Abstract
Background
Terlipressin and noradrenaline are effective in the management of hepatorenal syndrome (HRS). There are no reports on the combination of these vasoconstrictors in type-1 HRS.
Aim
To evaluate terlipressin with or without noradrenaline in type-1 HRS not responding to terlipressin at 48 hours.
Methods
Sixty patients were randomized to receive either terlipressin (group A; n = 30) or a combination of terlipressin and noradrenaline infusion (group B; n = 30). In group A, terlipressin infusion was started at 2 mg/day and increased by 1 mg/day (maximum 12 mg/day). In group B, terlipressin was given at a constant dose of 2 mg/day. Noradrenaline infusion was started at 0.5 mg/h at baseline and increased to 3 mg/h in a stepwise manner. The primary outcome was treatment response at 15 days. Secondary outcomes were 30-day survival, cost–benefit analysis and adverse events.
Results
There was no significant difference in the response rate between the groups (50% vs. 76.7%, p = 0.06) and 30-day survival was similar (36.7% vs. 53.3%, p = 0.13). Treatment was more expensive in group A (USD 750 vs. 350, p < 0.001). Adverse events were more frequent in group A (36.7% vs. 13.3%, p < 0.05).
Conclusions
The combination of noradrenaline and terlipressin infusion results in a non-significantly higher rate of HRS resolution with significantly fewer adverse effects in HRS patients who do not respond to terlipressin within 48 hours.
Trial registration.
Clinicaltrials.gov (NCT03822091).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
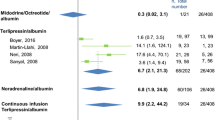
Hepatorenal syndrome (HRS) develops as a result of splanchnic vasodilation leading to decreased effective arterial blood volume [1]. Terlipressin is the most extensively studied vasoconstrictor in the treatment of HRS [2,3,4,5,6,7,8]. It mainly acts on V1 receptors. The efficacy of terlipressin plus albumin to reverse renal failure in patients with type 1 HRS has been reported to be < 45% when used in the bolus form [2,3,4,5,6,7,8]. Intravenous infusion of terlipressin was shown to be equally effective with fewer adverse effects in a recent trial [7]. Noradrenaline has also been used in the treatment of HRS patients and acts by increasing mean arterial pressure (MAP) by its alpha-1-mediated effect on systemic vascular resistance and beta-1-mediated inotropic activity [8,9,10,11].Terlipressin and noradrenaline are effective individually in the management of HRS. Combination of these may be more effective with possibly decreased side effects by virtue of action at different target receptors. However, there are no reports on the use of combination of terlipressin and noradrenaline in type-1 HRS. Therefore, we evaluated terlipressin vs. a combination of terlipressin and noradrenaline infusion in patients with type-1 HRS who did not respond to terlipressin infusion at 48 hours.
Methods
Total 110 consecutive patients with cirrhosis and HRS type 1, visiting the hepatology department of a tertiary center between July 2018 and May 2019, were prospectively evaluated for inclusion in the study. Thirty of the 110 screened patients were excluded due to various reasons (Fig. 1). Twenty of these 80 patients responded to terlipressin infusion of 2 mg/24 h for 48 hours (response was defined as serum creatinine decrease ≥ 25% at 48 hours). The remaining 60 non-responders, who met the inclusion criteria, were entered into the study (Fig. 1). The study was approved by the Ethics Committee of Postgraduate Institute of Medical Education and Research, Chandigarh. Written informed consent was obtained. The randomized clinical trial was registered at the US National Institutes of Health (clinical trial identifier NCT03822091). All authors had access to the study data and had reviewed and approved the final manuscript.
We included patients > 18 years of age with cirrhosis and a diagnosis of type-1 HRS based on the criteria of International Club of Ascites [12]. Patients with a history of coronary artery disease, peripheral vascular disease, arrhythmias, hepatocellular carcinoma or contraindications to the use of terlipressin or noradrenaline were excluded (Supplementary Text). Patients were randomly assigned to receive terlipressin infusion alone (group A; n = 30) or terlipressin plus noradrenaline infusion (group B; n = 30). A computer made the randomization code with 60 envelopes, half for terlipressin alone (group A) and half for terlipressin plus noradrenaline (group B). Patients and investigators were not blinded to the treatment assignments. Additionally, all patients also received 20 g albumin/day.
As per regular criteria, patients receiving terlipressin are monitored after 48 hours and dosage is increased accordingly, while patients receiving noradrenaline are monitored after every four hours and dosage increased according to response. To ensure a common time frame of action and comparison, we kept the monitoring time as 24 hours, after which drug dosage could be increased. More frequent monitoring would ensure earlier dose escalation and could potentially lead to a shorter treatment duration and earlier reversal of HRS. Dosage escalation was done in both groups every 24 hours, if the decline in serum creatinine was < 12.5% or increase in mean arterial pressure (MAP) was < 10 mmHg or urine output was < 200 mL in four hours.
Patients in group A received terlipressin infusion at a rate of 2 mg/24 h. The dose of terlipressin was increased by 1 mg after 24 hours as per the above criteria up to a maximum of 12 mg/24 h. Patients in group B received a fixed dose of terlipressin infusion at a rate of 2 mg/24 h and noradrenaline was given as a continuous infusion starting at a dose of 0.5 mg/h. The dose of noradrenaline was increased every 24 hours in steps of 0.5 mg/h up to the maximum dose of 3 mg/h. Vasoconstrictors were continued until complete response was attained as defined by serum creatinine < 1.5 mg/dL or for a maximum of 15 days. Albumin was also administered in patients of either group at a dose of 20 g/day. Albumin was withheld if central venous pressure (CVP) was more than 18 cm of saline. All patients were admitted to a liver high-dependency unit (HDU) and followed up for up to 30 days. Clinical and biochemical parameters were assessed at baseline, everyday up to day 15 and every week thereafter until 30 days.
Outcome measures
The primary end point of the study was response to vasoconstrictor therapy as defined by a serum creatinine less than 1.5 mg/dL. Secondary end points included 30-day survival, safety of treatment and cost analysis.
Statistical analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 22.0 for Microsoft Windows (IBM, Corp, Armonk, NY., USA). The results were expressed as mean ± standard deviation (SD) or median with interquartile range. Comparisons between groups were performed using Student’s 't'-test or the Mann–Whitney U test for normally distributed and skewed quantitative data, respectively. For categorical data, the Chi-square test or Fisher’s exact test was applied. Survival analysis was performed using the Kaplan–Meier method and compared using the log-rank test. Patients who were lost to follow-up or withdrawn from the study were censored. Baseline predictors of response to therapy were inferred from a multivariate logistic regression model incorporating the variables identified on univariate analysis with p < 0.1. Multi-collinearity was assessed by variable inflation factors. VIF > 5 was taken as critical. All statistical analyses were performed two-sided with p < 0.05 being considered statistically significant.
Sample size calculation
A previous study using terlipressin infusion in type-1 HRS documented reversal in approximately 50% of patients [7]. A recent meta-analysis on vasoconstrictors in HRS demonstrated recovery in approximately 35% of patients [13]. Thus, keeping an α error of 5% and assuming 10% dropouts, 30 patients were allocated to each arm to detect an absolute increase in the response rate by 35% with a power of 80%.
Results
The two groups were comparable at baseline with respect to clinical and laboratory parameters except the 24-hour urinary volume and 24-hour urinary sodium (Table 1). All patients had ascites at presentation. None of the patients underwent liver transplant. Patients in the monotherapy group received a significantly higher mean daily dose of terlipressin (4.97 ± 1.37 mg) than patients in the combination group, all of whom received 2 mg of terlipressin per day (p < 0.001). In the combination arm, the mean rate of noradrenaline infusion was 1.23 ± 0.53 mg/h. However, there was no difference in the duration of treatment between the two groups (9 ± 3.61 days vs. 7.83 ± 2.57 days, p: 0.15) (Table 2).
Primary outcome
The rate of response was higher in the combination arm (76.7%) as compared to the terlipressin monotherapy group (50%), although this difference was not statistically significant (p = 0.06). Decline in serum creatinine was significantly lower in the terlipressin monotherapy group (− 1.67 ± 0.8) compared to that in the combination arm (− 2.21 ± 0.94; p: 0.02) (Table 2).
On univariate analysis, baseline serum bilirubin (p: 0.005), creatinine (p < 0.001), Child-Turcotte-Pugh (CTP) score (p: 0.004) and model for end-stage liver disease-sodium (MELD-Na) score (p < 0.001) were significantly associated with response (Table 3). On multivariate logistic regression analysis, only serum creatinine (OR: 0.31, 95% CI: 0.11 to 0.63, p: 0.005) and combination therapy (OR: 17.41, 95% CI 3.10 to 168.4, p: 0.004) were significantly predictive of response.
Secondary outcomes
No significant difference in the 30-day survival was observed between patients who received the terlipressin monotherapy (36.7%) compared to those who received the combination therapy (53.3%, p: 0.13) (Fig. 2).
Treatment-related severe adverse events were significantly more common in the monotherapy group (36.7% vs. 13.3%, p < 0.05) (Table 4). Overall, diarrhea was the most common adverse event observed in four (13.3%) and two (6.67%) patients in the monotherapy and combination groups, respectively. The cost of therapy was significantly cheaper in the combination group (USD355 ± 108) in comparison to that in the terlipressin monotherapy group (USD755 ± 457, p < 0.001).
Discussion
HRS may be described as acute kidney injury occurring in the setting of arterial vasodilatation and suboptimal cardiac output with consequent decreased glomerular filtration occurring in patients with decompensated cirrhosis. Vasoconstrictors along with albumin are the mainstay of pharmacologic management of HRS. Multiple studies have documented the efficacy of terlipressin in reversing HRS and it is currently recommended as the first-line vasoconstrictor in international guidelines [14]. However, almost 50% of patients fail to completely respond to terlipressin as defined by a serum creatinine of < 1.5 mg/dL after a maximum of 14 days of therapy [2,3,4,5,6,7,8, 14]. Increased vasodilatation, which is fundamental to the pathogenesis of HRS, leads to arterial underfilling that is sensed by baroreceptors, leading to increased release of vasopressin despite the relatively low oncotic pressures [15, 16]. It is reasonable to presume that in HRS, the V1 receptors may be partially occupied by endogenous vasopressin, thereby potentially limiting the efficacy of terlipressin. Those who have sufficient unoccupied V1 receptors are likely to show an early response to terlipressin, while patients who have insufficient free V1 receptors are likely to benefit from the addition of a second vasoconstrictor targeting alternate receptors. Additional adrenergic receptor–mediated vasoconstriction may thus be helpful in HRS patients who fail to show an early response to terlipressin alone. Noradrenaline monotherapy has previously been shown to be beneficial in HRS in a few studies and is more cost-effective than terlipressin [8, 9, 11]. For the first time, we report a novel approach of combining two vasoconstrictors (terlipressin and noradrenaline) in HRS patients who do not respond to terlipressin monotherapy within 48 hours.
In our study, there was a trend to a higher rate of response in the combination arm as compared to those who were continued on terlipressin monotherapy (76.7% vs. 50%, p: 0.06) with significantly greater reductions in serum creatinine (− 2.21 ± 0.94 vs. − 1.67 ± 0.8 vs. p: 0.02). While acknowledging that “trends to significance” should be interpreted with caution, we would like to emphasize that the response rate of 76.7% in the combination arm appears to be clinically meaningful. Moreover, on multivariate analysis, combination therapy was associated with significantly higher odds of attaining response (OR: 17.41, 95% CI 3.10 to 168.4, p: 0.004). It should be noted that our sample size calculations were largely based on assumptions due to the lack of previous data on the use of combination of vasoconstrictors in HRS. On post-hoc analysis, the power of our study was only 57%. Thus, a larger sample of patients would be required to establish statistical significance. Intriguingly, we did not find any difference in change in MAP between the two groups. This may have been due to the small sample size and the lack of invasive monitoring of blood pressure in our patients. We further acknowledge that some of our patients may have had acute-on-chronic liver failure at baseline which may have led to heterogeneity and confounded our findings.
Our patients had extremely avid sodium retention at baseline as evidenced by the 24-hour sodium of < 10 mEq/L. This is probably reflective of the underlying state of profound vasodilatation with consequential intense activation of renin-angiotensin-aldosterone system (RAAS) and vasopressin secretion. Dose escalation in our study was based on changes in serum creatinine, rise in MAP and urine output. Urinary sodium levels were not used for response assessment. Recently, urinary sodium–guided “slow albumin-furosemide infusion” with terlipressin ± noradrenaline has been shown to improve survival and ascites mobilization in patients with acute-on-chronic liver failure [17]. Whether a similar approach to response assessment using urinary sodium is therapeutically beneficial in HRS needs to be evaluated in future studies.
As opposed to most previous studies which have used terlipressin boluses, we used an infusion protocol as it has been shown to be associated with response at a lower cumulative dose with fewer adverse effects [7]. Complete response was attained in 50% of patients who received terlipressin infusion alone which is comparable to the observations of Cavallin et al. (55.88%) [7]. Treatment-related adverse events were observed in 36.7% of patients who received terlipressin monotherapy, which is also comparable to previous findings in HRS patients receiving terlipressin infusion [7]. More importantly, the combination of terlipressin and noradrenaline was well tolerated and associated with a significantly lower rate of adverse events as compared to terlipressin monotherapy (36.7% vs. 13.3%, p < 0.05). This is possibly because the fixed daily dose of terlipressin in the combination group (2 mg/day) was significantly lower than the mean daily dose of terlipressin in the monotherapy group (4.97 ± 1.37 mg/day).
The average cost of treatment in patients who received terlipressin infusion alone was more than double that of patients who received the combination therapy (USD 355 ± 108 vs. USD 755 ± 457, p < 0.001). It should be noted that our cost calculations did not take into account the cost of albumin and other expenses incurred during hospitalization.
Recently, HRS-1 has been rechristened HRS-AKI (acute kidney injury) and its definitions have been changed to include patients with a rise in creatinine by ≥ 0.3 mg/dL in 48 hours or ≥ 50% from the baseline. Definitions of response have also been changed with complete response being now defined as return of serum creatinine to within 0.3 mg/dL of the baseline value [18]. Our approach of using a combination of vasoconstrictors in patients showing lack of early response to terlipressin monotherapy needs to be further studied in HRS-AKI patients using these new definitions. It is possible that the earlier diagnosis of HRS-AKI at lower levels of serum creatinine will lead to an increase in response rates. The waiting time before declaring a patient as an early non-responder and switching to combination therapy also needs to be further defined. Our results need to be further explored in larger, multicentric trials. We acknowledge the limitations of our study including the small sample size, the open label nature of the study and the lack of invasive monitoring of blood pressure and other hemodynamic parameters including systemic vascular resistance and cardiac output.
In conclusion, in comparison to terlipressin monotherapy, the combination of noradrenaline and terlipressin infusion is associated with a trend to a higher rate of HRS resolution with significantly fewer adverse effects in HRS patients who do not show an early response to terlipressin within 48 hours.
References
Schrier RW, Arroyo V, Bernardi M, Epstein M, Henriksen JH, Rodes J. Peripheral arterial vasodilatation hypothesis: A proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology. 1988;8:1151–7.
Sanyal AJ, Boyer T, Garcia-Tsao G, et al. A randomized prospective double blind, placebo controlled study of terlipressin for type 1 hepatorenal syndrome. Gastroenterology. 2008;134:1360–8.
Martin-Llahi M, Pepin MN, Guevara M, et al. Terlipressin and albumin vs albumin in patients with cirrhosis and hepatorenal syndrome: A randomized study. Gastroenterology. 2008;134:1352–9.
Rodriguez E, Elia C, Sola E, et al. Terlipressin and albumin for type-1 hepatorenal syndrome associated with sepsis. J Hepatol. 2014;60:955–61.
Cavallin M, Kamath PS, Merli M, et al. Terlipressin plus albumin vs. midodrine and octreotide plus albumin in the treatment of hepatorenal syndrome: A randomized trial. Hepatology. 2015;62:567–74.
Boyer TD, Sanyal AJ, Wong F, et al. Terlipressin plus albumin is more effective than albumin alone in improving renal function in patients with cirrhosis and hepatorenal syndrome type 1. Gastroenterology. 2016;150:1579–89.
Cavallin M, Piano S, Romano A, et al. Terlipressin given by continuous intravenous infusion vs. intravenous boluses in the treatment of hepatorenal syndrome: A randomized controlled study. Hepatology. 2016;63:983–92.
Singh V, Ghosh S, Singh B, et al. Noradrenaline vs. terlipressin in the treatment of hepatorenal syndrome: A randomized study. J Hepatol. 2012;56:1293–8.
Alessandria C, Ottobrelli A, Debernardi-Venon W, et al. Noradrenalin vs terlipressin in patients with hepatorenal syndrome: A prospective, randomized, unblinded, pilot study. J Hepatol. 2007;47:499–505.
Duvoux C, Zanditenas D, Hezode C, et al. Effects of noradrenalin and albumin in patients with type I hepatorenal syndrome: A pilot study. Hepatology. 2002;36:374–80.
Sharma P, Kumar A, Shrama BC, Sarin SK. An open label, pilot, randomized controlled trial of noradrenaline vs. terlipressin in the treatment of type 1 hepatorenal syndrome and predictors of response. Am J Gastroenterol. 2008;103:1689–97.
Salerno F, Gerbes A, Gines P, Wong F, Arroyo V. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut. 2007;56:1310-8.
Best LM, Freeman SC, Sutton AJ, et al. Treatment for hepatorenal syndrome in people with decompensated liver cirrhosis: A network meta-analysis. Cochrane Database Syst Rev. 2019;9:CD013103.
Angeli P, Bernardi M, Villanueva C, et al. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406–60.
John S, Thuluvath PJ. Hyponatremia in cirrhosis: Pathophysiology and management. World J Gastroenterol. 2015;21:3197–205.
Bichet D, Szatalowicz V, Chaimovitz C, Schrier RW. Role of vasopressin in abnormal water excretion in cirrhotic patients. Ann Intern Med. 1982;96:413–7.
Pande G, Hatti M, Rai MK, et al. Response guided slow infusion of albumin, vasoconstrictors and furosemide improves ascites mobilization and survival in acute on chronic liver failure: A proof-of-concept study. J Inflamm Res. 2022;1:5027–39.
Angeli P, Gines P, Wong F, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: Revised consensus recommendations of the International Club of Ascites. J Hepatol. 2015;62:968–74.
Author information
Authors and Affiliations
Contributions
Virendra Singh: conceived the study, design of the study protocol, patient enrolment, data collection and manuscript writing; Akshaya Jayachandran: patient enrolment, data collection and manuscript writing; Arka De: patient enrolment, data collection and analysis, manuscript writing; Akash Singh: patient enrolment and data collection; Shivani Chandel: data collection and analysis; Navneet Sharma: data collection. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
VS, AJ, AD, AS, SC and NS declare no competing interests.
Informed consent in studies with human subjects
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, V., Jayachandran, A., De, A. et al. Combination of terlipressin and noradrenaline versus terlipressin in hepatorenal syndrome with early non-response to terlipressin infusion: A randomized trial. Indian J Gastroenterol 42, 388–395 (2023). https://doi.org/10.1007/s12664-023-01356-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-023-01356-6