Abstract
Background and Objectives
Acute liver failure (ALF) is an uncommon but potentially dramatic syndrome characterized by massive hepatic necrosis and has a very high mortality rate of 50% to 75% without liver transplantation. This study is aimed at analyzing the etiological spectrum of ALF patients and compare these with ALF mimics such as malaria, dengue fever and other tropical infectious diseases.
Methods
The study population included patients who presented with ALF and ALF mimics in a tertiary care center over two years. We retrospectively analyzed the patient case files and a comparison was made concerning the baseline demographic details, clinical profile, laboratory values and outcomes.
Results
Sixty-three patients were assessed, with 32 in ALF and 31 in ALF mimics group. The most common cause for ALF was hepatitis A virus (25%), followed by hepatitis B virus (18.7%), drug-induced liver injury (12.7%), autoimmune hepatitis (12.5%), hepatitis E virus (9.3%) and Wilson’s disease (6.25%). In the ALF mimics group, malaria (58.06%) was the most common cause, followed by dengue fever (16.1%), leptospirosis (12.9%) and scrub typhus (12.9%). Patients in the ALF mimics group had significantly higher incidence of fever (p = 0.001), hepatosplenomegaly (p = 0.01), anemia (p = 0.02) and shorter jaundice to encephalopathy duration (p = 0.032) as compared to the ALF group, while higher transaminase levels (p = 0.03), bilirubin (p = 0.01), prothrombin time (p = 0.01), serum ammonia (p = 0.02) and mortality (p = 0.02) were observed in ALF patients.
Conclusions
The most common cause for ALF was hepatitis A virus, followed by hepatitis B virus, while in ALF mimics it was malaria followed by dengue fever, in our study. Patients of ALF mimics can have similar presentation, but a high index of suspicion and awareness is required to identify the common infectious ALF mimics for early diagnosis.
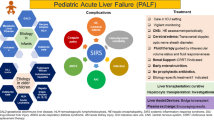
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute liver failure (ALF) is an uncommon but potentially dramatic syndrome characterized by massive hepatic necrosis and has a very high mortality rate of 50% to 75% without liver transplantation (LT) [1, 2]. In the Indian perspective, hepatotropic viruses are the most common causes for ALF and acute liver injury ranges from 60% to 90% [3]. The reported common causes in literature are non-A and E hepatitis (38%), hepatitis E virus (31%), followed by drug-induced liver injury (DILI), anti-tubercular drugs (ATT) being the most common culprits [1]. In the Indian Network for Drug-Induced Liver Injury (INDILI) registry, ATT induced DILI reached up to 63% of the cases [4]. A study revealed that hepatitis A virus-related ALF cases are increasing, while hepatitis E virus-related cases are decreasing, but the data on this recent change in the etiological spectrum of ALF is limited [1]. The causes for ALF in developed countries vary from India; DILI still being the most common cause. The commonest drug is paracetamol, followed by viral and autoimmune hepatitis [5]. Identifying the underlying etiology of ALF is essential, as prompt specific therapy and supportive care may decrease the mortality. Early LT in ALF is crucial, especially for those meeting the King’s College Hospital criteria [6].
In India, infections such as malaria, enteric fever, leptospira, dengue, amebic liver abscesses, tuberculosis and other bacterial and fungal infections with or without human immunodeficiency virus (HIV)-related diseases are also common and are known to present with jaundice and altered sensorium mimicking as ALF [7,8,9]. Similar presentation in the form of fever, jaundice and encephalopathy is a challenge to differentiate these ALF mimics cases from actual ALF patients. Hence, a patient with jaundice and encephalopathy should not always be considered to have ALF and should be suspected for these infections in tropical countries such as India for definite diagnosis and early treatment. There is a lack of data on recent changes in the etiological spectrum of ALF and on the comparison of ALF with ALF mimics in literature. In this retrospective study, we aimed at analyzing the etiological spectrum of ALF patients and compared these patients with ALF mimics such as malaria, dengue fever and other tropical infectious diseases.
Methods
This retrospective descriptive study was performed over two years, from January 2022 to December 2023. All patients admitted with the diagnosis of ALF in the Department of Gastroenterology, SMS Medical College, Jaipur, were enrolled and compared with a similar number of patients diagnosed as ALF mimics. The ALF was defined according to the Indian National Association for Study of the Liver (INASL) definition [2]. The patients of ALF mimics who had similar presentations were also enrolled in the ALF mimics group for comparison. After enrollment, both outpatient and inpatient medical data were reviewed in detail. Patient's demographic parameters, clinical features, laboratory values, including complete hemogram, liver function test, renal function test, prothrombin time, ammonia, random blood sugar, acid–base gas analysis and other relevant laboratory parameters, were documented. Details about the etiological workup were also assessed. A comparison was made concerning the baseline demographic details, clinical profile, laboratory parameters and the outcomes. All ALF and ALF mimics patients received etiological and supportive treatment based on the standard practicing guidelines.
The institutional review ethics committee approved the study protocol. (Ethics committee number- 4491/MC/EC/2021).
Statistical analysis
The statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) trial version 23.0 for Windows (SPSS, Chicago, IL, USA). Categorical variables were expressed as absolute numbers with percentages, while continuous data was presented as mean ± standard deviation (SD). The significance of differences between treatment groups was assessed using Chi-square or Fisher's exact tests as appropriate. Receiver operating characteristic curves (ROC) were used to identify the cut-off points for various variables to differentiate ALF from ALF mimics at the time of admission. Based on best cut-off points obtained from ROC curve, different diagnostic measures such as sensitivity, specificity and predictive values were reported. A p-value of less than 0.05 was considered significant.
Results
As many as 63 patients were enrolled, with 32 patients in ALF group and 31 in ALF mimics group. Of 52 patients diagnosed as ALF mimics, only 31 were enrolled for a head-to-head comparison, as they met the defining criteria for ALF, i.e. jaundice followed by encephalopathy and coagulopathy. The baseline demographic, laboratory and clinical parameters of the study population are shown in Tables 1 and 2. The ALF involved a younger population in both groups and males were affected more than females in both groups.
The most common cause for ALF was hepatitis A virus in eight patients (25%), followed by hepatitis B virus in six (18.75%), DILI in four (12.5%), autoimmune hepatitis in four (12.5%), hepatitis E virus in three (9.3%) and Wilson’s disease in two (6.25%) patients and it was unknown in five (15.6%) patients. The most common cause for ALF mimics was malaria in 18 (58.06%), followed by dengue fever in five (16.1%), leptospirosis in four (12.9%) and scrub typhus in four (12.9%) patients as shown in Table 3. Renal failure was slightly more common in ALF mimics compared to ALF group, although it was not statistically significant (58.1% vs. 50%, p = 0.85). The comparison of laboratory parameters between ALF and ALF mimics is shown in Table 4. None of the study patients were pregnant at the time of illness.
Patients in the ALF mimics group had significantly higher incidences of fever at the onset of illness, hepatosplenomegaly, shorter jaundice to encephalopathy duration, higher serum lactate dehydrogenase (LDH), low hemoglobin and low platelet count compared to ALF group, as shown in Tables 1, 3 and 4. In contrast, higher aspartate aminotransferase (AST) and alanine transaminase (ALT), bilirubin, prothrombin time, serum ammonia and mortality were observed in ALF patients compared to ALF mimics, as shown in Tables 1, 3 and 4. The number of patients who had high LDH compared to ALT (64.5% vs. 6.25%, p = 0.01) and low albumin (48.4% vs. 15.6%, p = 0.02) were significantly higher in ALF mimics group compared to ALF group as shown in Table 4. None of the study patients underwent liver transplants. Diagnostic accuracy of various variables was assessed at the time of admission. The ROC curves were used to assess the diagnostic accuracy of various variables. The area under receiver operating characteristic curve (AUROC) for predicting ALF at baseline for hemoglobin, bilirubin, AST and ALT were 0.67, 0.82, 0.81 and 0.78, respectively, as shown in Fig. 1 and Table 5. The bilirubin has the best sensitivity (87.88%) and transaminases level (AST and ALT) has best specificity (68.75%) for differentiating ALF from ALF mimics as shown in Table 5. The AST level has best positive predictive value (PPV), which was 73.68% and negative predictive value (NPV), which was 81.48% as shown in Table 5.
Discussion
Our study revealed that the most common cause for ALF was hepatitis A virus, followed by hepatitis B virus, DILI, autoimmune hepatitis, hepatitis E virus and Wilson's disease. The most common cause for ALF mimics was malaria, followed by dengue fever, leptospirosis, scrub typhus and sepsis. In earlier studies as well, the common causes for ALF were hepatotropic viruses [1,2,3]. Initially, it was believed that hepatitis E virus was one of the most common causes for ALF in our population. However, in our study and in an earlier published study, it is seen that the incidence of hepatitis E-related ALF is decreasing and hepatitis A-related ALF is becoming the leading cause for ALF [1, 2]. This is likely because of improvement in sanitation and hygiene, which leads to decreased exposure of childhood HAV infection. This results in increased numbers of non-immune adolescents and adults in general population. However, in pregnant patients, hepatitis E virus is still a major cause for ALF, although none of our hepatitis E virus-related ALF patients were pregnant [2].
In tropical countries such as India, tropical fevers including malaria, dengue, enteric fever and scrub typhus can present as encephalopathy and jaundice in severe form, which may mimic ALF. One must be well aware of these endemic diseases, especially in the rainy season, during which the incidence of these diseases increases exponentially. All patients with suspected ALF should undergo baseline laboratory investigations along with etiological workup for tropical diseases, especially when fever is preceding the illness. Prompt diagnosis, specific therapy and supportive treatment results in high recovery rate and decrease mortality in such cases. Mortality rate was less in ALF mimics as compared to ALF patients in our study. These results are similar to previously published study, in which ALF patients had higher mortality compared to ALF mimics (50% vs. 25%, p = < 0.05) [10]. Patients in the ALF mimics group were slightly younger than those in the ALF group, although the difference was not statistically significant. These results are in concordance with an earlier study, where the mean age was 38.2 ± 11.2 in the ALF group and 36.8 ± 10.2 in the ALF infectious disease group [10].
In ALF mimics patients, fever was seen in a majority of cases and the duration of onset of jaundice to encephalopathy was significantly less compared to ALF patients, similar to an earlier published study [1]. The presence of mild ALT and AST elevation, raised LDH, LDH/ALT ratio of > 1, low platelet counts and borderline increased prothrombin time should raise clinical suspicion of ALF mimics as observed in our ALF mimics patients [10]. Lower hemoglobin and a trend towards renal dysfunction was also observed in ALF mimics group. On the other hand, higher bilirubin, transaminase levels, prolonged prothrombin time, grade 3 or 4 hepatic encephalopathy and higher mortality was more in ALF group, as observed in other studies [1, 2, 10]. A study on more than 1000 ALF patients, reported hepatic encephalopathy in 80% of patients within two weeks of icterus and in all patients within four weeks [11]. Similarly, in our study, 78.1% of patients developed encephalopathy within two weeks and all patients developed it within four weeks of jaundice.
A retrospective series comparing 27 patients of enteric hepatitis with 27 of acute viral hepatitis, also revealed that ALT/LDH ratio (< 4) was a good discriminator and features such as high-grade fever, relative bradycardia, leukopenia, raised ALT and AST < 5 times upper limit of normal were favoring enteric hepatitis [12]. One series suggested that disproportionate anemia, renal failure and mildly elevated liver enzymes could help in differentiating falciparum malaria from acute liver failure due to viral etiology [13] and similar results were observed in our study. As the mortality in patients who present late is high, early diagnosis and treatment with specific therapy may be life-saving in such cases.
True hepatic encephalopathy is rare in malaria. A study on 86 patients with malarial hepatopathy reported hypersomnia, delirium and inversion of the sleep rhythm in 15 patients. Arterial blood ammonia levels were high in all patients (range 120–427 mEq/L), but flapping tremors were observed in only in nine patients [14]. In our study, seven patients out of 18 malarial patients had increased serum ammonia levels (116.45 ± 12.06 mEq/L).
Dengue-induced liver injury is usually manifested by hepatomegaly elevated transaminase levels. Presentation with jaundice may mimic acute viral hepatitis. Severe dengue can present as fulminant hepatic failure with high mortality. Most cases have a mild course of illness, with less than 11% having a rise in transaminase levels more than 10 times of the upper limit. Several authors have reported jaundice in 2% to 25% of cases. Dengue-related ALF is less common and is observed mainly in children with up to 50% mortality, though it can also occur in adults [9, 15]. Liver function derangement and jaundice can be seen in 21% to 60% cases of enteric fever [16], but ALF is rare in these patients.
There are many challenges for considering liver transplant as a treatment in patients of ALF mimics. The diagnostic dilemma between ALF and ALF mimics is an important challenge, as specific etiological therapy along with supportive management at appropriate time can completely cure the patient of ALF mimic. Other challenges include non-availability of prognostic scores, sepsis and multi-organ failure in ALF mimics [17].
Our study showed a changing spectrum of ALF in a tertiary care setting and compared these patients with ALF mimics, which are commonly seen in our clinical practice. Retrospective study design and small sample size are the limitations of our study. Further prospective studies with large sample size are required to validate our results. In conclusion, the most common cause for ALF was hepatitis A virus, followed by hepatitis B virus, while in ALF mimics it was malaria followed by dengue fever. Patients of ALF mimics can have similar presentation, but a high index of suspicion and awareness is required to identify the common infectious ALF mimics for early diagnosis and treatment. Patients in the ALF mimics group have significantly higher incidences of fever, hepatosplenomegaly, shorter jaundice to encephalopathy duration, low platelet counts and higher serum LDH compared to ALF group, while higher transaminase levels, bilirubin, prothrombin time, serum ammonia and mortality were observed in ALF patients. This approach will help in identifying patients with ALF mimics early, who may have very low mortality if specific treatment is instituted promptly. It will also help in prioritizing ALF patients for LT listing and prevent the unnecessary burden of ALF mimics in the transplant category.
Data availability
Department of Gastroenterology, SMS Hospital, Jaipur, India.
References
Acharya SK. Acute liver failure: Indian perspective. Clin Liver Dis (Hoboken). 2021;18:143–9.
Anand AC, Nandi B, Acharya SK, et al. Indian National Association for the Study of the Liver consensus statement on acute liver failure (Part 1): epidemiology, pathogenesis, presentation and prognosis. J Clin Exp Hepatol. 2020;10:339–76.
Shalimar, Acharya SK, Lee W. Worldwide differences in acute liver failure. In: Williams R, Wendon J, editors. Future Medicine Ltd. Critical Care in Acute Liver Failure. 2013;2013:32–46. https://doi.org/10.2217/ebo.12.326.
Devarbhavi H, Joseph T, Sunil Kumar N, et al. The Indian network of drug-induced liver injury: etiology, clinical features, outcome and prognostic markers in 1288 patients. J Clin Exp Hepatol. 2021;11:288–98.
Marudanayagam R, Shanmugam V, Gunson B, et al. Aetiology and outcome of acute liver failure. HPB (Oxford). 2009;11:429–34.
Mehrotra S, Mehta N, Rao PS, et al. Live donor liver transplantation for acute liver failure: a single center experience. Indian J Gastroenterol. 2018;37:25–30.
Murthy GL, Sahay RK, Sreenivas DV, Sundaram C, Shantaram V. Hepatitis in falciparum malaria. Trop Gastroenterol. 1998;19:152–4.
Joshi YK, Tandon BN, Acharya SK, Babu S, Tandon M. Acute hepatic failure due to Plasmodium falciparum liver injury. Liver. 1986;6:357–60.
Anand AC, Garg HK. Approach to clinical syndrome of jaundice and encephalopathy in tropics. J Clin Exp Hepatol. 2015;5:S116–30.
Deepak NA, Patel ND. Differential diagnosis of acute liver failure in India. Ann Hepatol. 2006;5:150–6.
Kumar R, Shalimar, Bhatia V, et al. Antituberculosis therapy induced acute liver failure: magnitude, profile, prognosis, and predictors of outcome. Hepatology. 2010;51:1665–74.
Bernal W, Auzinger G, Wendon J. Prognostic utility of the bilirubin lactate and etiology score. Clin Gastroenterol Hepatol. 2009;7:249–53.
Anand AC, Ramji C, Narula AS, Singh W. Malarial hepatitis: a heterogeneous syndrome? Natl Med J India. 1992;5:59–62.
Kochar DK, Agarwal P, Kochar SK, et al. Hepatocyte dysfunction and hepatic encephalopathy in Plasmodium falciparum malaria. QJM. 2003;96:505–12.
Viswanathan S, Iqbal N, Anemon PP, Kumar GS. Fatal fulminant hepatic failure in a diabetic with primary dengue. J Trop Med. 2010;2010:41356.
Ramachandran S, Godfrey JJ, Perera MVF. Typhoid typhoid fever hepatitis. JAMA. 1974;230:236–40.
Kumar R, Anand U, Priyadarshi RN. Liver transplantation in acute liver failure: Dilemmas and challenges. World J Transplant. 2021;11:187–202.
Acknowledgements
Jaya Maharshi – For typing, formatting and grammar corrections. Shalini Singh- For Statistical Analysis.
Funding
None.
Author information
Authors and Affiliations
Contributions
Saksham Seth, Kamlesh Kumar Sharma: Acquisition, analysis or interpretation of the data. Sudhir Maharshi, Rupesh Pokharna, Sandeep Nijhawan, Shyam Sunder Sharma : Study conception, design and supervision, drafting of article and critical revision for import ant intellectual content, final approval of the version to be published. Sudhir Maharshi: Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
SS, SM, KKS, RP, SN and SSS declare no conflict of interest for this article.
Ethics statement
The study was performed conforming to the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Ethical approval
The institutional ethics committee approved the study protocol, which was conducted in accordance with the Declaration of Helinski. Patient gave their written consent.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Seth, S., Maharshi, S., Sharma, K.K. et al. Changing etiological spectrum of acute liver failure. Indian J Gastroenterol 43, 452–458 (2024). https://doi.org/10.1007/s12664-024-01578-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-024-01578-2