Abstract
Breast cancer is the most common cancer among women worldwide. Common disadvantages of chemotherapy, such as drug resistance, nausea, and vomiting, have encouraged researchers to use herbal remedies. In this study, constituents of Mentha piperita essential oil were identified using GC-MS analysis with five major ingredients of menthol (31.0%), menthone (22.1%), camphane (7.0%), menthofuran (6.0%), and iso-menthone (5.8%). The essential oil anticancer activity was evaluated at various incubation periods (24, 48, and 72 h) against three human breast cancer cell lines. After that, nanoemulsions of M. piperita were prepared, and long- and short-time stability tests were also performed. The anticancer effect of the best nanoemulsion with a mean droplet size of 136 ± 2 nm (PDI 0.3 and SPAN 0.8) was significantly better than that of non-formulated essential oil. Interestingly, the obtained effect from nanoemulsion with an exposure time of 24 h was significantly better than essential oil even within 72-h exposure time. M. piperita possesses an antiemetic effect, and by preparation of its nanoemulsion dosage form, its anticancer effect was also improved. Therefore, this green nanoemulsion could be used as an anticancer agent for further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Breast cancer is the most common cancer among women worldwide, and with a 15.4% mortality rate; it is also the second leading cause of death in developed countries after lung cancer [1, 2]. Many approaches are currently used to treat cancers, such as surgery, chemotherapy, and radiotherapy [3, 4]. Drug resistance, recurrence of the disease, and metastasis to other parts of the body are significant causes of cancer treatment failure [5].
In recent years, the investigation of essential oils’ anticancer properties (EOs) has received more attention worldwide. For example, the half-maximal inhibitory concentration (IC50) of EOs of Cinnamomum zeylanicum, Citrus limon, and Citrus paradise on two types of human breast cancer cell lines, including MCF-7 and MDA-MB-231, were reported: 14 and 16.9 μg/mL, 94 and > 100 μg/mL, and 79.7 and 50.6 μg/mL, respectively [6]. Besides, the anticancer effects of Mentha piperita (MPEO) against some cell lines such as Hep-2 cell (human epidermoid cancer), K562 (human chronic myelogenous leukemia), and SGC-7901 (human gastric cancer cell line) were reported [7, 8].
Nausea and vomiting are two common side effects of chemotherapy drugs; 70–80% of patients experience this condition [9, 10]. Interestingly, antiemetic properties of some EO, such as MPEO after chemotherapy drugs, have been reported [11,12,13]. For instance, a randomized, double-blind clinical trial study was performed previously on those suffering any cancer diagnosis and receiving chemotherapy on an outpatient basis. The intervention group received routine medications (granisetron, dexamethasone, or metoclopramide) plus MPEO capsules (containing two drops and filled with sugar). In contrast, the control group received only routine medications. A significant reduction was reported in the intensity and number of emetic events than the control, and no adverse effects were reported [13].
Some breast cancer subtypes have been proposed based on hormone receptor (HR) and human epidermal growth factor receptor (HER2) [14, 15]. Luminal A (HR+, HER2−) is the most common subtype of breast cancer. The basal subtype (HR−, HER2−) is due to a lack of biomarkers’ expression and is biologically aggressive, and often has a poor prognosis. Claudin-low (HR−, HER2−) is classified as a Basal subgroup due to a lack of biomarkers’ expression. However, due to differences in the regulation of some of the other markers, it is classified separately [16,17,18].
In this study, the anticancer effect of MPEO on all the mentioned subtypes of human breast cancer cell lines, including MCF-7 (Luminal A), MDA-MB-468 (Basal), and MDA-MB-231 (Claudin-low), was investigated. After that, we had attended to improve the anticancer effect of MPEO by formulating MPEO to the nanoemulsion dosage form.
2 Materials and Methods
2.1 Materials
Zardband Pharmaceutical Company (Iran) provided Mentha piperita EO. Tween 20 and ethanol were bought from Merck Chemicals (Germany). MTT powder (thiazolyl blue tetrazolium bromide) and PBS tablets (phosphate-buffered saline), and FBS (fetal bovine serum) were bought from Sigma (USA). Penicillin and streptomycin, trypsin, DMEM media culture, and DMSO (dimethyl sulfoxide) were purchased from Shellmax (China). Breast cancer cell lines, including MCF-7 (ATCC HTB-22), MDA-MB-231 (ATCC: HTB-26), and MDA-MB-468 (ATCC: HTB-132), were supplied from the Tehran Institute of Pasteur (Iran).
2.2 GC-MS procedure
Components of MPEO were identified by GC-MS analysis using a 6890 Network GC system coupled with a 5973 network mass selective detector (Agilent Technologies, Santa Clara, CA, USA). The separation of MPEO components was carried out on HP-1MS silica-fused columns (30-m length; 0.25 mm i.d.; and 0.25 μM film thickness. The GC-MS column temperature was programmed as follows: the initial temperature was set at 40 °C and fixed for 1 min and increased with 3 °C/min to the final heat of 250 °C and held for 60 min. The temperature of the injection port and detector fixed at 250 and 230°C, respectively. Other instrument parameters, including split flow (25 mL/min), septum purge (6 mL/min), and column flow rate (1 mL/min), were set, as well. Helium gas with a purity of 99.9% was used as the carrier gas.
Ingredients of the MPEO were identified as described in our previous study [19]. In brief, by comparing obtained retention indices (RIs) with reference to a homologous series of C6–C27 n-alkanes, components were identified. The identification was also confirmed by comparison of their mass spectra with those stored in the Wiley7n.l MS computer library. The linear temperature programmed RIs of all the constituents were calculated from the gas chromatogram by interpolating bracketing n-alkanes using Eq. 1. We used the peak area normalization procedure for the quantitative determination of the compounds in MPEO.
where z is the number of carbon atoms in the smaller n-alkane, tR(i), tR(z), and tR(z+1) are the retention times of the desired compound, the smaller n-alkane, and the larger n-alkane, respectively.
2.3 Preparation of Nanoemulsion
The spontaneous approach was conducted for the development of nanoemulsions. MPEO (25 μL) and different amounts of tween 20 (10–200 μL) and ethanol (10–200 μL) were mixed at 500 rpm (5 min, room temperature) to form a homogeneous solution. Then, the final volume of samples reached 5000 μL by the dropwise addition of PBS. Then, samples were stirred at 2000 rpm for another 30 min to prepare nanoemulsion [20]. The best nanoemulsion (see Section 3.5.) was prepared using 25 μL MPEO, 10 μL tween 20, and 4965 μL PBS.
2.4 Characterization of the Prepared Nanoemulsions
2.4.1 Size Analyses
A nanoparticle size analyzer (HORIBA sz-100 version 2.20) was used to determine the droplet size and droplet size distribution of the prepared nanoemulsions. In terms of medical nanotechnology, droplet size must be lower than 200 nm [21]. The dispersity in droplet size was presented by two indices, polydispersity index (PDI) and droplet size distribution (SPAN). PDI was calculated using Eq. 2.
Where σ is the standard deviation of the nanodroplet’s mean diameter, and d is the mean diameter of droplets. The acceptable value for PDI should be less than 0.7 [22]. The SPAN value was measured by Eq. 3.
Where D10, D50, and D90 were diameters where 10, 50, and 90% of droplets were smaller than those values. SPAN value of less than 1 indicated a narrow size distribution [23]. Therefore, all prepared nanoemulsions with a droplet size of < 200 nm and acceptable amounts of PDI and SPAN were selected for stability tests.
2.5 Stability Tests for Selected Nanoemulsions
2.5.1 Short-term Analysis
Three examinations were carried-out for short-term analysis of the stability of nanoemulsions. For each test, at least 3 samples with a volume of 5 mL were prepared. Centrifugation, the nanoemulsions were centrifuged for 30 min at three temperatures of − 4, 4, and + 25 °C (22,000 g). The heating-cooling cycle and freeze-thaw cycle were performed to investigate nanoemulsions’ stability in the heat and freeze conditions. In the heating-cooling cycle, the nanoemulsions for 6 successive cycles of 48 h were stored at + 45 °C (Bain-Marie) and + 4 °C (refrigerator) [24]. While in the freeze-thaw cycle, the nanoemulsions were placed successively at ambient temperature (+ 25 °C) and freezer (− 21 °C) for 6 cycles of 48 h [25].
After performing each of the mentioned tests, nanoemulsions were subjected to DLS analysis for investigating any significant change in their droplet size, PDI, and SPAN. Nanoemulsions that passed short-term stability tests were selected for long-term stability tests.
2.5.2 Long-term Analyses
The selected nanoemulsions were placed in the refrigerator (+ 4 °C) and room temperature (+ 25 °C) for 6 months. Nanoemulsions were then visually checked for any creaming, sedimentation, or biphasic state [26]. Stable nanoemulsions were selected for investigation of the anticancer effect.
2.6 Assessment of Anticancer Activity of MPEO and Selected Nanoemulsions
The cell lines were cultured in DMEM complete medium (containing FBS 10% and penicillin-streptomycin 1%) and incubated at 37 °C and CO2 5%. The samples’ anticancer activity (serial dilution of MPEO and selected nanoemulsions) was investigated using MTT assay. First, 100 μL of each cell line was filled in 96-well plates (separately) and incubated for 24 h for attaching and reached 70–80% confluence. After that, the wells’ liquid content was discarded, and 150 μL of DMEM complete medium and 50 μL of samples were added to each well. The plates were then incubated at 3 different times (24, 48, and 72 h) separately.
After that, the wells’ liquid content was replaced with 90 μL DMEM and 10 μL MTT solution (0.5 mg/mL) and incubated for another 4 h. Then, 100 μL/well of DMSO was added to dissolve formed formazan crystals. Finally, absorbance (A) of wells was read at 570 nm using a plate reader (Synergy HTX Multi-Mode Reader, USA). The cell viability at each well was calculated by Eq. 4. The tests were carried out in triplicates; three wells in each plate were considered control groups filled with 200 μL DMEM complete medium.
2.7 Statistical Analysis
All tests were repeated at least three times, and the final values were reported as mean ± SD. Drawing of charts and calculating means and standard deviations were performed with Excel v. 2010. The calculation of IC50 was performed using CalcuSyn version 2.11. The anticancer activity of MPEO at different concentrations and nanoemulsions was compared using one-way ANOVA and independent-sample t test, using SPSS software (v.22, IBM, USA). The confidence interval in this study was considered 95%.
3 Results and Discussions
3.1 Ingredients of MPEO
Constituents of MPEO were identified using GC-MS analysis (see Table 1). Five major components are menthol (31.0%), menthone (22.1%), camphane (7.0%), menthofuran (6.0%), and iso-menthone (5.8%).
3.2 Anticancer Activity of MPEO
Figure 1 shows the anticancer properties of MPEO at incubation times of 24, 48, and 72 h against 3 human breast cancer cell lines (MCF-7, MDA-MB-231, and MDA-MB-468). In 24 h (Fig. 1A), the viabilities of all cell lines were higher than 50%, concluding that the anticancer activity of MPEO at 24 h was not considerable. However, by increasing incubation time to 48 and 72 h, effectiveness was improved (Fig. 1B and C). Interestingly, all examined cell lines’ viability after 72-h exposure with MPEO 2500 μg/mL decreased to lower than 10%. Besides, observed IC50s at different incubation periods are listed in Table 2. The best IC50s were observed at 72 h; MCF-7: 165 μg/mL, MDA-MB-231: 25 μg/mL, and MDA-MB-468: 2536 μg/mL, respectively. Furthermore, as Figs. 1A, B, and C show, MPEO 1250 μg/mL was the lowest concentration that reduced at least 50% viability of all three cell lines. Therefore, we tried to increase the efficiency of MPEO and reduce the exposure time by formulating MPEO to nanoemulsion.
Reviewing the literature, the authors were found some reports on the anticancer properties of MPEO. In one study, the anticancer effect of MPEO on MCF-7 and LNCaP (human breast and prostate cancer cell lines, respectively) was confirmed [27]. In another one, MPEO showed proper anticancer activities against cancer cell lines of SPC-A1 (lung), K562 (blood), and SGC-7901 (gastric) with IC50s of 11, 16, and 38 μg/mL, respectively [8].
Many reports on the anticancer properties of EOs against these cell lines have been found in the literature. For instance, IC50s of EOs of Pistacia lentiscus and Blepharocalyx salicifolius against MDA-MB-231 were reported as 616 and 46 μg/mL, respectively [28, 29]. These values for other EOs on MCF-7 are as follows: Hedyosmum spruce 32 μg/mL and Nepeta cataria 500 μg/mL [30, 31]. Interestingly, only two reports were found on the anticancer effect of EOs against MDA-MB-468; IC50s of EOs of Kelussia odoratissima, Peristrophe bicalyculata, and Borreria verticillata were reported as 85, 66.6, and 20.4 μg/mL, respectively [32, 33].
3.3 Prepared Nanoemulsions
Details of prepared formulations are listed in Table 3. The MPEO was formulated using tween 20 and ethanol as common surfactant and co-surfactant, respectively [34]. Tween 20 is a non-ionic and non-toxic surfactant-containing fatty acid ester of sorbitol and its anhydrides [35]. Amongst the prepared nanoemulsions, only two nanoemulsions (F1 and F9) had proper characteristics; mean droplet size < 200 nm, SPAN < 1, and PDI < 0.7. Their droplet sizes were 136 ± 2 and 11 ± 3 nm, respectively. The observed PDI and SPAN for F1 were 0.3 and 0.8; these values for F9 were 0.3 and 0.5, respectively. Therefore, these nanoemulsions were selected for stability tests (their DLS diagrams are given in Fig. 2).
In the preparation of nanoemulsions, an equilibrium between the oil phase (a mixture of oil and surfactant/s) and aqueous phases must occur [20, 34]. Co-surfactant, especially ethanol and isopropyl alcohol, is also sometimes used to reach equilibrium. Because the preparation and optimization of nanoemulsions are an experimental process, many research types on the use or non-use of co-surfactants in such processes have been reported. In our previous report, the best nanoemulsion of Dill EO was prepared only with tween 20, i.e., without using co-surfactant [34]. In another study, ethanol was used for optimizing nanoemulsion of artemether (medication used for the treatment of malaria) [36]. Alternatively, in another report, nanoemulsion of eugenol was optimized using isopropyl alcohol as a co-surfactant [24].
3.4 Stability of the Chosen Nanoemulsions
No significant changes were observed in droplet size, PDI, and SPAN of selected nanoemulsions (F1 and F9) after short-time stability tests, including centrifugation, heating-cooling, and freeze-thaw cycles. Moreover, no creaming, deposition, and biphasic conditions were observed in F1 and F9 after completing long-time stability tests (data not shown). Therefore, their stabilities were considered excellent. Given the stability of the nanoemulsions in critical situations (short-time), it could be concluded that even if an accident occurs in the drug transport chain, the formulations remain stable.
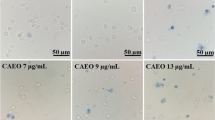
3.5 Anticancer Activity of Nanoemulsion
The anticancer properties of the selected nanoemulsions (F1 and F9) at a concentration of 1250 μg/mL as well as the anticancer effect of their ingredients, i.e., (F1(-oil) and F9(-oil), are depicted in Fig. 3(A, B, and C). Interestingly, F9(-oil), F1, and F9 showed excellent cytotoxicity against the whole of the cell lines at all three incubation periods; viabilities were decreased to < 5%. As depicted in Fig. 1A and B, MPEO (1250 μg/mL) could not decrease at least 50% in cell lines’ viabilities after 24- and 48-h incubation times. Even when the incubation time increased to 72 h, the viability of MDA-MB-468 remained at ~ 45% (Fig. 1C). In other words, the effectiveness of F9(-oil), F1, and F9 at incubation time 24 h was even better than that of MPEO at 72 h.
Besides, F1(-oil) did not have a considerable effect on cell lines at 24, 48, and 72 h; viabilities of all cell lines at all incubation times were higher than 95%. Therefore, it is concluding that components of F1 have a negligible impact on its final performance. Moreover, the anticancer effects of MPEO and F1 have been investigated at the same concentration (1250 μg/mL); the only difference between them was the size of the EO’s dispersed droplets. This improvement was related to decreasing MPEO droplet size, which led to better penetration into the cells [37, 38].
From the literature, in some researches, EO-based nanoemulsions were used as carriers for chemical drugs, including ifosfamide and mitomycin C [39, 40]. However, some studies on the anticancer properties of EO-based nanoemulsions against breast cancer cell lines have been reported. However, unlike this study, only one cell line was considered (MCF-7). For instance, a nanoemulsion of Prunus cerasus EO with a droplet size of 36.5 nm was reported. The nanoemulsion was prepared using the ultrasonication method, and its cytotoxicity (50 μg/mL) on the MCF-7 cell line was examined; viability was decreased to around 50% after 72-h incubation time [41]. Because the anticancer properties of the EO and the constituent of nanoemulsion have not been reported, the effect of formulating EO into nanoemulsion dosage form could not be assessed accurately. To prepare the mentioned nanoemulsion, the EO was first formulated (using polysorbate 20, polysorbate 80, polyethylene glycol) into an emulsion with a droplet size of 1338 ± 0.71 nm. Then, the emulsion was exposed to ultrasonic frequency (20 kHz) at different intervals (14, 10, 6, 2, and 0 min); droplets size was reduced to 36.5 nm after 14 min [41].
In another study, the EO of Nigella sativa (3% v/v) was formulated with polysorbate 80 (droplet size 300 nm). The emulsion was then sonicated (20 kHz) for 1 h; droplet size was reduced to 64.4 nm. The viability of the MCF-7 cell line after 48-h incubation with the nanoemulsion (100 μL/mL) was reduced to ~ 30%. Like the previously mentioned report, the anticancer effect of the EO was not reported [42].
Furthermore, exploiting ultrasound emulsification in preparation of nanoemulsions has some drawbacks; first, droplet size increases over time [43]. When ultrasonic power or exposure time increases, the droplet size of a fraction (e.g., EO) decreases in a dispersed phase; however, this phenomenon could lead to coalescence [44]. In this regard, the two mentioned nanoemulsions’ stability was not reported in a long time; P. cerasus (14 days) and N. sativa: ~ 6 days [42, 41]. However, this study’s prepared nanoemulsions (using spontaneous emulsification) were stable for at least 6 months.
4 Conclusions
Anticancer properties of MPEO were evaluated against three human breast cancer cell lines at three incubation periods (24, 48, and 72 h). Two nanoemulsions of MPEO with mean droplet sizes of 136.9 ± 2.0 and 11.5 ± 3.4 nm were selected as optimum samples; they sowed excellent stability in both short-time and long-time stability tests. Interestingly, the anticancer effect of the MPEO on the cell lines within 72-h exposure time was achieved in 24-h treatment by newly developed nanoemulsions; they could be used as anticancer agents for further investigation.
References
Ghoncheh, M., Pournamdar, Z., & Salehiniya, H. (2016). Incidence and mortality and epidemiology of breast cancer in the world. Asian Pacific Journal of Cancer Prevention, 17(S3), 43–46.
Movahedi, M., Haghighat, S., Khayamzadeh, M., Moradi, A., Ghanbari-Motlagh, A., Mirzaei, H., & Esmail-Akbari, M. (2012). Survival rate of breast cancer based on geographical variation in Iran, a national study. Iranian Red Crescent Medical Journal, 14(12), 798.
Suganuma, M., Saha, A., & Fujiki, H. (2011). New cancer treatment strategy using combination of green tea catechins and anticancer drugs. Cancer Science, 102(2), 317–323.
Hassanvand, A., Zare, M. H., Shams, A., Nickfarjam, A., Shabani, M., & Rahavi, H. (2019). Investigation of the effect of radiosensitization of tungsten oxide nanoparticles on AGS cell line of human stomach cancer in megavoltage photons radiation. Journal of Nanostructures, 9(3), 563–578.
Housman, G., Byler, S., Heerboth, S., Lapinska, K., Longacre, M., Snyder, N., & Sarkar, S. (2014). Drug resistance in cancer: an overview. Cancers, 6(3), 1769–1792.
Powers, C., Osier, J., McFeeters, R., Brazell, C., Olsen, E., Moriarity, D., Satyal, P., & Setzer, W. (2018). Antifungal and cytotoxic activities of sixty commercially-available essential oils. Molecules, 23(7), 1549.
Abirami, S. G., & Nirmala, P. (2014). A comparative–invitro study of anticancer effect of Mentha piperita, Ocimum basilicum and Coleus aromaticus against human laryngeal epidermoid carcinoma (HEP-2) cell lines. Journal of Medicinal Plants Studies, 2(1), 6–9.
Sun, Z., Wang, H., Wang, J., Zhou, L., & Yang, P. (2014). Chemical composition and anti-inflammatory, cytotoxic and antioxidant activities of essential oil from leaves of Mentha piperita grown in China. PLoS One, 9(12), e114767.
Gottesman, M. M. (2002). Mechanisms of cancer drug resistance. Annual Review of Medicine, 53(1), 615–627.
Shipitsin, M., Campbell, L. L., Argani, P., Weremowicz, S., Bloushtain-Qimron, N., Yao, J., Nikolskaya, T., Serebryiskaya, T., Beroukhim, R., & Hu, M. (2007). Molecular definition of breast tumor heterogeneity. Cancer Cell, 11(3), 259–273.
Eghbali, M., Varaei, S., Yekaninejad, M., Mohammadzadeh, F., & Shahi, F. (2017). To what extend aromatherapy with peppermint oil effects on chemotherapy induced nausea and vomiting in patient diagnosed with breast cancer? A randomized controlled trial. Journal of Hematology & Thromboembolic Diseases, 5(6), 1–6.
Janelsins, M. C., Tejani, M. A., Kamen, C., Peoples, A. R., Mustian, K. M., & Morrow, G. R. (2013). Current pharmacotherapy for chemotherapy-induced nausea and vomiting in cancer patients. Expert Opinion on Pharmacotherapy, 14(6), 757–766.
Tayarani-Najaran, Z., Talasaz-Firoozi, E., Nasiri, R., Jalali, N., & Hassanzadeh, M. (2013). Antiemetic activity of volatile oil from Mentha spicata and Mentha× piperita in chemotherapy-induced nausea and vomiting. Ecancermedicalscience, 7, 290–296.
Moradi-Marjaneh, M., Homaei-Shandiz, F., Shamsian, S., Mashhadi, I. E.-Z., & Hedayati-Moghadam, M. (2008). Correlation of HER2/neu over expression, p53 protein accumulation and steroid receptor status with tumor characteristics: An Iranian study of breast cancer patients. Iranian Journal of Public Health, 37(3), 19–28.
Nafissi, N., Khayamzadeh, M., Zeinali, Z., Mohammadi, G., Hosseini, M., & Akbari, M. (2017). Breast cancer in Iran, from epidemiology, clinicopathological and biomarker feature. Advances in Bioresearch, 8(2).
Badve, S., Dabbs, D. J., Schnitt, S. J., Baehner, F. L., Decker, T., Eusebi, V., Fox, S. B., Ichihara, S., Jacquemier, J., & Lakhani, S. R. (2011). Basal-like and triple-negative breast cancers: a critical review with an emphasis on the implications for pathologists and oncologists. Modern Pathology, 24(2), 157.
Holliday, D. L., & Speirs, V. (2011). Choosing the right cell line for breast cancer research. Breast Cancer Research, 13(4), 215.
Ma, H., Ursin, G., Xu, X., Lee, E., Togawa, K., Duan, L., Lu, Y., Malone, K. E., Marchbanks, P. A., & McDonald, J. A. (2017). Reproductive factors and the risk of triple-negative breast cancer in white women and African-American women: a pooled analysis. Breast Cancer Research, 19(1), 6.
Osanloo, M., Sedaghat, M. M., Sereshti, H., Rahmani, M., Saeedi Landi, F., & Amani, A. (2019). Chitosan nanocapsules of tarragon essential oil with low cytotoxicity and long-lasting activity as a green nano-larvicide. Journal of Nanostructures, 9(4), 723–735.
Osanloo, M., Abdollahi, A., Valizadeh, A., & Abedinpour, N. (2020). Antibacterial potential of essential oils of Zataria multiflora and Mentha piperita, micro-and nano-formulated forms. Iranian Journal of Medical Microbiology, 12(1), 43–51.
Osanloo, M., Arish, J., & Sereshti, H. (2019). Developed methods for the preparation of electrospun nanofibers containing plant-derived oil or essential oil: a systematic review. Polymer Bulletin, 77, 6085–6104.
Danaei, M., Dehghankhold, M., Ataei, S., Hasanzadeh Davarani, F., Javanmard, R., Dokhani, A., Khorasani, S., & Mozafari, M. (2018). Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics, 10(2), 57.
Lee, M.-J., Seo, D.-Y., Lee, H.-E., Wang, I.-C., Kim, W.-S., Jeong, M.-Y., & Choi, G. J. (2011). In line NIR quantification of film thickness on pharmaceutical pellets during a fluid bed coating process. International Journal of Pharmaceutics, 403(1-2), 66–72.
Esmaeili, F., Rajabnejhad, S., Partoazar, A. R., Mehr, S. E., Faridi-Majidi, R., Sahebgharani, M., Syedmoradi, L., Rajabnejhad, M. R., & Amani, A. (2016). Anti-inflammatory effects of eugenol nanoemulsion as a topical delivery system. Pharmaceutical Development and Technology, 21(7), 887–893.
Samson, S., Basri, M., Fard Masoumi, H. R., Abdul Malek, E., & Abedi Karjiban, R. (2016). An artificial neural network based analysis of factors controlling particle size in a virgin coconut oil-based nanoemulsion system containing copper peptide. PLoS One, 11(7), e0157737.
Alam, M. S., Ali, M. S., Alam, M. I., Anwer, T., & Safhi, M. M. A. (2015). Stability testing of beclomethasone dipropionate nanoemulsion. Tropical Journal of Pharmaceutical Research, 14(1), 15–20.
Hussain, A. I., Anwar, F., Nigam, P. S., Ashraf, M., & Gilani, A. H. (2010). Seasonal variation in content, chemical composition and antimicrobial and cytotoxic activities of essential oils from four Mentha species. Journal of the Science of Food and Agriculture, 90(11), 1827–1836.
Catalani, S., Palma, F., Battistelli, S., & Benedetti, S. (2017). Oxidative stress and apoptosis induction in human thyroid carcinoma cells exposed to the essential oil from Pistacia lentiscus aerial parts. PLoS One, 12(2), e0172138.
Furtado, F. B., Borges, B. C., Teixeira, T. L., & Garces, H. G. (2018). Chemical composition and bioactivity of essential oil from Blepharocalyx salicifolius. International Journal of Molecular Sciences, 19(1), 33.
Guerrini, A., Sacchetti, G., Grandini, A., Spagnoletti, A., Asanza, M., & Scalvenzi, L. (2016). Cytotoxic effect and TLC bioautography-guided approach to detect health properties of Amazonian Hedyosmum sprucei essential oil. Evidence-based Complementary and Alternative Medicine, 2016, 1638342.
Emami, S. A., Asili, J., Hossein Nia, S., Yazdian-Robati, R., Sahranavard, M., & Tayarani-Najaran, Z. (2016). Growth inhibition and apoptosis induction of essential oils and extracts of Nepeta cataria L. on human prostatic and breast cancer cell lines. Asian Pacific Journal of Cancer Prevention, 17(S3), 125–130.
Momtazi, A. A., Askari-Khorasgani, O., Abdollahi, E., Sadeghi-Aliabadi, H., Mortazaeinezhad, F., & Sahebkar, A. (2017). Phytochemical analysis and cytotoxicity evaluation of Kelussia odoratissima Mozaff. Journal of Acupuncture and Meridian Studies, 10(3), 180–186.
Ogunwande, I. A., Walker, T. M., Bansal, A., Setzer, W. N., & Essien, E. E. (2010). Essential oil constituents and biological activities of Peristrophe bicalyculata and Borreria verticillata. Natural Product Communications, 5(11), 1815–1818.
Osanloo, M., Sereshti, H., Sedaghat, M. M., & Amani, A. (2018). Nanoemulsion of Dill essential oil as a green and potent larvicide against Anopheles stephensi. Environmental Science and Pollution Research, 25(7), 6466–6473.
Rowe, R., Sheskey, P., & Owen, S. (2006). Handbook of pharmaceutical excipients, Royal Pharmaceutical Society of Great Britain. London: Prarmaceutical Press.
Laxmi, M., Bhardwaj, A., Mehta, S., & Mehta, A. (2015). Development and characterization of nanoemulsion as carrier for the enhancement of bioavailability of artemether. Artificial Cells, Nanomedicine, and Biotechnology, 43(5), 334–344.
Tang, L., Yang, X., Yin, Q., Cai, K., Wang, H., Chaudhury, I., Yao, C., Zhou, Q., Kwon, M., & Hartman, J. A. (2014). Investigating the optimal size of anticancer nanomedicine. Proceedings of the National Academy of Sciences, 111(43), 15344–15349.
Bao, H., Zhang, Q., Xu, H., & Yan, Z. (2016). Effects of nanoparticle size on antitumor activity of 10-hydroxycamptothecin-conjugated gold nanoparticles: in vitro and in vivo studies. International Journal of Nanomedicine, 11, 929.
Alkhatib, M. H., AlMotwaa, S. M., & Alkreathy, H. M. (2019). Incorporation of ifosfamide into various essential oils -based nanoemulsions ameliorates its apoptotic effect in the cancers cells. Scientific Reports, 9(1), 695.
Al-Otaibi, W. A., Alkhatib, M. H., & Wali, A. N. (2018). Cytotoxicity and apoptosis enhancement in breast and cervical cancer cells upon coadministration of mitomycin C and essential oils in nanoemulsion formulations. Biomedicine & Pharmacotherapy, 106, 946–955.
Maragheh, A. D., Tabrizi, M. H., Karimi, E., Seyedi, S. M. R., & Khatamian, N. (2019). Producing the sour cherry pit oil nanoemulsion and evaluation of its anti-cancer effects on both breast cancer murine model and MCF-7 cell line. Journal of Microencapsulation, 36(4), 399–409.
Periasamy, V. S., Athinarayanan, J., & Alshatwi, A. A. (2016). Anticancer activity of an ultrasonic nanoemulsion formulation of Nigella sativa L. essential oil on human breast cancer cells. Ultrasonics Sonochemistry, 31, 449–455.
Mahdi Jafari, S., He, Y., & Bhandari, B. (2006). Nano-emulsion production by sonication and microfluidization—a comparison. International Journal of Food Properties, 9(3), 475–485.
Gaikwad, S. G., & Pandit, A. B. (2008). Ultrasound emulsification: effect of ultrasonic and physicochemical properties on dispersed phase volume and droplet size. Ultrasonics Sonochemistry, 15(4), 554–563.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was ethically approved (IR.FUMS.REC.1397.037).
Conflict of Interest
The authors declare that they have no conflict of interest.
Research Involving Humans and Animals Statement
This research did not include human and in vivo studies, and all experiments were performed in vitro conditions. Therefore no informed consent was used.
Funding
The Fasa University of Medical Sciences supported this study with a grant number of 97011.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abedinpour, N., Ghanbariasad, A., Taghinezhad, A. et al. Preparation of Nanoemulsions of Mentha piperita Essential Oil and Investigation of Their Cytotoxic Effect on Human Breast Cancer Lines. BioNanoSci. 11, 428–436 (2021). https://doi.org/10.1007/s12668-021-00827-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12668-021-00827-4