Abstract
Purpose
Before implant surgery, a preoperative radiological evaluation is recommended for recognizing maxillary inflammatory conditions. In order to avoid a failure of the dental procedure and prevent medical–legal consequences, it is necessary to treat patients suffering of maxillary sinus pathologies. The classification proposed in our study aims to standardize the reference values for mucosal thickening and to verify their association with the odontogenic or disventilatory causes of sinus pathology.
Methods
The maximum mucosal thickness was measured at the level of the maxillary sinus floor: mucosal thickness was present when greater than 1 mm and was classified according to its extension within the sinus cavity.
Results
Imaging data of 270 adult patients were included, performed for dental diagnosis and treatment planning, and they were divided into four main classes: Class I (85 pt.), mucosal thickness lesser than 2 mm, not pathological. Class II A (52 pt.), mucosal thickness between 2 and 5 mm, localized to the maxillary sinus floor: it is still considered non-pathological, and a “wait-and-see” approach is recommended. Class II B (46 pt.), mucosal thickness greater than 5 mm but localized at sinus floor: pathological mucosa with odontogenic etiology, requiring dental treatment. Class III A (39 pt.), mucosa thicker than 5 mm and concentric, most likely due to sinus ventilation disfunction: it requires maxillary antrostomy. Class III B (30 pt.), sinonasal manifestations such as nasal polyposis, retention cysts, mucocele, dental foreign body: pathological mucosa to be treated with ESS. Class IV (12 pt.), oroantral fistula: nasal endoscopic or oral approach.
Conclusions
Our classification intends to suggest the better therapeutic option, in case of sinus pathology, according to the entity and pathogenesis of the mucosal thickening, in order to reduce complication and failure rate of dental surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to the literature, the incidence of maxillary sinusitis secondary to odontogenic diseases ranges from 8 to 29% of cases [1].
Until a few years ago, odontogenic asymptomatic maxillary sinusopathies were underestimated because of dental evaluation which was usually focused on the alveolar process of the maxillary bone [1].
In order to avoid a failure of the dental procedure and prevent medical–legal consequences, it is prior necessary to treat patients suffering from maxillary sinus pathologies; therefore, a preoperative radiological evaluation is recommended in order to recognize and treat maxillary inflammatory conditions before implant surgery [2].
Several classifications are present in the literature related to the conditions of the bone tissue of the alveolar process of the maxilla, while a careful evaluation of the state of the maxillary sinus mucosa, which is necessary since it plays a key role in inflammatory processes, is often neglected [3,4,5].
Paranasal sinuses are covered by a thin respiratory mucous membrane, adherent to the periosteum, which is normally about 1 mm thick; infectious or allergic noxae can cause inflammatory processes that may increase 10–15 times the thickness of the membrane, becoming visible radiographically [6]. A thickness of up to 2 mm is considered physiological; a thickness exceeding 5 mm is pathological, revealing a poor mucosal function, an impaired mucociliary transport, and it highly correlates with chronic sinusitis symptoms [7].
Moreover, a poor ventilation of the maxillary sinus caused by mucosal pathology of the middle meatus might compromise the success of dental treatment [8].
The aim of this study is to propose a classification focused on the state of the maxillary mucosa and on the possible treatment algorithm during the management of odontogenic diseases, in order to identify and treat patients with maxillary diseases, avoiding postoperative complications and failures.
Our classification, focused namely on the state of health of the maxillary sinuses mucosa, is proposed as a valuable and standardized system of interpretation of the radiological findings, which are also fundamental to complete the assessment of the patient’s sinonasal disease, in order to offer clinicians a helpful tool to be used during the diagnostic and therapeutic process.
Materials and Methods
This retrospective radiologic study included imaging data of 270 adult patients, collected from January 2017 to January 2018, performed for dental diagnosis and treatment planning. Computed tomography (CT) or cone-beam computed tomography (CBCT) scans belonging to adult patients who underwent radiologic pre-evaluation for dental assessment, implant placement, pre-orthodontic or pre-sinus lift procedures were included in our study, while the exclusion criteria regarded patients younger than 18 years old, those with any case of bone disease (drug-related bone changes, skeletal asymmetries, congenital or syndromic disorders) and patients who had already undergone sinonasal surgery.
Radiological evaluation was performed with thin-slice technique without contrast injection. Coronal and sagittal images were then reconstructed to better evaluate the sinonasal structures. Raw data were processed with both bone and soft-tissue algorithms to evaluate changes and alterations of the paranasal sinus mucosa. Localized or concentric mucosal thickenings, as well as any “dome-shaped” hypodense image, opacification or fluid presence within the maxillary sinus were selected. Informed consent was obtained from all participants included in the study.
The maximum mucosal thickness was measured on the maxillary sinus floor; the mucosa was considered thickened when higher than 1 mm, and it was therefore classified according to its extension within the sinus cavity as follows:
-
Localized, when restricted to the region involving up to two adjacent teeth and only the sinus floor;
-
Concentric and diffuse, when the thickening affected the other sinus walls.
The 270 patients were hence divided into four main classes (Table 1):
-
I CLASS Mucosal thickening on the maxillary sinus floor lesser than 2 mm. Sinus involvement is often unilateral. This type is considered not pathological, and no treatment is required. Therefore, there are no contraindications to possible sinus lift procedures or implant surgery.
-
II CLASS II A mucosal thickening between 2 and 5 mm, localized at the sinus floor. It is defined as “moderate,” and it is still considered para-physiological, justifying a “wait and see” approach, as reported by numerous previous studies that we recommend should last for at least 6 months after the last dental procedure. II B: mucosal thickness exceeding 5 mm and localized at maxillary sinus floor is considered pathological, and therefore requires the most appropriate dental treatment to reach the resolution of the radiological findings.
-
III CLASS The IIIA class includes patients with disventilatory sinus disease and specific imaging changes in maxillary sinus: opacification, increased concentric thickness of the maxillary mucosa with occlusion of the osteo-meatal complex, involvement of other paranasal sinuses. In these cases, the maxillary hyperplastic mucosa must be completely removed, and a large inferior meatal antrostomy should be created, in order to broaden the natural ostium in the middle meatus and thereby ensure adequate ventilation and drainage of the antral secretions.
Patients with concomitant sinonasal manifestations that impair sinus functions, such as nasal polyposis, retention cyst and pseudocyst, mucoceles and dental foreign bodies, belong to III B class. Those patients who are candidate to a maxillary sinus lift procedure or dental implant, the presence of a large cyst may first constitute an obstacle to the separation of the sinus floor from the maxillary bone walls and, moreover, it may cause the obstruction of the ostium, resulting in an impaired maxillary sinus drainage [9]. Therefore, these conditions are considered as contraindications for sinus lift and maxillary floor elevation procedures, given the high risk of surgical failure they correlate with [10]. In these cases, the most appropriate treatment consists in endonasal sinus surgery (ESS).
-
IV CLASS It includes cases of oroantral communication, which may occur during the extraction of posterior maxillary teeth, or cases of dental foreign bodies. In these cases, an endoscopic nasal approach or an oral one becomes the first surgical technique to choose.
Results
CT and CBCT images of 540 maxillary sinuses, belonging to 270 patients (142 female, 128 males; age range between 18 to 78 years old, mean 45.02 ± 2.82) were evaluated retrospectively. Patients were divided into four classes using our computed tomography (CT) scoring system.
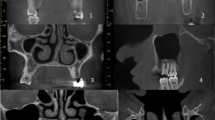
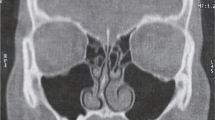
Among all the 270 patients examined, a mucosal thickening < 2 mm was recorded in 85 patients (31.48%) with a mean value of 0.9 ± 1.4 mm (I class) (Fig. 1); 63 of them (74.11%) showed unilateral involvement, while 22 (25.88%) had a bilateral involvement. One hundred and eighty-five patients (68.51%) are presented with sinus mucosal thickening major than 2 mm at various degrees. Mucosal thickening > 2 mm < 5 mm localized at maxillary sinus floor was reported in 58 patients (21.48%) with a mean thickness of 3.02 ± 4.5 mm, mostly unilaterally suggesting sinusitis of odontogenic origin (47 patients, 81.03% vs. 11 patients bilaterally, 18.96%) (IIA class) (Fig. 2). In 46 patients (17.03%), a mucosal thickening > 5 mm localized at maxillary sinus floor was found, with a mean value of 8.5 ± 3.6 mm (IIB class) (Fig. 3). Unilateral involvement is prevalent, with 32 patients (69.56%) versus 14 patients (30.43%) with bilateral involvement. Concentric mucosal thickening of maxillary sinus floor > 5 mm was identified in 39 patients (14.44%), with a mean value of 23.3 ± 8.6 mm (III A class) (Fig. 4). This condition occurred mostly bilaterally, involving 29 patients (74.35%) versus ten patients (25.64%) who showed unilateral involvement, suggesting a probable not odontogenic origin. Manifestations such as nasal polyps, retention cyst and pseudocyst, mucoceles, and dental foreign bodies (III B class) (Fig. 5) occurred in 30 patients (11.13%), predominantly unilaterally (28 patients 93.33%) with a mean value of 10.01 ± 2.7 mm. Foreign bodies of iatrogenic origin were found in five sinuses (16.66%), such as tooth roots and dental fillings, which resulted to be located in the sinus consequently to dentists’ actions. Lastly, only in 12 cases (4.44%), a condition of oroantral fistula was recorded and successfully treated with oral surgery (IV class) (Fig. 6), with a mean value of mucosal thickness of 18.23 ± 8.5 mm (Table 2).
Discussion
Chronic sinusitis is radiologically identified as a mucosal thickening of the paranasal sinuses. Several inflammatory conditions may cause mucosal reactive hyperplasia, compromising the physiological sinus drainage with mucus retention, decreasing mucociliary clearance, and predisposing to bacterial growth. Pathogens and their products easily spread from the oral cavity to the maxillary sinus, through the porous bone layer that separates these two cavities, or indirectly through blood and lymphatic stream [11].
Radiological evaluation is essential to identify the sinonasal alterations and the potential causes; computed tomography (CT) and cone-beam computed tomography (CBCT) represent the gold standard techniques. They in fact provide high-resolution images and allow simultaneous and accurate assessment of maxillary sinuses, teeth and adjacent tissues in all planes [12]. Therefore, they are indispensable, together with an accurate clinical evaluation, to produce a correct diagnosis, hence a better treatment planning, as they also allow to assess possible contraindications and risk factors to sinus floor surgery [13].
To date, a direct relationship between radiological changes of the maxillary bone and dental pathology has been ascertained: bone thickness plays a fundamental role in guaranteeing the stability and favorable prognosis of the dental procedure [14]. Different classifications have been formulated: in 1987, Misch [15] developed a classification based on the amount of “bone available,” identifying as adequate for implants a vertical bone of 12 mm, without any further manipulations. Wang et al. [16] developed a three-class system for implant success: class A represents abundant bone with > or = 10 mm bone height below the sinus floor, allowing proper implant placement. Class B indicates barely sufficient bone with 6 to 9 mm bone height below the sinus floor, and Class C indicates compromised bone with < or = 5 mm bone height below the sinus floor. In addition, Chiapasco et al. [17] introduced a pre-surgical classification regarding maxillary atrophy, and 4 mm value was used as a cut-off between different classes.
The current literature carefully studies the maxillary bone profile, but there are few classifications focused on the pre-surgical evaluation of the Schneiderian membrane’s thickness: Song et al. [18] proposed a classification considering a mucosal thickness < 2 mm as normal, 2–4 mm mild, 4–10 mm moderate, and > 10 mm severe.
Our classification aims to standardize the reference values for mucosal thickening and to identify an odontogenic or disventilatory cause of sinus pathology, through the evaluation of CT and CBCT scans. Mucosal thickening involving namely the maxillary sinus floor, often spreading toward the contiguous medial and lateral sinus walls, might be generated by several different causes. We focused our attention on odontogenic ones [19]. In these cases, a cooperation between different specialists is necessary to accurately identify this condition, in order to assure the most adequate treatment, before any dental surgery of the upper jaw [20]. On the other hand, the diffused and concentric thickening of the mucosa of the sinus walls, including the sinus roof, is usually a sign of a sinus ventilation disfunction [21]. In this case, endoscopic sinus surgery (ESS) restores a correct mucosal function, so that a safer and predictable dental surgery is then possible [22]. To date, Caldwell-Luc procedure is considered outdated, because of the increased morbidity and decreased efficacy compared to endoscopic sinus surgery. ESS, in fact, not only leads to a resolution of chronic sinusitis but also reduces the risk of postoperative failure of implant surgery or sinus lift procedures [23].
In conclusion, in case of increased Schneiderian membrane thickness, it is essential to recognize the cause of sinus disease through the interpretation of radiological images, anamnestic data and clinical evaluation, for a correct treatment planning.
The increased diagnostic accuracy of modern radiologic instruments (CT and CBCT), in fact, allows specialists to identify endonasal mucosal pathology, which was often neglected in the past. Moreover, it consents to select those patients who need proper treatment before undergoing dental implant surgery, through cooperation between Dentists, ENT specialists and Radiologists.
Our classification intends to suggest the better therapeutic option, in case of sinus pathology, according to the entity and pathogenesis of the mucosal thickening, in order to reduce complication and failure rate of dental implant procedures (Fig. 7).
References
Sheikhi M, Pozve NJ, Khorrami L (2014) Using cone beam computed tomography to detect the relationship between the periodontal bone loss and mucosal thickening of the maxillary sinus. Dent Res J (Isfahan) 11(4):495–501
Aksoy U, Orhan K (2019) Association between odontogenic conditions and maxillary sinus mucosal thickening: a retrospective CBCT study. Clin Oral Investig 23(1):123–131. https://doi.org/10.1007/s00784-018-2418-x
Niu L, Wang J, Yu H, Qiu L (2018) New classification of maxillary sinus contours and its relation to sinus floor elevation surgery. Clin Implant Dent Relat Res 20(4):493–500. https://doi.org/10.1111/cid.12606
Monje A, Diaz KT, Aranda L, Insua A, Garcia-Nogales A, Wang H-L (2016) Schneiderian membrane thickness and clinical implications for sinus augmentation: a systematic review and meta-regression analyses. J Periodontol 87(8):888–899. https://doi.org/10.1902/jop.2016.160041
Cakur B, Sümbüllü MA, Durna D (2013) Relationship among Schneiderian membrane, Underwood’s septa, and the maxillary sinus inferior border. Clin Implant Dent Relat Res. 15(1):83–87. https://doi.org/10.1111/j.1708-8208.2011.00336.x
Gracco A, Incerti Parenti S, Ioele C, Alessandri Bonetti G, Stellini E (2012) Prevalence of incidental maxillary sinus findings in Italian orthodontic patients: a retrospective cone-beam computed tomography study. Korean J Orthod. 42(6):329. https://doi.org/10.4041/kjod.2012.42.6.329
Carmeli G, Artzi Z, Kozlovsky A, Segev Y, Landsberg R (2011) Antral computerized tomography pre-operative evaluation: relationship between mucosal thickening and maxillary sinus function. Clin Oral Implants Res 22(1):78–82. https://doi.org/10.1111/j.1600-0501.2010.01986.x
Chiapasco M, Zaniboni M, Rimondini L (2008) Dental implants placed in grafted maxillary sinuses: a retrospective analysis of clinical outcome according to the initial clinical situation and a proposal of defect classification. Clin Oral Implants Res 19(4):416–428. https://doi.org/10.1111/j.1600-0501.2007.01489.x
Arslan İB, Uluyol S, Demirhan E, Kozcu SH, Pekçevik Y, Çukurova İ (2017) Paranasal sinus anatomic variations accompanying maxillary sinus retention cysts: a radiological analysis. Turkish Arch Otorhinolaryngol 55(4):162–165. https://doi.org/10.5152/tao.2017.2759
Giotakis EI, Weber RK (2013) Cysts of the maxillary sinus: a literature review. Int Forum Allergy Rhinol 3(9):766–771. https://doi.org/10.1002/alr.21177
Taschieri S, Torretta S, Corbella S et al (2017) Pathophysiology of sinusitis of odontogenic origin. J Investig Clin Dent 8(2):e12202. https://doi.org/10.1111/jicd.12202
Tian X, Qian L, Xin X, Wei B, Gong Y (2016) An analysis of the proximity of maxillary posterior teeth to the maxillary sinus using cone-beam computed tomography. J Endod 42(3):371–377. https://doi.org/10.1016/j.joen.2015.10.017
Martino F, Di Mauro R, Paciaroni K et al (2018) Pathogenesis of chronic rhinosinusitis in patients affected by β-thalassemia major and sickle cell anaemia post allogenic bone marrow transplant. Int J Pediatr Otorhinolaryngol 106:35–40. https://doi.org/10.1016/j.ijporl.2018.01.002
Nascimento EHL, Pontual MLA, Pontual AA, Freitas DQ, Perez DEC, Ramos-Perez FMM (2016) Association between odontogenic conditions and maxillary sinus disease: a study using cone-beam computed tomography. J Endod. 42(10):1509–1515. https://doi.org/10.1016/j.joen.2016.07.003
Misch CE (1989) Bone classification, training keys to implant success. Dent Today 8(4):39–44
Wang H-L, Katranji A (2008) ABC sinus augmentation classification. Int J Periodontics Restor Dent 28(4):383–389
Chiapasco M, Felisati G, Zaniboni M, Pipolo C, Borloni R, Lozza P (2013) The treatment of sinusitis following maxillary sinus grafting with the association of functional endoscopic sinus surgery (FESS) and an intra-oral approach. Clin Oral Implants Res 24(6):623–629. https://doi.org/10.1111/j.1600-0501.2012.02440.x
Ren S, Zhao H, Liu J, Wang Q, Pan Y (2015) Significance of maxillary sinus mucosal thickening in patients with periodontal disease. Int Dent J 65(6):303–310. https://doi.org/10.1111/idj.12186
Moskow BS (1992) A histomorphologic study of the effects of periodontal inflammation on the maxillary sinus mucosa. J Periodontol 63(8):674–681. https://doi.org/10.1902/jop.1992.63.8.674
Tavelli L, Borgonovo AE, Re D, Maiorana C (2017) Sinus presurgical evaluation: a literature review and a new classification proposal. Minerva Stomatol 66(3):115–131. https://doi.org/10.23736/S0026-4970.17.04027-4
Cipriani O, Vellone V, Arangio P, Della RF (2017) Sinus disventilation and atrophy of the upper maxilla: a combined surgical approach is possible? J Craniofac Surg 28(1):e1–e3. https://doi.org/10.1097/SCS.0000000000003151
Di Girolamo S, Pisani V, Di Girolamo M, Volpe S, Boghi F, Giacomini PG (2013) Atypical facial pain secondary to an unusual iatrogenic endonasal “contact point”. Pain Med. 14(1):167–168. https://doi.org/10.1111/j.1526-4637.2012.01512.x
Joe Jacob K, George S, Preethi S, Arunraj VS (2011) A comparative study between endoscopic middle meatal antrostomy and Caldwell-Luc surgery in the treatment of chronic maxillary sinusitis. Indian J Otolaryngol Head Neck Surg 63(3):214–219. https://doi.org/10.1007/s12070-011-0262-2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Founding Source
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di Girolamo, S., Martino, F., Guerrieri, M. et al. Odontogenic Maxillary Sinusopathies: a Radiological Classification. J. Maxillofac. Oral Surg. 21, 141–149 (2022). https://doi.org/10.1007/s12663-020-01329-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-020-01329-8