Abstract
Catheter-associated urinary tract infections (CAUTI) are one of the most common nosocomial diseases accounting for up to about 23% of healthcare-associated infections. High antibiotic resistance of biofilm-associated bacteria is a serious limiting factor in the treatment of patients. Therefore, the investigations of bacterial biofilms and their regulation can play a pivotal role in the development of new approaches to treating infections. P. aeruginosa is a key bacterium responsible for most urinary tract infections. In this study, urinary catheter–associated P. aeruginosa strains were isolated and their antibiotic resistance was studied. Polymicrobial biofilms were found on the urinary catheter surfaces derived from patients with different urinary tract diseases. Three strains of Pseudomonas aeruginosa isolated from the catheter-associated biofilms were resistant to meropenem. The resistance to carbapenemss of P. aeruginosa strains 96,347 and 96,349 was observed to be mediated by VIM-type metallo-β-lactamase gene expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Catheter-associated urinary tract infections (CAUTI) remain one of the most widespread nosocomial diseases that account for about 36% of all healthcare-associated infections [1]. In turn, a crucial portion of UTI involves catheter-associated UTI (CAUTI), which makes up approximately 67% of all UTI cases [1]. Various internal medical treatment devices, such as catheters, urethral stents, or sphincters, are considered favorable environments for bacterial growth and biofilm development resulting in the spread of urinary tract infections. Biofilm formation on catheters is a common phenomenon for most pathogenic and opportunistic microorganisms because, in their natural environment, bacteria predominantly grow as aggregates adhered to different surfaces. In biofilms, microorganisms acquire high resistance to host-derived immune system defense and antibiotics due to the impermeable extracellular matrix formation and cell physiology alterations [2]. Moreover, catheter materials, such as latex and silicone, are very adherent for negatively charged bacterial cells and cannot initiate the immune response of the organism in contrast to tissue surfaces of the bladder mucosa [3].
P. aeruginosa is a Gram-negative bacterium that remains a key role player in many diseases, in particular those associated with urinary tract infections. Due to its relatively large genome and flexible metabolism, this organism colonizes numerous ecological niches. As an opportunistic microorganism, P. aeruginosa inhabits various human tissues and organs especially weakened organisms, which is extremely dangerous for patients with nosocomial and ventilator-associated pneumonia, cystic fibrosis (CF), meningitis, abscess, soft tissue infections, urolithiasis, prostatic hyperplasia, cystitis, nephritis, catheter-associated infections, corneal infections, and conjunctival erythema, burn wounds, chronic obstructive pulmonary disease (COPD), and with many other diseases [4]. Generally, P. aeruginosa is characterized as a very fast-growing bacterium with high resistance to different antimicrobial agents including antibiotics. The whole-genome sequencing of P. aeruginosa shows the presence of host immune system and antibiotic resistance genes, including efflux system coding genes and genes of antibiotic-degrading enzymes providing resistance to beta-lactam and aminoglycoside antibiotics. Additionally, resistance to antibiotics is sometimes facilitated by mutations that modify or eliminate the molecular target of the antibiotic [5, 6]. Therefore, the high adaptability of P. aeruginosa makes it extremely refractory.
Besides antibiotic resistance, pathogenic bacteria can be defined by their tolerance to antimicrobial compounds, which is determined by the ability of bacterial cells to survive due to a reversible phenotype or modified mode of growth related to biofilms [7]. While in planktonic cultures bacteria usually display antibiotic resistance, antibiotic tolerance of P. aeruginosa is related to its biofilm formation. The mechanisms that contribute to antibiotic tolerance include restricted antimicrobial diffusion in the biofilm, slow growth rate, differential physiological activity of the bacteria, induction of specific tolerance mechanisms, and persister cell formation, oxygen gradients. Also, several studies have suggested that components of the biofilm matrix can bind to antibiotics and, thus, limiting their penetration into the cell [8, 9]. Persister cells in biofilms are characterized by a reduced dividing rate and all cellular processes including replication, translation, and cell wall synthesis, which make them less sensitive to antibiotics than the majority of the bacterial population [10]. Generally, bacteria detached from biofilms maintain new features even after transitioning back to the planktonic mode, which helps them to avoid antimicrobial compounds. Tolerance to antibiotics may also be associated with the expression of specific genes including genes encoding enzymes that destroy antibiotics, efflux system proteins, and others.
The most well-known antibiotic-degrading enzymes are β-lactamases produced by both gram-positive and gram-negative bacteria including uropathogenic Enterobacteriacea, Pseudomonas spp., and many other bacteria. β-lactamases produced by gram-negative bacteria are transferred into the periplasm, while gram-positive bacteria secrete these types of enzymes externally into the media. Secreted β-lactamases hydrolyze β-lactam antibiotics before they reach the bacterial cells; periplasmic enzymes resist the penetration of antibiotics through the inner membrane of bacteria. In biofilms, β-lactamase produced by bacteria is enclosed in the matrix and has the ability to inactivate β-lactam antibiotics [11, 12].
Notably, the expression of β-lactamases might have a completely opposite effect on the ability to form biofilms [13]. For example, strains of P. aeruginosa and E. coli that produced A and D classes of β-lactamases were characterized by low ability to form biofilms that presumably resulted from variations in peptidoglycan structure of the cell walls [13]. Additionally, sub-inhibitory concentrations of antibiotics can initiate a biofilm formation by different bacteria. It was shown that low dosages of tobramycin, tetracycline, and norfloxacin induced biofilm formation by Pseudomonas aeruginosa. β-lactams can likewise stimulate biofilm assembly in Haemophilus influenzae [14]. Therefore, exploration of biofilm-mediated bacterial resistance to antibiotics coupled with the production of enzymes, especially β-lactamases, is an important key to understanding the mechanisms of chronic and persistent infection development.
In this study, we aimed to isolate P. aeruginosa strains associated with biofilms on urinary catheters of patients with different urinary tract diseases and to characterize their antibiotic resistance particularly related to β-lactamases production. Analyzed clinical samples of catheters were contaminated with polymicrobial biofilms formed by different bacteria including Pseudomonas aeruginosa.
2 Material and Methods
2.1 Catheter Samples
Catheter samples were provided by the Department of Urology of the Medical and sanitary part of Kazan (Volga region) Federal University (Z.G. Gimadeev). Catheter samples were collected with patient consent. Catheter samples were taken from 8 patients of different age and gender with urinary tract diseases; catheters number used in experiment was limited by the clinical material at the sampling time period (August–September, 2016). Prepared samples were immediately placed in sterile containers with sterile 0.9% NaCl and stored at 4 °C for not more than 24 h before analysis.
2.2 Isolation of Catheter-Associated Bacteria
The bacterial strains used in this study were clinical isolates from indwelling urinary Foley catheters of patients with urinary tract infections (bladder stones, prostatic hyperplasia, urinary retention, acute tubulointerstitial nephritis). Bacteria were isolated from the inner surface of the catheter samples. In brief, catheter samples were initially washed 3 times in sterile 0.9% NaCl solution to remove planktonic bacterial cells. Material from the catheter surface was scrapped by a pipet tip, plated on LB agar medium in Petri dishes, and incubated at 37 °C for 18–48 h. Individual colonies were sub-cultured to new plates. Strains were identified using mass-spectrometry analysis as described below.
LB medium used for bacteria cultivation (lysogeny broth): tryptone — 10.0 g/l; yeast extract — 5 g/l; NaCl — 5 /l; solid medium included 2% bacto-agar.
2.3 Identification of Microorganisms by the MALDI-TOF Mass Spectrometry Method
Microorganism identification was performed using MALDI Biotyper (Microflex/Autoflex mass-spectrometer (Bruker, Germany). Sample preparation was performed according to the standard protocol [15]. Briefly, a single colony of the 18-h-grown bacterial culture was picked up from the LB-agar plate, placed on the mass-spectrometry analysis target, and dried at room temperature (RT). Dried colony samples were twice treated by 1 μl of 2.5-DHB (2.5-dihydroxybenzoic acid) and dried again at RT [16]. Microorganisms were identified on the MALDI Biotyper by comparing the spectra of bacterial ribosomal proteins with the databases provided by the manufacturer.
2.4 Biofilm Density Measurement
The relative density of biofilms on the surfaces of catheters and 24-well polystyrene tissue plates was measured using the biofilm staining method with crystal violet (CV) [17]. 0.5 cm × 0.5 cm pieces of catheter samples were washed three times for 2–3 min with 1 ml of sterile PBS (phosphate-buffered saline, 1xPBS: NaCl — 8 g/l; KCl — 0.2 g/l; KH2PO4 — 0.24 g/l; Na2HPO4 — 1.44 g/l; pH 7.4) to remove planktonic cells. Samples were placed in a test tube and incubated in 300 μl of a 0.1% CV solution for 15–20 min (CV solution: 0.001 g/ml CV dye dissolved in 96% ethanol and filtered through a 0.2-µm mesh sieve). After staining, CV solution was discarded and samples were carefully washed 3 times with PBS. Stained samples were then air dried at RT, and biofilm-bounded dye was eluted in 300 µl of 96% ethanol. Eluted solution was transferred into new tubes and the optical density OD590 was measured on a microplate Spectrophotometer (x MarkTM, Bio-RAD).
The efficiency of biofilm formation was assessed by the method described in Stepanovic et al., (2007) [18]. The results were calculated based on three standard deviations above that of uninoculated medium (negative control). The average OD values were calculated for all tested strains and the negative control since all experiments are performed in triplicate and repeated three times. The cut-off value (ODc) was established. It was defined as three standard deviations (SD) above the mean OD of the negative control: ODc = average OD of negative control + (3*SD of negative control). The final OD value of a tested strain was expressed as the average OD value of the strain reduced by ODc value (OD = average OD of a strain − ODc). The ODc value was calculated for each microtiter plate separately. If a negative value was obtained, it was presented as zero, while any positive value indicated biofilm production. Strains were divided into the following categories: no/weak biofilm producer, moderate biofilm producer, and strong biofilm producer, based upon the previously calculated OD values (for this type of calculation average OD value of the strain should not be reduced by ODc value): no/weak biofilm producer—ODc ≤ OD* ≤ 2 × ODc; moderate biofilm producer—2 × ODc < OD* ≤ 4 × ODc; strong biofilm producer—> ODc.
2.5 Scanning Electron Microscopy
Catheter samples for scanning electron microscopy (SEM) were processed following a previously described protocol [19]. Specifically, 0.5 cm × 0.5 cm pieces of catheters were washed twice with PBS for 10 min and placed in a fixative (1% glutaraldehyde in PBS buffer) for 18 h. The samples were then washed twice for 10 min with PBS and subsequently dehydrated with a series of ethanol washes (10% for 10 min, 25% for 10 min, 50% for 10 min, 75% for 10 min, 85% for 10 min, 96% for 15 min), and were air-dryed at RT. After air-drying, specimens were coated with gold–palladium mix and imaged using MERLIN scanning electron microscope (Carl Zeiss, Germany) at an accelerating voltage of 5 kV.
2.6 Optimization of Growth Conditions for Biofilms Formation
Short-term cultivation of bacterial biofilms was carried out under static conditions in polystyrene 24-well plates in 3 ml Muller-Hinton (MH, MAST, UK) medium per well. The initial optical density of bacteria cultures in the medium was 0.1 (OD590 = 0.1). Cultivation in wells was carried out statically at 37 °C for 5 days with the replacement of the nutrient medium with a fresh at 2nd and 4th days.
2.7 Urease Activity Assay
The bacterial urease activity was determined using Christensen’s urea medium [20]. This method resides in the changing of medium color from pale yellow to red-violet due to urea hydrolysis and pH changing under the secreted urease activity of the microorganisms. Christensen’s urea medium contained solution I and solution II. Solution I: peptone — 1.0 g/L; sodium chloride — 5.0 g/L; glucose — 1.0 g/L; monopotassium phosphate (KH2PO4) — 2.0 g/L; phenol red — 0.012 g/L; urea — 20.0 g/L; 100 ml dH2O; pH 6.8–6.9, sterilized by filtration. Solution II: autoclaved 1.7% agar. One hundred milliliters of solution I was added to solution II, cooled down to 50–55 °C, poured into sterile tubes, and finally cooled down in an inclined position to obtain a sloping column of the medium (yellow appearance). Bacterial cultures were inoculated onto the surface of the Christensen’s medium in tubes and incubated at 37 °C. Urease activity was detected visually after 2, 4, 6, and 24 h of incubation and determined as a shift of medium’s color from yellow to red-violet.
2.8 Carbapenemase Activity
Carbapenemase activity was measured using the disk diffusion test (DD-test).
2.9 Disk Diffusion Test
The test was performed according to the EUCAST (The European Committee on Antimicrobial Susceptibility Testing) standards [EUCAST clinical breakpoint tables for interpretation of MICs and zone diameters Version 11.0, valid from 2021–01-01]. Bacterial cultures were grown in Muller-Hinton (MH) broth at 37 °C for 18–24 h. Inoculates were prepared by resuspending cultures in sterile PBS at OD595 = 1.25 (correlates with a McFarland value of 0.5 or 1.5 × 108 CFU/ml). Bacterial suspension was inoculated on the MH plate by streaking in three directions using a sterile cotton swab. Disks with antibiotics (meropenem and imipenem, 10 μg per disk, BioRad) were placed on the MH agar medium immediately and the inoculated plates were incubated at 35 ± 1 °C for 16–20 h. After incubation, the diameter of each bacterial growth inhibition zones was measured, and the sensitivity category was evaluated according to EUCAST 2021 recommendations. Carbapenem-susceptible strain P. aeruginosa ATCC 27,853 was used as a control.
2.10 Real-time PCR
The detection of metal-β-lactamase (MBL) of molecular class B (metal lactamase: VIM, IMP, NDM) encoding genes was performed by Real-time PCR using the AmpliSense MDRMBL-FL hybridization-fluorescence detection kits (Interlab service, Russia). Genomic DNA was isolated from bacterial cells using a commercial GeneJetTM DNA Purification Kit (Fermentas, Thermo Scientific); all steps were performed according to the manufacturer’s protocol. The Real-time PCR mix (10 μl) contained the following: PCR mixture-2-FRT — 3.8 μl; TaqF polymerase — 0.2 μl; PCR mix-1-FRT MBL — 4 μl; internal control — 1 μl; DNA sample — 1 μl. Amplification was carried out using the protocol: stage 1 — 95 °C—15 min, 1 cycle; stage 2 — 95 °C—5 s, 60 °C—20 s, 5 cycles, 72° C—15 s; stage 3 — 95° C—5 s, 60° C—30 s, 40 cycles, with a change in fluorescence (FAM, HEX/JOE, ROX, Cy5), 72 °C—15 s. The internal DNA included in the kit was used as a control.
3 Results and Discussion
Catheter-associated biofilms play a crucial role in the development and persistence of infections. Considering this, studying biofilms, especially, formed by pathogenic bacteria, is highly important not only for the understanding of the physiology of biofilms and their regulation but for Medicine and healthcare to identify new strategies for infection treatment. In our study, we focused on one of the most clinically important pathogens P. aeruginosa associated with urinary catheters, and aimed to analyze its antibiotic resistance.
3.1 Identification of Bacterial Biofilms Associated with the Surface of Urological Catheters
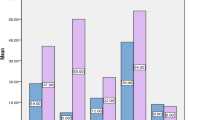
Urinary tract indwelling catheters were analyzed for the presence of biofilms. Eight samples of catheters were obtained from patients with urinary tract diseases including bladder stones, prostatic hyperplasia, urinary retention, and acute tubulointerstitial nephritis. Catheter samples were stained with CV to determine biofilm presence. Bacterial biofilms were detected on 6 out of the 8 studied catheter samples. Three samples had low-density biofilms, two samples were characterized as having medium-density biofilms, and only one sample exhibited a high-density biofilm (Table 1).
The morphology and biofilm composition of the catheter sample with the high-density biofilm (catheter No. 9, Table 1) was analyzed using scanning electron microscopy (SEM). Scanning electron microscopy revealed the presence of a heterogeneous matrix on the inner and outer surfaces of the catheter (Figs. 1 and 2). Rod-shaped and coccoid bacterial cells, matrix fragments, inclusions of blood cells, and salt crystals were observed both on the inner and the outer layer of the catheter (Fig. 1A, B; Fig. 2).
Scanning electron microscopy of the inside surface of the urinary catheter №9. Cocciform and rod-shaped bacterial cells are submerged into extracellular matrix. A Magnification × 10,000; scale bar 1 μm; B magnification × 500; scale bar 2 μm. White arrows indicate bacterial cells; black arrows indicate human red blood cells
As far as urological catheters directly contact with the patient’s internal tissues, host blood cells and salt crystals derived from the urea and other inclusions can be detected in bacterial biofilm structure [21]. Overall, urinary catheterization induces fibrinogen release into the bladder as part of the inflammatory response. This fibrinogen can accumulate both on the bladder surface and catheter surface. For instance, it was shown that Enterococcus faecalis cells attach to fibrinogen-coated catheters more efficiently than to the fibrinogen-free surfaces and use it for growth as the source of nutrients, enhancing biofilm development on the catheter [22].
3.2 Isolation and Identification of Catheter-Associated Biofilm-Forming Microorganisms
We focused on the isolation of Pseudomonas spp., especially P. aeruginosa due to its vital significance in the CAUTI. Among 25 obtained bacterial isolates, several strains had a blue-green pigmentation after 3 days of cultivation at RT which allowed us to consider these strains as candidate representatives of Pseudomonas genus. MALDI-TOF MS protein profile analysis confirmed that three of the isolated strains belong to P. aeruginosa (strains numbers 96345, 96,347, and 96,349) (score value > 2.4) (Table 2). All strains had a rod-shaped cell morphology and 3–4-μm long cells, which is usual for Pseudomonas genus (Fig. 3) [23]. All three P. aeruginosa strains were isolated from different catheter samples. Also, P. aeruginosa 96,345 was isolated from a catheter on which biofilm formation was not detected (Table 1).
Although the majority of bacteria isolated from urinary catheters belongs to the Enterobacteriaceae family (the most common group associated with the human urogenital tract), P. aeruginosa has an extremely high value in urinary tract infections [24]. Overall, P. aeruginosa is involved in the development of different human diseases including dental caries, otitis media, cystic fibrosis pneumonia, chronic wound infections, musculoskeletal infections, biliary tract infection, bacterial prostatitis, urinary tract infection, and a wide range of medical device-related infections. Additionally, chronic bacterial prostatitis and medical device–related infections are prominently caused by P. aeruginosa [8]. Pseudomonas aeruginosa is one of the most environmentally significant species among the genus Pseudomonas, widespread in nature. However, the increasing importance of P. aeruginosa strains acquired in medicine in nature, due to its high antimicrobial and broad spectrum resistance virulence factors [25]. P. aeruginosa is an opportunistic pathogen causing severe nosocomial infections in people with weakened immunity; it causes several types of infections, including dermatitis, endocarditis and infections of the urinary tract, eyes, ears, bones, joints, respiratory tract. Patients with cystic fibrosis who are extremely susceptible to Pseudomonas infections, have poor prognosis and high mortality. Urinary tract infections (UTIs) are among the most common bacterial infections which annually affect about 150 million people in all the world. UTIs are a significant cause of morbidity in boys, older men and women of all ages.
Thus, the study of infections caused by this microorganism is the highest priority task of modern medicine.
3.3 Urease Activity of Catheter-Associated P. aeruginosa
Salt crystals from the host’s internal environment can often be found in the biofilm matrix [23]. Presumably, the formation of salt crystals in the urogenital tract can be initiated by bacterial ureases. The pH value of human urine under normal conditions is usually 6.0–7.5 with a tendency to slightly acidic values, with a normal range from 4.5 to 8.0. Higher urine pH values of 8.5 or 9.0 indicate infections induced by urea-splitting microorganisms, such as Proteus, Klebsiella, and Ureaplasma urealyticum. Therefore, an asymptomatic patient with a high urine pH means UTI regardless of the other urine test results. Alkaline pH can also lead to the formation of struvite kidney stones, which are also known as “infection stones” [26]. Urease-producing pathogens hydrolyze host urea with the formation of ammonium (NH4+) and hydrogen (H+) ions, which leads to pH increasing and changes in the urine composition. These reactions result in the sedimentation of struvite (ammonium magnesium phosphate) and apatite (calcium phosphate) on the surface of urinary tract epithelium, as well as on the surface of catheters and stents.
As mentioned above, the presence of salt crystals was identified in biofilm samples using SEM (Fig. 2). Hence, a urease activity of the isolated Pseudomonas strains was studied to confirm the role of biofilm-associated bacteria in salt crystals formation. However, high urease activity was determined for only one strain, P. aeruginosa 96,349. We suppose that the high urease activity causes the formation of salt crystals associated with the biofilm formed by this strain, which also correlates with the density of the biofilm.
3.4 Antibiotic Resistance of Catheter-Associated Biofilm-Forming P. aeruginosa Strains
Antibiotic resistance of P. aeruginosa strains 96,345, 96,347, and 96,349 was investigated using both microbiological and molecular methods. The growth of P. aeruginosa 96,345 was inhibited by by imipenem in high exposure of antibiotic (growth inhibition zone was 33 mm that is between sensitivity and resistance breakpoints) but not by meropenem (growth inhibition zone was 11 mm) (Fig. 4A). In contrast, it was shown that two P. aeruginosa strains (96,347 and 96,349) exhibit high resistance to β-lactam antibiotics, particularly carbapenems (imipenem and meropenem). Growth inhibition zones were not observed for these strains (Fig. 4B, C).
The DD-test is usually recommended for the qualitative analysis of antibiotic resistance. Moreover, this method provides no detailed information on the mechanisms of resistance. Instead, qPCR analysis is commonly adopted for the detection of wide-spread beta-lactamase genes such as KPC, NDM, OXA-48, VIM, IMP, and OXA-23 carbapenemases. Generally, antibiotic resistance of many Gram-negative bacteria can be associated with other mechanisms including efflux pumps and reducing of porin number.
However, according to many studies on antibiotic resistance [8, 27, 28], P. aeruginosa usually shows high β-lactamase activity. Thus, we performed a qPCR analysis to detect genes of the most widespread types of these enzymes, metallo-β-lactamase (NDM—metallo-β-lactamase of New Delhi, VIM- and IMP-types). The VIM-type metallo-β-lactamase gene was detected in P. aeruginosa 96,347 and 96,349 strains but not in the strain 96,345, which correlated with the DD-test results (Fig. 5).
VIM- metallo-β-lactamase is extensively widespread in different bacteria including Pseudomonas spp., Acinetobacter spp., and members of the Enterobacteriaceae family [28]. Moreover, carbapenemase activity is one of the most common resistance mechanisms in the family Pseudomonadaceae. While carbapenemases belonging to class A (NMC/IMI, SME, and KPC) and class D (several types of OXA) are mainly detected in bacteria of the genus Acinetobacter, class B which includes zinc-depended metalloenzymes are often found in Pseudomonas spp. [29, 30]. All types of carbapenemases pose a serious threat to the therapeutic value of all β-lactam antibiotics. Particularly, the distribution of metallo-β-lactamase among the major Gram-negative human pathogens (P. aeruginosa, Acinetobacter spp., Enterobacteriaceae) represents a high clinical and epidemiological importance. Therefore, the presence of the VIM-type metallo-β-lactamase genes in the genomes of studied isolates confirmed the distribution of these enzymes among Pseudomonas sp. Moreover, this fact could allow us to suppose that the VIM metallo-β-lactamases play the leading role in the high antibiotic resistance and pathogenesis of studied CAUTI isolates.
4 Conclusions
Bacterial biofilm formation is one of the most serious problems in infectious diseases control because of the increased antibiotic resistance in biofilms comparing to free-living bacteria. In this study, we reported on the three biofilm-associated P. aeruginosa strains isolated from urinary tract catheters. The analysis of polymicrobial catheter-associated biofilm density, and also urease activity, and the distribution of β-lactamase genes in isolated strains confirmed the high pathogenic potential of the isolated Pseudomonas strains. All P. aeruginosa strains demonstrated antibiotic resistance to imipenem and meropenem according to VIM-type β-lactamase gene expression. P. aeruginosa 96,349 showed urease activity, while P. aeruginosa 96,345 was isolated from a catheter sample for which biofilm formation was not detected. Overall, the 96,345 strain was sensitive to high exposure of imipenem and did not have genes of β-lactamases. Therefore, we showed that although P. aeruginosa is one of the bacterial pathogens associated with CAUTI, there can be intraspecies variations in antibiotic resistance and pathogenicity factors. This calls for further studies on biofilm formation in vitro and the distribution of other pathogenicity factors in isolates of P. aeruginosa. The data presented contributes to the knowledge on the role of P. aeruginosa in CAUTI.
Data Availability
Not available.
References
Parker, V., Giles, M., Graham, L., Suthers, B., Watts, W., O’Brien, T., & Searles, A. (2017). Avoiding inappropriate urinary catheter use and catheter-associated urinary tract infection (CAUTI): A pre-post control intervention study. BMC Health Services Research, 17, 314.
Domenech, M., Ramos-Sevillano, E., García, E., Moscoso, M., & Yuste, J. (2013). Biofilm formation avoids complement immunity and phagocytosis of Streptococcus pneumoniae. Infection and Immunity, 81(7), 2606–2615.
Singha, L. P., Kotoky, R., & Pandey, P. (2017). Draft genome sequence of Pseudomonas fragi Strain DBC, which has the ability to degrade high-molecular-weight polyaromatic hydrocarbons. Genome Announcements, 5(49), e01347-e1417.
Williamson, W., Fuld, J., Westgate, K., Sylvester, K., Ekelund, U., & Brage, S. (2012). Validity of reporting oxygen uptake efficiency slope from submaximal exercise using respiratory exchange ratio as secondary criterion. Pulmonary Medicine, 2012, 874020.
Sommer, L. M., Johansen, H. K., & Molin, S. (2020). Antibiotic resistance in Pseudomonas aeruginosa and adaptation to complex dynamic environments. Microbial Genomics, 2020, 6. https://doi.org/10.1099/mgen.0.000370
Madaha, E. L., Mienie, C., Gonsu, H. K., Bughe, R. N., Fonkoua, M. C., Mbacham, W. F., Alayande, K. A., Bezuidenhout, C. C., & Ateba, C. N. (2020). Whole-genome sequence of multi-drug resistant Pseudomonas aeruginosa strains UY1PSABAL and UY1PSABAL2 isolated from human broncho-alveolar lavage, Yaounde´, Cameroon. PLoS ONE, 15(9), e0238390. https://doi.org/10.1371/journal.pone.0238390
Olsen, I. (2015). Biofilm-specific antibiotic tolerance and resistance. European Journal of Clinical Microbiology and Infectious Diseases, 34, 877–886.
Tolker-Nielsen, T. (2014). Pseudomonas aeruginosa biofilm infections: From molecular biofilm biology to new treatment possibilities. APMIS Supplementum, 138, 1–51. https://doi.org/10.1111/apm.12335
Tolker-Nielsen, T. (2015). Biofilm development. ASM. Microbiol Spectrum, 3(2), 3.2.21, MB-0001–2014. https://doi.org/10.1128/microbiolspec.MB-0001-2014.
Brooun, A., Liu, S., & Lewis, K. (2000). A dose-response study of antibiotic resistance in Pseudomonas aeruginosa Biofilms. Antimicrobial Agents and Chemotherapy, 44(3), 640–646.
Ciofu, O., & Tolker-Nielsen, T. (2019). Tolerance and resistance of Pseudomonas aeruginosa biofilms to antimicrobial agents—how P. aeruginosa can escape antibiotics. Frontiers in Microbiology, 10, 913. https://doi.org/10.3389/fmicb.2019.00913
Hengzhuang, W., Ciofu, O., Yang, L., Wu, H., Song, Z., Oliver, A., & Høiby, N. (2013). High β-lactamase levels change the pharmacodynamics of β-lactam antibiotics in Pseudomonas aeruginosa biofilms. Antimicrobial Agents and Chemotherapy, 57(1), 196–204.
Gallant, C. V., Daniels, C., Leung, J. M., Ghosh, A. S., Young, K. D., Kotra, L. P., & Burrows, L. L. (2005). Common β-lactamases inhibit bacterial biofilm formation. Molecular Microbiology, 58(4), 1012–1024. https://doi.org/10.1111/j.1365-2958.2005.04892.x
Wu, F., Chen, L., Wang, J., & Alhajj, R. (2014). Biomolecular networks and human diseases. BioMed Research International, 2014, 363717.
Bizzini, A., & Greub, G. (2010). Matrix-assisted laser desorption ionization time-of-flight mass spectrometry, a revolution in clinical microbial identification. Clinical Microbiology & Infection, 16, 1614–1619.
Lau, S. K. P., Lam, C. S. K., Ngan, A. H. Y., Chow, W.-N., Wu, A. K. L., & Tsang, D. N. C. (2016). Matrix-assisted laser desorption ionization time-of-flight mass spectrometry for rapid identification of mold and yeast cultures of Penicillium marneffei. BMC Microbiology, 16, 36. https://doi.org/10.1186/s12866-016-0656-0
Merritt, J. H., Kadouri, D. E., & O’Toole, G. A. (2005). Growing and analyzing static biofilms. Current Protocols in Microbiology, 01, Unit-1B .1. https://doi.org/10.1002/9780471729259.mc01b01s00
Stepanovic, S., Vukovic, D., Hola, V., Di Bonaventura, G., Djukic, S., C´Irkovic, I., & Ruzicka, F. (2007). Quantification of biofilm in microtiter plates: overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS, 115, 891–899.
Van Laar, T. A., Chen, T., You, T., & Leung, K. P. (2015). Sublethal concentrations of carbapenems alter cell morphology and genomic expression of Klebsiella pneumoniae biofilms. Antimicrobial Agents and Chemotherapy, 59, 1707–1717.
Cui, M.-J., Teng, A., Chu, J., & Cao, B. (2022). A quantitative, high throughput urease activity assay for comparison and rapid screening of ureolytic bacteria. Environmental Research, 208, 112738.
van Gennip, M., Christensen, L. D., Alhede, M., Qvortrup, K., Jensen, P. Ø., Høib, N., Givskov, M., & Bjarnsholt, T. (2012). Interactions between polymorphonuclear leukocytes and Pseudomonas aeruginosa biofilms on silicone implants in vivo. Infection and Immunity, 80(8), 2601–2607.
Donlan, R. M. (2002). Biofilm: Microbial life on surface. Emerging Infectious Diseases, 8, 881–890.
Chauhan, V., Howland, M., & Wilkins, R. (2012). A comparitive assessement of cytokine expression in human-derived cell lines exposed to alpha particles and X-rays. The Scientific World Journal, 2012, 609295.
Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nature Reviews Microbiology, 13(5), 269–284. https://doi.org/10.1038/nrmicro3432
Abbas, H. A., El-Ganiny, A. M., & Kamel, H. A. (2018). Phenotypic and genotypic detection of antibiotic resistance of Pseudomonas aeruginosa isolated from urinary tract infections. African Health Sciences, 18(1), 11–21.
Bono, M. J., Leslie, S. W., Reygaert, W. C. (2022). Urinary tract infection. [Updated November 28, 2022.]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470195/
Glen, K. A., & Lamont, I. L. (2021). β-lactam resistance in Pseudomonas aeruginosa: Current status, futureprospects. Pathogens, 10, 1638. https://doi.org/10.3390/pathogens10121638
Shevchenko, O. V., Mudrak, D. Y., Skleenova, E. Y., Kozyreva, V. K., Ilina, E. N., Ikryannikova, L. N., Alexandrova, I. A., Sidorenko, S. V., & Edelstein, M. V. (2007). First detection of VIM-4 metallob-lactamase-producing Escherichia coli in Russia. Clinical Microbiology & Infection, 18, 214–217.
Halat, D. H., & Moubareck, C. A. (2022). The current burden of carbapenemases: Review of SIGNIfiCANT PROPERTIES AND DISSEMINATION AMONG GRAM-NEGATIVE BACTERIA. Antibiotics, 9, 186. https://doi.org/10.3390/antibiotics9040186
Queenan, A. M., & Bush, K. (2007). Carbapenemases: The Versatile -Lactamases. Clinical Microbiology Reviews, 20(3), 440–458.
Acknowledgements
This paper has been supported by the Kazan Federal University Strategic Academic Leadership Program (PRIORITY-2030). The authors would like to thank the Laboratory of Clinical Bacteriology at the Republican Clinical Hospital of the Republic of Tatarstan for the support in the work with clinical samples.
Funding
This work was funded by the Russian Foundation for Basic Research (research project no.20–315-90093).
Author information
Authors and Affiliations
Contributions
All authors contributed significantly to the current work. L.V. and M.S. designed the experiments. N.K., L.V., E.S., D.K., and V.V. performed the experiments. L.V., N.K., Z.G., and M.S. analyzed data. Z.G. provided the clinical material (catheters). L.V. and N.K. wrote the paper with contributions from all other authors. Correspondence and requests for materials should be addressed to L.V. or M.S. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Research Involving Humans and Animals Statement
None.
Informed Consent
The materials used in this study do not contain personal data of patients. Informed consent was obtained from all the patients recruited in this study. Clinical samples were provided in accordance with the university ethical regulations.
Conflict of Interest
All authors’ individual rights were respected and information regarding data, pictures and the overall draft was made with their concern.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khabipova, N., Valeeva, L., Shaidullina, E. et al. Antibiotic Resistance of Biofilm-Related Catheter-Associated Urinary Tract Isolates of Pseudomonas aeruginosa. BioNanoSci. 13, 1012–1021 (2023). https://doi.org/10.1007/s12668-023-01123-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12668-023-01123-z