Abstract
Background
Alteration in the natural history of Crohn’s disease (CD) since the advent of biologic therapy remains to be proven. Our aim was to look at the intestinal surgical rates and the association with biologic therapy over the last two decades.
Methods
This was a retrospective study in which all CD patients seen in two tertiary referral hospitals in Malaysia were recruited. Patients were stratified into two cohorts; cohort 1 was patients diagnosed from year 1991 to 2000 and cohort 2 was patients diagnosed from year 2001 to 2010. These time cohorts were selected based on initial availability of biologic agents in Malaysia in year 2000. Details of demography, disease location, medications and cumulative surgical rates over 7 years were recorded.
Results
A total of 207 patients were recruited: 70 from cohort 1 and 137 from cohort 2. Differences seen in terms of disease location, phenotype, and use of immunomodulatory therapy between the two cohorts were not significant. Patients who were ever exposed to biologics were significantly different between the two cohorts, approximately two times higher at 35.8% (n = 49) in cohort 2, and 18.6% (n = 13) in cohort 1, p = 0.011. There was a significant reduction in the 7-year cumulative intestinal surgical rates between cohort 1 and cohort 2, from 21.4% (n = 15) to 10.2% (n = 14), p = 0.028. However, there was no statistically significant difference in biologic exposure between those who underwent surgery and those who did not.
Conclusions
There has been a significant reduction in intestinal surgical rates for Crohn’s disease over the last two decades but does not appear to be associated with the increased use of biologics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Crohn’s disease (CD) remains one of the most challenging gastroenterological conditions to manage and previously up to 70% of patients with CD would expect to have at least one major operation [1]. This is due to the fact that the disease may progress from chronic inflammation to complications such as fistula, abscess, perforation and strictures [2,3,4]. Complication rates remained high despite the improvement in management of CD over the years. The introduction of anti-TNFs in the late 1990s has resulted in a paradigm shift in the management of this condition. However, alteration in the clinical course since the advent of biologic therapy remains to be proven. Furthermore, biologic usage is a huge burden to the health care system, especially in resource-limited countries such as Malaysia. A study in Netherlands found that biologics has superseded hospitalization and surgical costs in treatment of CD [5]. Hence, usage of biologics needs to be justified based on cost-benefit analysis.
Biologic therapy (mainly anti-TNFs), which was introduced in the management of Crohn’s disease in Malaysia in the year 2000 has also been increasingly used in our population. Our main aim of this study is to look at whether or not the introduction of biologic therapy in the country has impacted on the clinical course of the disease, namely the need for major surgery. Our secondary objective is to evaluate the major surgical rates over two decades in the country.
Methods
Study population and design
We retrospectively evaluated all patients who were diagnosed with CD from year 1991 to year 2010 at two major tertiary referral hospitals in Malaysia (University Malaya Medical Centre–[UMMC], and University Kebangsaan Malaysia Medical Centre–[UKMMC]). UMMC and UKMMC are University Hospitals in Greater Kuala Lumpur, Malaysia. Both are major referral hospitals for both government and private hospitals especially in the field of inflammatory bowel disease (IBD) in Malaysia. Only confirmed CD diagnosed based on combination of clinical, endoscopic, cross-sectional imaging and histological investigations were included. Ethical approval was obtained from University Malaya Medical Centre Research Ethics Committee (UMMC MREC) (Reference No.: 201716-4766).
Patients were stratified into two cohorts: cohort 1 (pre-biological era) consisted of patients diagnosed from year 1991 to year 2000 and cohort 2 (post-biological era) included those diagnosed from year 2001 to year 2010. These time cohorts were selected based on initial availability of biologics in Malaysia. Biologic therapy (mainly anti-TNFs) was introduced in the management of Crohn’s disease in Malaysia in year 2000.
Data collection and definition
Data were collected from August 2017 to December 2017. All existing IBD databases, outpatient clinics, inpatients’ available physical and electronic records were reviewed. Details of demography, disease location, phenotypes, medications and whether or not patients underwent surgery, as well as the details of the surgery, were recorded. Data on patients’ baseline characteristics in the first 7 years after the diagnosis of CD in both cohorts were analyzed. Phenotype of disease was defined according to Montreal consensus: non-stricturing, non-penetrating type (B1), stricturing (B2) and penetrating disease (B3) [6]. We only included first significant intestinal surgery such as resection, stoma formation or stricturoplasties for analysis. “Minor” perianal surgical procedures such as seton insertion, incision and drainage and fistulotomy were excluded. The cumulative 7-year surgical rates were then calculated.
Statistical analysis
Data was analyzed using IBM SPSS version 21 (SPSS, Inc.). Continuous variables were presented as means and standard deviations (SD) and compared using unpaired t test. Association between two qualitative variables was studied by Pearson’s Chi-square test. Kaplan–Meier plots were used to estimate the cumulative surgical rates. Kaplan–Meier curves were compared using log-rank test. Binary regression analysis was used to calculate the relation between the use of immunomodulators and biologics and the intestinal surgical rates. P-value of less than 0.05 was considered significant.
Results
Baseline demography
A total of 511 patients were screened and only 207 were recruited: 70 from cohort 1 and 137 from cohort 2 (Fig. 1). Comparison of the baseline demography of the two cohorts is shown in Table 1. Disease locations for both cohorts were similar: terminal ileum 20.0% vs. 17.5%, colon 37.1% vs. 48.9%, ileocolon 40.0% vs. 30.7% in cohorts 1 and 2, respectively (p-value = 0.427). There was no statistically difference in phenotype of disease in both the cohorts at time of inclusion: stricturing 28.9% vs. 29.2%, penetrating 18.6% vs. 16.1% in cohort 1 and cohort 2, p = 0.900.
Medical therapy
Patients who were ever exposed to biologics were significantly different between the two cohorts, approximately two times higher at 35.8% (n = 49) in cohort 2, and 18.6% (n = 13) in cohort 1, p = 0.011. Mean time to initiation of biologic therapy was shorter at 4.92 (± 2.70) years and duration longer at 24.43 (± 25.24) months in cohort 2, compared to cohort 1 at 7.75 (± 3.40) years and 11.00 (± 8.72) months, respectively.
There was no statistically significant difference between cohort 1 and cohort 2 in relation to exposure to immunomodulators (e.g. azathioprine, mercaptopurine and methotrexate) (Table 2).
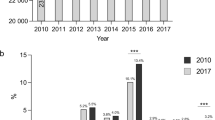
Intestinal surgery
There was statistically significant difference between cohorts 1 and 2 in terms of the 5-year and 7-year cumulative surgical rates; 21.4% (n = 15) vs. 10.2% (n = 14), p = 0.028 for the 7-year cumulative surgical rates and from 15.7% (n = 11) to 6.5% (n = 9), p = 0.035 for 5-year cumulative surgical rates. On the other hand, the cumulative 1-year surgical rates between the two cohorts were similar: 8.6% (n = 6) vs. 5.8% (n = 8) in cohorts 1 and 2, respectively, p = 0.459 (Fig. 2). The main indications for surgery for cohorts 1 and 2 included fibrotic stricture: 40% (n = 6) and 36% (n = 5), and inflammatory disease: 33% (n=5) and 29% (n = 4), respectively. The remaining patients had surgery due to abscess/fistulating disease. When comparing between those who underwent surgery and those who did not within the first 7 years from diagnosis (Table 3), the mean age was not older in the surgery group (29.5 [± 13.7] vs. 25.6 [± 10.8], p = 0.015). However, there was no statistically significant difference in biologic use (34.5% vs. 29.2%, p = 0.566) and immunomodulators exposure (79.3% vs. 79.2%, p = 0.979). Multivariate analysis was not done due to small sample size (number of patients who had surgery).
Within the 7-year after the diagnosis of CD, most patients in both the cohorts achieved clinical remission after surgery. Four patients (27%) in cohort 1 had recurrence after surgery for whom surgery had to be repeated. Three patients (21%) in cohort 2 had recurrence after operation two of whom required a second surgery.
Discussion
Crohn’s disease is relatively uncommon in Asian countries, including Malaysia, but there is a markedly increasing trend of the incidence of CD over the years [7, 8]. As it is a progressive disease, from purely inflammatory to the development of strictures and fistulaes [9], surgical treatment is not uncommonly needed during the course of the disease [10]. Although over the years there appeared to be an improvement in the surgical rates [11,12,13], the complication rates before the biologic era remained high.
Biologic therapy is associated with high rates of mucosal healing and the general consensus is that ‘treating to target’ (i.e. escalating therapy to achieve mucosal healing) will alter the natural history of the disease, thus reducing the need for surgery [14,15,16]. However, the results from the studies on intestinal surgical rates after biologics were largely mixed, whereby although several randomized controlled trials showed that biologics reduced surgical rates, a few real-world data suggested otherwise [17,18,19,20,21].
Apart from the cost factor, biologic therapy was initiated in our centres based on an accelerated step-up approach, where patients were rapidly transitioned to biologic therapy within few months if mucosal healing was not achieved. In our study, 18.6% (n = 13) from cohort 1 and approximately two times higher at 35.8% (n = 49) from cohort 2 (p = 0.011) were ever exposed to biologics, representing the pre- and post-biologic era, respectively. Not surprisingly, the mean time for initiating biologic therapy from diagnosis was shorter and mean duration of therapy longer in cohort 2.
We found that there was a statistically significant reduction in the 7-year cumulative intestinal surgical rates between cohort 1 and cohort 2, from 21.4% (n = 15) to 10.2% (n = 14), p = 0.035. However, there was no difference in phenotype of disease between the two cohorts at the point of data collection: stricturing 28.9% vs. 29.2% and penetrating 18.6% vs. 16.1% in cohorts 1 and 2, respectively. In addition, although patients in cohort 2 were twice as likely to receive biologic therapy, the study failed to show an association between biologic exposure and eventual surgery. In fact, our findings are identical to a recent population-based study of Dutch IBDSL cohort with 1162 patients in which there was no change of progression to complicated phenotype in the pre- and post-biologic era cohorts, even though surgical rates appeared to be reduced in the latter cohort [22].
Results from clinical trials clearly showed that mucosal healing following early initiation of biologic therapy (within 2 years) resulted in prevention of disease progression and decreased hospitalization and surgery but even in the second cohort in our study, the mean time to starting biologic therapy was 5 years; the disease might have already progressed and mucosal healing might not be possible [23]. It is also noteworthy that there was only limited duration of usage among those on biologics, even those in cohort 2 (mean duration of approximately 24 months), which means that in many cases, the use of biologics was not optimized. This is due to the unsustainability of biologics in the long-term as most patients are self-paying or dependent on limited welfare support. Similar to other emerging economies, majority of our patients in public/university hospitals do not have medical insurances and biologics, especially the newer types (e.g. vedolizumab), are often unaffordable.
There were several limitations in this study. As mentioned previously, the total number of patients was small as CD is still a relatively uncommon disease in Malaysia. The median follow up time was relatively short. The time of onset of symptoms to the diagnosis of CD was also not taken into consideration and it may be that in view of increased awareness and better access to endoscopy over the last decade, the mean time to diagnosis of CD was much earlier in the second cohort (i.e. patients were diagnosed at an early stage), therefore resulting in apparently better outcomes (lead time bias). Meanwhile, the patients who required surgery were relatively small and multivariate analysis on factors related to surgery were not possible.
One of the main strengths of the study is that we chose a very objective outcome, which is surgery rather than other more subjective ones such as hospitalization. Hospitalization of patients with CD could be multifactorial, such as for diagnostic purposes and health insurance reimbursement issues, apart from being due to disease activity [4]. On the contrary, assessment of intestinal surgical rates is more objective as surgery will only be performed if clinically indicated.
An ideal follow up study would be a prospective one looking specifically at the cumulative surgical rates in patients who are treated early with biologic therapy, i.e. within the first year of diagnosis. Early treatment with biologics may prove to be even more important for emerging economies as it may allow for exit strategies (with long-term conventional immunomodulators) if mucosal healing is achieved.
In conclusion, in our setting over the last two decades, there has been a significant reduction in intestinal surgical rates for CD, which, however, does not appear to be associated with the increased use of biologic therapy.
References
Vester-Andersen MK, Prosberg MV, Jess T, et al. Disease course and surgery rates in inflammatory bowel disease: a population-based, 7-year follow-up study in the era of immunomodulating therapy. Am J Gastroenterol. 2014;109:705–14.
Solberg IC, Vatn MH, Hoie O, et al. Clinical course in Crohn’s disease: results of a Norwegian population-based ten-year follow-up study. Clin Gastroenterol Hepatol. 2007;5:1430–8.
Zallot C, Peyrin-Biroulet L. Clinical risk factors for complicated disease: how reliable are they? Dig Dis. 2012;30 Suppl 3:67–72.
Golovics PA, Mandel MD, Lovasz BD, Lakatos PL. Inflammatory bowel disease course in Crohn’s disease: is the natural history changing? World J Gastroenterol. 2014;20:3198–207.
van der Valk ME, Mangen MJ, Leenders M, et al. Healthcare costs of inflammatory bowel disease have shifted from hospitalisation and surgery towards anti-TNFalpha therapy: results from the COIN study. Gut. 2014;63:72–9.
Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55:749–53.
Hilmi I, Jaya F, Chua A, Heng WC, Singh H, Goh KL. A first study on the incidence and prevalence of IBD in Malaysia--results from the Kinta Valley IBD epidemiology study. J Crohns Colitis. 2015;9:404–9.
Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn’s and colitis epidemiology study. Gastroenterology. 2013;145:158–65.e152.
Lovasz BD, Lakatos L, Horvath A, et al. Evolution of disease phenotype in adult and pediatric onset Crohn's disease in a population-based cohort. World J Gastroenterol. 2013;19:2217–26.
Burisch J, Kiudelis G, Kupcinskas L, et al. Natural disease course of Crohn's disease during the first 5 years after diagnosis in a European population-based inception cohort: an Epi-IBD study. Gut. 2019;68:423–33.
Ramadas AV, Gunesh S, Thomas GA, Williams GT, Hawthorne AB. Natural history of Crohn’s disease in a population-based cohort from Cardiff (1986-2003): a study of changes in medical treatment and surgical resection rates. Gut. 2010;59:1200–6.
Lakatos PL, Golovics PA, David G, et al. Has there been a change in the natural history of Crohn’s disease? Surgical rates and medical management in a population-based inception cohort from Western Hungary between 1977-2009. Am J Gastroenterol. 2012;107:579–88.
Bernstein CN, Loftus EV Jr, Ng SC, et al. Hospitalisations and surgery in Crohn’s disease. Gut. 2012;61:622–9.
Shah SC, Colombel JF, Sands BE, Narula N. Systematic review with meta-analysis: mucosal healing is associated with improved long-term outcomes in Crohn’s disease. Aliment Pharmacol Ther. 2016;43:317–33.
Akobeng AK, Zachos M. Tumor necrosis factor-alpha antibody for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2004:Cd003574.
Behm BW, Bickston SJ. Tumor necrosis factor-alpha antibody for maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev. 2008:CD006893.
Rungoe C, Langholz E, Andersson M, et al. Changes in medical treatment and surgery rates in inflammatory bowel disease: a nationwide cohort study 1979-2011. Gut. 2014;63:1607–16.
de Buck van Overstraeten A, Wolthuis A, D'Hoore A. Surgery for Crohn’s disease in the era of biologicals: a reduced need or delayed verdict? World J Gastroenterol. 2012;18:3828–32.
Costa J, Magro F, Caldeira D, Alarcão J, Sousa R, Vaz-Carneiro A. Infliximab reduces hospitalizations and surgery interventions in patients with inflammatory bowel disease: a systematic review and meta-analysis. Inflamm Bowel Dis. 2013;19:2098–110.
Jones DW, Finlayson SR. Trends in surgery for Crohn’s disease in the era of infliximab. Ann Surg. 2010;252:307–12.
Lazarev M, Ullman T, Schraut WH, Kip KE, Saul M, Regueiro M. Small bowel resection rates in Crohn’s disease and the indication for surgery over time: experience from a large tertiary care center. Inflamm Bowel Dis. 2010;16:830–5.
Jeuring SF, van den Heuvel TR, Liu LY, et al. Improvements in the long-term outcome of Crohn’s disease over the past two decades and the relation to changes in medical management: results from the population-based IBDSL cohort. Am J Gastroenterol. 2017;112:325–36.
Ma C, Beilman CL, Huang VW, et al. Anti-TNF therapy within 2 years of Crohn’s disease diagnosis improves patient outcomes: a retrospective cohort study. Inflamm Bowel Dis. 2016;22:870–9.
Acknowledgements
The authors would like to thank Dr. Wong Shin Yee and Ms. Lorainne Bt Angal for their assistance in the research project.
Author information
Authors and Affiliations
Contributions
Conceptualization: Ida Normiha Hilmi. Methodology: Kee-Huat Chuah, Raja Affendi Raja Ali and Ida Normiha Hilmi. Formal analysis: Kee-Huat Chuah. Project administration: Kee-Huat Chuah, Raja Affendi Raja Ali and Ida Normiha Hilmi. Visualization: Kee-Huat Chuah, Raja Affendi Raja Ali and Ida Normiha Hilmi. Writing—original draft: Kee-Huat Chuah. Writing—review and editing: Kee-Huat Chuah, Raja Affendi Raja Ali and Ida Normiha Hilmi. Approval of final manuscript: all authors. Supervision: Ida Normiha Hilmi and Raja Affendi Raja Ali.
Corresponding author
Ethics declarations
Conflict of interests
KHC, RARA, and INH declare that they have no conflict of interest.
Ethics statement
The study was performed conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chuah, K.H., Raja Ali, R.A. & Hilmi, I.N. Decreasing major surgical rates for Crohn’s disease in an emerging economy over two decades: Is it due to biologic therapy?. Indian J Gastroenterol 39, 261–267 (2020). https://doi.org/10.1007/s12664-020-01044-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-020-01044-9