Abstract
Aim
To provide a concise review on risk factors, stages, pathophysiology, prevention and possible treatment options for both MRONJ and ORN individually.
Methods
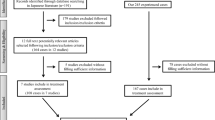
The review was conducted according to the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ (PRISMA) guidelines. A comprehensive search of the PUBMED, Ebsco, SCOPUS, WEB OF SCIENCE and NDH for articles published up until 2021 was performed. After screening and full text analyses, 44 studies were included in this review. Definition, risk factors, etiology, symptoms, stages, pathophysiology, prevention and possible management options were explored and highlighted in this article.
Results
Three studies described osteonecrosis of jaw (ONJ) in general, 15 studies described ONJ associated with radiotherapy and 26 studies described ONJ associated with medications. Both the two conditions (ORN) and (MRONJ) have relatively similar clinical presentations clearing the fact that a resemblance in clinical presentations does not necessarily denote a similar pathophysiology.
Conclusion
However, various advancements have been made in the control and management of ONJ, but until and unless need for high tumoricidal doses exists, ONJ will certainly continue to remain as a clinical challenge demanding satisfactory treatment to improve the quality of life of the patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
‘Osteo-necrosis’ is a process by which the blood flow to the living cells of the bones and bone marrow decreases and the cells die causing the bone to collapse. Initially, the term ‘osteonecrosis’ was used to refer to femoral head avascular necrosis in medical orthopaedics literature and eventually it was found affecting the head and neck area and termed as ‘Osteonecrosis of jaw’. Two main aetiologies of osteonecrosis of jaw that has been described in the literature are medication related osteonecrosis of jaw (MRONJ) and osteoradionecrosis (ORN). However, many sources report positive correlation between MRONJ and ORN and tooth extraction and/ or alveolar trauma and infection [1, 2]. Osteoblasts, osteocytes, osteoclast, and bone lining cells play a role in coordination in replacing mature bone by new bone which is a lifelong process called bone remodelling [3, 4]. Although osteoclasts contribute to bone resorption and their differentiation plays an important role in bone healing and remodelling of all areas of the skeleton, osteonecrosis is more common in the jaw for various reasons related to the anatomical and physiological features of the jaw [3, 4]. When there is imbalance in the regulation of the process of bone metabolism, many skeletal complications including osteoporosis occurs. An epidemic of exposed bone osteonecrosis exclusively in the jaws occurred at around 1858—1906, known as ‘Phossy jaw’ and was linked to ‘yellow phosphorous’, the main ingredient used in factories that makes match [5].Forensic evidences says that yellow phosphorous (P4O10) gets converted into potent amino-bisphosphonate when combined with H2O2 and CO2 by natural chemical reaction in the human body, which was found to be the aetiology behind the phossy jaw [5]. Today’s Bisphosphonates related osteonecrosis of jaw (BRONJ) is the 2nd epidemic of ‘Phossy jaw’ [5]. Bisphosphonate were first synthesized in Germany in 1865 and used to treat a number of metabolic and oncologic pathologies that contribute to the destruction of the skeletal system [6]. ONJ was also found to be related to the anti-angiogenic medication family [7,8,9]. They inhibit osteoclast function and differentiation and increase osteoclast apoptosis which reduces bone turnover in the affected area and reduces angiogenesis, ultimately leading to osteonecrosis [7,8,9]. So, to include all drugs that are effective in causing osteonecrosis of jaw, the American Association of Oral and Maxillofacial Surgery (AAOMS) renamed the term BRONJ to MRONJ considering the increasing incidence of osteonecrosis with other anti-resorptive and anti-angiogenic agents and in 2014 they also published a position paper explaining the same [10]. Also, first report about osteoradionecrosis of jaw (ORN) after radiotherapy was published by Regaud, in 1992 [2]. After that, multiple theories have been given to describe the pathophysiology of ORN among which Hypoxic-hypocellular theory and Radiation-induced fibro-optic theory are the two most accepted one [2, 11]. Definition, aetiology, clinical features, diagnosis, risk factors, pathophysiology, prevention and possible treatment options of both (ORN and MRONJ) have been discussed here.
Discussion
Osteoradionecrosis (ORN)
Radiation therapy in the management of head and neck cancer plays an important role in osteoradionecrosis (ORN) of the jaws. Incidence of ORN ranges from 20–22% and is most often noted in first 3 years after end of treatment [12]. ORN of mandible is more prevalent when compared to maxilla due to poor vascularization and dense bone of mandible relatively.Posterior region of the mandible is more commonly affected by ORN than the anterior region, because of compact and dense bone of the mandible [13]. Incidence of ORN is three times higher in dentate compared to edentulous patients due to trauma and infections from extractions and periodontal disease, respectively [14]. Risk factors associated with development of ORN are—primary site of tumour, proximity of tumour to bone, extent of mandible included in primary radiation field, state of dentition (odontogenic and periodontal disease), poor oral hygiene, radiation dose more than 60 Gy, use of brachytherapy, dental extractions, poor nutrition, concomitant chemo-radiation, acute trauma from surgical procedures to the jaw, tobacco and alcohol abuse and ill-fitting prosthesis causing chronic trauma [15] (Table 2).
ORN occurs after radiation because it changes the lumen of blood vessels, stops tissue perfusion and affects small blood vessels in the bones, leading to endarteritis with the formation of small clots. So, the bone loses its repair and remodelling capacity, and in such condition even a small external trauma causes ulceration and infection leading to bone necrosis. To explain the pathophysiology of ORN some theories have been proposed [2, 11]. According to Meyer’s theory of trauma and infection, the damage facilitates the penetration of oral microflora into the irradiated bone [11]. This theory underlies the widespread use of antibiotics in surgical interventions for the treatment of ORN. Marx’s pathological sequence for explaining his hypoxic-hypocellular theory—irradiation, formation of hypoxic-hypocellular, hypovascular tissue and breakdown of tissues driven by persistent hypoxia that can lead to a chronic non-healing wound [11]. This explanation laid the keystone for the treatment of ORN by using hyperbaric oxygen (HBO) therapy [11]. Radiation-induced fibro-atrophic theory is the newest theory of pathophysiology of ORN which was introduced in 2004 [2, 16]. This theory, states that the main event for the initiation and development of osteoradionecrosis is the aberrant stimulation and regulation of function of fibroblast, that results in tissue degeneration within the area which is irradiated previously [16] (Table 2).
The diagnosis of ORN is arrived at by considering a combination of certain predominant clinical signs such as ulceration of oral mucosa with exposure of necrotic bone along with symptoms of halitosis, pain, paraesthesia, altered taste sensation and food impaction in the concerned area [17] (Table 2).
Measures for prevention of ORN should be evaluated to reduce the risk of ORN—thorough dental check-ups are indicated prior to radiotherapy to rule out decayed tooth with poor prognosis, periodontal disease or with existing infections; dentures should be regularly checked for pressure areas and adjusted to avoid excessive pressure points that may cause pressure ulcers; removal of all mandibular molars in field of > 60 Gy unless the patient has excellent oral hygiene, daily application of topical fluoride, xerostomia patients should be provided with neutral PH saliva substitutes and close follow ups with the patient should be maintained to rule out ORN of the jaws [18]. Advancement in the field of radiation therapy in the form of Intensity Modulated Radiation Therapy (IMRT) have led to reduction in the incidence and severity of ORN as compared to conventional radiotherapy [19]. Based on the pathophysiology of ORN new prevention protocols have been given. Pentoxifylline 400 mg twice daily for 8 weeks with tocopherol 1000 IU, starting a week before the any surgical procedure can be given as prescription [15] (Table 2).
Management of ORN includes conservative as well as surgical measures (Table 2). Conservative treatment includes mouth rinses (saline rinses, NaHCO3 or 0.02% chlorhexidine) and systematic antibiotics along with gentle removal of the sequestrum over the lesion additionally can help in management of early stage of ORN [20]. The new therapeutic regime that includes pentoxifylline and tocopherol acts synergistically and act as a potent anti-fibrotic agent which helps to reverse changes related to radiation-induced fibrosis ultimately preventing its conversion to ORN [20]. Hyperbaric Oxygen Therapy (HBO) was described in 1973 as an adjunct to the treatment of ORN. HBO increases tissue oxygen tension and promotes collagen synthesis, angiogenesis, and epithelization [21]. Wilford Hall HBO osteoradionecrosis protocol given by Marx, stages ORN in its reaction to its HBO management protocol [2], [21]
-
Stage I—30 consecutive exposures—wound shows no improvement clinically—10 more exposures (total of 40 exposures)—if wound fails to heal after 3 months—disease advanced to stage II.
-
Stage II—alveolar sequestrectomy to remove exposed bone and 20 HBO exposures are given (60 exposures in total)—if wound fail to heal—condition is progressed to Stage III
-
Stage III—failure of stage II, pathological fracture, formation of orocutaneous fistula.
According to Marx, HBO therapy alone cannot treat osteonecrotizing bone and suggested combining surgery and HBO therapy [22]. Recommended management includes 30 HBO exposure along with resection to bleeding bone followed by reconstruction and then additional 10 exposures of HBOT. If healing fails, surgery is repeated followed by 10 more HBO treatments [22]. Ultrasound was introduced as a treatment option for ORN in 1992 by Haris, which was found to improve the blood flow to muscle, induce angiogenesis and healing of ischaemic ulcers. Protocol advised was 40e 50v (10 min) ultrasound sessions [23]. Post-op sequels such as bone loss and soft tissue defects cannot be avoided after aggressive surgical procedure, so the reconstruction after such complications is important in view of maintaining the functions and aesthetics [24]. To achieve the superior results after traditional grafting techniques (replacement of dead bone with vascularized bone containing flaps), angiogenic cytokines and bone substitutes are introduced [24].
The current researches approve the theory of radiation-induced fibro-atrophic process in the pathogenesis of ORN in which free reactive oxygen species plays the role and can be reduced by the administration of new therapeutic regime which include administration of pentoxifylline with tocopherol [15].
Medication Related Osteonecrosis of Jaw (MRONJ)
MRONJ, has become an arising disease in recent years because of highly prescribed anti-resorptive as well as anti-angiogenic drugs to treat oncologic and osteoporotic patients. The incidence of MRONJ is reported as 1% in cancer patients and 0.1% in patients with metabolic bone disease and it is more common following dental extractions [25]. MRONJ is more common in mandible (73%) than maxilla (22.5%) and in areas with bone prominences (tori, exostoses, and the mylohyoid ridge) with thin overlying mucosa [26]. Risk factors of MRONJ are many—I.V Bisphosphonates (BPs), zoledronate, dental extractions, periodontal disease, glucocorticoid, chemotherapy, smoking and obesity are the most common [9, 10, 12, 25]. Anti-resorptive drugs (Bisphosphonate and Denosunab) are monoclonal antibodies acting against receptor activator of neuclear factor kappa-B ligand (RANKL) which are found to be causing MRONJ in fewer doses [9, 12]. Anti-angiogenic drugs (Sunitinib and Bevacizumab) are humanized monoclonal antibodies directed against several activated Receptors Tyrosine Kinase (i.e. vascular endothelial growth factor receptor) [9, 12]. Anti-angiogenic therapy is used in the management of malignancies involving ovary, metastatic renal cell cancer, breast cancer, non-small cell lung cancer (NSCLC), colorectal cancer and glioblastoma multiforme [27]. There is a significant relationship between duration of exposure and development of MRONJ of anti-angiogenic medication administered with anti-resorptive medication [27]. Few case reports have also found an association between ONJ and isolated use of infliximab (chimeric human-murine IgG1 monoclonal antibody) and sorafenib (tyrosine kinase inhibitor used as anti-angiogenic) [28, 29]. Steroid and methotrexate are the newly added drugs that may be associated with MRONJ [30]. Concomitant use of BPs or denosumab along with corticosteroids increases the risk of developing ONJ. Methotrexate(cytotoxic medication) is a drug which is indicated in the treatment of a number of solid tumours, haematological malignancies and rheumatoid arthritis is also found to cause ONJ if used concomitantly along with BPs/denosumab [30]. Some systemic and local risk factors in the development of MRONJ are diabetes and anaemia have also been found [30] (Table 2).
Many hypotheses have been suggested for pathophysiology of MRONJ (Table 2)
-
(1)
Imbalance in osteoblasts and osteoclasts in bone remodelling—osteoclast help in bone resorption and the absorbed bone is replaced by fresh bone produced by osteoblast [31]. Apoptosis of osteoclast and inhibition of its differentiation and function resulting in decrease in bone resorption are the actions of BPs and other anti-resorptive drugs [31, 32]. Osteoclasts in the jaw are more sensitive to BPs than those in the long bones due to presence of less amount of fat than other bones [31, 32]. Though BPs are successfully used to treat many bone diseases like paget’s disease, osteoporosis but it can affect the survival of osteoblasts and their progenitor cells if it reaches its toxic level within a bone [31,32,33]. Also in a recent study, it was found that treatment with BPs reduces the expression of BMP-2 (bone morphogenicprotein-2) which has a major role in bone remodelling, development, and osteoblast differentiation [34]. There is suppression of early differentiation marker Type 1 collagen, intermediate differentiation marker such as osterix and alkaline phosphatase (ALP), and the late differentiation marker osteocalcin [34]. BP treatment alters the RANKL-OPG complex which stimulates osteoclasts via its receptor RANK [31, 34]. Recently developed drug Denosumab inhibit osteoclasts by blocking RANKL-RANK interaction and thus decrease bone resorption [35]. As a result, decrease in bone turnover occurs and the expression of RANK is altered by multiple signalling pathways, giving rise to accumulation of non-renewed and hypermineralized bone [35]. So, it was found that the signalling pathway of RANK/RANKL/OPG is triggered in MRONJ subjects [35].
-
(2)
Inhibition of angiogenesis—angiogenesis is regeneration of new blood vessels facilitated by VEGF which is a very important process for viability of body organs including bones. Seeing that the cancer cellstaking advantage of angiogenesis intumour invasion and metabolism, anti-angiogenic drugs have been introduced [7, 12]. In early 2000, avascular necrosis was given as one of the early theories of MRONJ. In addition, on a clinical level, mandible was found to be more prone to avascular necrosis than maxilla due to lower vascularity and dense compact bone of mandible [34]. Role of zoledronic acid in decreasing the level of VEGF has also been reported in literature [34].
-
(3)
Immune system dysfunction—bone remodelling is closely linked to immune system. Neutrophils helps in defence mechanism to promote wound healing following non-infectious injuries and this ability of neutrophils is altered by MRONJ [34, 36]. BPs causes an inhibitory effect and reduce the liability and differentiation capacity of the macrophage, leading to impaired wound healing in MRONJ affected areas [35, 36]. Drug Denosumab inhibits the RANK-RANKL interaction which being normal increases the production of proinflammatory cytokines and reduces monocytes, resulting in MRONJ [35, 36]. Expression of interleukins (IL6 andIL-36 α) are elevated following treatment with BPs which are related to immune response involving lymphocytes and macrophages [35, 36]. These interleukins are found to be activating STAT 3 pathway and TGF-β pathway, therefore giving evidences of multiple signalling pathway involving in pathogenesis of MRONJ [34, 35].
-
(4)
Soft tissue toxicity—in few literatures it has been found that the BPs are also related to the soft tissue toxicity with mucosal ulceration being the initial pathologic event occurring in MRONJ. It has been found that alteration in TGF-β1 signalling after BP treatment may lead to change in oral mucosal tissue [37].
-
(5)
Infection/inflammation—in the biopsied specimens of necrotic bone removed from the patients with ONJ, various bacteria have been found [34]. In some studies, it was found that MRONJ occurs following extraction of teeth in patient’s having periodontal or periapical infections, while some studies found that patient having periapical and periodontal infection can suffer from MRONJ with or without extraction because number and function of osteoclast are modified by infection [34]. A key factor that is found in thepathogenesis of MRONJ is the presence of IL-36 in the gingival crevicular fluid in the patients with with periodontal disease which is indirectly related to TGF-beta signalling pathway [34].
-
(6)
Other factors relating to pathogenesis of MRONJ are—systemic disease like rheumatoid arthritis, diabetes mellitus, which are in turn related to other pathways of injuries such as microvascular ischaemia and reduced bone remodelling [38]. Some literature also supported genetic factors related to pathogenesis of MRONJ such as single nucleotide polymorphisms (SNPs) which are associated with certain metabolic bone disease [39, 40].
MRONJ shows an area of yellowish white exposed necrotic bone with smooth or ragged surfaces unilaterally (mostly) and bilaterally (less frequently) or sometimes multifocal on clinical diagnosis [41]. Some criteria have been given to confirm the diagnosis of MRONJ—presence of any exposed bone that can be explored through extra-oral or intraoral fistula in the oral and maxillofacial area for eight weeks and there is positive history of treatment with anti-angiogenic or anti-resorptive drugs but not with any radiation therapy [12] (Table 1). A staging system of MRONJ is given depending upon which management of MRONJ is decided [12]
Prevention of MRONJ includes—prophylactic dental intervention before anti-resorptive therapy, dental radiographs of cancer patients before receiving anti-resorptive medications, patient’s education, application of fluoride and chlorhexidine rinses and controlling risk factors such as smoking and alcohol (Table 2). These have been found to reduce the risk of MRONJ by 50% [42].
Established diagnosis of MRONJ can be managed by both with non-surgical conservative therapy and surgical therapy [10] (Table 2). If the MRONJ condition is between stage 0 and stage 1 (and even for certain stage 2 cases), management approach can be conservative which includes, maintenance of optimum oral hygiene, regular dental examination, anti-microbial mouth rinse and systemic antibiotics in addition to non-surgical sequestrectomy [10, 12]. In symptomatic patients along with removal of necrotic bone, careful selection of anti-microbial agents (topical and/ or systemic) is recommended [10, 12]. Antibiotic groups such as Amoxicillin and/ amoxiclav, metronidazole, quinolones, clindamycin and erythromycin can be given. In addition to systemic antibiotics, chlorhexidine mouthwash can be prescribed in order to reduce bacterial load in the oral cavity and this conservative therapy can be continued up to several weeks [10, 12]. If the patient with MRONJ does not respond to conservative therapy, surgery is indicated [12, 43]. Aggressive surgery is done by elevating a full thickness mucoperiosteal flap revealing the whole region of the exposed bone and beyond the healthy margins with proper mobilization and closure to accomplish tension free mucosal healing [43]. Additionally, along with the established conservative and surgical treatment options, laser assisted surgical debridement, administration of ozone oil or platelet-rich plasma or platelet derived growth factor over the surgical wound have also been explored [44].
Conclusion
Osteonecrosis of jaw, occurs in patient with bone diseases undergoing systemic anti-resorptive therapy (or) anti-angiogenic therapy (or) radiotherapy, makes the disease multifactorial. Both the two conditions (MRONJ and ORN) have relatively similar clinical presentation clearing the fact that a resemblance in clinical presentation does not necessarily denote a similar pathophysiology. Stage 0 of ONJ has gained more attention currently as bone necrosis does not always lead to bone exposure. Stage I, II and III clinical ONJ is not diagnosed, provided there is loss of soft tissue probidity [12]. The clinical and microscopic findings in ONJ cases suggests the presence of biofilm mediated infectious process that must be prevented and treated and thus conventional management is favoured by many. But, conservative management with a couple of HBO dives and surgical debridement can turn out to be very costly. So, to lower the financial burden and psychological pressure of the patient, persevering directly to a surgical option can help in cases which are suitable. Patients who have been treated with bone-altering agents but with no visible necrotic bone should be considered ‘at risk’. Prophylactic dental treatment can reduce the prevalence of ONJ before starting of any treatment with anti-resorptive, anti-angiogenic and radiation therapy. Until and unless need for high tumoricidal doses exists, especially in advanced head and neck cancers, ONJ will certainly continue to remain as a clinical challenge demanding satisfactory treatment to improve the quality of life of the patient. Continued clinical studies are required to know the key players in the development, severity, progression and resolution of osteonecrosis of jaw especially in advanced head and neck cancers.
References
Balogh JM, Sutherland SE (1989) Osteoradionecrosis of the mandible: a review. J Otolaryngol 18(5):245–250
Nadella KR, Kodali RM, Guttikonda LK, Jonnalagadda A (2015) Osteoradionecrosis of the jaws: clinico-therapeutic management: a literature review and update. J Maxillofacial Oral Surg 14(4):891–901
Landesberg R, Woo V, Cremers S, Cozin M, Marolt D, Vunjak-Novakovic G, Kousteni S, Raghavan S (2011) Potential pathophysiological mechanisms in osteonecrosis of the jaw. Ann N Y Acad Sci 1218(1):62–79
Shibahara T (2019) Antiresorptive agent-related osteonecrosis of the jaw (ARONJ): a twist of fate in the bone. Tohoku J Exp Med 247(2):75–86
Hoefert S, Hoefert CS, Widmann M (2015) History of osteonecrosis of the jaw. In: Otto S (ed) Medication-related osteonecrosis of the jaws. Springer
Sigua-Rodriguez EA, da Costa RR, de Brito AC, Alvarez-Pinzon N, de Albergaria-Barbosa JR (2014) Bisphosphonate-related osteonecrosis of the jaw: a review of the literature. Int J Dentistry. https://doi.org/10.1155/2014/192320
Pimolbutr K, Porter S, Fedele S (2018) Osteonecrosis of the jaw associated with antiangiogenics in antiresorptive-naive patient: a comprehensive review of the literature. Biomed Res Int 23:2018
Pakosch D, Papadimas D, Munding J, Kawa D, Kriwalsky MS (2013) Osteonecrosis of the mandible due to anti-angiogenic agent, bevacizumab. Oral Maxillofac Surg 17(4):303–306
Lombard T, Neirinckx V, Rogister B, Gilon Y, Wislet S (2016) Medication-related -osteonecrosis of the jaw: new insights into molecular mechanisms and cellular therapeutic approaches. Stem Cells Int 18:2016
Schwartz HC. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update and CTX. Journal of Oral and Maxillofacial Surgery. 2015 Mar 1;73(3):377.
Lyons A, Ghazali N (2008) Osteoradionecrosis of the jaws: current understanding of its pathophysiology and treatment. Br J Oral Maxillofac Surg 46(8):653–660
Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O’Ryan F (2014) Medication-related osteonecrosis of the jaw—2014 Update. J Oral Maxillofac Surg 72(10):1938–1956
Ravindran Rathy SS, Nivia M (2013) Osteoradionecrosis of mandible: case report with review of literature. Contemporary Clin Dentistry 4(2):251
Wan JT, Sheeley DM, Somerman MJ, Lee JS (2020) Mitigating osteonecrosis of the jaw (ONJ) through preventive dental care and understanding of risk factors. Bone Res 8(1):1–2
Fan H, Kim SM, Cho YJ, Eo MY, Lee SK, Woo KM (2014) New approach for the treatment of osteoradionecrosis with pentoxifylline and tocopherol. Biomater Res 18(1):1
Ajila V, Hegde S (2020) Osteoradionecrosis-a review of clinical features and management. Gülhane Tip Dergisi 62(4):213
Chronopoulos A, Zarra T, Ehrenfeld M, Otto S (2018) Osteoradionecrosis of the jaws: definition, epidemiology, staging and clinical and radiological findings. Concise Rev Int Dental J 68(1):22–30
Devi S, Singh N (2014) Dental care during and after radiotherapy in head and neck cancer. Nat J Maxillofacial Surg 5(2):117
Hong TS, Ritter MA, Tome WA, Harari PM (2005) Intensity-modulated radiation therapy: emerging cancer treatment technology. Br J Cancer 92(10):1819–24
Chrcanovic BR, Reher P, Sousa AA, Harris M (2010) Osteoradionecrosis of the jaws—a current overview—part 2: dental management and therapeutic options for treatment. Oral Maxillofac Surg 14(2):81–95
Marx RE (1983) Osteoradionecrosis: a new concept of its pathophysiology. J Oral Maxillofac Surg 41(5):283–288
Sultan A, Hanna GJ, Margalit DN, Chau N, Goguen LA, Marty FM, Rabinowits G, Schoenfeld JD, Sonis ST, Thomas T, Tishler RB (2017) The use of hyperbaric oxygen for the prevention and management of osteoradionecrosis of the jaw: a Dana-Farber/Brigham and women’s cancer center multidisciplinary guideline. Oncologist 22(3):343–350
Gorick CM, Chappell JC, Price RJ (2019) Applications of ultrasound to stimulate therapeutic revascularization. Int J Mol Sci 20(12):3081
Madrid C, Abarca M, Bouferrache K (2010) Osteoradionecrosis: an update. Oral Oncol 46(6):471–474
Murphy J, Mannion CJ (2020) Medication-related osteonecrosis of the jaws and quality of life: review and structured analysis. Br J Oral Maxillofac Surg 58(6):619–624
AlRowis R, Aldawood A, AlOtaibi M, Alnasser E, AlSaif I, Aljaber A, Natto Z (2022) Medication-related osteonecrosis of the jaw (MRONJ): a review of pathophysiology, risk factors, preventive measures and treatment strategies. Saudi Dental J 25:87
Vasudev NS, Reynolds AR (2014) Anti-angiogenic therapy for cancer: current progress, unresolved questions and future directions. Angiogenesis 17(3):471–494
Garuti F, Camelli V, Spinardi L, Bucci L, Trevisani F (2016) Osteonecrosis of the jaw during sorafenib therapy for hepatocellular carcinoma. Tumori J 102:S69–S70
Favia G, Tempesta A, Limongelli L, Crincoli V, Iannone F, Lapadula G, Maiorano E (2017) A case of osteonecrosis of the jaw in a patient with crohn’s disease treated with infliximab. Am J Case Rep 18:1351
Singar S, Parihar AP, Reddy P, Maurya A, Bamaniya V (2020) Medication-related osteonecrosis of the jaw: a review about etiology, risk factors, pathophysiology, and treatment. J Indian Acad Oral Med Radiol 32(1):50
Aghaloo T, Hazboun R, Tetradis S (2015) Pathophysiology of osteonecrosis of the jaws. Oral Maxillofacial Surg Clin 27(4):489–496
Badel T, Savić Pavičin I, Jelinić Carek A, Rošin-Grget K, Grbeša Đ (2013) Pathophysiology of osteonecrosis of the jaw in patients treated with bisphosphonate. Coll Antropol 37(2):645–651
Chang J, Hakam AE, McCauley LK (2018) Current understanding of the pathophysiology of osteonecrosis of the jaw. Curr Osteoporos Rep 16(5):584–595
He L, Sun X, Liu Z, Qiu Y, Niu Y (2020) Pathogenesis and multidisciplinary management of medication-related osteonecrosis of the jaw. Int J Oral Sci 12(1):1–1
Qaisi M, Hargett J, Loeb M, Brown J, Caloss R (2016) Denosumab related osteonecrosis of the jaw with spontaneous necrosis of the soft palate: report of a life threatening case. Case Rep Dentistry 28:2016
Zhang W, Gao L, Ren W, Li S, Zheng J, Li S, Jiang C, Yang S, Zhi K (2021) The role of the immune response in the development of medication-related osteonecrosis of the jaw. Front Immunol 25(12):438
Reid IR, Bolland MJ, Grey AB (2007) Is bisphosphonate-associated osteonecrosis of the jaw caused by soft tissue toxicity? Bone 41(3):318–320
Peer A, Khamaisi M (2015) Diabetes as a risk factor for medication-related osteonecrosis of the jaw. J Dent Res 94(2):252–260
Kim KM, Rhee Y, Kwon YD, Kwon TG, Lee JK, Kim DY (2015) Medication related osteonecrosis of the jaw: 2015 position statement of the Korean society for bone and mineral research and the Korean association of oral and maxillofacial surgeons. J Bone Metabol 22(4):151–165
Katz J, Gong Y, Salmasinia D, Hou W, Burkley B, Ferreira P, Casanova O, Langaee TY, Moreb JS (2011) Genetic polymorphisms and other risk factors associated with bisphosphonate induced osteonecrosis of the jaw. Int J Oral Maxillofac Surg 40(6):605–611
AlDhalaan NA, BaQais A, Al-Omar A (2020) Medication-related osteonecrosis of the jaw: a review. Cureus 12:2
Poxleitner P, Engelhardt M, Schmelzeisen R, Voss P (2017) The prevention of medication-related osteonecrosis of the jaw. Dtsch Arztebl Int 114(5):63
Negrini S, Daleffe F, Audino E, Salgarello S, Castellani A. Surgical treatment of medication-related osteonecrosis of the jaw: technical report and prognosis assessment. Qeios. https://doi.org/10.32388/AWN86A
On SW, Cho SW, Byun SH, Yang BE (2021) Various therapeutic methods for the treatment of medication-related osteonecrosis of the jaw (MRONJ) and their limitations: a narrative review on new molecular and cellular therapeutic approaches. Antioxidants 10(5):680
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kalita, F., Gupta, D.S., Gehlot, N. et al. Osteonecrosis of the Jaws: An Update and Review of Literature. J. Maxillofac. Oral Surg. 22, 344–351 (2023). https://doi.org/10.1007/s12663-023-01876-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-023-01876-w