Abstract
Objective
The aim of study was to determine the association between signs of temporomandibular disorders (TMD), occlusal support, and alterations in the craniofacial structure of elderly Vietnamese by using cephalometric analysis.
Methods
The cross-sectional study consisted of 244 participants aged 65–74 years. Participants were examined for signs of TMD, including limited mouth opening, temporomandibular joint (TMJ) crepitus, TMJ tenderness, and muscle tenderness. Dentition was divided into four occlusal support zones based on occluding pairs of posterior teeth by using Eichner’s classification: Class A = 4 support zones; Class B = 1–3 support zones or only contact in anterior teeth; Class C = 0 support zones. Fifteen angular and seven linear parameters were used for sagittal craniofacial skeleton analysis.
Results
10.3% of participants had limited mouth opening, 49.6% TMJ crepitus, 16.3% TMJ tenderness, and 24.2% muscle tenderness; 45.5% had Class A occlusal support, 38.5% Class B, and 16.0% Class C. Those with Class C had significantly smaller ramus inclination, articular angle, and angles formed by the mandibular plane and shorter facial height compared to Class A and Class B (P < .001). TMD signs were significantly associated with: angles formed by mandibular plane, gonial angle, cranial base angle, effective mandibular length, and anterior facial height (P < .05).
Conclusions
The alteration of craniofacial structures was significantly associated with TMD signs among elderly Vietnamese. The higher number of lost occlusal support zones, the more significant the changes to craniofacial structures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Temporomandibular disorders (TMD) are a major concern regarding the oral health of elderly people. Signs of TMD occur in 40% of elderly people worldwide and increase with age. Most signs co-occur with TMD are temporomandibular joint sounds at levels ranging from 28 to 38% [1, 2]. Masticatory muscle tenderness has been observed in 14% of elderly people and is considered to cause of impaired masticatory performance [3], and a limited mouth opening occurs more often among the elderly than any other age group [2].
Elderly people often have occlusal problems owing to a progressive loss of teeth, and they have to adapt new functional mastication, which can lead to a change in the movement trajectory of the temporomandibular joint (TMJ). Missing teeth can reduce the vertical dimension of occlusion, cause imbalanced occlusion, and influence neuromuscular adaption, as well as increase the likelihood of TMD [4]. Hiltunen et al. [5] found an association between inadequate occlusal support and TMD.
Facial harmony affects esthetics, functionality, and social communication. Cephalometry has a significant role in the analysis of alterations to craniofacial structures. A decreased vertical dimension of occlusion can result in alteration of the anterior facial height [6]. Many studies have used cephalometry to examine changes to the mandibular structures of edentulous people [7,8,9,10]. Progressive tooth loss results in a larger gonial angle and a smaller ramus of the mandible [8, 9].
Other investigations have used magnetic resonance imaging (MRI) and cone beam computerized tomography (CBCT) to observe changes to the structures of the temporomandibular joint; however, the high exposure to radioactivity and cost of these methods are disadvantages of these methods compared to cephalography. Cephalography has been recognized as a supporting tool for craniofacial morphology analysis of TMD patients [11,12,13,14,15,16]. Emshoff et al. [13] found accordance between cephalometric and MRI analysis of TMJ structural characteristics. In addition, cephalometric findings significantly associated with TMD; Matsuo et al. [15] showed that the ratio between the condyle and ramus heights was lower among subjects with TMJ crepitus. Chen et al. [12] demonstrated that a degenerative TMJ joint results in a decreased posterior facial height, while Ahn et al. [11] suggested that several cephalometric parameters could be used as an auxiliary diagnostic tool for identifying patients with TMJ internal derangement. Anterior open-bite and Class II malocclusion based on cephalometric measurements are considered risk factors for TMD [17].
Facial skeletal characteristics differ between ethnic groups, and the cephalometric characteristics of a Vietnamese sample had not been studied yet. In addition, the number of occlusal supports affects the stability and balance of occlusion, which is known as the key to preventing TMD, but this has not been investigated using cephalometric analysis, including among elderly people, who often have missing teeth. Last, significant associations between TMD signs and craniofacial structures have been insufficiently reported based on the cephalometric analysis.
Therefore, the aim of this study was to determine the association between signs of temporomandibular disorders, occlusal support and alteration in the craniofacial structure of elderly Vietnamese based on cephalometric measurements.
Materials and Methods
Study Sample Size
This cross-sectional study involved examining the oral health, temporomandibular disorder status, and occlusion of elderly people aged 65–74 years living in Danang City, Vietnam. The sample size was calculated at a 90% confidence level; hypothesizing the prevalence of TMD in elderly Vietnamese is 50%; this gave an acceptable margin of error of 5%. The total sample equaled 300 participants. The selection criteria for participation were absence of physical and mental disabilities, and no history of TMJ trauma or orthodontic or facial surgery.
A multistage stratified random sampling method was used to select participants based on their demographic characteristics. One rural district and three urban districts were randomly taken from eight districts of Danang city for the current study. Lists of elderly citizens were obtained from the Community Unions for Older Adults, into which all those aged 65–74 years are incorporated. Finally, participants from each of selected urban district (50 subjects) and rural (150 subjects) were randomly sampled and stratified according to gender. The sample selection is shown in Fig. 1.
Written informed consent that explained detailed study procedures including clinical examination and cephalography was obtained from all participants. This study was approved by the Human Research Ethics Committee of Danang University of Medical Technology and Pharmacy (No. 523/CN-DHKTYDDN) and performed in accordance with the World Medical Association’s Helsinki Declaration.
Signs of TMD
Signs of TMD were based on clinical examination using the Diagnosis Criteria for Temporomandibular disorders (DC/TMD) Axis I [18]. TMD signs consisted of: limited mouth opening (maximum assisted mouth opening <40 mm); deviation of mouth-opening pattern; TMJ clicking and/or crepitus sounds during mandibular movement; TMJ tenderness; muscle tenderness.
The first author who was trained by professional expert for diagnosis of TMD conducted all clinical temporomandibular examinations. A pilot study of a group of 25 elderly people was performed to calibrate the examiner, and ten percent of the total sample were re-examined after 3 days to test the reliability of the examination. The calculated Kappa values were above 0.85, indicating a high degree of intra-examiner and inter-examination reliability.
Occlusal Support
An alginate impression was taken for fabrication of a diagnostic cast, and the participant’s centric occlusion was recorded using a wax bite. After a dental cast has been scanned, occlusion was analyzed using Ortho Analyzer™ software (3Shape A/S, Copenhagen, Denmark).
Occlusal support was analyzed using Eichner’s classification [19], which divides the posterior teeth into four zones based on the existence of occluding pairs of posterior teeth. Class A equates to contact at all four support zones; Class B lacks at least one support zone, or the loss of all four supporting zones but intact anterior region; Class C has no contact of any coupled teeth. The number of occlusal support zones is shown in Fig. 2. In cases where a participant had fixed crowns or bridge prosthesis, these were also considered as remaining teeth; however, a removable prosthesis, a stump or broken tooth were registered as missing teeth.
Cephalometric Analysis
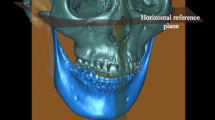
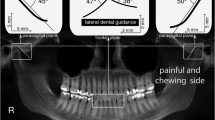
The cephalometric images were recorded using a digital CRANEX D Digital X-ray unit (73 kV, 10 mA, 17.6 s, CC-detector sensor; Soredex, Tuusula, Finland). The first author measured all images using the NemoCeph 2D software (Nemotec, Madrid, Spain). Hard tissue points were used as landmarks during cephalometric analysis, with the reference planes consisting of the Frankfort, mandibular, and cranial base planes (Table 1). Seven linear and fifteen angular parameters were used for sagittal skeletal analysis. All parameters are shown in Figs. 3 and 4.
Angular parameters used in the cephalometric analysis: (1) N–S–Ar, (2) N–A to the Frankfort plane, (3) SNA, (4) SNB, (5) SNPog, (6) N–Pog to FH, (7) ANB, (8) Ans–Pns to the mandibular plane, (9) mandibular plane to S–N, (10) mandibular plane to the Frankfort plane, (11) S–Ar–Go, (12) Ar–Go–Me, (13) N–Go–Me, (14) N–Go–Me, (15) Ar–Go to N–S
The cephalometric images of 25 randomly selected participants were measured again after 30 days to evaluate the level of observational error of the examiner. The Dahlberg’s formula was used to assess method errors. Of the 15 angular parameters, the errors ranged from 0.2° (of ANB angle) to 1.5° (of S–Ar–Go angle); of the 7 linear parameters, errors ranged from 0.4 mm (of N–Me) to 0.8 mm (of Co–Gn).
Statistical Analysis
Data entry and statistical analysis were performed using SPSS Statistics for Windows, Version 17.0 (SPSS Inc., Chicago, Illinois, USA). The Student’s t test was used to determine significant variations of cephalometric parameters related to TMD signs. The Bonferroni test was used to compare cephalometric parameters between the Eichner classes. The confidence level of 95% and a two-sided P value of < 0.05 were used to reveal significant differences.
Results
Of the 300 elderly aged 65–74 years, 56 subjects failed to participate in the study, the final sample consisted of 122 females and 122 males. Of the final sample, 10.3% had limited mouth opening (< 40 mm), 49.6% TMJ crepitus, 16.3% TMJ tenderness, and 24.2% muscle tenderness. Regarding Eichner’s classification, 45.5% of the sample were Class A, 38.5% Class B, and 16.0% Class C (Table 2).
Table 3 shows the angular and linear skeletal differences between the three Eichner classes. Multiple comparisons using Bonferroni test also indicated that Class C had SNB angle, S–N–Pog angle, and the angle formed by N–Pog to the Frankfort plane statistically larger compared to those of Class A and Class B (P < .001). No other parameter was significantly different among the three classes (P > .05): saddle angle (N–S–Ar), SNA, angle gonial angle (Ar–Go–Me), ramus height (Ar–Go), mandibular body length (Go–Me), and effective mandibular length (Co–Gn). However, the lower gonial angle (N–Go–Me), articular angle (S–Ar–Go), mandibular plane to S–N, and mandibular plane to Frankfort plane of both Class A and Class B were statistically larger than those of Class C (P < .001).
Of the linear parameters, anterior facial height (N–Me) and lower anterior facial height (Ans–Me) were statistically different between the three classes (P < .001). Posterior facial height (S–Go) of Class C was significantly shorter than those of Class A or Class B (P < .001). Facial height ratio (S–Go/N–Me) and lower anterior facial height ratio (Ans–Me/N–Me) of Class C were statistically different compared to Class A and Class B (P = .014 and P < .001, respectively).
Table 4 shows the correlations between cephalometry values and TMD signs. Limited mouth opening was significantly associated with a small angle formed by N–Pog to the Frankfort plane (P = .020), and large ANB angle (P = .035). TMJ crepitus significantly associated with large angles of: S–N–Pog (P = .039), ANB (P = .001), the angle formed by N–Pog to the Frankfort plane (P = .036), and the upper gonial angle (Ar–Go–N, P = .023).
TMJ tenderness was found statistically associated with a short effective mandibular length (Co–Gn, P = .014), a short anterior facial height (N–Me, P = .003), small angles between: mandibular plane and palatal plane (P = .009), mandibular plane and S–N (P = .048), and mandibular plane the Frankfort plane (P = .017). Participants with muscle tenderness had a large upper gonial angle (Ar–Go–N, P = .024) but small lower gonial angle (N–Go–Me, P = .025). Lower anterior facial ratio (Ans–Me/N–Me) was significantly associated with a limited mouth opening (P = .042), TMJ crepitus (P = .027), and TMJ tenderness (P = .002).
Discussion
The main findings of the current study indicate that craniofacial structure alterations among elderly Vietnamese are related to reduced occlusal support and TMD signs. Participants without any occlusal support had a significantly different mandibular protrusion; they had larger S–N–Pog angle, and larger angle formed by N–Pog line and the Frankfort plane than those having occlusal support. Owing to the lack of any occlusal support zone, the mandible has to adapt to a new functional position for masticatory performance. Merrot et al. [9] performed a comparison of the changes to the mandible between dentate and edentate subjects and found a reduced symphysis height among the edentate group, which could possibly lead to a change to the protrusive position of the Pogonion point.
The results of the current study seem to confirm that edentulous subjects had substantial morphological changes of craniofacial structure, especially in the mandible, between Class A, Class B, and Class C. Participants with Class C had significantly decreased ramus inclination (Ar–Go to N–S) and larger upper gonial angle (Ar–Go–N) compared to those of Class A and Class B. This suggests that the mandibular ramus rotates in an anti-clockwise direction. Moreover, accompanied by decreased occlusal vertical dimension, Class C participants had significantly smaller angles formed by the mandibular plane with the cranial base, palatal, and Frankfort planes. These findings are consistent with the findings of other cephalometry investigations among elderly populations [7, 8].
Our study demonstrated that the gonial angle (Ar–Go–Me) of Class C did not differ as compared to Class A and Class B; however, Class C participants had significantly larger upper gonial angle than those of Class A and Class B. It could be explained by the fact that missing posterior teeth caused mandibular bone resorption, especially in mandibular angle; therefore, the gonial tends to rapidly increase after tooth extraction. Our finding is in accordance with the study by Okşayan et al. [20], but contrasts with other studies that reported edentulous subjects having a gonial angle larger than dentate ones [8,9,10]. This was probably due to the Class C participants in our study having several natural teeth or stumps that had not been extracted.
In a comparison of all cephalometric parameters between participants with occlusal support (Class A or Class B) and those without (Class C), we found significant differences in linear distances in term of lower anterior facial height (Ans–Me). The average of the lower anterior facial height of Class C elderly was 54.8 mm, while those of Class A and Class B were 65.7 and 62.7 mm, respectively. No occlusal support seems to cause loss of vertical dimension of occlusion and resulted in a shorter vertical facial height. Rosa et al. [21] found that the average of the lower anterior facial height of edentulous and dentate Brazilians was 62.7 and 72.7 mm, respectively. A study conducted in Japan found that facial height does not change significantly if the elderly person has enough occluding pairs of teeth [22]. No occlusal support also reduces posterior facial height in the current study mainly because of the decreased lower facial height. Being edentulous might result in significantly shorter mandibular symphysis height, ramus height, and mandibular length, and deeper mandibular notch [9, 10, 21].
Cephalometric parameters can also vary within ethnic groups. The average anterior facial height of elderly Vietnamese (N–Me, 116.3 mm) in the current study is shorter than those of elderly Japanese (123.9 mm) and Brazilians (126.0 mm) [21, 22]. Our elderly Vietnamese participants also had a shorter total mandibular length (Co–Gn, 107.6 mm) compared to elderly Caucasians in France (112.6 mm), Finland (128.7 mm), and Brazil (124.2 mm) [7, 9, 21]. In addition, the short ramus height (Ar–Go) and small gonial angle in the elderly of our sample are typical anthropological characteristics of Vietnamese people.
Craniofacial structure changes may cause TMD signs. In the current study, those elderly who suffered from TMJ tenderness had a significantly shorter anterior face heights (N–Me and Ans–Me), and smaller mandibular plane angles compared to non-sufferers. TMJ tenderness has been significantly associated with loss of posterior occlusal support [23]; therefore, persons with TMJ tenderness are at risk of losing the vertical dimension of occlusion, which can result in a shorter anterior face and alterations to the angles formed by the mandibular plane related to the maxillary plane and cranial base plane.
In our sample, those with TMJ tenderness had shorter total mandibular length, which could be explained by the fact that TMJ tenderness may result in ankylosis and inhibit mandibular movement in a clockwise direction. This finding is reinforced by the studies of Ahn et al. [11] and Matsumoto et al. [14] who wrote that TMD patients had a relatively shorter mandibular and progressive mandibular retrusion.
In the current study, participants with TMJ crepitus had a significantly different Pogonion position. Those elderly also had a larger upper gonial, S–N–Pog angle, and angle formed by N–Pog to the Frankfort plane, but presented a smaller ANB angle, and reduced the lower facial height ratio, compared to the participants without TMJ crepitus. It is possible that there is the growth of the protrusion and anti-clockwise rotation of the mandible, leading to the Pogonion point moving upward and forward. Our finding contrasts with the study by Matsuo et al. [15] where TMJ crepitus was significantly associated with retrusion of the mandible; this could be due to Matsyuo’s sample only including participants with Angle Class II malocclusion. Moreover, crepitus often indicates TMJ arthritis and is associated with edentulousness and advancing age [24]. Wiese et al. [25] concluded that crepitus is often accompanied by osseous changes of the TMJ, such as flattening, erosion, osteophytes, and sclerosis. Therefore, the alteration in the craniofacial structure could lead to crepitus.
Muscle tenderness was found to significantly associate with a small lower gonial mandible (N–Go–Me) in the current study. The temporalis and masseter muscles are powerful masticatory muscles, and when muscle tenderness occurs, mandible could be retracted upward that caused alteration to the gonial mandible and consequently shorter anterior facial height.
The elderly participants with a limited mouth opening had significantly larger ANB angle and smaller angle formed by N–Pog and the Frankfort plane compared to those with a mouth opening of ≥ 40 mm. These characteristics might be explained by limited mouth opening resulting in mandibular retrusion. Limited mouth opening can be associated with myofascial pain; therefore, the mandible of such subjects has to be retruded to adapt the function of movement.
In addition, mouth-opening limitation is also a sign of osteoarthritis that related to the osseous changes of the TMJ condyle such as erosion and fattening. Several studies have demonstrated that TMJ osteoarthritis was observed more often among TMD patients with a facial skeletal pattern of Class II malocclusion [26], and such patients often had a smaller SNB, larger ANB, and shorter ramus height [27]. Therefore, participants with limited mouth opening in our study might have osseous changes of the condyle that caused change position of the mandible.
In summary, the results showed that craniofacial structures had significant differences between Class A (4 occlusal support zones), Class B (1–3 occlusal support zones), and Class C (no occlusal support zone) participants such as: an increased upper gonial angle and S–N–Pog angle; a decreased ramus inclination and shorter anterior facial height. The TMD signs of limited mouth opening, TMJ tenderness, TMJ crepitus, and muscle tenderness were found to significantly associate with alteration in the craniofacial structures.
The current study has several limitations. We compared craniofacial structure changes of different types of occlusal support according to Eichner classification; however, we did not perform a follow-up study to observe changes of structures on the same person who lost occlusal support from Class A to Class C. Lateral cephalogram is often used to measure craniofacial structures based on two dimensional radiographic image, but not for detailed analysis of minor osseous changes of temporomandibular joint structure. A cone beam computed tomography or magnetic resonance imaging should be used for more accurate analysis of TMJ; however, medical center of current study had not been equipped with those radiographic devices yet.
Conclusion
Among elderly Vietnamese, the alteration of craniofacial structures was significantly associated with TMD signs. The higher number of lost occlusal support zones, the more significant the changes to elderly’s craniofacial structure.
References
Ikebe K, Hazeyama T, Iwase K, Sajima H, Gonda T, Maeda Y et al (2008) Association of symptomless TMJ sounds with occlusal force and masticatory performance in older adults. J Oral Rehabil 35:317–323
Schmitter M, Rammelsberg P, Hassel A (2005) The prevalence of signs and symptoms of temporomandibular disorders in very old subjects. J Oral Rehabil 32:467–473
Gesch D, Bernhardt O, Alte D, Schwahn C, Kocher T, John U et al (1985) Prevalence of signs and symptoms of temporomandibular disorders in an urban and rural German population: results of a population-based Study of Health in Pomerania. Quintessence Int Berl Ger 2004(35):143–150
Moreno-Hay I, Okeson JP (2015) Does altering the occlusal vertical dimension produce temporomandibular disorders? A literature review. J Oral Rehabil 42:875–882
Hiltunen K, Vehkalahti M, Ainamo A (1997) Occlusal imbalance and temporomandibular disorders in the elderly. Acta Odontol Scand 55:137–141
Tavano KTA, Seraidarian PI, de Oliveira DD, Jansen WC (2012) Determination of vertical dimension of occlusion in dentate patients by cephalometric analysis–pilot study. Gerodontology 29:e297–e305
Brzoza D, Barrera N, Contasti G, Hernández A (2005) Predicting vertical dimension with cephalograms, for edentulous patients. Gerodontology 22:98–103
Huumonen S, Sipilä K, Haikola B, Tapio M, Söderholm A-L, Remes-Lyly T et al (2010) Influence of edentulousness on gonial angle, ramus and condylar height. J Oral Rehabil 37:34–38
Merrot O, Vacher C, Merrot S, Godlewski G, Frigard B, Goudot P (2005) Changes in the edentate mandible in the elderly. Surg Radiol Anat SRA 27:265–270
Uma M, Shetty R, Shenoy KK (2013) Cephalometric: evaluation of influence of edentulousness on mandibular morphology: a comparative study. J Indian Prosthodont Soc 13:269–273
Ahn SJ, Baek SH, Kim TW, Nahm DS (2006) Discrimination of internal derangement of temporomandibular joint by lateral cephalometric analysis. Am J Orthod Dentofacial Orthop 130:331–339
Chen S, Lei J, Fu KY, Wang X, Yi B (2015) Cephalometric analysis of the facial skeletal morphology of female patients exhibiting skeletal class II deformity with and without temporomandibular joint osteoarthrosis. PLoS ONE 10:e0139743
Emshoff R, Moriggl A, Rudisch A, Brunold S, Neunteufel N, Crismani A (2011) Cephalometric variables discriminate among magnetic resonance imaging-based structural characteristic groups of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:118–125
Matsumoto R, Ioi H, Nishioka M, Goto TK, Nakata S, Nakasima A et al (2006) TMJ osteoarthritis/osteoarthrosis and dentofacial morphology in Japanese females. Orthod Waves 65:101–106
Matsuo Y, Kajii TS, Yasunaga M, Sakaguchi Y, Tamaoki S, Ishikawa H (2016) Characteristics of maxillofacial morphology of angle class II patients with temporomandibular disorders involving crepitus. Orthod Waves 75:27–34
Xie Q, Yang C, He D, Cai X, Ma Z, Shen Y et al (2016) Will unilateral temporomandibular joint anterior disc displacement in teenagers lead to asymmetry of condyle and mandible? A longitudinal study. J Cranio-Maxillofac Surg 44:590–596
Selaimen CMP, Jeronymo JCM, Brilhante DP, Lima EM, Grossi PK, Grossi ML (2007) Occlusal risk factors for temporomandibular disorders. Angle Orthod 77:471–477
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet J-P et al (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 28:6–27
Eichner K (1990) Renewed examination of the group classification of partially edentulous arches by Eichner and application advices for studies on morbidity statistics. Stomatol DDR 40:321–325
Okşayan R, Asarkaya B, Palta N, Şimşek İ, Sökücü O, İşman E (2014) Effects of edentulism on mandibular morphology: evaluation of panoramic radiographs. Sci World J 2014:254932
Rosa WGN, de Lima Navarro R, de Castro Ferreira Conti AC, de Almeida MR, Oltramari-Navarro PVP (2015) Assessment of cephalometric characteristics in the elderly. Braz Oral Res 29:1–9
Shimizu T, Motegi E, Nomura M, Kaneko Y, Takeuchi F, Yamaguchi T et al (2006) Cephalometric study of elderly with nearly intact dental arches. Gerodontology 23:60–63
Türp JC, Schindler H (2012) The dental occlusion as a suspected cause for TMDs: epidemiological and etiological considerations. J Oral Rehabil 39:502–512
Sipilä K, Näpänkangas R, Könönen M, Alanen P, Suominen AL (2013) The role of dental loss and denture status on clinical signs of temporomandibular disorders. J Oral Rehabil 40:15–23
Wiese M, Svensson P, Bakke M, List T, Hintze H, Petersson A et al (2008) Association between temporomandibular joint symptoms, signs, and clinical diagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. J Orofac Pain 22:239–251
Krisjane Z, Urtane I, Krumina G, Neimane L, Ragovska I (2012) The prevalence of TMJ osteoarthritis in asymptomatic patients with dentofacial deformities: a cone-beam CT study. Int J Oral Maxillofac Surg 41:690–695
Ioi H, Matsumoto R, Nishioka M, Goto TK, Nakata S, Nakasima A et al (2008) Relationship of TMJ osteoarthritis/osteoarthrosis to head posture and dentofacial morphology. Orthod Craniofac Res 11:8–16
Acknowledgements
This study was supported by an Estonian Science Foundation Grant (No. 9255), the Estonian Research Council Grant IUT 20–46, and the European Social Fund’s Doctoral Studies and Internationalisation Programme DoRa, which is carried out by Archimedes Foundation. The authors would also like to thank the Unimed United Clinics, Estonia, for their support in analyzing occlusion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have a conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Nguyen, M.S., Saag, M., Voog-Oras, Ü. et al. Temporomandibular Disorder Signs, Occlusal Support, and Craniofacial Structure Changes Among the Elderly Vietnamese. J. Maxillofac. Oral Surg. 17, 362–371 (2018). https://doi.org/10.1007/s12663-017-1057-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-017-1057-0