Abstract
Central giant cell granuloma (CGCG) is an aggressive osteolytic, benign neoplasm of the craniomaxillofacial region. Of all the giant cell lesions, CGCG is the most common and is more prevalent in the Indian population. The etiology and pathogenesis of these lesions still remain an enigma and need to be differentiated from other similar-looking lesions for a proper treatment planning. A case of large destructive CGCG involving the anterior mandibular region, causing extensive bone resorption, and buccal as well as lingual cortical expansion, in a 9-year-old child is presented. It was treated successfully by enucleation and aggressive curettage followed by peripheral ostectomy preserving the continuity of the mandible. Also, a review of the literature has been presented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central giant cell granuloma (CGCG) is a histologically benign, but locally aggressive and destructive osteolytic lesion of osteoclastic origin that occurs in the craniomaxillofacial region, especially in jaw bones [1]. It was first described by Jaffe in 1953 as a giant-cell reparative granuloma of the jaw bones [2].
CGCG is described by the World Health Organization as an intraosseous lesion consisting of cellular fibrous tissue that contains multiple foci of hemorrhage, aggregations of multinucleated giant cells, and some trabeculae of woven bone [3]. It accounts for less than 7% of all benign tumors of the jaws. Mandible is more commonly affected than maxilla [4]. In the mandible, it usually occurs in the body region, anterior to the first molar teeth. It usually affects children and young adults under the age of 30 years, with a predominance for females [5].
Clinically, in most cases, the lesion presents as a solitary, slow-growing swelling of the jaw. It is usually painless, and sensory disturbances are rare. There can be displacement of teeth and cortical perforation [5, 6]. Radiological findings of CGCG may vary from patient to patient, ranging from a small unilocular lesion to large multilocular lesions with displacement of teeth and tooth germs, root resorption, and cortical perforation. Histologically identical lesions occur in patients with known genetic defects such as Noonan syndrome, cherubism, or neurofibromatosis type 1 [7].
In this article, we describe a case of CGCG in the anterior mandible of a 9-year-old boy. Also, a review of the literature has been presented.
Case Report
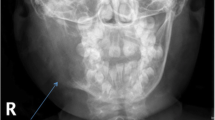
A 9-year-old male child was brought to our institution by his parents with the complaints of a slowly growing, painless swelling in the anterior lower jaw region for the past two months. Past medical, dental and family histories were noncontributory. Extraorally, there was a diffuse, roughly spherical swelling on the right side of the anterior mandibular region measuring approximately 4.5 × 3.5 cm. The skin overlying the swelling appeared normal, with no visible pulsations or secondary changes. On palpation, the swelling was bony hard in consistency, nontender, noncompressible, and nonpulsatile. No paresthesia was noted. No expansion of the inferior border of the mandible was noted. Mouth opening was unrestricted. There was no regional lymphadenopathy noted. On intraoral examination, a bony hard, nontender swelling was noted in the anterior mandibular region extending from 32 to 44 region. There was appreciable buccal and lingual cortical plate expansion in the area with visible displacement of 42. The overlying mucosa showed no secondary changes, or sinus opening, with no change in color and appearance. An orthopantomogram (OPG) was acquired. In the OPG, the lesion appeared to have a multilocular radiolucency with well-defined margins at certain areas and ill-defined margins at other areas. It was seen extending from the root tips of 32 and the developing canine on the left side of the mandible to the developing first premolar and the canine tooth bud and its follicle on the right side of the mandible. There was marked deviation of 31, 32, 41 and 42 (Fig. 1). An incisional biopsy was performed, and the histopathological report for the lesion revealed CGCG.
The surgical plan involved aggressive surgical curettage and peripheral ostectomy of the lesion under general anesthesia. Vertical releasing incisions along with crevicular incision were placed to expose the site. The lesion was covered by a thin shell of bone which was perforated in several areas, exposing the mass within. Once the almost eggshell thin areas of overlying bone were nibbled away with rongeur forceps, the mass was exposed to view. It appeared reddish brown in color, interspersed with hemorrhagic areas welling up with blood. The mass had a soft spongy texture. The lesion was removed in pieces (Fig. 2). Vigorous curettage of the residual bony cavity was carried out, followed by peripheral ostectomy using vulcanite burs. The oozing from the underlying bone was controlled using bone wax and electrocautery. Hemostasis was achieved, and closure was done with resorbable vicryl 3–0 sutures.
Postoperative recovery of the patient was uneventful. The postoperative pain and edema were controlled with analgesic anti-inflammatory drugs, and the patient was placed on intravenous broad-spectrum antibiotics for 5 days. The excised tissue mass was sent for pathological examination and was confirmed as CGCG. There is no clinical or radiographic evidence of recurrence of the lesion till date (Fig. 3).
Discussion
Proper identification and diagnosis of tumors of the craniomaxillofacial region can be quite challenging. CGCG are often confused with other pathologies such as the brown tumor of hyperparathyroidism, giant cell tumor, non-ossifying fibroma and other osteolytic lesions of the jawbones associated with giant cells histologically like cherubism, aneurysmal bone cyst and so on, and needs to be differentiated from them [9]. Although rare, lymphoid neoplasia such as non-Hodgkin's lymphomas can also manifest themselves in intraoral locations, including the jaw bones and hence, justify their inclusion in the differential diagnosis of CGCG [5].
Chuong et al [10] in 1986 and Ficarra et al [11] in 1987 suggested categorizing CGCG into aggressive and non-aggressive types based on their clinical and radiographic characteristics. Commonly, lesions are non-aggressive, painless and grew slowly. Only 20% of patients present with pain or paresthesia. Radiographically, they appear as well-defined unilocular or multilocular radiolucencies with undulating borders. Aggressive lesions are encountered in a younger age group and tend to grow faster and recur more often. Radiographically, these lesions have ill-defined borders with variable amounts of cortical destruction. This is especially true for maxillary lesions [7].
Management of CGCG is controversial and differs according to the nature, size and location. Various treatment modalities have been suggested in the literature such as surgery, radiation, interferon, intralesional steroids and tyrosine kinase inhibitors (Imatinib) [12, 13]. The gold standard of treatment of CGCG is surgical curettage or, in aggressive lesions, resection. In our case, aggressive curettage with peripheral ostectomy was done. However, while using surgical curettage, undesirable damage to the teeth or tooth germs and the jaw is often unavoidable and recurrences are frequent [8]. Prognosis is good when complete removal is achieved. Early diagnosis, intervention and treatment produce a better outcome [5]. Curettage used in combination with cryotherapy may reduce the rate of recurrence, which has been reported to be > 50% when curettage alone is used. Radiation can also be used as a therapeutic modality, but the subsequent development of sarcoma has been reported 5].
Although studies done by M A Pogrel [14], Bayrak NB et al. [15] and Tabrizi et al. [16] suggested calcitonin as a treatment modality, one randomized controlled trial found no improvement in results compared to placebo [17]. A combination of surgery and adjuvant interferon therapy has shown promising results in another study specific for aggressive CGCG, with increased tumor control and decreased operative morbidity [12].
Conclusion
Early and prompt diagnosis and management of CGCG can greatly improve morbidity and long-term outcomes. As children and young adults are usually affected, early management can help in reducing the chances of recurrence requiring further ablative surgical procedures. An early and accurate diagnosis can be made with the help of panoramic radiographs, computed tomographic scans, blood and urine investigations (to rule out metabolic disorders producing radiographically similar lesions of the bone), and histopathological examination of biopsy specimens from the lesion. Although aggressive curettage with peripheral ostectomy is effective in treatment for the majority of CGCG of the jaws, aggressive lesions should be treated by surgical resection.
References
Dimitrakopoulos I, Lazaridis N, Sakellariou P, Asimaki A (2006) Giant-cell granuloma in the temporal bone: a case report and review of the literature. J Oral Maxillofac Surg 64:531–536
Garg P, Jain J, De N, Chatterjee K (2017) A central giant cell granuloma in posterior part of maxilla - a case report. Int J Surg Case Rep 30:222–225
Barnes L, Everson J, Reichart P (2005) WHO Classification of Tumours. Pathology and Genetics of Head and Neck Tumours. Lyon: IARC p. 234–5.
Lopez-Arcas JM, Cebrian L, Gonzalez J, Burgueno M (2007) Aneurysmal bone cyst of the mandible: case presentation and review of literature. Med Oral Patol Oral Cir Bucal 12:401–403
Jeyaraj P (2019) Management of central giant cell granulomas of the jaws: an unusual case report with critical appraisal of existing literature. Ann Maxillofac Surg. 9(1):37–47
Abdelkarim AZ, Abu El Sadat SM, Chmieliauskaite M, Syed AZ (2018) Radiographic diagnosis of a central giant cell granuloma using advanced imaging: cone beam computed tomography. Cureus 10(6):2735
Jadu FM, Pharoah MJ, Lee L, Baker GI, Allidina A (2011) Central giant cell granuloma of the mandibular condyle: a case report and review of the literature. Dentomaxillofac Radiol 40(1):60–64
Lange Jande, van den Akker Hans P, van den Berg Henk (2007) Central giant cell granuloma of the jaw: a review of the literature with emphasis on therapy options. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 104(5):603–615
Ramesh V (2020) Central giant cell granuloma - an update. J Oral Maxillofac Patho 24(3):413–415
Chuong R, Kaban L, Kozakewich H, Perez-Atayde A (1986) Central giant cell lesions of the jaws: a clinicopathologic study. J Oral Maxillofac Surg 44:708–713
Ficarra G, Kaban L, Hansen L (1987) Central giant cell lesions of the mandible and maxilla: a clinicopathologic and cytometric study. Oral Surg Oral Med Oral Pathol 64:44–49
Wang Y, Le A, El Demellawy D et al (2019) An aggressive central giant cell granuloma in a pediatric patient: case report and review of literature. J Otolaryngol Head Neck Surg 48:32
Kaban LB, Troulis MJ, Ebb D, August M, Hornicek FJ, Dodson TB (2002) Antiangiogenic therapy with interferon alpha for giant cell lesions of the jaws. J Oral Maxillofac Surg 60(10):1103–1111
Pogrel MA (2003) Calcitonin therapy for central giant cell granuloma. J Oral Maxillofac Surg 61(6):649–654
Bayrak NB et al (2018) Treatment of mandibular central giant cell granuloma with administration of systemic calcitonin: A case report. Selcuk Dent J 5:73–79
Tabrizi R, Fardisi S, Zamiri B, Amanpour S, Karagah T (2016) Can calcitonin nasal spray reduce the risk of recurrence of central giant cell granulomaof the jaws? A double-blind clinical trial. Int J Oral Maxillofac Surg 45:756–759
de Lange J, van den Akker HP, van VeldhuijzenZanten GO, Engelshove HA, van den Berg H, Klip H (2006) calcitonin therapy in central giant cell granuloma of the jaw: a randomized double-blind placebo-controlled study. Int J Oral Maxillofac Surg. 35(9):791–5
Funding
Nil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nath, P., Nath, T. Central Giant Cell Granuloma of the Jaw: A Case Report and Review of the Literature. J. Maxillofac. Oral Surg. (2022). https://doi.org/10.1007/s12663-022-01769-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12663-022-01769-4