 1. The MBSR and control group did not significantly differ in age, sex, level of education, or any of the cognitive measures. On average, participants in the MBSR group reported significantly greater depressive symptomatology compared with the R&R group. The cognitive and psychosocial data were analyzed using GDS as a covariate, to assess whether this baseline difference was significantly related to outcome. As GDS was not significantly associated with outcome, the variable was not entered as a covariate for the subsequent analyses.
Regarding study attrition, 52 MBSR participants (91 %) and 28 R&R participants (70 %) completed (i.e., attended at least six out of eight sessions) the study. Time commitments and unforeseen health concerns were the primary reasons for dropout. Although there were more non-completers in the R&R group, this difference was not statistically significant (χ 2 (1, 99) = 3.32, p = 0.08). Independent t tests and χ 2 analyses were conducted to test for differences in baseline factors that may have differentiated completers and non-completers. Non-completers were characterized by recalling significantly fewer words in the Long Delay Free Recall component of the CVLT-II (t(95) = −2.15, p = 0.03), displayed significantly slower time to complete the TMT-B (t(95) = 2.15, p = 0.03), and naming significantly fewer words (t(97) = −3.69, p < 0.0001) and animals (t(95) = −3.12, p < 0.0001) on the COWAT. Of the 97 individuals recruited into the study, 89 (91 %) completed the post-intervention follow-up cognitive testing session.
Controlling for age, sex, and education, a 2 × 2 mixed ANCOVA demonstrated that cognitive performance was not affected by time or group assignment in either ITT or PPT analyses, although the interaction between group and time on CVLT Long Delay Free Recall performance among intervention completers was marginally significant (p = 0.08; see Table 2).
A series of 2 × 2 mixed ANCOVAs were conducted to determine whether there were any group differences in the psychosocial variables over time (see Table 3). There was a significant interaction between group and time on MAAS score among completers, with the MBSR group endorsing slightly less mindfulness at post-intervention and the R&R group increasing in mindfulness (F(1, 75) = 4.09, p = 0.047). With regard to quality of life, there was a significant interaction between time and group for both ITT (F(1, 83) = 6.51, p = 0.01) and PPT (F(1, 77) = 5.24 p = 0.03) analyses, with the MBSR group reporting a higher QOL at post-intervention and the R&R group reporting lower QOL at post-intervention. No other group differences were observed.
At post-intervention, participants were asked to rate their facilitator on genuineness, warmth, empathy, professionalism, and a number of other nonspecific factors. Analyses indicate that facilitator ratings did not significantly differ between groups, suggesting the absence of nonspecific facilitator effects on intervention outcome (all ps ≥ 0.35).
Discussion
This study examined the effects of mindfulness training on executive function and psychosocial factors in psychologically healthy non-demented older adults, in a study comprised of a standard MBSR protocol and an active control group. Results of the current study are at odds with research that demonstrates beneficial cognitive effects of MBSR in clinical populations. For instance, Lenze et al. (2014) collected data from 34 older adults who endorsed anxiety disorders and/or depression, plus cognitive dysfunction. The participants were randomized into either an 8-week or modified 12-week MBSR protocol. Lenze et al. measured patient satisfaction with the protocols, as well as performance on two tasks of executive function. At the end of the program, participants noted that the protocol-recommended time to practice yoga was too strenuous, as was the full-day retreat. Regarding cognitive outcomes, both the 8-session and 12-session groups resulted in equal and significant improvements in measures of executive function, suggesting that older adults do not require more than eight sessions to experience beneficial effects of mindfulness training.
Despite the comparable sample size to the Lenze et al. (2014) study, we were unable to detect a significant benefit of mindfulness training on executive function following 8 weeks of MBSR. The contrast in study findings may be attributed to characteristics of the group under investigation, namely baseline psychological well-being. For the most part, mindfulness studies have comprised patient samples or participants reporting significant amounts of distress. Lenze et al. recruited older adults with stress-related anxiety symptoms and cognitive impairment. In the current study, older adult participants were high functioning, reported engagement in physical activity, were active members of the community, and had a body mass index in the normal range. All of these factors are known to support cognitive health (Yaffe et al. 2009). Further, according to normative data, participants in this study performed within the normal range on the TMT-B task for their age and level of education (Tombaugh 2004). The current sample also scored in the normal range for depressive symptomatology and perceived stress. Based on these sample characteristics, it may be suggested that older adult participants in the current study were already performing at optimal level, with no room for improvement after 8 weeks of mindfulness training. It may further be suggested that mindfulness training only produces beneficial cognitive effects for highly distressed individuals, which may explain some of the null findings in the literature in healthy adults (Anderson et al. 2007; Chambers et al. 2008; Heeren et al. 2009; Josefsson and Broberg 2010; Lykins et al. 2012).
Another potential, albeit unlikely, explanation for current findings may stem from the modifications that were made to the MBSR protocol, including decreasing daily practice from 45 to 30 min, and eliminating the half-day retreat. These modifications may have resulted in too little mindfulness training to elicit robust changes in executive function in this healthy sample. Although the Lenze et al. (2014) report on program acceptance does not support this hypothesis, high functioning healthy older adults may require more time and motivation to fully integrate this process into their daily lives. It is possible that high functioning study participants may not be as motivated to engage in the home-practice component of the training program, which may further impact study outcomes. Further, older adults in the current study may have required more time to test out mindfulness principles before having enough justification to use them to replace or support their current (and presumably successful) coping strategies. A final speculation may be that mindfulness training in high functioning older adults maintains rather than improves cognitive function. Future studies using longitudinal designs are required to test this hypothesis.
A strength of the current study, and one major methodological limitation in previous studies, is inclusion of an active control comparison condition. As previously noted, the inclusion of an active control group helps the researcher control for the effects of contact with a researcher, duration of weekly sessions, social engagement within a group setting, cognitive stimulation, and completing at-home assignments. In the current study, participants were assigned to the MBSR condition or the R&R condition. The control condition was carefully designed to control for the acquisition of relaxation techniques and cognitive engagement. Participants were not aware that the R&R condition was designed to control for the MBSR condition until completion of all study procedures. Due to feasibility issues, some of the participants were not randomized into each condition but rather were allocated depending on their availability (i.e., which of the 2 days they were available to attend). Although strict randomization was not feasible at all times, all participants were informed of both interventions during the recruitment phase and were under the impression that they would be randomized. While a number of participants expressed disappointment in their group allocation (some participants wanted to be in the MBSR condition and some wanted to be in the R&R condition), only one participant refused to participate following group allocation and withdrew from the study completely. Based on facilitator rating forms and qualitative reports (data not presented here), both groups reported an equally positive experience with the program.
Surprisingly, the MBSR group did not demonstrate increased mindfulness at study completion, while the R&R group showed a slight increase. Although completely unexpected, choice of measurement tool may have played a role in this finding. The MAAS is a single-factor scale that measures present-centered attention/awareness (Brown and Ryan 2003). Although the cultivation of attention and awareness were not explicitly communicated to participants in the R&R condition, the practice of PMR, which entails tensing and relaxing muscles and noticing the difference between the two body states, is an exercise of attention/awareness. While mindful attention/awareness is a central component of mindfulness, the MAAS neglects to assess other core aspects of mindfulness, including non-judgment, non-reactivity, self-compassion, and acceptance.
In the current study, significant group differences were found for self-report quality of life, with the MBSR group reporting higher scores on the QOL scale and R&R reporting lower scores on the QOL scale at post-intervention. This group difference may have resulted from the cultivation of other core mindfulness traits in the MBSR group, including non-judgment, self-compassion, and acceptance. Indeed, previous research shows that self-compassion is positively associated with quality of life (Pinto‐Gouveia et al. 2014) and is more predictive of quality of life than mindful attention/awareness (Van Dam et al. 2011). Unfortunately, this hypothesis is purely speculative given that we did not assess these mindfulness characteristics in the current study. Future research would benefit from using more comprehensive mindfulness scales, such as the Five Facet Mindfulness Questionnaire (Baer et al. 2006). As suggested by our results, this is especially important when incorporating an active control group in the study design.
In a review of research related to meditation and spirituality in the elderly, Lindberg (2005) noted although meditation/relaxation can be successfully taught to older adults, none of the 36 studies they reviewed included a quantification of learning rates. In a study by Brown and Ryan (2003). the developers of the MAAS, the authors found that it is not the amount of time one practices meditation, but the amount of years of practice that significantly and positively correlates with scores on the MAAS. As a result, we speculate that it might take substantially longer than 8 weeks of mindfulness training to produce significant increases in the MAAS in an older adult population. In contrasting the cultivation of attention/awareness through the practice of mindfulness to the acquisition of attention/awareness through PMR, it may be postulated that attending to the tensing and releasing of muscles is easier for older adults to learn and develop than simply attending to the breath.
The primary limitation of the present study was the sample size. Our sample size was generally larger than that of previous studies; according to a systematic review of 23 randomized controlled trial studies that examine the effects of mindfulness on objective measures of cognitive functions, the average number of participants per group is 30 (Chiesa et al. 2011). Nonetheless, it is likely that we were underpowered. In determining the sample size needed for this study, a power calculation using the means and standard deviations on an executive function task reported in the Lenze et al. (2014) study shows that an estimated 122 participants (61 in each group) is required in order to make inferences about the population for the primary outcome measure (Crawley 2005). The current study sample (N = 97) consisted of 57 participants in the MBSR condition and 40 in the control condition. It is possible that the inclusion of additional participants would increase the statistical power needed to detect a meaningful group difference on the executive function task.
The study is also limited by the fact that an additional waitlist control condition was not included, which may have allowed us to replicate previous research that show MBSR is at least more beneficial than the passage of time (e.g., Moynihan et al. 2010). Inclusion of a waitlist control group would also exclude the possibility that the non-significant findings were a result of regression toward the mean.
A final limitation of the current study was the lack of an independent assessor for the facilitator quality check. Although facilitators followed a standard protocol and completed a self-adherence checklist, without an independent assessor, there is no guarantee that bias was not introduced. Although facilitator effects are not uncommon in clinical research (Martindale 1978). participants in the current study were asked to rate facilitators on genuineness, warmth, professionalism, and a number of other nonspecific factors. Analyses of these ratings suggest that there were no significant differences between facilitators on any of the aforementioned factors, suggesting the absence of nonspecific facilitator effects on intervention outcome.
Despite the aforementioned limitations, this exploratory study provides valuable insight into the feasibility, acceptability, and effectiveness of psychosocial interventions for healthy older adults. It is important to note that the completion rate in the MBSR intervention was marginally higher than the control group, which suggests that participants were more satisfied with the group and further demonstrates that mindfulness training is an acceptable intervention for healthy older adults. Qualitative data (not reported here) suggest that participants who completed the MBSR intervention felt that the group helped to “de-clutter” the mind, increase physical and mental awareness, increase patience and acceptance, reduce physical pain, and enhance the ability to cope with stressors. However, the majority of participants in the control group also gave similarly positive feedback, stating that the group was associated with an improvement in sleep quality, an increased sense of control over stressors, and increased relaxation.
With an aging population on the rise, it is important to assess interventions and programs that may maintain cognitive and emotional health in late life. Although the current sample size may have limited statistical power in detecting group differences on outcome measures, characteristics of the sample must also be considered. While the current findings do not support a beneficial effect of mindfulness training on cognitive function after 8 weeks in psychologically healthy, high functioning older adults, research with follow-up assessments is needed to determine whether long-term mindfulness practice facilitates maintenance of cognitive function over time in high functioning individuals. It is recommended that future studies employ similar guidelines with respect to the use of a standardized mindfulness program and an active control condition in healthy older adults who report heightened levels of distress. Overall, this research contributes to the scarce literature that evaluates the effects of mindfulness training in late life.
References
Anderson, N. D., Lau, M. A., Segal, Z. V., & Bishop, S. R. (2007). Mindfulness-based stress reduction and attentional control. Clinical Psychology & Psychotherapy, 14, 449–463. doi:10.1002/cpp.544.
Anderson-Hanley, C., Arciero, P. J., Brickman, A. M., Nimon, J. P., Okuma, N., Westen, S. C., & Zimmerman, E. A. (2012). Exergaming and older adult cognition. American Journal of Preventive Medicine, 42, 109–119. doi:10.1016/j.amepre.2011.10.016.
Astin, J. A. (1997). Stress reduction through mindfulness meditation: effects on psychological symptomatology, sense of control, and spiritual experiences. Journal of Psychotherapy and Psychosomatics, 66, 97–106. doi:10.1159/000289116.
Azulay, J., Smart, C. M., Mott, T., & Cicerone, K. D. (2012). A pilot study examining the effect of mindfulness-based stress reduction on symptoms of chronic mild traumatic brain injury/postconcussive syndrome. The Journal of Head Trauma Rehabilitation, 1, 1–9. doi:10.1097/HTR.0b013e318250ebda.
Baer, R. A. (2003). Mindfulness training as a clinical intervention: a conceptual and empirical review. Clinical Psychology: Science & Practice, 10, 125–143. doi:10.1093/clipsy.bpg015.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27–45. doi:10.1177/1073191105283504.
Barry, D., Bates, M. E., & Labouvie, E. (2008). FAS and CFL forms of verbal fluency differ in difficulty: a meta-analytic study. Applied Neuropsychology, 15, 97–106. doi:10.1080/09084280802083863.
Bernstein, D. A., Borkovec, T. D., & Hazlett-Stevens, H. (2000). New directions in progressive relaxation training: a guidebook for helping professionals. Westport: Praeger.
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., & Devins, G. (2004). Mindfulness: a proposed operational definition. Clinical Psychology: Science and Practice, 11, 230–241. doi:10.1093/clipsy.bph077.
Brayne, C., & Calloway, P. (1990). The association of education and socioeconomic status with the Mini Mental State Examination and the clinical diagnosis of dementia in elderly people. Age & Ageing, 19, 91–96. doi:10.1093/ageing/19.2.91.
Breytspraak, L. M., & George, L. K. (1979). Measurement of self-concept and self-esteem in older people: state of the art. Experimental Aging Research, 5, 137–148.
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84, 822–848. doi:10.1037/0022-3514.84.4.822.
Burckhardt, C. S., Woods, S. L., Schultz, A. A., & Ziebarth, D. M. (1989). Quality of life of adults with chronic illness: a psychometric study. Research in Nursing & Health, 12, 347–354. doi:10.1002/nur.4770120604.
Cahn-Weiner, D. A., Malloy, P. F., Boyle, P. A., Marran, M., & Salloway, S. (2000). Prediction of functional status from neuropsychological tests in community-dwelling elderly individuals. Clinical Neuropsychologist, 14, 187–195. doi:10.1076/1385-4046.
Carlson, M. C., Fried, L. P., Xue, Q. L., Bandeen-Roche, K., Zeger, S. L., & Brandt, J. (1999). Association between executive attention and physical functional performance in community-dwelling older women. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 54, S262–S270. doi:10.1093/geronb/54B.5.S262.
Carlson, L. E., Speca, M., Patel, K. D., & Goodey, E. (2003). Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosomatic Medicine, 65, 571–581. doi:10.1097/01.PSY.0000074003.35911.41.
Chambers, R., Lo, B. C. Y., & Allen, N. B. (2008). The impact of intensive mindfulness training on attentional control, cognitive style and affect. Cognitive Therapy & Research, 32, 303–322. doi:10.1007/s10608-007-9119-0.
Chiesa, A., & Serretti, A. (2009). Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. The Journal of Alternative and Complementary Medicine, 15, 593–600.
Chiesa, A., Calati, R., & Serretti, A. (2011). Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clinical Psychology Review, 31, 449–464. doi:10.1016/j.cpr.2010.11.003.
Cohen, S., Kamarch, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396.
Crawley, M. J. (2005). Statistics—an introduction using R. West Sussex: John Wiley & Sons Ltd.
Deary, I. J., Corley, J., Gow, A. J., Harris, S. E., Houlihan, L. M., Marioni, R. E., Penke, L., Rafnsson, S. B., & Starr, J. M. ( 2009). Age-associated cognitive decline. British Medical Bulletin, 92(1), 135–152.
Eslinger, P. J., Damasio, A. R., & Benton, A. L. (1984). The Iowa screening battery for mental decline. Iowa City, IA: University of Iowa.
Fan, J., McCandliss, B. D., Sommer, T., Raz, A., & Posner, M. I. (2002). Testing the efficiency and independence of attentional networks. Journal of Cognitive Neuroscience, 14, 340–347. doi:10.1162/089892902317361886.
Fisher, L. D., Dixon, D. O., Herson, J., Frankowski, R. K., Hearron, M. S., & Peace, K. E. (1990). Intention to treat in clinical trials. In K. E. Peace (Ed.), Statistical issues in drug research and development (pp. 331–350). New York: Marcel Dekker.
Flanagan, J. C. (1978). A research approach to improving our quality of life. American Psychologist, 33(2), 138–147.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. doi:10.1016/0022-3956(75)90026-6.
Franzen, M. D., Paul, D., & Iverson, G. L. (1996). Reliability of alternate forms of the Trail Making Test. The Clinical Neuropsychologist, 10, 125–129. doi:10.1080/13854049608406672.
Goldin, P. R., & Gross, J. J. (2010). Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion, 10, 83–91. doi:10.1037/a0018441.
Grigsby, J., Kaye, K., Baxter, J., Shetterly, S. M., & Jamman, R. F. (1998). Executive cognitive abilities and functional status among community-dwelling older persons in the San Luis Valley health and aging study. Journal of the American Geriatrics Society, 46(5), 590–596.
Hamarat, D. T., Zabrucky, K. M., Steele, D., Matheny, K. B., & Aysan, F. (2001). Perceived stress and coping resource availability as predictors of life satisfaction in young, middle-aged, and older adults. Experimental Aging Research, 27, 181–196. doi:10.1080/036107301750074051.
Heeren, A., Van Broeck, N., & Philippot, P. (2009). The effects of mindfulness on executive processes and autobiographical memory specificity. Behaviour Research and Therapy, 47, 403–409. doi:10.1016/j.brat.2009.01.017.
Hoaglin, D. C., Iglewicz, B., & Tukey, J. W. (1986). Performance of some resistant rules for outlier labeling. Journal of the American Statistical Association, 81(396), 991–999.
Jain, S., Shapiro, S. L., Swanick, S., Roesch, S. C., Mills, P. J., Bell, I., & Schwartz, G. E. (2007). A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine, 33(1), 11–21.
Jha, A. P., Stanley, E. A., Kiyonaga, A., Wong, L., & Gelfand, L. (2010). Examining the protective effects of mindfulness training on working memory capacity and affective experience. Emotion, 10, 54–64. doi:10.1037/a0018438.
Johansson, B., Bjuhr, H., & Rönnbäck, L. (2012). Mindfulness-based stress reduction (MBSR) improves long-term mental fatigue after stroke or traumatic brain injury. Brain Injury, 26, 1621–1628. doi:10.3109/02699052.2012.700082.
Josefsson, T., & Broberg, A. (2010). Meditators and non-meditators on sustained and executive attentional performance. Mental Health, Religion & Culture, 14, 291–309. doi:10.1080/13674670903578621.
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General Hospital Psychiatry, 4, 33–47.
Kabat-Zinn, J. (1990). Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Delta Trade Paperbacks.
Kabat-Zinn, J., Massion, A. O., Kristeller, J., Peterson, L. G., Fletcher, K. E., Pbert, L., & Santorelli, S. F. (1992). Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry, 149(7), 936–943.
Kemper, S., & McDowd, J. M. (2008). Dimensions of cognitive aging: executive function and verbal fluency. In S. M. Hofer & D. F. Alwin (Eds.), Handbook of cognitive aging: interdisciplinary perspectives (pp. 181–192). Los Angeles, CA: Sage.
Klatt, M. D., Buckworth, J., & Malarkey, W. B. (2008). Effects of low-dose mindfulness-based stress reduction (MBSR-ld) on working adults. Health Education & Behavior, 36, 601–614. doi:10.1177/1090198108317627.
Lenze, E. J., Hickman, S., Hersheym, T., Wendleton, L., Ly, K., Dixon, D., Dore, P., & Wetherell, J. L. (2014). Mindfulness-based stress reduction for older adults with worry symptoms nad co-occuring cognitive dysfunction. Geriatric Psychiatry, 29(10), 991–1000.
Lezak, M. D., Howieson, D. B., & Loring, D. W. (2004). Neuropsychological assessment (4th ed.). New York: Oxford University Press.
Lykins, E. L. B., Baer, R. A., & Gottlob, L. R. (2012). Performance-based tests of attention and memory in long-term mindfulness meditators and demographically matched nonmeditators. Cognitive Therapy and Research, 36, 103–114. doi:10.1007/s10608-010-9318-y.
Martindale, C. (1978). The therapist-as-fixed-effect fallacy in psychotherapy research. Journal of Consulting and Clinical Psychology, 46, 1526–1530.
Montorio, I., & Izal, M. (1996). The Geriatric Depression Scale: a review of its development and utility. International Psychogeriatrics, 8, 103–112. doi:10.1017/S1041610296002505.
Morone, N. E., Lynch, C. S., Greco, C. M., Tindle, H. A., & Weiner, D. K. (2008). I felt like a new person. The effects of mindfulness meditation on older adults with chronic pain: qualitative analysis of diary entries. Journal of Pain, 9, 841–848. doi:10.1016/j.pain.2008.04.003.
Morone, N. E., Rollman, B. L., Moore, C. G., Qin, L., & Weiner, D. K. (2009). A mind-body program for older adults with chronic low back pain: results of a pilot study. Pain Medicine, 10, 1395–1407. doi:10.1111%2Fj.1526-4637.2009.00746.x.
Moynihan, J. A., Klorman, R., Chapman, B. P., Duberstein, P. R., Brown, K. W., Krasner, M., & Talbot, N. L. (2010). Mindfulness to improve elders’ immune and health status. Psychoneuroimmunology, 24, S13. doi:10.1016/j.bbi.2010.07.041.
Palta, P., Page, G., Piferi, R. L., Gill, J. M., Hayat, M. J., Connolly, A. B., & Szanton, S. L. (2012). Evaluation of a mindfulness-based intervention program to decrease blood pressure in low-income African-American older adults. Journal of Urban Health, 89, 208–316. doi:10.1007/s11524-01109654-6.
Pinto‐Gouveia, J., Duarte, C., Matos, M., & Fráguas, S. (2014). The protective role of self‐compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clinical Psychology & Psychotherapy, 21, 311–323. doi:10.1002/cpp.1838.
Pruessner, J. C., Baldwin, M. W., Dedovic, K., Renwick, R., Mahani, N. K., Lord, C., & Lupien, S. (2005). Self-esteem, locus of control, hippocampal volume, and cortisol regulation in young and old adulthood. NeuroImage, 28, 815–826. doi:10.1016/j.neuroimage.2005.06.014.
Rasmusson, D. X., Zonderman, A. B., Kawas, C., & Resnick, S. M. (1998). Effects of age and dementia on the Trail Making Test. The Clinical Neuropsychologist, 12, 169–178. doi:10.1076/clin.12.2.169.2005.
Reitan, R., & Wolfson, D. (1993). The Halstead–Reitan neuropsychological test battery: theory and clinical interpretation. Tucson, AZ: Neuropsychology Press.
Roselli, F., Tartaglione, B., Federico, F., Lepore, V., Defazio, G., & Livrea, P. (2009). Rate of MMSE score change in Alzheimer’s disease: influence of education and vascular risk factors. Clinical Neurology and Neurosurgery, 111, 327–330. doi:10.1016/j.clineuro.2008.10.006.
Royall, D. R., Palmer, R., Chiodo, L. K., & Polk, M. J. (2004). Declining executive control in normal aging predicts change in functional status: the freedom house study. Journal of American Geriatric Society, 52(3), 346–352.
Rosenberg, M. (1965). Society and the adolescent self-image. Princeton, N.J: Princeton University Press.
Segal, Z. J., Williams, M. G., & Teasdale, J. D. (2002). Mindfulness based cognitive therapy for depression: a new approach to preventing relapses. New York: Guildford Press.
Shapiro, S. L., Schwartz, G. E., & Bonner, G. (1998). Effects of mindfulness-based stress reduction on medical and premedical students. Journal of Behavioral Medicine, 21(6), 581–599.
Shapiro, S. L., Brown, K. W., & Biegel, G. M. (2007). Teaching self-care to caregivers: effects of mindfulness-based stress reduction on the mental health of therapists in training. Training and Education in Professional Psychology, 1, 105–115. doi:10.1037/1931-3918.1.2.105.
Speca, M., Carlson, L. E., Goodey, E., & Angen, M. (2000). A randomized, waitlist controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosomatic Medicine, 62(5), 613–622.
Steinberg, B. A., Bieliauskas, L. A., Smith, G. E., & Ivnik, R. J. (2005). Mayo’s older Americans normative studies: age- and IQ-adjusted norms for the Trail-Making Test, the Stroop test, and MAE controlled oral word association test. The Clinical Neuropsychologst, 19, 329–377. doi:10.1080/13854040590945210.
Stroop, J. R. (1935). Studies of interference in serial verbal reactions. Journal of Experimental Psychology, 18, 643–662. doi:10.1037/h0054651.
Thompson, L. W., Gallagher, D., & Breckenridge, J. S. (1987). Comparative effectiveness of psychotherapies for depressed elders. Journal of Consulting and Clinical Psychology, 55, 385–390. doi:10.1037/0022-006X.55.3.385.
Tombaugh, T. N. (2004). Trail Making Test A and B: normative data stratified by age and education. Archives of Clinical Neuropsychology, 19, 203–214. doi:10.1016/S0887-6177(03)00039-8.
Tombaugh, T. N., & McIntyre, N. J. (1992). The mini-mental state examination: a comprehensive review. Journal of the American Geriatrics Society, 40(9), 922–935.
Van Dam, N. T., Sheppard, S. C., Forsyth, J. P., & Earleywine, M. (2011). Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. Journal of Anxiety Disorders, 25, 123–130. doi:10.1016/j.janxdis.2010.08.011.
Wang, L., Van Belle, G., Kukull, W. B., & Larson, E. B. (2002). Predictors of functional change: a longitudinal study of nondemented people aged 65 and older. Journal of the American Geriatrics Society, 50(9), 1525–1534.
Wenk-Sormaz, H. (2005). Meditation can reduce habitual responding. Advances in Mind-Body Medicine, 21(3–4), 33–49.
Wiltsey-Stirman, S. W., Monson, C. M., & Resick, P. (2013). Cognitive processing therapy: therapist adherence and competence protocol. Unpublished manuscript.
Yaffe, K., Fiocco, A. J., Lindquist, K., Vittinghoff, E., Simonsick, E. M., Newman, A. B., & Harris, T. B. (2009). Predictors of maintaining cognitive function in older adults: the Health ABC Study. Neurology, 72, 2029–2035. doi:10.1212/WNL.0b013e3181a92c36.
Yesavage, J. A., Brink, T. L., Rose, T. L., Lum, O., Huang, V., Adey, M., & Leirer, V. O. (1983). Development and validation of a geriatric depression screening scale: a preliminary report. Journal of Psychiatric Research, 17, 37–49. doi:10.1016/0022-3956(82)90033-4.
Young, L., & Baime, M. (2010). Mindfulness-based stress reduction: effect on emotional distress in older adults. Complementary Health Practice Review, 15, 59–64. doi:10.1177/1533210110387687.
Acknowledgments
We would like to thank Katy Curtis, Robin Hurlow, Kirstin Bindseil, and Dr. Farah Jindani for helping us lead the MBSR groups. We would also like to thank all research assistants of the Stress and Healthy Aging Research Lab who helped with testing procedures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was partially supported by Ryerson University’s Health Research Fund.
Rights and permissions
About this article
Cite this article
Mallya, S., Fiocco, A.J. Effects of Mindfulness Training on Cognition and Well-Being in Healthy Older Adults. Mindfulness 7, 453–465 (2016). https://doi.org/10.1007/s12671-015-0468-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-015-0468-6