Abstract
Purpose
The aim of this study is to evaluate the clinicopathologic prognostic factors of cancer-specific survival (CSS) in hepatocellular carcinoma (HCC) patients who underwent liver transplantation (LT) stratified by tumor size.
Methods
From the Surveillance, Epidemiology, and End Results (SEER) 18 registries (2004–2012), we retrieved data of 570 patients who underwent LT for a solitary primary HCC lesion ≤5 cm. A two multivariable Cox models were constructed to identify prognostic factors of CSS in a two different tumor sizes (2 cm cutoff).
Results
Out of 570 HCC patients (median age 57 years), 16% had microvascular invasion (MVI) and 12% had a poorly differentiated tumor. Male sex (odds ratio [OR] 2.6), tumor size >2 cm (OR 1.78), elevated AFP (OR 2.31), and poor tumor differentiation (OR 2.59) are significant predictors of MVI. With a median follow up of 41.5 months (range 1–107 months), the 5-year CSS rate was 90% in the absence of MVI compared to 75% in the presence of MVI (p<0.001). Multivariate models revealed that age ≥60 years (hazard ratio [HR] 2.08), MVI (HR 2.26), and poor tumor differentiation (HR 2.42), were significant risk factors of a dismal CSS with HCC size >2 cm, but not with HCC ≤2 cm.
Conclusions
Primary HCC tumor size ≤2 cm had an excellent prognosis after LT and was not affect by the presence of MVI or poor tumor differentiation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common malignant tumor and the third leading cause of cancer-related deaths, worldwide [1]. The incidence of HCC is tripled since 1980 in the USA [2]. Approximately 40% to 80% of HCCs detected are solitary, and half of them are surgically treated [3]. Currently, 4.5% of recipients on the waiting list in the USA for a liver transplant are HCC [4].
In patients with HCC diameter less than or equal 5 cm who underwent liver transplantation (LT), the 5-year overall survival (OS) was 71% [5]. The HCC recurrence rate after LT in era before Milan criteria was >60%, but after Milan criteria was <10% [6, 7]. It is noteworthy, although LT depends on strict macromorphological selection criteria (size and number of nodules), that these criteria may have prognostic limitations [8]. Microvascular invasion (MVI) and high histopathologic grading were detected in 16%, and 11% of HCC underwent surgical modalities [9, 10]. MVI should be considered in HCC treatment strategies, as it is a predictor for survival and recurrence after tumor resection or LT [11]. Several studies clarify prognostic role of pre-LT variables such as tumor size, tumor multiplicity, vascular invasion, histopathologic grading, and serum alpha-fetoprotein (AFP) level in HCC patients [12–14].
The current American Joint Committee on Cancer (AJCC) 7th edition classifies all solitary HCCs as T1 or T2 based on MVI regardless of tumor size that had an implication on survival. Thus, recent reports [15–17] proposed modification of the AJCC 7th classification by including size of lesions (cutoff size ≤2 cm) in a solitary HCC of AJCC staging system. According to all of the above, this US population-based study was aimed at evaluating the clinicopathologic risk factors including MVI and tumor grading for cancer-specific survival (CSS) in patients with a single HCC lesion who underwent LT, stratified by tumor size. In addition, we addressed the clinical predictors of pre-LT MVI and tumor differentiation. To our knowledge, no population-based reports addressed these issues in the USA.
Methods
Data source and subjects
The Surveillance, Epidemiology, and End Results (SEER) database currently collects and publishes cancer incidence and survival data from 18 population-based cancer registries, covering approximately 28% of the US population. Herein, we retrieved data of 1162 patients who underwent LT for a single primary HCC lesion ≤5 cm, which were identified by International Classification of Diseases for Oncology, 3rd edition (ICD-O-3 morphology codes; 8170–8175) [18] between 2004 and 2012 from the 18 SEER registries (www.seer.cancer.gov/data). Of 1162 patients, 479 (41.2%) had a tumor diameter ≤2 cm, 163 (14%) had a MVI, and 95 (8.2%) had a high histological grade (III-IV). The final cohort was 570 patients after exclusion of (1) cases diagnosed by autopsy or death certificate, (2) cases without active follow up, and (3) cases with incomplete information of follow up time, AFP, and pathologic data. The MIV in a SEER data was identified by variable “CS extension (2004+).” The LT was identified according to the SEER site-specific surgery (total hepatectomy and transplant; code = 61) in the SEER variable of “RX Summ--Surg Prim Site.” The selection of variables of the SEER database of HCC has been fully described in a previous SEER study by El-Fattah et al. [19]. We also excluded fibrolamellar HCC, as it has a different epidemiology and prognosis compared to other histologic variants of HCCs [20]. We select tumor size ≤2 cm as a cutoff value in analysis, as recent studies revealed that prognostic role of MIV had been disappeared in HCC size ≤2 cm compared to >2 cm [15–17]. However, these studies have not collected a large number of patients [16] or collected patients from a multicenter in different countries (USA, France, and China) [15] and therefore have been susceptible to bias. In the SEER database, it is not clear whether the size of the tumor or tumor biopsy is obtained from explant liver or preoperative imaging. In a SEER data, the CSS was defined as the interval between the date of HCC diagnosis and the date of HCC-related death. The OS was the interval between the date of diagnosis to the date of death from any cause or date of last follow up. Data were censored on December 31, 2012, from the date of HCC diagnosis.
Statistical analysis
Categorical variables were expressed as proportional and continue variables as median and range/or interquartile range (IQR). Categorical data were compared using χ 2 or Fisher’s exact test as appropriate. Overall survival and cancer-specific survival curves were calculated using the Kaplan–Meier method and compared using the log-rank test. Two multivariable Cox regression models were used to identify prognostic factors of CSS in two different tumor sizes (≤2 and >2 cm). Results were considered statistically significant when a two-tailed test of a p-value of less than 0.05 was achieved. All analyses were performed by Stata version 12 (Stata Corp., College Station, TX, USA).
Results
Clinicopathologic features of patients
The clinicopathological characteristics of the 570 HCC patients with a tumor size ≤5 cm are summarized in Table 1.
The median age at HCC diagnosis was 57 years (IQR 52 to 62 years), 77.4% male (male to female ratio of 4.3: 1), and 77.4% Caucasian. The median tumor size was 2.5 cm (IQR 1.5–3.2 cm), and 222 patients (38.9%) had a tumor size ≤2 cm. More than half of the patients (57.5%) had an elevated pre-LT AFP. MVI was identified in 16% of patients and poorly differentiated tumor in 11.9%. Along a 9-year follow up time, 10% of patients (n = 57) died due to HCC and 12.8% of deaths (n = 73) were due to non-HCC-related causes.
Clinical comparison among the MVI+ and MVI− groups
The clinicopathologic variables of the MVI+ group (presence of MVI) were compared with those of the non-MVI+ group (Table 2 ). The frequency of MVI+ was not related to age groups (p = 0.41), race (p = 0.14), marital status (p = 0.24), or year of diagnosis (p = 0.18). However, the frequency of MVI+ is significantly higher in men than women (17.9% vs. 9.3%; p = 0.019). Notably, as tumor size increased, the frequency of MVI+ increased (≤2 vs. >2 cm; 10.4% vs. 19.5%, respectively; p = 0.00). Patients with an elevated pre-LT AFP had significantly higher MVI compared with those with a normal AFP (20.4% vs. 9.9%, respectively; p = 0.001). The poorly differentiated tumors were significantly higher in MVI+ than MVI− groups (24.2 vs. 9.6; p = 0.000) (Table 2 ). As shown in Table 3, the multivariate logistic regression revealed that the independent predictors of the presence of MVI were male sex (odds ratio [OR] 2.60, 95% confidence interval [95% CI] 1.34–5.06; p = 0.005), tumor diameter >2 cm (OR 1.78, 95% CI 1.05–3.01; p = 0.032), an elevated AFP (OR 2.31, 95% CI 1.37–3.88; p = 0.002), and poorly differentiated tumors (OR 2.59, 95% CI 1.43–4.6; p = 0.002).
Clinical comparison among the poor/undifferentiated and well-moderately differentiated tumor groups
The frequency of poorly differentiated tumor was 15.5% for all tumors measuring >2 cm, compared with 6.3% for all tumors measuring ≤2 cm (p = 0.01) (Table 2 ). In addition, the patients with an elevated AFP had significantly higher poorly differentiated tumors compared to those with normal AFP (14.6% vs. 8.3%; p = 0.02). The frequency of poorly differentiated tumor was not related to age (p = 0.07), sex (p = 0.42), year of diagnosis (p = 0.19), or marital status (p = 0.73). Regarding the race, Asians were more likely to have poorly differentiated tumors compared to white (23.9% vs. 10%; p = 0.009) (Table 2).
Overall and cancer-specific survivals in clinical variables
With a median follow up of 41.5 months (range 1–107 months) in the 570 HCC patients who underwent LT, the 1-, 3-, 5-, and 7-year OS rates were 92%, 81%, 75%, and 68%, respectively, in all patients and CSS rates were 97%, 92%, 87%, and 84%, respectively. Patients 60 year or older, those with tumor diameter >2 cm, and those with an elevated AFP have a worse 5-year CSS than patients aged <60 years, tumor ≤2 cm, and normal AFP, respectively (81% vs. 91%; p = 0.004; 84% vs. 93%; p = 0.000, and 84% vs. 92%; p = 0.04, respectively). Sex (p = 0.06), race (p = 0.06), and marital status (p = 0.3) have no impact on CSS (Table 1).
Overall and cancer-specific survival rates according to tumor biology
Survival outcomes in MVI+ and MVI− groups
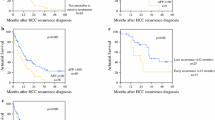
The 1-, 3-, and 5-year OS rates were 88%, 71%, and 66%, respectively, in MVI+ groups compared to 93%, 83%, and 77%, respectively, in MVI− groups (p = 0.04). The 1-, 3-, and 5-year CSS rates were 95%, 81%, and 75%, respectively, in MVI+ groups compared to 98%, 94%, and 90%, respectively, in MVI− groups (p = 0.000) (Table 1 ). In HCC size <2 cm, MVI had no impact on CSS, whether in univariate or multivariate analysis (Fig. 1 ). However, in HCCs >2 cm, patients with MVI+ had 2.26-fold (p = 0.01) significantly higher risk of cancer-specific mortality compared with MVI− after adjusting for age, gender, AFP, and tumor differentiation (Table 4, Fig. 2 ).
Survival outcomes according to tumor differentiation
The 1-, 3-, and 5-year OS rates were 93%, 83%, and 78%, respectively, in well-moderately differentiated tumor compared to 89%, 70%, and 57%, respectively, in poorly differentiated tumors (p = 0.005). The 1-, 3-, and 5-year CSS rates were 97%, 94%, and 91%, respectively, in well-moderately differentiated tumor compared to 95%, 78%, and 64%, respectively, in poorly differentiated tumors (p = 0.000) (Table 1 ). In a multivariate Cox regression analysis adjusted for age, gender, AFP, and MVI, the patients with a poorly differentiated HCC have a 2.26-fold higher risk of cancer-specific mortality than those with well-moderately differentiated tumors, only in a tumor diameter >2 cm (Table 4 ).
Prognostic factors of cancer-specific mortality stratified by tumor size
Our multivariate Cox regression analyses (Table 4 ) revealed that age ≥60 years (HR 2.08, 95% CI 1.16–3.73; p = 0.01), MVI (HR 2.26, 95% CI 1.21–4.20; p = 0.01), and poor tumor differentiation (HR 2.42, 95% CI 1.32–4.44; p = 0.004) were significant risk factors for unfavorable CSS with HCC size >2 cm, but not with HCC ≤2 cm. Gender, years of diagnosis, and AFP are not associated with CSS, regardless of tumor size. It is clear that the impact of tumor pathology (MVI and grading) on CSS after LT is depending on tumor size (2-cm cutoff value).
Discussion
The data from this study confirms that primary HCC tumor size ≤2 cm had an excellent prognosis after LT and was not affected by the presence of MVI or poor tumor differentiation. Thus, resection for pathological assessment prior to LT for HCC could be not necessary (in HCCs sized ≤2 cm), and integration of tumor size in a solitary HCC of 7th AJCC staging system is a candidate. Again, as the current AJCC 7th edition classifies all solitary HCCs as T1 or T2 based on MVI regardless of tumor size, we support recent reports proposing modification of this classification by including size of lesions (cutoff size ≤2 cm) in a solitary HCC [9, 15–17].
In our study, patients aged ≥60 years had a significantly poor 5-year CSS (81% vs. 91%) and having risk of cancer-specific mortality of 2-fold (HR 2.08; p = 0.01) in HCCs diameter >2 cm. It seems that the age played an important role in survival as did MVI (HR 2.26; p = 0.01) or tumor differentiation (HR 2.42; p = 0.004). Some studies reported a poorer survival after LT in young HCC patients than older ones, because they have an aggressive tumor biology [21, 22], while other studies showed opposite results [23, 24]. In general, age may play a paradoxical role in the prognosis of HCC patients after LT [22, 25].
In the entire cohort, the 5-year OS was 75% (95% CI 70–78), the outcome expected for patients who meet the Milan criteria [26]. Mazzaferro and colleagues [26] pointed out that OS in HCC transplanted patients met the Milan criteria was 73.3%. Moreover, Tamura et al. [5] stated that, after LT, 5-year OS in patients with tumors sized ≤5 cm was 71%, which was the same survival of LT in non-HCC cirrhotic patients. We also found that 5-year CSS was 87% in all patients, which was higher, compared to reports coming from Korea (71.4%) [27] and Canada (79%) [28]. After introduction of MELD allocation (model for end-stage liver disease) in 2002, 5-year OS and 5-CSS survival of HCC after LT was 71% and 95%, respectively [4].
In the present work, the prevalence of MIV was 16% in all patients, which was higher compared to MVI that presents in 11% of HCC patients who underwent LT within the Milan criteria in a recent report [26]. In a prospective study [9] of 1786 HCC South Korean patients who underwent tumor resection, MVI was 16%. We also observed that 10% of patients with HCC diameter ≤2 cm had MVI that was much lower compared to 27% reported in other western patients having the same tumor size [16]. The prevalence of MVI in HCCs has widely ranged from 15% to 57%, which could be attributed to interobserver/intraobserver variability [29]. Moreover, the risk of MIV depends on tumor size, which rises up to 41% of patients transplanted outside the Milan criteria [26]. A recent meta-analysis [30] of transplanted patients revealed that MVI and poorly differentiated tumors are detected in 10% to 15% and 13% to 33%, respectively, in patients met the Milan criteria, compared to 35% to 56% and 38% to 50%, respectively, in patients not meeting the Milan criteria.
We stratified multivariate analysis by tumor size (2-cm cutoff value) and observed that the MVI and the high histological grading were associated with 2.26- and 2.42-fold increased risk of cancer-specific mortality, respectively, only in HCC size >2 cm. However, these associations disappeared in a HCC diameter ≤2 cm. In agreement with our findings, a recent multicenter study pointed out that small HCCs (≤2 cm) are associated with an excellent prognosis regardless of the status of MVI [15]. It seems that the prognostic impact of MIV on HCC outcome after LT is dependent on tumor size.
We observed that the 5-year CSS rates for patients with and without MVI were 75% and 90%, respectively. A retrospective study of 155 HCC patients met the Milan criteria and underwent LT; the 5-year CSS was 79% [28]. Sumie et al. [31] demonstrated that among 110 resected HCC, the 5-year CSS was 59.3% and 92% in patients with and without MVI, respectively. Therefore, some investigators have proposed referring all patients found to have MVI after hepatic resection for liver transplantation due to the significant risk of recurrence [32].
In the current study, male sex (OR 2.60), tumor size >2 cm (OR 1.78), an elevated AFP (OR 2.31), and poorly differentiated tumor (OR 2.59) significantly predict presence of MVI. In literature, female patients tend to have more favorable tumor biology of HCC at initial diagnosis compared to male [33]. Regarding tumor size, Esnaola et al. [34] reported that tumor size greater than 4 cm and high histopathologic grade increased the odds of MVI by 3- and 6.3-fold, respectively. One report stated that tumor size (OR 4.1) and AFP >100 (OR 5) were associated with MVI [35]. Shirabe et al. [36] designed a scoring system and found that tumor size, histological grade of the tumor, and serum des-gamma-carboxy prothrombin levels significantly predict MVI. Recently, maximum standardized uptake value on 2-[18F]-fluoro-2-deoxy-d-glucose positron emission tomography also predicts MVI [37].
A recent meta-analysis [38] of 651 HCC patients who underwent LT concluded that MVI is related to 2.2-fold decrease of 5-year OS. In line with this meta-analysis [38], we found that the presence of MIV increases the risk of mortality 2-fold in a tumor size >2 cm. It is worth noting that the poor survival in MVI and poor tumor differentiation is attributed to their high association with a tumor recurrence [39, 40] and extrahepatic metastasis [10].
In the current work, the frequency of poorly differentiated HCC was 11.9% that was consistent with results of two recent studies investigating HCC lesions ≤5 cm in Japan (10.7%) [10] and China (12%) [41]. Although, multicenter study analyzed clinicopathologic features of HCC patients treated in the USA, France, and Japan that showed histopathologic differences with comparable outcomes [42]. Furthermore, we had reported that poorly differentiated HCCs are associated with worse survival compared with well-moderately differentiated HCC (HR 2.38; 95% CI 1.29–4.36) which was consistent with several reports [8, 43]. The poorly differentiated HCC tumors are at risk of a distant metastasis [10], which, in part, explains poor outcomes. One study found distant metastasis in about 40% of patients with poorly differentiated HCCs sized >3 cm [10].
Our univariate analyses demonstrated that old age, large tumor size, high tumor grading, and elevated AFP are unfavorable prognostic factors for CSS in all patients. In literatures, there were a strong correlation between HCC distant metastasis and tumor size [44], AFP [45], and aggressive tumor biology [44]. Tumor size may be a surrogate marker for vascular invasion and multifocality [40]. Elevated AFP increases risk of HCC recurrence after LT [46], as AFP may promote metastasis of HCC via upregulating expression of metastasis-related proteins [45]. A recent meta-analysis of 535 liver cancer patients demonstrated that circulating liver cancer cells are associated with tumor size, clinical stage, and metastasis [47].
Finally, in our multivariate analysis stratified by tumor size, the independent risk factors for cancer-specific mortality were old age (HR 2.08), MVI (HR 2.26), and poor tumor differentiation (HR 2.42) in tumors sized >2 cm. However, none of these preoperative variables were risk factors for CSS in tumors sized ≤2 cm. Our results are in line with recent reports [15–17] and demonstrated a favorable prognosis of HCC ≤2 cm after LT, regardless of MVI. Jonas et al. [14] pointed out that the tumor diameter and the multiplicity were predictive of a vascular invasion only in HCC larger than 5 cm.
Although our study addresses important issues, it carries a number of limitations to be acknowledged. Unfortunately, the SEER database did not provide information of some independent risk factors (MELD score, etiology of liver disease, partial or live donor grafts, etc.) that can influence outcomes of patients undergoing LT for HCC. However, the data from this study confirms that primary HCC tumor size ≤2 cm had an excellent prognosis after LT, irrespective of MVI or tumor grading. Therefore, I and others proposed the following: (i) first, integration of tumor size in solitary HCC lesion in AJCC staging system; (ii) second, resection for pathological assessment prior to LT for HCC may be not necessary in a tumor size ≤2 cm; and (iii) third, because age is a highly significant predictor for MVI, I propose early pre-LT assessment of MVI in elderly HCC patients.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
El-Serag HB, Kanwal F. Epidemiology of hepatocellular carcinoma in the United States: where are we? Where do we go? Hepatology. 2014;60:1767–75.
Bruix J, Llovet JM. Prognostic prediction and treatment strategy in hepatocellular carcinoma. Hepatology. 2002;35:519–24.
Doyle MB, Vachharajani N, Maynard E, et al. Liver transplantation for hepatocellular carcinoma: long-term results suggest excellent outcomes. J Am Coll Surg. 2012;215:19–28. discussion 28-30
Tamura S, Kato T, Berho M, et al. Impact of histological grade of hepatocellular carcinoma on the outcome of liver transplantation. Arch Surg. 2001;136:25–30. discussion 31
Iwatsuki S, Gordon RD, Shaw BW Jr, Starzl TE. Role of liver transplantation in cancer therapy. Ann Surg. 1985;202:401–7.
Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–9.
Cillo U, Vitale A, Bassanello M, et al. Liver transplantation for the treatment of moderately or well-differentiated hepatocellular carcinoma. Ann Surg. 2004;239:150–9.
Hwang S, Lee YJ, Kim KH, et al. The impact of tumor size on long-term survival outcomes after resection of solitary hepatocellular carcinoma: single-institution experience with 2558 patients. J Gastrointest Surg. 2015;19:1281–90.
Oishi K, Itamoto T, Amano H, et al. Clinicopathologic features of poorly differentiated hepatocellular carcinoma. J Surg Oncol. 2007;95:311–6.
Roayaie S, Blume IN, Thung SN, et al. A system of classifying microvascular invasion to predict outcome after resection in patients with hepatocellular carcinoma. Gastroenterology. 2009;137:850–5.
Han K, Tzimas GN, Barkun JS, et al. Preoperative alpha-fetoprotein slope is predictive of hepatocellular carcinoma recurrence after livertransplantation. Can J Gastroenterol. 2007;21:39–45.
Yao FY, Saab S, Bass NM, et al. Prediction of survival after liver retransplantation for late graft failure based on preoperative prognosticscores. Hepatology. 2004;39:230–8.
Jonas S, Bechstein WO, Steinmüller T, et al. Vascular invasion and histopathologic grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology. 2001;33:1080–6.
Shindoh J, Andreou A, Aloia TA, et al. Microvascular invasion does not predict long-term survival in hepatocellular carcinoma up to 2 cm: reappraisal of the staging system for solitary tumors. Ann Surg Oncol. 2013;20:1223–9.
Roayaie S, Obeidat K, Sposito C, et al. Resection of hepatocellular cancer ≤2 cm: results from two Western centers. Hepatology. 2013;57:1426–35.
Yamashita Y, Tsuijita E, Takeishi K, et al. Predictors for microinvasion of small hepatocellular carcinoma ≤2 cm. Ann Surg Oncol. 2012;19:2027–34.
Fritz A, Percy C, Jack A, et al. International classification of diseases for oncology (ed 3). Geneva: Switzerland, World Health Organization; 2000.
El-Fattah MA, Aboelmagd M, Elhamouly M. Prognostic factors of hepatocellular carcinoma survival after radiofrequency ablation: a US population-based study. United European Gastroenterol J. 2016; doi:10.1177/2050640616659024.
El-Serag HB, Davila JA. Is fibrolamellar carcinoma different from hepatocellular carcinoma? A US population-based study. Hepatology. 2004;39:798–803.
Shimada S, Kamiyama T, Yokoo H, et al. Clinicopathological characteristics and prognostic factors in young patients after hepatectomy for hepatocellular carcinoma. World J Surg Oncol. 2013;11:52.
Chen CH, Chang TT, Cheng KS, et al. Do young hepatocellular carcinoma patients have worse prognosis? The paradox of age as a prognostic factor in the survival of hepatocellular carcinoma patients. Liver Int. 2006;26:766–73.
Niederle IM, Wörns MA, Koch S, et al. Clinicopathologic features and prognosis of young patients with hepatocellular carcinoma in a large German cohort. J Clin Gastroenterol. 2012;46:775–8.
Kim JH, Choi MS, Lee H, et al. Clinical features and prognosis of hepatocellular carcinoma in young patients from a hepatitis B-endemicarea. J Gastroenterol Hepatol. 2006;21:588–94.
Yamazaki Y, Kakizaki S, Sohara N, et al. Hepatocellular carcinoma in young adults: the clinical characteristics, prognosis, and findings of a patient survival analysis. Dig Dis Sci. 2007;52:1103–7.
Mazzaferro V, Llovet JM, Miceli R, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10:35–43.
Hyeon J, Ahn S, Lee JJ, Song DH, Park CK. Prognostic significance of BCL9 expression in hepatocellular carcinoma. Korean J Pathol. 2013;47:130–6.
Shah SA, Tan JC, McGilvray ID, et al. Does microvascular invasion affect outcomes after liver transplantation for HCC? A histopathological analysis of 155 consecutive explants. J Gastrointest Surg. 2007;11:464–71.
Fan L, Mac MT, Frishberg DP, et al. Interobserver and intraobserver variability in evaluating vascular invasion in hepatocellular carcinoma. J Gastroenterol Hepatol. 2010;25:1556–61.
Mazzaferro V, Bhoori S, Sposito C, et al. Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transpl. 2011;17:S44–57.
Sumie S, Kuromatsu R, Okuda K, et al. Microvascular invasion in patients with hepatocellular carcinoma and its predictable clinicopathological factors. Ann Surg Oncol. 2008;15:1375–82.
Sala M, Fuster J, Llovet JM, et al. High pathological risk of recurrence after surgical resection for hepatocellular carcinoma: an indication for salvage liver transplantation. Liver Transpl. 2004;10:1294–300.
Tangkijvanich P, Mahachai V, Suwangool P, Poovorawan Y. Gender difference in clinicopathologic features and survival of patients with hepatocellular carcinoma. World J Gastroenterol. 2004;10:1547–50.
Esnaola NF, Lauwers GY, Mirza NQ, et al. Predictors of microvascular invasion in patients with hepatocellular carcinoma who are candidates for orthotopic liver transplantation. J Gastrointest Surg. 2002;6:224–32. discussion 232
McHugh PP, Gilbert J, Vera S, Koch A, Ranjan D, Gedaly R. Alpha-fetoprotein and tumour size are associated with microvascular invasion in explanted livers of patients undergoing transplantation with hepatocellular carcinoma. HPB (Oxford). 2010;12:56–61.
Shirabe K, Itoh S, Yoshizumi T, et al. The predictors of microvascular invasion in candidates for liver transplantation with hepatocellular carcinoma—with special reference to the serum levels of des-gamma-carboxy prothrombin. J Surg Oncol. 2007;95:235–40.
Kornberg A, Freesmeyer M, Bärthel E, et al. 18F-FDG-uptake of hepatocellular carcinoma on PET predicts microvascular tumor invasion in liver transplant patients. Am J Transplant. 2009;9:592–600.
Rodríguez-Perálvarez M, Luong TV, Andreana L, Meyer T, Dhillon AP, Burroughs AK. A systematic review of microvascular invasion in hepatocellular carcinoma: diagnostic and prognostic variability. Ann Surg Oncol. 2013;20:325–39.
Hameed B, Mehta N, Sapisochin G, Roberts JP, Yao FY. Alpha-fetoprotein level >1000 ng/mL as an exclusion criterion for liver transplantation in patients with hepatocellular carcinoma meeting the Milan criteria. Liver Transpl. 2014;20:945–51.
Shetty K, Timmins K, Brensinger C, et al. Liver transplantation for hepatocellular carcinoma validation of present selection criteria in predicting outcome. Liver Transpl. 2004;10:911–8.
Huang ZY, Liang BY, Xiong M, et al. Severity of cirrhosis should determine the operative modality for patients with early hepatocellular carcinoma and compensated liver function. Surgery. 2016;159:621–31.
Esnaola NF, Mirza N, Lauwers GY, et al. Comparison of clinicopathologic characteristics and outcomes after resection in patients with hepatocellular carcinoma treated in the United States, France, and Japan. Ann Surg. 2003;238:711–9.
Zheng SS, Xu X, Wu J, et al. Liver transplantation for hepatocellular carcinoma: Hangzhou experiences. Transplantation. 2008;85:1726–32.
Jun L, Zhenlin Y, Renyan G, et al. Independent factors and predictive score for extrahepatic metastasis of hepatocellular carcinoma following curative hepatectomy. Oncologist. 2012;17:963–9.
Lu Y, Zhu M, Li W, et al. Alpha fetoprotein plays a critical role in promoting metastasis of hepatocellular carcinoma cells. J Cell Mol Med. 2016;20:549–58.
Duvoux C, Roudot-Thoraval F, Decaens T, et al. Liver transplantation for hepatocellular carcinoma: a model including α-fetoprotein improves the performance of Milan criteria. Gastroenterology. 2012;143:986–94.
Jin T, Peng H, Wu H. Clinical value of circulating liver cancer cells for the diagnosis of hepatocellular carcinoma: a meta-analysis. Biomed Rep. 2013;1:731–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was not funded.
Conflict of interest
MA El-F declares that he has no conflict of interest.
Human informed consent
There were no human consents, as this study was a retrospective database report.
Rights and permissions
About this article
Cite this article
El-Fattah, M.A. Hepatocellular carcinoma biology predicts survival outcome after liver transplantation in the USA. Indian J Gastroenterol 36, 117–125 (2017). https://doi.org/10.1007/s12664-017-0732-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-017-0732-x