Abstract
Introduction
Since the advent of rigid fixation, there has been a paradigm shift in the management of condylar fractures from closed treatment options to open reduction and rigid internal fixation.
Materials and Method
Sixty-eight cases of condylar fractures reporting to Vydehi Institute of Dental Sciences, Bangalore, between 2009 and 2018 were reviewed in terms of age, sex, type of fracture, position of the mandibular third molar and the treatment rendered.
Results
The majority of the patients were males (60). There was an involvement of the right side in 34, left in 21 and bilateral involvement in 13 cases. Forty-three of the fractures were subcondylar, and 25 were intracapsular. Significantly in most cases, the mandibular third molar was either fully erupted (42) or missing (12). Sixty-one cases were subjected to surgical management including 49 cases of rigid internal fixation, and 12 of the intracapsular fractures had the condylar stump/segment removed. Only seven cases were not treated surgically. Most of the cases (44) were in the age group of 21–40, 12 were in the age group of 41–60, 9 were in the age group of 1–20, and 3 patients were above 60.
Conclusion
Condylar fractures more often do not require surgical intervention, and their incidence is more likely to occur when the third molar is either fully erupted or missing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 11–16% of all facial fractures and 30–40% of all mandibular fractures (MFs) are fractures of the mandibular condyle. Most are not caused by direct trauma, but follow indirect forces transmitted to the condyle from a blow elsewhere [1, 2].
There are two principal therapeutic modalities for these fractures: non-surgical (functional) and surgical. Historically, non-surgical treatment of MCFs by means of maxillomandibular fixation (MMF) followed by physiotherapy was the standard practice [3].
The proponents for non-surgical management of condylar fractures have given reasons like reduced overall morbidity, acceptable occlusal results in most cases, avoidance of any of typical surgical complications, a simpler procedure and less risk of ankylosis and avascular necrosis [4]. However, there are many instances of long-term complications like pain, arthritis, open bite, deviation of the mandible on opening and closing, inadequate restoration of vertical height of the ramus leading to malocclusion, and ankylosis with non-surgical treatment. The advent of rigid internal fixation and improved materials used along with the refinement of surgical techniques has led to a shift to open reduction and internal fixation (ORIF). The ORIF technique provides stable three-dimensional reconstruction, promotes primary bone healing, shortens the treatment time and eliminates the need for early release of the MMF. A decreased dependence on MMF improves post-treatment respiratory care, nutritional intake, and oral hygiene measures. Subcondylar fractures usually result in loss of ramal height and occlusal discrepancies. The usual treatment in these cases is open reduction and rigid internal fixation. However, intracapsular fractures involving the condylar head can occur with or without the loss of ramal height and treatment options can be confusing when the choice is put forward. This is because previous reports have also shown that the clinical outcomes are inconsistent, even when the same treatment is used for the same kind of intracapsular condylar fracture, which suggests that their prognosis may also depend on factors other than the site of the fracture line within the mandibular condyle.
The sagittal fracture variety in this group can occur in any position from medial to lateral part of the condylar head [5]. The position would define the change in height and dictate treatment options. The paper reviews the cases done during the 10-year period with an aim to analyse the result so as to arrive at a consensus on the correct treatment protocol to be followed based on the presenting clinical and radiological scenario.
Materials and Method
Records of 68 cases of condylar fractures that reported to the Department of Oral and Maxillofacial Surgery, Vydehi Institute of Dental Sciences, Bangalore, from 2009 to 2018 were reviewed and analysed. Informed consent was obtained from all individual participants included in the study as part of standard protocol.
The treatment of the condylar fractures was based on the presenting complaints, clinical findings and radiological evidence. All fractures that were asymptomatic without any altered occlusion were not subjected to surgical treatment. They were treated by soft diet alone or were given 2 weeks of IMF.
The patients were grouped into age brackets of 20 years each.
Sixty-one cases were subjected to surgical management in the form of rigid internal fixation or removal of the displaced condylar stump/fragment. The indications for surgical intervention of the cases were occlusal discrepancy, pain in the region during mandibular movements, restricted protrusive/laterotrusive movements and gross displacement of the segments. The results were analysed on parameters of function in terms of mandibular movement, pain and occlusion.
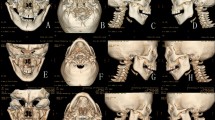
The surgical approach for subcondylar fractures with displaced, deviated or dislocated condyle segment (Fig. 1) was retromandibular, and fixation was done using two plates (Figs. 2, 3), one along the posterior border and one angulated below the sigmoid notch.
Intracapsular fractures that led to altered ramal height were taken up for open reduction and rigid internal fixation through a preauricular approach and fixed using single plate because of the restricted area for implant fixation. Intracapsular fractures with a sagittal variety that caused limited mandibular movements or caused pain but did not alter the ramal height (Fig. 4) were treated by surgical removal of the medially placed stump through a preauricular approach (Fig. 5).
The post-operative analysis was based on improvement in all pre-existing complaints and findings. The patients were followed up for a period of 3–6 months.
Results
In the 68 cases, 60 were males and 8 were females. The highest incidence (64.7%) was seen in the third and fourth decade of life accounting for 44 cases. Twelve cases were seen in the fifth and sixth decades (17.6%), 9 in the first two decades (13.2%) and 3 after the age of 60 (4.4%) (Fig. 6). The fractures involved the right side in 34 cases, 21 on the left side and 13 were bilaterally involved. Forty-three of the cases were subcondylar fractures, and 25 were intracapsular.
Seven out of the 68 fractures were not taken up for surgical intervention. They included 5 cases of subcondylar fractures which were treated conservatively using intermaxillary fixation for 2 weeks since they were undisplaced and there were no signs or symptoms necessitating surgical intervention. Two intracapsular fractures which were diacapitular in nature were not given any treatment since they were asymptomatic.
Forty-nine cases including 38 subcondylar fractures and 11 intracapsular fractures were treated by open reduction and rigid internal fixation. Twelve cases of intracapsular fractures had a medially displaced condylar segment that necessitated its removal due to limited mandibular movement and pain on manipulating the mandible for normal actions of eating or speaking.
A significant finding was the radiographic picture revealing an overwhelming number of cases having either fully erupted (42) or missing (12) third molars totalling 64 (79.4%) on the involved side (Fig. 7).
In reviewing the results of the cases treated, all cases treated non-surgically healed well without any major problem except the initial period of limited mouth opening for a period of 1–2 weeks. The average mouth opening in the cases was 20 mm, and the same improved to 30 mm in the immediate phase after open reduction and rigid internal fixation. In cases where only the stump was removed, the average post-operative mouth opening was 35 mm. There was complete absence of pain after 3 months in all the treated cases. There was no incidence of mandibular deviation in the post-operative period after 3 months. All post-operative radiographs showed an adequate reduction in the segments in open reduction and rigid fixation cases. Of the 49 cases treated by open reduction and rigid internal fixation, there was 1 case of plate fracture necessitating a second intervention in the subcondylar fracture. Function in the form of restored occlusion, mandibular movements and adequate mouth opening was achieved in all cases. In the 12 cases where the medially fractured condylar stump was removed, there was relief from pain and improved mandibular movements in all cases. Temporary facial nerve involvement of the temporal branch was seen in 12 cases and that of the marginal mandibular nerve in 10 cases which resolved in a couple of weeks time.
Out of the 68 cases, 53 cases were followed up for 3 months and another 9 for 6 months. The other 6 did not report back after the initial hospitalization period.
Discussion
There has been a considerable controversy regarding the treatment of condylar fractures, whether they should be treated conservatively or surgically. Both surgical (open) and functional (non-surgical, closed) treatment options are available to clinicians, and the choice of the best treatment requires careful consideration of the kind of fracture. The treatment aims at pain reduction, re-establishment of occlusal contacts and posterior facial heights with symmetrical gonial angles, and functional restoration of the temporomandibular joints, mouth opening greater than 40 mm, minimal lateral deviation at maximum MO and unrestricted lateral and protrusive movements.
Contemporary literature has shown good results with surgical intervention and rigid internal fixation [6]. The argument in favour of open reduction is that it allows good anatomical repositioning and immediate function. The potential advantages of an open treatment are restoration of correct anatomical position and a shorter duration of MMF, which would lead to immediate mobilization and more efficient functioning of the joint [7].
It is a known fact that ORIF of condylar fractures is technically difficult due to the difficulty in manipulating the fragments in a small area, the resultant visible external scar, increased costs and hospitalization time and the risk of facial nerve injury [8].
Although most patients are satisfied with the results of closed treatment, the development of images (CT) scans and magnetic resonance imaging helps surgeons detect condylar deformities that may affect the temporomandibular joint (TMJ) function [8, 9].
However, there is no consensus regarding the choice of the best type of osteosynthesis [10]. From data in the literature, it is evident that the technique used most frequently is the positioning of a single plate, despite complications concerning plate fracture or screw loosening having been reported by various authors [11].
The philosophy behind using two plates in fixation of condylar fractures stems from the work of Throckmorton [12] who identified the presence of tensile strains occurring on the anterior and lateral surfaces of the condylar process and of compressive strains on the posterior surface. But it was Meyer [13] in 2002 who for the first time developed a masticatory load device, capable of reproducing with accuracy the forces applied on the mandible during mastication. He highlighted and confirmed, through a photoelastic analysis, the presence of compressive strains running along the posterior border of the ramus and tensile strains positioned parallel to and below the sigmoid notch.
Choi et al. [14] comparing the biomechanical stability of four different plating techniques used to fix condylar neck fractures when submitted to a functional load demonstrated that a double miniplate was more stable than a single plate.
Therefore, all these studies suggest that new concepts need to be considered in the positioning of osteosynthesis plates along the tensile strains lines. The tensile strains lines are mainly responsible for the complications concerning plate fracture or screw loosening that lead to the displacement of the reduced condylar fragment with the consequent presence of a gap in the fracture line [15]. First plate helps to obtain “intermediary stability”, so permitting the restoration of the height of the ramus. But this same plate is not capable of resisting the biomechanical strains that occur in the condylar region during mastication, and more precisely the sagittal tension correlated with the tensile strain lines that lead to the displacement of the condylar fragment with the consequent appearance of the gap. This is the reason why it is necessary to position a second plate in an oblique direction along the tensile strain lines that run below and parallel to the sigmoid notch, in agreement with Champy’s concept of stable osteosynthesis functionality.
Complications related open reduction is a deterrent to most surgeons in considering this treatment option. The most serious complication is probably damage to the facial nerve. Fortunately, this is transient in most cases, with a reported incidence of between 12 and 48% when the most commonly used incision (the retromandibular transparotid approach) is used [16]. In the studies included in this review, the incidence of temporary weakness was higher with transparotid dissection than with non-transparotid dissection.
Other complications that have been listed include scarring and development of sialocele in addition to wound infections. The infection rate was quite variable among the studies, most presumably due to differences in surgical and antibiotic protocols.
There has been a matter of inconsistency in planning management of intracapsular fractures. On the basis of axial and coronal CT scans, Dongmei et al. have divided the condylar head into three portions: lateral third, central third and medial third [17], and then classified the fracture into four types according to the location of the fracture line: type A, a fracture through the lateral third portion of the condylar head with the reduction in the ramus height; type B, a fracture through the central third portion of the condylar head without the reduction in the ramus height; type C, a fracture through the medial third portion of the condylar head without the reduction in the ramus height; and type M, a fracture that has multiple fragments of the condylar head. The treatment principles according to the different fracture types based on the classification are as follows: for type A fractures, ORIF is used in most cases, especially bilateral cases, because it reduces the ramus height. The fragment is relatively large enough for ORIF. For type B fractures, closed treatment is used in most cases. It is difficult to perform ORIF, because the fragment is small and deep. For type C fractures, closed treatment or removal of the fragment with disc reduction should be performed. For type M fractures, closed treatment or reduction in the large segment with fixation, which is usually very difficult, should be performed. All 12 cases in our series of intracapsular fractures that necessitated removal were type C or M.
The classification described by Neff et al. [18] based on the site of the fracture line and the reduction in mandibular height is also very popular. Ying et al. [5] have recommended a new classification with special stress on the disc position for intracapsular fractures. According to them, without restoration of the position of the disc, the anatomical reduction in the condyle alone cannot ensure full recovery of the functions of the TMJ. Anatomical reduction in the disc is known to be beneficial for the TMJ and decreases the complications of open surgery, which suggests that it is important to restore the disc to its proper position, and the disc and the condyle must be managed as a whole unit.
Another significant finding in this study was the relation of the mandibular third molar with respect to condylar fractures. 79.4% of the condylar fractures in our study had either fully erupted or missing third molars. The study by Rajshekar et al. [19] revealed that the highest incidence of condyle fracture was noticed typically in the absence of impacted third molars (either partial or complete).
Some authors have postulated that the presence of impacted third molars (either partial or complete) reduces the incidence of condyle fractures [20].
When the unerupted third molar is absent, most of the force is conveyed to the condylar region leading to its fractures. It has also been suggested that removal of unerupted third molars makes the mandible more vulnerable to condyle fractures.
Conclusion
This 10-year retrospective study on the incidence of condylar fractures showed a very high incidence in the third and fourth decades. Most of the fractures were subcondylar, and the clinical features and functional limitations of the patients usually warrant open reduction and rigid internal fixation with at least two plates. The dilemma of whether to treat conservatively or open the area is more evident in intracapsular fractures where pain and limited excursions are the only main indications to open the TMJ and either fix the fracture or remove the offending segment. There is also a definite relation between the eruptive status of the mandibular third molar and condylar fractures with most condylar fractures in mandibles that had either fully erupted or missing third molars.
References
Chrcanovic BR (2012) Factors influencing the incidence of maxillofacial fractures. Oral Maxillofac Surg 16:3–17
Chrcanovic BR, Abreu MH, Freire-Maia B, Souza LN (2012) 1454 mandibular fractures: a 3- year study in a hospital in Belo Horizonte, Brazil. J Craniomaxillofac Surg 40:116–123
Chrcanovic BR (2012) Open versus closed reduction: mandibular condylar fractures in children. Oral Maxillofac Surg 16:245–255
Posnick JC, Wells M, Pron GE (1993) Pediatric facial fractures: evolving patterns of treatment. J Oral Maxillofac Surg 51:836–844 (discussion 844–5)
Ying BB, Zhang QQ, Zhu SS, Li YF (2018) Outcomes of treatment for intracapsular fractures of the mandibular condyle: recommendation for a new classification. Br J Oral Maxillofac Surg 56:139–143
Ellis E III, Throckmorton GS, Palmieri C (2000) Open treatment of condylar process fractures: assessment of adequacy of repositioning and maintenance of stability. J Oral Maxillofac Surg 58:27–34 (discussion 35)
Rozeboom L, Dubois R, Bos R, de Spijker J (2017) Lange: open treatment of unilateral mandibular condyle fractures in adults: a systematic review. Int J Oral Maxillofac Surg 46:1257–1266
Sforza Chiarella, Ugolini Alessandro, Sozzi Davide, Galante Domenico, Mapelli Andrea, Bozzetti Alberto (2011) Three-dimensional mandibular motion after closed and open reduction of unilateral mandibular condylar process fractures. J Craniomaxillofac Surg 39:249–255
Hlawitschka M, Loukota R, Echelt U (2005) Functional and radiological results of open and closed treatment of intracapsular (diacapitular) condylar fractures of the mandible. Int J Oral Maxillofac Surg 34:597
Tominaga K, Habu M, Khanal A, Mimori Y, Yoshioka I, Fukuda J (2006) Biomechanical evaluation of different types of rigid internal fixation techniques for subcondylar fractures. J Oral Maxillofac Surg 64:1510–1516
Ellis E III, Dean J (1993) Rigid fixation of mandibular condyle fractures. Oral Surg Oral Med Oral Pathol 76:6–15
Throckmorton GS, Dechow PC (1994) In vitro strain measurements in the condylar process of the human mandible. Arch Oral Biol 39:853–867
Meyer C, Kahn JL, Boutemi P, Wilk A (2002) Photoelastic analysis of bone deformation in the region of the mandibular condyle during mastication. J Craniomaxillofac Surg 30:160–169
Choi BH, Kim KN, Kim HJ, Kim MK (1999) Evaluation of condylar neck fracture plating techniques. J Craniomaxillofac Surg 27:109–112
Parascandolo Salvatore, Spinzia Alessia, Parascandolo Stefano, Piombino Pasquale, Califano Luigi (2010) Two load sharing plates fixation in mandibular condylar fractures: biomechanical basis. J Craniomaxillofac Surg 38(385):390
Rozeboom AVJ, Dubois L, Bos RRM, Spijker R, de Lange J (2018) Open treatment of condylar fractures via extraoral approaches: a review of complications. J Cranio-Maxillo-Fac Surg 46:1232–1240
He Dongmei, Yang Chi, Chen Minjie, Jiang Bin, Wang Baoli (2009) Intracapsular condylar fracture of the mandible: our classification and open treatment experience. J Oral Maxillofac Surg 67:1672–1679
Neff A, Kolk A, Deppe H et al (1999) New aspects for indications of surgical management of intra-articular and high temporomandibular dislocation fractures. Mund Kiefer Gesichtschir 3:24–29
Gaddipati R, Ramisetty S, Vura N, Kanduri RR, Gunda VK (2014) Impacted mandibular third molars and their influence on mandibular angle and condyle fractures: A retrospective study. J Cranio-Maxillo-Fac Surg 42:1102–1105
Zhu SJ, Choi BH, Kim HJ, Park WS, Huh JY, Jung JH et al (2005) Relationship between the presence of unerupted mandibular third molars and fractures of the mandibular condyle. Int J Oral Maxillofac Surg 34:382–385
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this retrospective study involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Menon, S., Kumar, V., Archana, S. et al. A Retrospective Study of Condylar Fracture Management in a Tertiary Care Hospital—A 10-Year Experience. J. Maxillofac. Oral Surg. 19, 380–386 (2020). https://doi.org/10.1007/s12663-019-01257-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-019-01257-2