Abstract
Cerebral ischemia/reperfusion (I/R) injury is the main cause of death following trauma. The neuroprotective effect of sevoflurane (Sev) has been implicated in cerebral I/R injury. However, the mechanisms remain elusive. In this study, we aimed to explore its function in PC12 exposed to oxygen–glucose deprivation/reoxygenation (OGD/R) and in rats challenged with I/R. Sev pretreatment reduced the damage of PC12 cells after OGD/R treatment. Moreover, Sev pretreatment ameliorated neurobehavioral deficits induced by I/R treatment, reduced brain infarct volume, and decreased apoptosis of neurons in hippocampal tissues. Sev pretreatment reduced the surface expression of glutamate receptor 1 (GRIA1) in neurons, while GRIA1 reduced the neuroprotective effects of Sev pretreatment in vitro and in vivo. There was no difference in the surface expression of GRIA2 in rats with I/R and PC12 cells exposed to OGD/R. The ratio of GRIA1/GRIA2 surface expression was reduced, and calcium permeable-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (CP-AMPAR) was blocked by Sev. Together, Sev might exert beneficial effects on cerebral I/R-induced neuronal injury through inhibiting the surface expression of GRIA1 and blocking CP-AMPAR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke involves the rapid onset of focal neurological disturbances, and ischemic strokes, which are caused by the occlusion in the cerebral blood vessels, account for about 87% of all strokes (Stuckey et al. 2021). Ischemia triggers a constellation of events that initiate with loss of electrical function and progress to disturbance of membrane function with calcium influx contributing to calcium-dependent excitotoxicity, production of reactive oxygen species, and eventually destruction of cell membranes and lysis of cells (Feske 2021). To date, thrombolytic therapy with intravenous recombinant tissue-type plasminogen activator is recommended within the first 3–4.5 h (Mo et al. 2022). Despite significant advances in recanalization strategies, patients still suffer from ischemia/reperfusion (I/R) injuries (Jurcau and Simion 2021).
Back to 1963, it was observed that patients under general anesthesia were more tolerant to cerebral ischemia than unanesthetized patients (Neag et al. 2020). Because of the risk of cerebral ischemic injury, the brain is believed to have developed a backup machinery to survive in the event of an injury, and preconditioning can exploit the fundamental characteristic of adaptability in organisms (Thushara Vijayakumar et al. 2016). As a widely used anesthetics, sevoflurane (Sev) administration either prior to or after surgery has been reported to provide tolerance to ischemia both directly and indirectly (Xu et al. 2018). Sev treatment could reduce nerve function injury, cerebral infarction volume, neuronal apoptosis, and antioxidant stress (Liang et al. 2021). On top of that, the protective effects of Sev have been highlighted in multiple organs, including the heart (Hu et al. 2022), the liver (Zhang et al. 2022), and the spinal cord (Wang et al. 2021). Regarding the downstream molecular mechanism, researchers have focused on microRNAs (Ji et al. 2022; Li et al. 2020). However, there was little information regarding the downstream proteins of Sev in cerebral I/R. In the present study, by using two different bioinformatics websites BATMAN-TCM (http://bionet.ncpsb.org.cn/batman-tcm/index.php/Home/Index/index) and STITCH (http://stitch.embl.de/cgi/input.pl?UserId=5d5hKidRT7HO&sessionId=qXNII9CgUcBy), we identified that glutamate receptor 1 (GRIA1) was the common target of Sev. During ischemia, increased cell catabolism, decreased amount of ATP available, intracellular sodium accumulation, changes in membrane potential, and increased activity of excitatory neurotransmitters, such as glutamate, can be observed (Nunes et al. 2013). Glutamate receptors of the AMPA type (AMPARs) are the major contributors of fast excitatory transmission in the brain, and AMPA receptors are heteromeric dimers-of-dimers that draw from a pool of four subunits (GluA1-GluA4) encoded by four genes (GRIA1-4) (Shen and Limon 2021). Therefore, the present study examined whether GRIA1 was involved in the neuroprotection of Sev preconditioning and investigated the potential mechanism underlying this effect against cerebral I/R injury.
Materials and Methods
Cell Culture and Infection
PC-12 cells provided by the National Infrastructure of Cell Line Resource (Beijing, China) were cultured in Dulbecco’s modified Eagle’s medium (DMEM) plus 10% FBS and 1% penicillin/streptomycin in a 5% CO2 incubator at 37 °C. The packaged GRIA1 overexpressing adeno-associated virus (AAV, AAV-GRIA1) and its negative control (AAV-NC) were purchased from WZ Biosciences (Jinan, Shandong, China). The cells were seeded into 24-well plates. When the cells reached a 60% confluence, AAV solution was added to PC12 cell culture medium for a 72-h infection.
OGD/R In Vitro
The PC12 cells were detached and seeded into 96-well plates. When the cell density to 60–70%, the OGD treatment was performed by replacing the culture medium with glucose-free DMEM, and the cultures were placed in an anaerobic chamber containing 95% N2 and 5% CO2. After 2 h, the cell culture medium was renewed with fresh DMEM/F12K complete medium and cultured in a 37 °C incubator with 5% CO2 for 22 h.
Cell Viability Assay
The PC12 cells were exposed to OGD/R and assayed for cell viability using the cell counting kit-8 (CCK-8) assays. In brief, the cells were treated with OGD/R and incubated at 37 °C for 2 h with 10 μL of CCK-8 reagent (ab228554, Abcam, Cambridge). Finally, the optical density (OD) value at 450 nm was measured on a microplate reader.
Cell Proliferation Assay
The PC12 cells were treated with OGD/R, and cell proliferation was detected by EdU kits (C0071S, Beyotime Biotechnology Co., Ltd., Shanghai, China). EdU was added after OGD/R treatment and incubated for 2 h. The cells were subsequently fixed with formaldehyde for 15 min, treated with Triton X-100 for 15 min, and incubated for 30 min with click reaction solution in the dark. The cells were stained with Hoechst 33,342, photographed, and observed by fluorescence microscopy.
Cell Apoptosis Assay
Apoptosis was detected according to the Annexin V-fluorescein isothiocyanate (FITC) Apoptosis Detection Kit (APOAF, Sigma-Aldrich Chemical Company, St Louis, MO, USA). The cells after OGD/R treatment were collected, detached, washed with PBS, and resuspended to a density of 1 × 106 cells/mL with Annexin V binding buffer. The cell suspension was incubated with FITC-Annexin V and propidium iodide (PI) in the dark to detect apoptosis by flow cytometry.
Lactate Dehydrogenase (LDH) Release Assay
LDH kit (Beyotime) was used to confirm the release of LDH from neurons. Cell culture supernatant was taken after OGD/R treatment, and LDH detection reagents were added as described in the kit. The cellular LDH release was detected by OD490 readings.
RNA Isolation and RT-qPCR
Cells or tissues were subjected to total RNA extraction using TRIzol reagent (15,596,026, Invitrogen Inc., Carlsbad, CA, USA). For quantitative real-time PCR, cDNAs were prepared using PrimeScript™ RT reagent Kit (RR037A, Takara Holdings Inc., Kyoto, Japan). RT-qPCR was performed with TB Green® Premix Ex Taq™ II (RR820A, TaKaRa). Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as a reference. The relative level of each mRNAs was calculated using the 2−△△Ct method. All PCR primer sequences were as follows: GRIA1 forward: 5′-GGACAACTCAAGCGTCCAGA-3′, reverse: 5′-CACAGTAGCCCTCATAGCGG-3′; GRIA2 forward: 5′-ATGCGGTTAACCTCGCAGTA-3′, reverse: 5′-CAATAGTGGCTGCGGAAACG-3′; GAPDH forward: 5′-GCATCTTCTTGTGCAGTGCC-3′, reverse: 5′-GATGGTGATGGGTTTCCCGT-3′.
Western Blot
Total cellular proteins were extracted using RIPA lysis buffer (89,901, Thermo Fisher). The BCA Protein Quantification Kit (23,225, Thermo Fisher) was used for the quantitative analysis of proteins. After the proteins were separated by electrophoresis and transferred, the membranes were sealed with 5% milk for 1 h. The polyvinylidene difluoride membranes were probed with primary antibodies against cleaved-caspase 3 (1:1000, #9664, CST, Beverly, MA, USA) and GAPDH (1:10,000, ab181602, Abcam) overnight at 4 °C and with HRP-labeled goat anti-rabbit IgG secondary antibody (1:2000, ab6721, Abcam) for 60 min at room temperature. Finally, the ECL luminescence kit (ab65623, Abcam) was used for development and analysis.
Detection of Intracellular Calcium
Changes in intracellular calcium concentration were detected according to the instructions provided by the Fluo-4, AM (CA1190, Beijing Solarbio Life Sciences Co., Ltd., Beijing, China) kit. After detachment and collection of the treated cells, 4 µM Fluo-4, AM working solution was prepared with Hank’s balanced salt solution (HBSS). Fluo-4, AM working solution was added to the cells and incubated for 20 min at 37 °C. The cells were incubated with HBSS containing 1% FBS for 40 min, resuspended in HEPES buffer, and incubated for 10 min at 37 °C before flow cytometry analysis.
Animals
The procedures regarding animals were carried out as per with the institutional guideline of Guide for the Care and Use of Laboratory Animals (proposed by NIH), and the protocols used in the present study were approved by the Ethics Committee for the Second Hospital of Hebei Medical University. Adult male Sprague–Dawley rats (280–320 g) were purchased from Vital River (Beijing, China). Rats were randomly divided into 5 groups (n = 10): sham (sham-operated), ischemia–reperfusion (I/R), Sev pretreatment followed by I/R (Sev + I/R), NC AAC delivery followed by Sev pretreatment, and I/R (AAV-NC + Sev + I/R), AAV targeting GRIA1 delivery followed by Sev pretreatment and I/R (AAV-GRIA1 + Sev + I/R).
The rats were anesthetized by 3% Sev and fixed on a brain stereotaxic instrument (Stoelting Co., Chicago, IL, USA). The stainless-steel catheter was stereotaxically fixed to the ventricles. The anterior fontanelle point was centered, and the lateral ventricles were stereotaxically positioned at coordinates of 1.0 mm toward bregma and 1.2–1.5 mm lateral to the midsagittal line. AAV solution (2 μL) was microinjected into the ventricles, and subsequent experiments were performed after 72 h.
The rats were treated with 3% Sev for anesthesia. An incision was made in the middle of the neck to isolate and expose the neck vessels. The external and internal carotid arteries were separated, and a 3–0 antimicrobial suture (MCP316H, Ethicon, INC., Somerville, NJ, USA) was inserted into the internal carotid artery for middle cerebral artery occlusion. After 2 h of occlusion, the nylon sutures were drawn out to let the blood flow recover for 22 h. During the procedure, the rats were placed on a 37 °C heating pad to maintain the body temperature. For the sham-operated group, the same surgical operation was implemented without occlusion.
Sev Preconditioning
For in vivo experiments, the rats were pretreated in a 2.7% Sev and O2 environment for 1 h. In in vitro experiments, the PC12 cells were treated with 3.3% Sev and 5% CO2 for 2 h and placed back into a 5% CO2 incubator at 37 °C for 1 h, followed by the OGD/R exposure.
Neurobehavioral Assessment and Infarct Evaluation
The rats were scored according to their neurological status on the following criteria: 0, no deficit; 1, contralateral forelimb flexion; 2, contralateral forelimb flexion and spontaneous rotation; 3, rotation to the hemiplegic side; and 4, unconsciousness and no spontaneous movement.
After reperfusion, the brain tissues were sliced into 2-mm-thick coronal sections. TTC (T8877, Sigma-Aldrich Chemical Company, St Louis, MO, USA) staining was used to detect the cerebral infarction in rats. The sections were immersed in 2% TTC for 30 min at 37 °C and then placed in paraformaldehyde for fixation. The infarcted area was white, and the non-infarcted area was pink. ImageJ software (NIH, Bethesda, MD, USA) was applied to analyze the volume of the infarcts.
Immunofluorescence Staining
To detect the surface expression of GRIA1 and GRIA2, cells or tissue sections were fixed with 4% paraformaldehyde, sealed with 4% goat serum, and treated with mouse antibodies to GluA1 N-terminal (1:500, MAB2263, Sigma) or GluA2 N-terminal (1:500, MAB397, Sigma) at 4 °C. Subsequently, the coverslips or sections were incubated with Alexa Fluor® 647-coupled goat anti-mouse IgG secondary antibody (1:200, ab150115, Abcam). The coverslips were permeabilized with Triton-X-100 after PBS washing and then counter-stained with DAPI. Tissue sections were permeabilized in Triton-X-100 and incubated with FITC-coupled NeuN antibody (1:100, ab223994, Abcam). Finally, images were captured under a fluorescent microscope.
Histology
The hippocampal sections were fixed in paraformaldehyde and then dewaxed in xylene. The sections were stained with hematoxylin–eosin (HE, Solarbio) or Nissl staining solution (Beyotime) after hydration in gradient alcohol. Finally, the sections were sealed with resin after dehydration and clearing.
TUNEL Detection
Brain tissues were examined for apoptosis as described in the instructions for the TUNEL Apoptosis Detection Kit (40306ES20, Yeasen Biotechnology Co., Ltd., Shanghai, China). The tissues were fixed in 4% paraformaldehyde for 30 min, incubated with Proteinase K for 10 min, and then equilibrated in equilibration buffer. The sections were treated with TUNEL reaction mixture in the dark, and DAPI was applied for nuclei counterstaining. Finally, images were taken with a fluorescence microscope.
Statistical Methods
Data was performed using GraphPad Prism 8.0.2 (GraphPad, San Diego, CA, USA), and the results were expressed as mean ± SD. Statistical analyses involved an unpaired t-test to compare two groups and a one-way ANOVA with Tukey’s post hoc test for between-group differences to compare three or more groups. The difference was statistically significant at p < 0.05.
Results
Sev Inhibits OGD/R-Induced Neuronal Damage
PC12 cell activity after OGD/R treatment was measured using CCK-8 assays. PC12 cell activity was found to be decreased in the OGD/R group, while was restored in the Sev + OGD/R group (Fig. 1A). The EdU assay showed that the proliferative capacity of cells was hampered by OGD/R exposure, while Sev pretreatment increased the proliferative activity of cells (Fig. 1B). The release of LDH from cells in the OGD/R group was increased, which was reduced by pretreatment with Sev (Fig. 1C). The flow cytometry results indicated that the apoptosis was elevated in the OGD/R group, and Sev pretreatment decreased the apoptosis (Fig. 1D). In addition, Sev pretreatment decreased the expression of cleaved-caspase 3 induced by OGD/R in PC12 cells (Fig. 1E).
Sev pretreatment exerts a protective effect against OGD/R-induced neuronal damage. A CCK-8 assay for PC12 cell viability. B EdU assays for cell proliferation. C LDH release of PC12 cells. D PC12 cell apoptosis assessed by flow cytometry. E Western blot detection of cleaved-caspase 3 expression in PC12 cells. n = 3; *p < 0.05 vs. the control or OGD/R groups. All data were expressed as mean ± SD. One-way ANOVA with Tukey’s post hoc test was applied for statistical analysis
Sev Alleviates Cerebral I/R-Induced Neurological Injury
Sham-operated rats had no neurobehavioral deficits, whereas rats in the I/R group had significant neurobehavioral deficits, which were reduced by Sev pretreatment (Fig. 2A). TTC results showed a significant increase in the volume of cerebral infarcts in rats with I/R, and Sev pretreatment reduced the volume of cerebral infarcts (Fig. 2B). HE staining showed that the hippocampal tissues in the sham-operated rats had more neurons and regular cell arrangement. Neurons in the I/R group were atrophied and irregularly shaped. Compared with the I/R group, the damage of neurons in the Sev + I/R group was alleviated, and the cells were arranged more closely than those in the I/R group (Fig. 2C). The results of Nissl staining demonstrated that the sham-operated rats had regular neuronal morphology, deep neuronal staining, and increased number of Nissl bodies. The I/R group had irregularly arranged neurons and a reduced number of Nissl bodies. The number of neurons in the Sev + I/R group was increased (Fig. 2D). After that, we examined the neuronal apoptosis in hippocampal tissues using TUNEL assay. It was found that the level of neuronal apoptosis was increased in the I/R group compared to the Sham group, while Sev pretreatment alleviated the neuronal apoptosis in rats (Fig. 2E).
Sev preconditioning induces neuroprotection against cerebral I/R injury in rats. A Neurobehavioral scores in rats (n = 10). B TTC assay for cerebral infarct volume in rats (n = 5). C Representative HE staining of rat hippocampal tissues. D Nissl staining for neuronal damage in hippocampal tissues. E TUNEL assay for apoptosis in rat neurons (n = 5). *p < 0.05 vs. the sham or I/R groups. All data were expressed as mean ± SD. One-way ANOVA with Tukey’s post hoc test was applied for statistical analysis
Sev Preconditioning Inhibits the Expression of GRIA1
We predicted downstream target proteins of Sev (PubChem CID:5206) in BATMAN-TCM (http://bionet.ncpsb.org.cn/batman-tcm/index.php/Home/Index/index) and STITCH (http://stitch.embl.de/cgi/input.pl?UserId=5d5hKidRT7HO&sessionId=qXNII9CgUcBy) (Fig. 3A–B). The two databases shared a common target protein: GRIA1 (Fig. 3C). We examined the difference in GRIA1 expression after Sev pretreatment. RT-qPCR results displayed that GRIA1 expression was elevated in PC12 cells in the OGD/R group, and Sev pretreatment inhibited the GRIA1 mRNA expression stimulated by OGD/R (Fig. 3D). The expression of GRIA1 mRNA in vivo had the same trend as in the PC12 cells (Fig. 3E). The surface expression of GRIA1 in PC12 and hippocampal tissues was detected by immunofluorescence, and the results showed that Sev pretreatment decreased the surface expression of GRIA1 in PC12 cells as well as neuronal cells in hippocampal tissues (Fig. 3F–G).
Sev preconditioning reduces the GRIA1 surface expression in PC12 cells and hippocampal tissues of rats with I/R. A Prediction of downstream target proteins of Sev in BATMAN-TCM. B Prediction of downstream target proteins of Sev in STITCH. C Intersection of Sev downstream target proteins in BATMAN-TCM and STITCH. D Detection of GRIA1 expression in PC12 cells by RT-qPCR (n = 3). E Expression of GRIA1 mRNA in hippocampal tissues of rats with I/R by RT-qPCR (n = 5). F Immunofluorescence detection of surface expression of GRIA1 in PC12 cells (n = 3). G Immunofluorescence detection of surface expression of GRIA1 in neurons from hippocampal tissues of rats with I/R (n = 5). *p < 0.05 vs. the OGD/R or I/R groups. All data were expressed as mean ± SD. Unpaired t test was applied for statistical analysis
GRIA1 Overexpression Promotes Neuronal Damage After OGD/R Treatment
The PC12 cells were infected with AAV-GRIA1 or the control AAV-NC to study the effects of GRIA1 on neuronal damage in vitro. The mRNA and surface expression of GRIA1 in PC12 cells after Sev pretreatment and OGD/R exposure was examined by RT-qPCR and immunofluorescence, respectively. The results showed increased GRIA1 mRNA levels and surface expression in PC12 cells in the AAV-GRIA1 + Sev + OGD/R group compared with the AAV-NC + Sev + OGD/R group (Fig. 4A–B). AAV-GRIA1 infection led to reduced cell viability (Fig. 4C) and proliferation in PC12 cells (Fig. 4D), as judged by CCK-8 and EdU assays. In addition, the extent of cell damage was found to increase after GRIA1 overexpression by LDH release assay (Fig. 4E), and flow cytometry and Western blot results showed an increase in PC12 cell apoptosis (Fig. 4F–G).
Overexpression of GRIA1 in PC12 cells aggravates cell damage after Sev pretreatment and OGD/R treatment. A Detection of GRIA1 expression in PC12 cells by RT-qPCR. B Immunofluorescence detection of surface expression of GRIA1 in PC12 cells. C CCK-8 assay for PC12 cell viability. D EdU assays for cell proliferation. E LDH release of PC12 cells. F PC12 cell apoptosis detected by flow cytometry. G Western blot detection of cleaved-caspase 3 expression in PC12 cells. n = 3; *p < 0.05 vs. The AAV-NC + Sev + OGD/R groups. All data were expressed as mean ± SD. Unpaired t test was applied for statistical analysis
GRIA1 Overexpression Exacerbates Neuronal Injury Induced by Cerebral I/R in Rats
AAV-GRIA1 or the control AAV-NC was delivered into the rats via an intracerebroventricular injection. In the same vein, we observed enhanced GRIA1 mRNA levels, and surface expression was increased in hippocampal tissues of rats administrated with AAV-GRIA1 (Fig. 5A, B). We performed Sev pretreatment and cerebral I/R in AAV-NC- as well as AAV-GRIA1-infected rats. Rats overexpressing GRIA1 had more severe neurological deficits and brain infarction (Fig. 5C, D). HE staining showed that neurons in the AAV-GRIA1 + Sev + I/R group exhibited more severe damage compared with the AAV-NC + Sev + I/R group (Fig. 5E). Nissl staining showed a decrease in the number of Nissl bodies in the AAV-GRIA1 + Sev + I/R group (Fig. 5F). It was also displayed by TUNEL assay that GRIA1 overexpression increased apoptosis of neurons in brain tissues (Fig. 5G).
Overexpression of GRIA1 attenuates the neuroprotective effect of Sev preconditioning against cerebral I/R injury. A Expression of GRIA1 mRNA in rat hippocampal tissue detected by RT-qPCR (n = 5). B Immunofluorescence detection of surface expression of GRIA1 in neurons in rat hippocampal tissues (n = 5). C Neurobehavioral scores in rats (n = 10). D TTC assay for cerebral infarct volume in rats (n = 5). E Representative HE staining of rat hippocampal tissues. F Nissl staining for neuronal damage in hippocampal tissues. G TUNEL assay for apoptosis in rat neurons (n = 5). *p < 0.05 vs. the AAV-NC + Sev + I/R groups. All data were expressed as mean ± SD. Unpaired t test was applied for statistical analysis
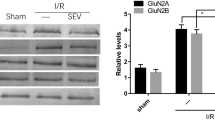
Sev Blocks CP-AMPAR
We detected an elevated concentration of intracellular Ca2+ in PC12 cells after OGD/R treatment, which was reduced by Sev (Fig. 6A). RT-qPCR results showed that Sev did not affect the expression of GRIA2 mRNA in PC12 cells and hippocampal tissues of rats (Fig. 6B–C). No significant variations regarding the surface expression of GRIA2 in PC12 cells as well as hippocampal tissue neurons were seen upon Sev pretreatment, as demonstrated by immunofluorescence (Fig. 6D–E). We have demonstrated that Sev decreased the surface expression of GRIA1, suggesting that Sev blocks CP-AMPAR by decreasing the ratio of GRIA1/GRIA2 surface expression.
Sev decreases the ratio of GRIA1/GRIA2 surface expression and blocks CP-AMPAR. A Intracellular Ca2+ concentration in PC12 cells detected by flow cytometry (n = 3). B RT-qPCR detection of GRIA2 mRNA expression in PC12 cells (n = 3). C Detection of GRIA2 mRNA expression in hippocampal tissues by RT-qPCR (n = 5). D Immunofluorescence detection of GRIA2 surface expression in PC12 cells (n = 3). E Immunofluorescence detection of GRIA2 surface expression in hippocampal tissues (n = 5). *p < 0.05 vs. the OGD/R or I/R groups. All data were expressed as mean ± SD. Unpaired t test was applied for statistical analysis
Discussion
The role of GRIA1 in the neuroprotective effect induced by Sev preconditioning against I/R events was studied in vitro and in vivo. The main findings are as follows: (i) Sev preconditioning improved cell viability and reduced apoptosis in PC12 cells challenged by OGD/R, (ii) Sev preconditioning improved neurological outcomes and narrowed infarction volume in rats induced with MCAO, (iii) Sev preconditioning decreased surface expression of GRIA1, and (iv) tolerance to OGD/R in the cells and to I/R injury in the rats induced by Sev preconditioning was compromised by upregulation of GRIA1. These results indicate that GRIA1 depletion plays a pivotal role in the induction of the neuroprotective effect by Sev preconditioning.
Sev treatment has been reported to reduce the inflammatory response and neuronal apoptosis in rats and mice with cerebral I/R (Zhong et al. 2020). Furthermore, Sev preconditioning significantly attenuated OGD-induced cell injury in vitro and reduced infarct volume and improved neurological deficits induced by cerebral I/R injury in a transient ischemia rat model (Cai et al. 2017; Tong et al. 2014). These evidences were largely in line with our observation. In addition, the liver functions were obviously improved after Sev treatment, as determined by the histopathological studies and alterations in liver enzymes such as LDH (Ma et al. 2021; Xu et al. 2021). Here, we also noted that the cytotoxicity induced by OGD/R was partially alleviated by Sev preconditioning in PC12 cells, as judged by lowered LDH levels. Likewise, Sev postconditioning boosted coronary flow, accelerated functional recovery, and decreased Bax/Bcl-2 and the extent of apoptosis in aging rats (Jiang et al. 2016). The anti-apoptotic properties of Sev have been validated also in vitro and in vivo in the present study.
Intriguingly, Sev preconditioning has been verified to provide neuroprotection against cerebral I/R injury by inhibiting the tyrosine phosphorylation of GluN2A/GluN2B (Jin and Bo 2021). In the present study, we identified GRIA1 as the downstream target of Sev. The overactivation of postsynaptic receptors, such as NMDA receptors and CPAMPAR, leads to an overload of intracellular calcium, which is a major event responsible for neuronal death associated with stroke (Achzet et al. 2021). In the same vein, we observed the overexpression of GRIA1 in PC12 cells under the exposure to OGD/R and in hippocampal tissues of rats with I/R injury, which was reduced by Sev preconditioning. In hippocampal CA1 neurons, the majority of AMPAR are made up of GRIA1/GRIA2 and GRIA2/GRIA3 heterotetramers, and the composition of the receptor tetramer principally determines the functionality of the receptor (Qu et al. 2021). The existence and dynamic regulation of GRIA2-lacking CP-AMPAR enable these special receptors to function as signaling molecules via calcium influx (Man 2011). On the other hand, the regulated expression and trafficking of GRIA1-homomeric subtype of CP-AMPAR mediates diverse types of synaptic plasticity, thereby playing important roles in brain function and dysfunction (Ge and Wang 2021). GRIA1 is dominant in activity-dependent recruitment of AMPARs to synapses, which is mediated by phosphorylation of GRIA1 and interaction with synaptic PDZ domain-containing proteins that recruit and retain GRIA1-GRIA2 AMPARs at synapses during the induction of long-term potentiation (Henley and Wilkinson 2016). GRIA1 has been recently shown as a part of a synaptic protein complex that modulates neuronal excitability (Ibanez et al. 2022). To further characterize the involvement of GRIA1 in Sev-mediated neuroprotection, we overexpressed GRIA1 in PC12 cells or rats by delivery of AAV containing GRIA1. It was found that the neuroprotective effects of Sev were compromised by GRIA1 overexpression.
More specifically, Stockwell et al. reported that hypoxia (20 min) induced internalization of both AMPAR subunits, and following normoxic reperfusion (45 min) augmented GRIA1 but persistently reduced GRIA2 surface expression (Stockwell et al. 2016). Gerace et al. presented that PARP-1 activation using N-methyl-N′-nitro-N′-nitrosoguanidine increased the ratio of GRIA1/GRIA2 expression, leading to a significant deterioration of neuronal membrane properties and neuronal death in the hippocampal CA1 region (Gerace et al. 2014). Here, we found that the concentration of Ca2+ was elevated in PC12 cells upon the treatment of OGD/R. However, no significant variations were seen in the mRNA and surface expression of GRIA2 in the cell and tissues upon the application of Sev. These findings suggested that Sev blocked CP-AMPAR by decreasing the ratio of GRIA1/GRIA2 surface expression. We utilized a pheochromocytoma cell line PC12 in this study, which is a study limitation. It is unclear whether these results are reproducible in different cell lines and in primary cultures of neuronal cells, and further studies will need to be conducted to confirm these results.
Conclusion
In conclusion, our results indicate that exposure to Sev preconditioning has beneficial effects against neuronal apoptosis induced by cerebral I/R injury. Downregulation of GRIA1 and the ensuing CP-AMPAR deficit may underlie these alterations. These data provide a new insight of molecular mechanisms underlying Sev-induced neuroprotection (Fig. 7).
Availability of Data and Materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Achzet LM, Davison CJ, Shea M, Sturgeon I, Jackson DA (2021) Oxidative stress underlies the ischemia/reperfusion-induced internalization and degradation of AMPA receptors. Int J Mol Sci 22. https://doi.org/10.3390/ijms22020717
Cai M, Tong L, Dong B, Hou W, Shi L, Dong H (2017) Kelch-like ECH-associated protein 1-dependent nuclear factor-E2-related factor 2 activation in relation to antioxidation induced by sevoflurane preconditioning. Anesthesiology 126:507–521. https://doi.org/10.1097/ALN.0000000000001485
Feske SK (2021) Ischemic Stroke Am J Med 134:1457–1464. https://doi.org/10.1016/j.amjmed.2021.07.027
Ge Y, Wang YT (2021) GluA1-homomeric AMPA receptor in synaptic plasticity and neurological diseases. Neuropharmacology 197:108708. https://doi.org/10.1016/j.neuropharm.2021.108708
Gerace E et al (2014) PARP-1 activation causes neuronal death in the hippocampal CA1 region by increasing the expression of Ca(2+)-permeable AMPA receptors. Neurobiol Dis 70:43–52. https://doi.org/10.1016/j.nbd.2014.05.023
Henley JM, Wilkinson KA (2016) Synaptic AMPA receptor composition in development, plasticity and disease. Nat Rev Neurosci 17:337–350. https://doi.org/10.1038/nrn.2016.37
Hu B, Tian T, Hao PP, Liu WC, Chen YG, Jiang TY, Xue FS (2022) The Protective Effect of Sevoflurane Conditionings against Myocardial Ischemia/reperfusion Injury: a Systematic Review and Meta-Analysis of Preclinical Trials in in-Vivo Models Front Cardiovasc Med 9:841654. https://doi.org/10.3389/fcvm.2022.841654
Ibanez L et al (2022) Multi-ancestry GWAS reveals excitotoxicity associated with outcome after ischaemic stroke. Brain 145:2394–2406. https://doi.org/10.1093/brain/awac080
Ji H, Li H, Zhang H, Cheng Z (2022) Role of microRNA-218–5p in sevoflurane-induced protective effects in hepatic ischemia/reperfusion injury mice by regulating GAB2/PI3K/AKT pathway. Mol Med Rep 25. https://doi.org/10.3892/mmr.2021.12517
Jiang JJ, Li C, Li H, Zhang L, Lin ZH, Fu BJ, Zeng YM (2016) Sevoflurane postconditioning affects post-ischaemic myocardial mitochondrial ATP-sensitive potassium channel function and apoptosis in ageing rats. Clin Exp Pharmacol Physiol 43:552–561. https://doi.org/10.1111/1440-1681.12565
Jin L, Bo XM (2021) Neuroprotection of sevoflurane against ischemia/reperfusion-induced brain injury through inhibiting GluN2A/GluN2B-PSD-95-MLK3 module. Exp Brain Res 239:2701–2709. https://doi.org/10.1007/s00221-021-06157-x
Jurcau A, Simion A (2021) Neuroinflammation in cerebral ischemia and ischemia/reperfusion injuries: from pathophysiology to therapeutic strategies. Int J Mol Sci 23. https://doi.org/10.3390/ijms23010014
Li Y, Xing N, Yuan J, Yang J (2020) Sevoflurane attenuates cardiomyocyte apoptosis by mediating the miR-219a/AIM2/TLR4/MyD88 axis in myocardial ischemia/reperfusion injury in mice. Cell Cycle 19:1665–1676. https://doi.org/10.1080/15384101.2020.1765512
Liang TY, Peng SY, Ma M, Li HY, Wang Z, Chen G (2021) Protective Effects of Sevoflurane in Cerebral Ischemia Reperfusion Injury: a Narrative Review Med Gas Res 11:152–154. https://doi.org/10.4103/2045-9912.318860
Ma H et al (2021) Sevoflurane protects the liver from ischemia-reperfusion injury by regulating Nrf2/HO-1 pathway. Eur J Pharmacol 898:173932. https://doi.org/10.1016/j.ejphar.2021.173932
Man HY (2011) GluA2-lacking, calcium-permeable AMPA receptors–inducers of plasticity? Curr Opin Neurobiol 21:291–298. https://doi.org/10.1016/j.conb.2011.01.001
Mo Z, Zeng Z, Liu Y, Zeng L, Fang J, Ma Y (2022) Activation of Wnt/beta-Catenin Signaling Pathway as a Promising Therapeutic Candidate for Cerebral Ischemia/reperfusion Injury Front Pharmacol 13:914537. https://doi.org/10.3389/fphar.2022.914537
Neag MA, Mitre AO, Catinean A, Mitre CI (2020) An overview on the mechanisms of neuroprotection and neurotoxicity of isoflurane and sevoflurane in experimental studies. Brain Res Bull 165:281–289. https://doi.org/10.1016/j.brainresbull.2020.10.011
Nunes RR, Duval Neto GF, Garcia de Alencar JC, Franco SB, de Andrade NQ, Holanda Dumaresq DM, Cavalcante SL (2013) Anesthetics, cerebral protection and preconditioning. Braz J Anesthesiol 63:119–128. https://doi.org/10.1016/S0034-7094(13)70204-6
Qu W et al (2021) Emerging role of AMPA receptor subunit GluA1 in synaptic plasticity: implications for Alzheimer’s disease. Cell Prolif 54:e12959. https://doi.org/10.1111/cpr.12959
Shen K, Limon A (2021) Transcriptomic expression of AMPA receptor subunits and their auxiliary proteins in the human brain. Neurosci Lett 755:135938. https://doi.org/10.1016/j.neulet.2021.135938
Stockwell J, Chen Z, Niazi M, Nosib S, Cayabyab FS (2016) Protein phosphatase role in adenosine A1 receptor-induced AMPA receptor trafficking and rat hippocampal neuronal damage in hypoxia/reperfusion injury. Neuropharmacology 102:254–265. https://doi.org/10.1016/j.neuropharm.2015.11.018
Stuckey SM, Ong LK, Collins-Praino LE, Turner RJ (2021) Neuroinflammation as a key driver of secondary neurodegeneration following stroke?. Int J Mol Sci 22. https://doi.org/10.3390/ijms222313101
Thushara Vijayakumar N, Sangwan A, Sharma B, Majid A, Rajanikant GK (2016) Cerebral ischemic preconditioning: the road so far. Mol Neurobiol 53:2579–2593. https://doi.org/10.1007/s12035-015-9278-z
Tong L, Cai M, Huang Y, Zhang H, Su B, Li Z, Dong H (2014) Activation of K(2)P channel-TREK1 mediates the neuroprotection induced by sevoflurane preconditioning. Br J Anaesth 113:157–167. https://doi.org/10.1093/bja/aet338
Wang D, Fang B, Wang Z, Li X, Chen F (2021) Sevoflurane Pretreatment Regulates Abnormal Expression of MicroRNAs Associated with Spinal Cord Ischemia/reperfusion Injury in Rats Ann Transl Med 9:752. https://doi.org/10.21037/atm-20-7864
Xu H, Mei XP, Xu LX (2018) The effect of pre- and after-treatment of sevoflurane on central ischemia tolerance and the underlying mechanisms J Dent Anesth. Pain Med 18:1–8. https://doi.org/10.17245/jdapm.2018.18.1.1
Xu L, Ge F, Hu Y, Yu Y, Guo K, Miao C (2021) Sevoflurane postconditioning attenuates hepatic ischemia-reperfusion injury by limiting HMGB1/TLR4/NF-kappaB pathway via modulating microRNA-142 in vivo and in vitro. Front Pharmacol 12:646307. https://doi.org/10.3389/fphar.2021.646307
Zhang K, Xu X, Hu L (2022) Sevoflurane attenuates hepatic ischemia reperfusion injury by the miR-122/Nrf2 pathway. Ann Transl Med 10:350. https://doi.org/10.21037/atm-22-115
Zhong H, Chen H, Gu C (2020) Sevoflurane post-treatment upregulated miR-203 expression to attenuate cerebral ischemia-reperfusion-induced neuroinflammation by targeting MyD88. Inflammation 43:651–663. https://doi.org/10.1007/s10753-019-01147-2
Author information
Authors and Affiliations
Contributions
YL is the guarantor of integrity of the entire study and contributed to the concepts; ZL, SYL, XNW, and TY contributed to the experimental studies, data acquisition, and statistical analysis; KM and KC contributed to data analysis and manuscript review. All authors contributed to the manuscript preparation and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
The procedures regarding animals were carried out as per the institutional guideline of Guide for the Care and Use of Laboratory Animals (proposed by NIH), and the protocols used in the present study were approved by the Ethics Committee for the Second Hospital of Hebei Medical University.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, Y., Liang, Z., Lei, S. et al. Sevoflurane Preconditioning Downregulates GRIA1 Expression to Attenuate Cerebral Ischemia–Reperfusion-Induced Neuronal Injury. Neurotox Res 41, 29–40 (2023). https://doi.org/10.1007/s12640-022-00620-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-022-00620-5