Abstract
Background/Purpose
Patients with functional dyspepsia (FD) have poor health-related quality of life (HRQOL), but Indian data are lacking. Also, there is non-availability of validated disease-specific questionnaire to assess HRQOL in Hindi-speaking patients with dyspepsia. We aimed to develop and validate a reliable translation of Short-Form Nepean Dyspepsia Index (SF-NDI) in Hindi, and assess the impact of FD on HRQOL in Indian patients.
Methods
Cross-cultural adaptation of English version of SF-NDI, translation to Hindi, and adaptation of Hindi version were performed using standard procedures. English and Hindi versions were assessed against Short Form-36 (SF-36), examining for internal consistency, test–retest reliability, and validity.
Results
Total 211 FD patients (144 Hindi speaking, 67 English speaking) were enrolled (mean age 40.8 ± 11.7 years; male:female = 115:96). Median total SF-NDI scores for both languages were 38.75 and 40.0, respectively. Test–retest reliability intraclass correlation coefficients were 0.85 (Hindi) and 0.89 (English). Internal consistency evaluation revealed Cronbach’s α coefficient of 0.79–0.86 (Hindi) and 0.78–0.89 (English). SF-NDI sub-scales showed moderate to good correlation with various domains of SF-36 (content validity). There was significant (p < 0.001) decline of HRQOL in patients with severe dyspepsia relative to those with mild dyspepsia (construct validity). On multivariate analysis, factors independently associated with HRQOL were duration of symptoms and dyspepsia severity.
Conclusion
Both English and Hindi versions of SF-NDI are reliable and valid for HRQOL assessment in Indian FD patients, and will be useful in future epidemiological and clinical studies. Indian FD patients have poor HRQOL, being worse in those with severe dyspepsia and longer duration of symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Dyspepsia refers to a symptom or a constellation of symptoms that is (are) considered to originate from the gastroduodenal region [1]. These symptoms include epigastric pain, epigastric burning, postprandial fullness, early satiation, bloating in the upper abdomen, nausea, vomiting, and belching [1]. Patients with chronic, recurrent upper abdominal symptoms who have not yet undergone clinical evaluation are identified with a preliminary diagnosis of uninvestigated dyspepsia [1, 2]. If an organic, systemic, or metabolic cause is identified, where, if the disease improves or is eliminated, symptoms also improve or resolve, patients are categorized as secondary dyspepsia [2]. Approximately 80% of patients who have no identifiable explanation for the symptoms are labelled as functional dyspepsia (FD) [2, 3]. According to Rome IV, FD is further categorized into postprandial distress syndrome (PDS), characterized by meal-induced dyspeptic symptoms, and epigastric pain syndrome (EPS), referring to epigastric pain/burning that does not occur exclusively postprandially, can occur during fasting, and can be even improved by meal ingestion [2]. FD commonly overlaps with other disorders of gut–brain interaction [2, 4]. The pathophysiology of FD is multifactorial, and is often attributed to a combination of visceral hypersensitivity and upper gastrointestinal dysmotility that varies with each individual and with time [2, 3].
Worldwide prevalence of FD varies between 10% and 16% [3]. Dyspepsia is rarely fatal, but a majority of patients suffer from significant levels of abdominal symptoms that interrupt daily activities. Dyspepsia has a significant impact on physical, mental, and social aspects of health-related quality of life (HRQOL) [2, 3, 5]. In addition, dyspepsia presents a significant financial burden to patients and healthcare resources worldwide, in terms of chronic use of medications, repeated investigations, and loss of economic productivity due to sickness-related work absenteeism [2, 3, 5].
Several studies have evaluated the impact of FD on HRQOL using different questionnaires [5,6,7,8,9,10,11,12,13,14,15,16,17,18]. Most of these studies reported a significant reduction in at least some domains of HRQOL among patients with FD compared to controls. In general, the decline in scores of physical domains has been similar to those of mental domains [7]. Although the negative impact of FD on HRQOL has been reported in many western [8,9,10,11,12] and Asian countries [5, 13,14,15,16,17,18], there is lack of Indian data on this subject. Also, there is non-availability of any validated questionnaire to assess the HRQOL in Hindi-speaking patients with FD. Hindi, the Indian national language, is the third most commonly spoken language in the world, with about 615 million speakers [19].
Nepean Dyspepsia Index (NDI) was developed in the year 1999 as a new multi-dimensional disease-specific instrument to measure both symptom severity and HRQOL impairment in patients with dyspepsia [20]. Subsequently, a 10-item Short-Form of Nepean Dyspepsia Index (SF-NDI) was developed to be used in clinical trials of FD [21]. SF-NDI has proved to be a simple and easy to use tool, with short survey length and complexity, which is especially beneficial in regions with limited healthcare resources. SF-NDI has been used as a HRQOL assessment tool in many FD clinical trials, and has been translated and validated in several languages including Malay, Persian, and Kinyarwanda [5, 13, 22].
We aimed to develop and validate a reliable translation of the SF-NDI in Hindi, and to cross-culturally adapt both English and Hindi versions of the SF-NDI. We also aimed to assess the impact of FD on HRQOL among English- and Hindi-speaking FD patients in India.
Methods
Study design
This cross-sectional multi-centric study was conducted from January 2021 to July 2021 in three academic institutes in northern India, providing secondary and tertiary medical care. The institutional ethics committee approved the project, and all procedures were performed in accordance with the ethical standards of the Helsinki Declaration.
Patients
Consecutive patients with dyspepsia attending the Gastroenterology/Medicine outpatient departments were invited to participate. Inclusion criteria were as follows: age 18–65 years, FD diagnosed according to Rome IV criteria, normal esophagogastroduodenoscopy (EGD) (performed within past 1 year), and negative Helicobacter pylori infection documented by non-invasive testing or gastric biopsy. Exclusion criteria were as follows: presence of alarm symptoms (loss of appetite, loss of weight, dysphagia, anemia, new onset dyspepsia after 50 years age, persistent/recurrent vomiting, hematemesis/melena, severe pain abdomen), presence of another gastrointestinal disorder (e.g. irritable bowel syndrome, celiac disease, inflammatory bowel disease etc.), history of chronic intake of non-steroidal anti-inflammatory drugs (NSAIDs)/salicylates, pregnancy, presence of pancreatic, hepatobiliary, renal or metabolic diseases (uncontrolled diabetes, uncontrolled thyroid disorders) resulting in dyspepsia; history of surgery involving upper gastrointestinal tract, addictions, or significant co-morbidities (advanced cardiopulmonary disease, advanced depression/obscessive compulsive disorders [OCD] etc.). Patients were also excluded if they were unable to speak/understand Hindi or English language.
Procedures
All potentially eligible patients were subjected to thorough history and physical examination. They were categorized into FD sub-types (EPS, PDS or EPS-PDS overlap) according to the Rome IV criteria. [2]. Modified Kuppuswamy socioeconomic scale was used to assess the socioeconomic status [23]. Laboratory investigations including EGD and abdominal ultrasonography were noted. Patients who met inclusion and exclusion criteria received verbal and written information about the study, and written informed consent was taken.
Participants were informed that they would be required to fill SF-NDI questionnaire at two occasions—first, at the time of enrolment, and second time, about 2 weeks later—when they will be contacted on phone. All participants were given a printed copy of SF-NDI questionnaire and socio-demographic questionnaire to complete themselves at the time of enrolment. Participants who were not literate in English were provided the Hindi version of SF-NDI (described below).
Trained assessors were designated to provide guidance about completing SF-NDI questionnaire to every patient, on individual basis. They provided assistance and explanation wherever necessary, and ensured that questionnaire was completely filled. For illiterate patients or patients having physical disabilities, assessors read aloud each item of questionnaire without asking any leading questions, to avoid any discrepancies between patient self-report and external assessment. Two weeks later, study personnel administered same version of SF-NDI questionnaire to all participants over phone. Study personnel were blinded to results of initial evaluation, until second evaluation was completed.
Instruments
Short-Form Nepean Dyspepsia Index
SF-NDI is a self-report questionnaire, which measures severity of symptoms and HRQOL in patients with dyspepsia as experienced in past 2 weeks [21]. It is composed of two distinct, separately scored and interpreted instruments: a symptom checklist and a disease-specific HRQOL measure. The former is made up of a list of 15 common upper gastrointestinal symptoms, which respondents rate in terms of three dimensions: frequency, intensity, and bothersomeness. Assessment is performed by applying a scale of 0 (not at all) to 4 (daily) for frequency; 0 (not at all) to 5 (very severe) for intensity; and 0 (not at all) to 4 (extremely bothersome) for bothersomeness [21]. Total score for each symptom is calculated by adding the scores of all dimensions of each item.
SF-NDI HRQOL questionnaire consists of 10 items with 5 sub-scales, each examining the influence of dyspepsia on various domains of health, namely tension/anxiety, interference with daily activities, disruption to regular eating/drinking, knowledge towards/control over disease symptoms, and interference with work/study. Each sub-scale contains two items, and each item is measured by a 5-point Likert scale ranging from 1 (not at all or not applicable), 2 (a little), 3 (moderately), 4 (quite a lot) to 5 (extremely). The value of each sub-scale and total HRQOL score was re-scaled to a minimum of zero (lowest HRQOL score) and a maximum of 100 (highest HRQOL score) as per the developers’ original calculation formula [20].
Short Form 36 (SF-36) is an established generic HRQOL instrument, which comprises 36 questions in eight different subscales: physical functioning, physical role limitations, bodily pain, general health perceptions, vitality, social functioning, emotional role limitations, mental health, and 2 composite scores—physical component and mental component scores [24]. Maximum score of 100 indicates the best possible health state. This instrument has been translated and validated in Indian population [25].
Development of Hindi version of SF-NDI
After permission from relevant authorities, the original version of SF-NDI was translated into Hindi according to the WHO-QOL methodology of cross-culture adaptation for QOL [26], and methods adopted by previous researchers [5].
Cultural validation of the English version of the SF-NDI
Cross-cultural adaptation of the English version of SF-NDI was performed in 20 English-speaking healthy subjects of varied age and educational backgrounds. In-depth cognitive interviews were conducted to determine appropriateness of the original English version in Indian adults. All words and sentences of the English version of SF-NDI were completely understood, and the instrument was conceptually and semantically acceptable in Indian population. So, no alterations in the original instrument were required.
Translation of the Short-Form Nepean Dyspepsia Index
Hindi version of SF-NDI was developed using standard forward-back translation, following approval by the original instrument developer (Fig. 1). Three forward translations (English to Hindi) were performed independently—two by gastroenterologists with good fluency in both English and Hindi, and third by a commercial translation agency—with aim of achieving conceptual and semantic equivalence. All three forward versions were then reconciled, differences resolved through discussion, and a consensus Hindi version of SF-NDI was developed. Then, two back translations were carried out—one by an English teacher having good understanding of Hindi language also, and with no knowledge of SF-NDI, and second by the commercial translation agency. Finally, a Hindi draft version was derived from reconciliation of the original, back and forward translations. Cognitive interviews using the Hindi draft version were conducted with 20 subjects of varied age and educational backgrounds. Cognitive debriefing was performed till a conceptually and semantically acceptable Hindi version of SF-NDI (SF-NDI-H) was developed.
Statistical analysis
Data were checked for normal distribution using Shapiro–Wilk test. Categorical data are presented as proportions, and continuous data as mean and standard deviation (if parametric) and median and interquartile range (IQR) (if non-parametric). Categorical data were compared using Chi-square test or Fisher’s exact test. Continuous data were compared using t-test, Mann–Whitney U test, or Kruskal–Wallis test, as appropriate. Multiple linear regression analysis was performed to identify factors associated with HRQOL. P-value < 0.05 was considered to be statistically significant. Statistical analysis was done using Statistical Package of Social Sciences (SPSS) version 21 (SPSS Inc., Chicago, IL, USA).
Results
Cross-cultural adaptation of the English version of SF-NDI, translation to Hindi language and adaptation of the Hindi version of SF-NDI (SF-NDI-H) was performed, as described above. SF-NDI Hindi version is presented as Online Resource 1.
Patient characteristics
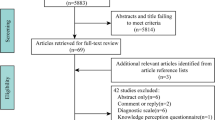
Of the total 257 consecutive patients with suspected FD screened, 43 were excluded (Online Resource 2). Remaining 214 patients were interviewed using SF-NDI symptom and HRQOL questionnaire (146 in Hindi, and 68 in English). Response rate was 98.5% (n = 211, male:female = 115:96). Besides the general instructions and guidance, 51 illiterate patients and 11 other patients required assistance in completing the questionnaire. None of the patients faced any difficulty in understanding the questions in English or Hindi version of SF-NDI. Table 1 summarises the socio-demographic and clinical attributes of study population. Mean duration of dyspeptic symptoms was 2.38 ± 3.1 years.
Dyspepsia sub-types and scores
Of the 211 patients, 86 (40.8%) had EPS, 69 (32.7%) had PDS, and 56 (26.5%) had EPS-PDS overlap. Frequency of individual symptoms, and symptom scores are shown in Table 2. Pain in upper abdomen was the most frequent symptom (47.9%), followed by fullness after eating (36.9%), and nausea (36.0%). Higher symptom scores were reported for symptoms of pain or discomfort in upper abdomen and fullness after eating. Comparison of clinical characteristics of patients with EPS, PDS, and overlap is shown in Table 3. Patients with EPS had significantly lower age, higher male percentage, higher symptom score, and higher HRQOL scores, compared to those with PDS.
SF-NDI HRQOL scores
HRQOL total and sub-scale scores of study population are shown in Fig. 2. The median total SF-NDI HRQOL scores among males and females were 40 (20–47.5) and 37.5 (27.5–47.5), respectively (p = 0.32); among patients with dyspepsia duration < 1 year and ≥ 1 year were 32.5 (22.5–52.5) and 40 (25–47.5), respectively (p = 0.04); and among patients with mild and severe dyspepsia were 26.25 (15–40) and 42.5 (32.5–62.5), respectively (p = 0.001).
Median SF-NDI health-related quality of life total and sub-scale scores of the study population. Boxes denote median and IQR; and vertical lines denote minimum and maximum values. Tension (0,100) = 50 (25 to 62.5); interference in daily activities (0,100) = 50 (25 to 62.5); eating and drinking (0, 100) = 50 (25 to 62.5); knowledge/control (0,100) = 12.5 (0 to 25), work/study (0,100) = 37.5 (25 to 50), total quality of life score (0,100) = 40 (23.75 to 47.5). SF-NDI Short-Form Nepean Dyspepsia Index, IQR interquartile range
In Hindi-speaking group, median total SF-NDI score was 38.75 (25.0–47.5); and SF-NDI sub-scale scores were as follows—tension/anxiety 50.0 (25.0–62.5), interference with daily activity 50.0 (25.0–62.5), eating/drinking 50.0 (25.0–62.5), knowledge/control 12.5 (0–25.0), and work/study 50 (25.0–50.0). In the English-speaking group, the median total SF-NDI score was 40.0 (18.75–48.75); and SF-NDI sub-scale scores were tension/anxiety 50.0 (25.0–56.25), interference with daily activity 50.0 (25.0–50.0), eating/drinking 50.0 (25.0–50.0), knowledge/control 0 (0.0–25.0), and work/study 37.5 (25.0–50.0).
Internal consistency
Internal consistency of both English and Hindi versions of SF-NDI questionnaires was evaluated using Cronbach’s α coefficient. Cronbach’s α coefficient for English version ranged from 0.78 to 0.89, and for Hindi version from 0.79 to 0.86.
Reliability
Out of the 211 patients, 187 (135 Hindi-speaking and 52 English-speaking) participated in the follow-up telephonic interview, which was conducted at a median of 12 days (range 11–17) after the first face-to-face interview. In Hindi-speaking group, intraclass correlation coefficients (ICC) between baseline and follow-up SF-NDI total scores were 0.85 (95% CI 0.81–0.91). In English-speaking group, ICC between baseline and follow-up SF-NDI total scores was 0.89 (95% CI 0.76–0.95). These results demonstrated excellent test–retest reliability.
Validity
Content validity demonstrated moderate to good correlation between Hindi and English versions of SF-NDI sub-scales with various domains of SF-36. Results for Hindi version are as follows:physical functioning (r = 0.37, p < 0.001); physical role limitations (r = 0.51, p < 0.001); bodily pain (r = 0.45, p < 0.001); general health perceptions (r = 0.64, p < 0.001); energy/vitality (r = 0.52, p < 0.001); social functioning (r = 0.38, p < 0.001); emotional role limitations (r = 0.45, p < 0.001). Results for English version are as follows:physical functioning (r = 0.47, p < 0.001); physical role limitations (r = 0.39, p < 0.001); bodily pain (r = 0.30, p < 0.001); general health perceptions (r = 0.37, p < 0.001); energy/vitality (r = 0.54, p < 0.001); social functioning (r = 0.69, p < 0.001); and emotional role limitations (r = 0.49, p < 0.001).
Known groups’ construct validity of the total and sub-scale scores of English and Hindi version of SF-NDI was established relative to the severity of dyspeptic symptoms using Mann–Whitney U test. For total SF-NDI score and all five sub-scale scores, there was significant (p < 0.001) decline of HRQOL for patients with severe dyspeptic symptoms relative to those with mild dyspeptic symptoms (Table 4).
Multivariate analysis of factors associated with HRQOL
Baseline patient-related factors that were evaluated for their potential association with HRQOL were as follows: age, gender, duration of symptoms, dyspepsia symptom severity, and dyspepsia subtype (PDS, EPS, or overlap) (online resource 3). On univariate analysis, factors significantly associated with HRQOL were dyspepsia symptom severity, duration of symptoms, and presence of EPS. On multivariate analysis, dyspepsia symptom severity (r = 0.854; p = 0.021) and duration of symptoms (r = 0.713; p = 0.044) were found to be independently associated with HRQOL.
Discussion
FD, although not a life-threatening disease, has a significant impact on quality of life. FD patients report poor HRQOL, especially in terms of social and environmental aspects, suggesting that more aggressive interventions are needed to improve FD symptoms [27, 28]. To the best of our knowledge, there is no data on the HRQOL among FD patients in India. Also, there is no disease-specific questionnaire available in Hindi language to reliably assess HRQOL among Hindi-speaking patients. In this study, we translated and validated the Hindi version of SF-NDI questionnaire, and assessed HRQOL among a large cohort of FD patients.
Using standard disease-specific validated instruments is an integral part of clinical research. These instruments should be able to evaluate problems in primary healthcare and reliably assess the impact of disease on patient’s HRQOL. Assessing HRQOL in clinical studies has gained much importance as an individual’s satisfaction as a whole, rather than just improvement in specific symptoms, is now being considered the absolute goal of treatment [29]. This is particularly important for diseases such as FD, which lack specific biomarkers or clinical markers for diagnosis and follow-up.
SF-NDI is a standardized questionnaire, which evaluates both symptom severity and HRQOL in patients with FD [21]. It includes questions on various aspects of HRQOL like generalized anxiety, emotional well-being, interference of disease with daily activities, hindrance in consuming desired food items, knowledge of the stomach problem including fear of serious illness and ability/enjoyment of work/study. In this study, we developed the Hindi version of the SF-NDI and determined that it is culturally suitable for Hindi-speaking adults. Both the original English and Hindi versions of the SF-NDI were found to be acceptable and easily understood by Indian patients with dyspepsia, and demonstrated to have good psychometric properties, suggesting that SF-NDI is suitable for use in these patients. Both English and Hindi versions of SF-NDI were found to have good internal consistency, and repeated measurements over a short period showed high correlation, indicating their reliability in Indian population. Content validity of the SF-NDI was demonstrated by comparing it with SF-36, a non-disease specific QOL questionnaire, which has already been validated and adapted for use in India [25]. Both English and Hindi versions of SF-NDI showed moderate to good correlation with various domains of the SF-36. Similar correlation of SF-NDI with generic HRQOL instruments such as SF-36 and SF-12 have been reported previously [21, 30].
In our study, most commonly reported symptoms were pain in upper abdomen (47.9%), fullness after eating (36.9%), and nausea (36.0%), while highest symptom scores were reported for pain or discomfort in upper abdomen and fullness after eating. In a study from Rwanda, indigestion was the most frequent symptom reported (25%), followed by heartburn (22%), regurgitation (15%), and nausea (9%) [31]. In a UK study using Short-Form Leeds Dyspepsia Questionnaire, indigestion was the most frequent symptom (17%), followed by heartburn (13%), regurgitation (8%), and nausea (9%) [32]. In a Chinese study, higher NDI scores were elicited for symptoms of discomfort, bloating, and pain or ache in upper abdomen, and fullness after eating or slow digestion [33].
Various studies, using different QoL questionnaires, have reported negative impact of dyspepsia on HRQOL. In a Korean study, HRQOL scores, evaluated by Korean version of SF-36, were worse for all 8 domains in patients with dyspepsia and irritable bowel syndrome (IBS) compared with those not having chronic gastrointestinal (GI) symptoms [16]. Two Asian studies reported lower HRQOL scores using EuroQOL (EQ-5D) instrument among subjects with dyspepsia (Rome II and III criteria), in rural and urban populations [17, 18]. Studies using SF-NDI in different populations reported a wide variation in the severity of HRQOL impairment among dyspeptic patients. While a Malaysian study reported median total SF-NDI HRQOL score in mild and severe dyspepsia to be 56.3 (22.5–100) and 77.5 (35–100) respectively [5], a study from Rwanda reported total SF-NDI HRQOL of 25 (20–44) in patients with mild dyspepsia, and 56 (20–92) in patients with severe dyspepsia [22]. In our study, median SF-NDI scores among patients with mild and severe dyspepsia were 26.25 (15–40) and 42.5 (32.5–62.5) respectively. Higher HRQOL scores in Malaysian study are likely due to the fact that patients with organic dyspepsia were also included in that study.
The effect of gender on prevalence of dyspepsia and its impact on HRQOL have been reported in several studies [2, 3, 27, 34, 35]. Females with FD have been reported to have poorer HRQOL, and higher anxiety and depression compared to males [27, 28, 36]. A population-based case–control study from Sweden reported that women with FD had significantly poorer QOL including physical function, limited physical role, physical pain, and overall health awareness compared to sex-matched controls [36]. A recent cross-sectional study from Asia reported several factors associated with a low HRQOL in FD patients including female sex, anxiety, depression, old age, severe symptoms, and low educational level [28]. However, in our study, no significant difference was noted in HRQOL scores among males and females. This may be due to the lower percentage of females enrolled in our study, which is likely due to the gender differences in the health-seeking behavior in our region, as highlighted by the lower percentage of females (36.4%) among patients attending gastroenterology Out Patient Department (OPD) in our institute. In concordance with our results, in another recently published Indian study, of the consecutive patients undergoing EGD for dyspeptic symptoms, only 24.7% were females [37]. On the contrary, studies in western populations have reported equal or higher rates of physician-consultation behavior, and school/work absenteeism in dyspeptic women compared to men [38, 39].
EPS and PDS are two distinct subgroups of patients with FD with different symptomatology, and variable responses to dietary and medical therapies [2, 3, 40]. However, till date there is no data on the difference in impact of these two subtypes on HRQOL in FD patients. Our study shows that patients having EPS have a significantly higher (worse) total HRQOL scores compared to those with PDS or overlap. Possible reason for the poorer HRQOL in EPS patients is that the bothersome epigastric pain in these patients occurs throughout the day and is not limited to postprandial period (as in PDS patients), which might have a more negative impact on daily activities and lead to more psychological distress.
On multivariate analysis, factors independently associated with HRQOL were duration of symptoms and dyspepsia symptom severity. Patients with longer duration of symptoms had significantly higher HRQOL scores compared to those with shorter duration. The impact of duration of dyspeptic symptoms on severity of HRQOL impairment has not been reported previously. The effect of dyspepsia severity on HRQOL, as demonstrated in our study, has been reported in previous studies (discussed above) [5, 22].
Besides being the first study assessing the HRQOL among Indian FD patients, some specific strengths of this study are inclusion of a large cohort of patients, and use of an internationally acceptable questionnaire with regional translation and validation performed using a clear and rigorous methodology. Our study fulfils the lacunae of a lack of a validated tool for symptom and HRQOL assessment in Hindi-speaking FD patients. Also, a good diversity of patients with variable education level, occupation, and socioeconomic status enrolled in this study add to its value. Overall, the severe impact of FD on the HRQOL reported in our study further validates the strict definition of FD proposed by Rome IV [2]. Also, the variable impairment of the HRQOL in EPS and PDS sub-groups in our study highlights the importance of sub-grouping of FD patients, which is also important for their differential management [2, 3, 40]. It also highlights the importance that should be placed on diagnosis and treatment of dyspepsia at a population level, as untreated dyspepsia debilitates people and impairs all aspects of HRQOL.
Our study has few limitations. We were unable to assess changes in dyspepsia scores and HRQOL scores over time, as this was a cross-sectional study. Future follow-up studies assessing the change in symptom and HRQOL scores with treatment may be more informative in this regard. Secondly, our results might not be applicable to the general dyspeptic population in the community as our study was carried out in medical centres providing secondary and tertiary healthcare, and we applied strict exclusion criteria for FD like H. pylori infection and major depressive illness. However, the wide range of SF-NDI symptom scores recorded in our study are reassuring, as they indicate the inclusion of patients with a variable severity of dyspepsia. Thirdly, administration of SF-NDI on phone, at the second occasion, to check test–retest reliability could be a potential limitation, but ICC values of 0.85–0.89 suggest that this method is reliable.
To conclude, both the original English SF-NDI questionnaire and its Hindi-translated version (developed in our study) were found to be culturally acceptable, reliable, and valid in Indian population with FD. These can be recommended for use in epidemiological and clinical research studies in Indian population. Indian FD patients were found to have impaired HRQOL, with EPS patients being more severely affected than PDS patients. Factors independently associated with poorer HRQOL were duration of symptoms and dyspepsia symptom severity. Future studies in larger populations including comparison of HRQOL in patients with functional and organic dyspepsia warranted.
References
Miwa H, Ghoshal UC, Gonlachanvit S, et al. Asian consensus report on functional dyspepsia. J Neurogastroenterol Motil. 2012;18:150–68.
Stanghellini V, Chan FK, Hasler WL, et al. Gastroduodenal disorders. Gastroenterology. 2016;150:1380–92.
Ford AC, Mahadeva S, Carbone MF, Lacy BE, Talley NJ. Functional dyspepsia. Lancet. 2020;396:1689–702.
Goyal O, Nohria S, Dhaliwal AS, et al. Prevalence, overlap, and risk factors for Rome IV functional gastrointestinal disorders among college students in northern India. Indian J Gastroenterol. 2021;40:144–53.
Mahadeva S, Wee HL, Goh KL, Thumboo J. Quality of life in South East Asian patients who consult for dyspepsia: validation of the short form Nepean Dyspepsia Index. Health Qual Life Outcomes. 2009;7:45.
Rane SV, Asgaonkar B, Rathi P, et al. Effect of moderate aerobic exercises on symptoms of functional dyspepsia. Indian J Gastroenterol. 2021;40:189–97.
Kumar A, Pate J, Sawant P. Epidemiology of functional dyspepsia. J Assoc Physicians India. 2012;60 Suppl:9–12.
Talley NJ, Locke GR 3rd, Lahr BD, et al. Functional dyspepsia, delayed gastric emptying, and impaired quality of life. Gut. 2006;55:933–9.
VanOudenhove L, Vandenberghe J, Vos R, Holvoe L, Demyttenaere K, Tack J. Risk factors for impaired health-related quality of life in functional dyspepsia. Aliment Pharmacol Ther. 2011;33:261–74.
Haag S, Senf W, Tagay S, et al. Is there any association between disturbed gastrointestinal visceromotor and sensory function and impaired quality of life in functional dyspepsia? Neurogastroenterol Motil. 2010;22:262-e79.
Haag S, Senf W, Häuser W, et al. Impairment of health-related quality of life in functional dyspepsia and chronic liver disease: the influence of depression and anxiety. Aliment Pharmacol Ther. 2008;27:561–71.
Mones J, Adan A, Segu JL, Lopez JS, Artes M, Guerrero T. Quality of life in functional dyspepsia. Dig Dis Sci. 2002;47:20–6.
Azimi M, Zolala F, Baneshi MR, Zahedi MJ. Validation of short-form Nepean Dyspepsia Index in Iranian patients with functional dyspepsia. Govaresh. 2017;22:89–94.
Lee HJ, Lee SY, Kim JH, et al. Depressive mood and quality of life in functional gastrointestinal disorders: differences between functional dyspepsia, irritable bowel syndrome and overlap syndrome. Gen Hosp Psychiatry. 2010;32:499–502.
Mahadeva S, Goh KL. Anxiety, depression and quality of life differences between functional and organic dyspepsia. J Gastroenterol Hepatol. 2011;26 Suppl3:49–52.
Jeong JJ, Choi MG, Cho YS, et al. Chronic gastrointestinal symptoms and quality of life in the Korean population. World J Gastroenterol. 2008;14:6388–94.
Mahadeva S, Yadav H, Rampal S, Goh KL. Risk factors associated with dyspepsia in a rural Asian population and its impact on quality of life. Am J Gastroenterol. 2010;105:904–12.
Mahadeva S, Wee HL, Goh KL, Thumboo J. The EQ-5D (Euroqol) is a valid generic instrument for measuring quality of life in patients with dyspepsia. BMC Gastroenterol. 2009;9:20.
What is the most spoken language? In: Ethnologue. SIL International. 2021. https://www.ethnologue.com/guides/most-spoken-languages. Last accessed 08 Nov 2021
Talley NJ, Verlinden M, Jones M. Validity of a new quality of life scale for functional dyspepsia: a United States multicentre trial of the Nepean Dyspepsia Index. Am J Gastroenterol. 1999;94:2390–7.
Talley NJ, Verlinden M, Jones M. Quality of life in functional dyspepsia: responsiveness of the Nepean Dyspepsia Index and development of a new 10-item short form. Aliment Pharmacol Ther. 2001;15:207–16.
Nkurunziza A, Dusabejambo V, Everhart K, Bensen S, Walker T. Validation of the Kinyarwanda-version Short-Form Leeds Dyspepsia Questionnaire and Short-Form Nepean Dyspepsia Index to assess dyspepsia prevalence and quality-of-life impact in Rwanda. BMJ Open. 2016;6:e011018.
Sheikh S. Modified Kuppuswamy socioeconomic scale update of the year 2020. Indian J Forensic Community Med. 2020;7:1-3
Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston: Nirmond press; 1993.
Sinha R, Van den Heuvel WJ, Arokiasamy P. Validity and reliability of MOS Short Form Health Survey (SF-36) for use in India. Indian J Community Med. 2013;38:22–6.
Leplege A, Verdier A. The adaptation of health status measures: methodological aspects of the translation procedure. In: Shumaker SA, Berzon RA, editors. The international assessment of health-related quality of life: theory, translation, measurement and analysis. Oxford: Rapid Communications; 1995. p. 93–101.
Kim YS, Kim N. Functional dyspepsia: a narrative review with a focus on sex-gender differences. J Neurogastroenterol Motil. 2020;26:322–34.
Hantoro IF, Syam AF, Mudjaddid E, Setiati S, Abdullah M. Factors associated with health-related quality of life in patients with functional dyspepsia. Health Qual Life Outcomes. 2018;16:83.
Halder SL, Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Impact of functional gastrointestinal disorders on health-related quality of life: a population-based case-control study. Aliment Pharmacol Ther. 2004;19:233–42.
Dodds WJ, Hogan WJ, Helm JF, Dent J. Pathogenesis of reflux esophagitis. Gastroenterology. 1981;81:376–94.
Bitwayiki R, Orikiiriza JT, Kateera F, et al. Dyspepsia prevalence and impact on quality of life among Rwandan healthcare workers: A cross-sectional survey. S Afr Med J. 2015;105:1064-9.
Fraser A, Delaney BC, Ford AC, Qume M, Moayyedi P. The Short-Form Leeds Dyspepsia Questionnaire validation study. Aliment Pharmacol Ther. 2007;25:477–86.
Tian XP, Li Y, Liang FR, et al. Translation and validation of the Nepean Dyspepsia Index for functional dyspepsia in China. World J Gastroenterol. 2009;15:3173–7.
Westbrook JI, Talley NJ, Westbrook MT. Gender differences in the symptoms and physical and mental well-being of dyspeptics: a population based study. Qual Life Res. 2002;11:283–91.
Huang I, Pranata R, Pangestu W, et al. The prevalence of uninvestigated dyspepsia and the association of physical exercise with quality of life of uninvestigated dyspepsia patients in Indonesia: an internet-based survey. Indian J Gastroenterol. 2021;40:176–82.
Lacy BE, Weiser KT, Kennedy AT, Crowell MD, Talley NJ. Functional dyspepsia: the economic impact to patients. Aliment Pharmacol Ther. 2013;38:170–7.
Shetty A, Balaraju G, Shetty S, Pai CG. Diagnostic utility of alarm features in predicting malignancy in patients with dyspeptic symptoms. Indian J Gastroenterol. 2021;40:183–8.
Jones R, Lydeard S. Dyspepsia in the community: a follow-up study. Br J Clin Pract. 1992;46:95–7.
Ahlawat SK, Richard Locke G, et al. Dyspepsia consulters and patterns of management: a population-based study. Aliment Pharmacol Ther. 2005;22:251–9.
Goyal O, Nohria S, Batta S, Dhaliwal A, Goyal P, Sood A. Low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols diet versus traditional dietary advice for functional dyspepsia: a randomized controlled trial. J Gastroenterol Hepatol. 2021. https://doi.org/10.1111/jgh.15694.
Funding
Department of Gastroenterology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
OG, PG, HK, JK, PK, and AS declare no competing interests.
Ethics approval
The questionnaire and methodology for this study were approved by the institutional ethics committee (DMCH/R&D/2021/13). All procedures performed were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki Declaration and its later amendments.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Goyal, O., Goyal, P., Kishore, H. et al. Quality of life in Indian patients with functional dyspepsia: Translation and validation of the Hindi version of Short-Form Nepean Dyspepsia Index. Indian J Gastroenterol 41, 378–388 (2022). https://doi.org/10.1007/s12664-021-01233-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-021-01233-0