Abstract
Bisphenol A (BPA) exposure can be associated with neurodevelopmental disorders due to impairment of cell proliferation and synaptic development. Our study evaluated the effects of melatonin (MEL) on ambulatory activity, lipid peroxidation, cytokines, ERK/NF-kB signaling pathway in the hippocampus and frontal lobe, and histopathological changes in the hippocampus of the BPA-treated rats. The animals were divided into 4 groups: control, BPA, BPA + MEL I, and BPA + MEL II. MEL I (20 mg/kg b.w.) and MEL II (40 mg/kg b.w.) were orally administered for 28 days. On the 29th day, BPA (1 mg/kg b.w.) was intraperitoneally administered, and, after 24 h, an open field test (OFT) and an elevated plus maze (EPM) were conducted. The results showed that the MEL II group made significantly more entries in the open arms of EPM, traveled significantly greater distance, and spent more time in the central part of OFT. Malondialdehyde levels were diminished by MEL II in the hippocampus and by MEL I in the frontal lobe. In the hippocampus, the MAPK level was significantly lowered by both doses of MEL (p < 0.05) while in the frontal lobe, only MEL II reduced the MAPK activation. MEL I and II significantly decreased the γH2AX and upregulated the NFkB and pNFkB expressions in the hippocampus while MEL II downregulated the MCP1 expression. Both doses of MEL attenuated the BPA-evoked histopathological alterations in the hippocampus. These data indicate that MEL can mediate the neuroprotection against BPA-induced neurotoxicity and improves behavioral changes suggesting a real potential as a protective agent in brain toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphenol A, (2, 2-bis-(4-hydroxyphenyl) propane), known as an endocrine disruptor compound (EDC), is frequently used in the manufacturing of plastics and epoxy resin, such as food and beverage containers, dental sealants, water supply pipes, toys, cigarette filters, electronics, sport equipment, or medical devices (Chouhan et al. 2014; Rebolledo-Solleiro et al. 2021; Santoro et al. 2019; Shafei et al. 2018).
Solid evidence indicates that exposure to BPA may be associated with infertility, cardiovascular diseases, cancer, alterations in metabolism (obesity and hyperinsulinemia), and impaired thyroid and brain function (Bittner et al. 2014; Rochester 2013).
Several authors sustain that BPA exposure can be associated with neurodevelopmental disorders (autism spectrum disorder, attention deficit hyperactivity disorder) or with neurodegenerative disorders (Parkinson’s disease, amyotrophic lateral sclerosis) (Homberg et al. 2016; Ishido and Masuo 2014; Morrice et al. 2006). Although the mechanisms of BPA on brain development are not fully understood, numerous studies sustain that it may impair neural stem cell proliferation and differentiation, synapse formation, and synaptic plasticity, especially in the hippocampus and prefrontal cortex (Ali et al. 2017; Carr et al. 2003; Hass et al. 2016).
Exposure to BPA has been linked to numerous health effects on the body, while the mechanism of BPA on the developing brain is still poorly understood.
Based on both in vivo and in vitro studies, BPA exposure has also been found to affect spatial learning and memory, emotionality, and behavior (social and sexual) (Hass et al. 2016; Nakamura et al. 2006).
The wide variety of cellular and molecular mechanisms that may explain the neurological effects of exposure to BPA could be endocrine-related and epigenetic-related or affect the mitochondria, calcium metabolism, free radicals’ generation, and inflammatory response. BPA can act as an agonist or antagonist on estrogen and androgen receptors, induce the alteration of the hypothalamic–pituitary–adrenal (HPA) axis and glucocorticoid receptor (GR), and modify the thyroid receptor expression leading to hypothyroxinemia, or trigger the disruption of the organization and function of the oxytocin (OT)/vasopressin (AVP) system. BPA also initiates epigenetic-related mechanisms, including the reduction in hippocampal acetylation of some histones (H3K9/H4K8) and hypermethylation of Fkbp5, Grin2b, Bdnf, Era, and Kcc2 genes in the hippocampus or cerebral cortex. BPA also affects the mitochondrial pathways (hippocampal mitochondrial fragmentation and altered mitochondrial dynamics), increases calcium, and causes oxidative stress (decreased cell viability; increased expression of beta secretase (BACE)-1, amyloid protein precursor (APP), amyloid beta (Aβ) 1–42, and phosphorylated tau proteins (P-Tau). Additionally, BPA exposure increases the expression of proinflammatory cytokines such as IL-6, IL-1 b, and TNF-a, reduces the expression of anti-inflammatory IL-10, and induces the activation of extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and some other mitogen-activated protein kinase (MAPK) and nuclear factor (NF-kB) pathways (Inadera 2015; Rebolledo-Solleiro et al. 2021).
Several in vivo and in vitro models reported that natural compounds (vitamins A, C, and E, quercetin, lycopene, gallic acid, ginseng, Tualang honey) may alleviate BPA-induced toxicity (Amjad et al. 2020). Melatonin (MEL), secreted by the pineal gland in the brain, is known for its diverse functions, such as circadian rhythm, energy metabolism, and immune system regulator, and has been reported to exert neuroprotection due to its antioxidant and antiapoptotic effects (Lee et al. 2019; Rehman et al. 2019).
Considering that oxidative stress appears to be an important contributor to the neurotoxicity induced by BPA and that antioxidants, with remarkable neuroprotective effects, could play a valuable protective role, our study aimed to evaluate the effects of MEL preadministration on ambulatory activity, lipid peroxidation, inflammatory cytokines, ERK/NF-kB signaling pathway in the hippocampus and frontal lobe, and histopathological changes in the hippocampus of the BPA-treated rats.
Materials and Methods
Animals and Experimental Design
Experimental procedures were approved by the Animal Ethics Board of “Iuliu Hatieganu” University on animal welfare according to Directive 2010/63/EU on the protection of animals used for scientific purposes. Two-month-old male Wistar rats (n = 24) were used under standard laboratory conditions, housed in a 12 h light—12 h dark cycle at room temperature (24 ± 2 °C). The rats had free access to a standard normocaloric pellet diet and received water ad libitum. To evaluate the effect of MEL on ambulatory activity, markers of lipid peroxidation, inflammation, ERK/NF-kB signaling pathway, and histopathological changes in the brain of rats treated with bisphenol A (BPA), the animals were divided into 4 groups of 6 rats each (Fig. 1). One group consisted of untreated rats and served as control. The animals in groups 3 and 4 were pretreated with MEL, for 28 days, before BPA administration. MEL was administered orally in two doses: 20 mg/kg b.w. (MEL I group) and 40 mg/kg b.w (MEL II group). On the 29th day of the experiment, the animals in groups 2, 3, and 4 were given BPA (1 mg/kg b.w.).
Experimental design. Four groups of animals were orally treated with 20 mg/kg b.w. or 40 mg/kg b.w. MEL for 28 days. BPA (1 mg/kg b.w.) was administered on the 29th day. At the end of the experiment, behavioral tests were conducted (day 30). The hippocampus, the frontal lobe, and the cerebellum for the oxidative stress assays and ELISA test were harvested. Hippocampus fragments were taken for western blotting technique and conventional histopathology
On the 30ty day of the experiment, the behavioral tests were conducted, and then, under anesthesia with an intraperitoneal injection of ketamine/xylazine cocktail (90 mg/kg b.w. ketamine and 10 mg/kg b.w. xylazine), all animals were euthanized. The hippocampus, the frontal lobe, and the cerebellum were harvested for the oxidative stress assays and ELISA test. Additionally, hippocampus fragments were taken for western blotting technique and conventional histopathology.
Behavioral Testing
Two widely used tests to evaluate general locomotion and emotionality—like behavior in rodents—are the open field test (OFT) and the elevated plus maze (EPM). A visual tracking system (Smart Basic Software version 3.0 Panlab Harvard Apparatus), using specific mazes for rats (Ugo Basil Animal Mazes for Video-Tracking), recorded the animals’ behavior continuously for 5 min. In OFT, the total and peripheral traveled distance and number of entries are common measures for general locomotor activity. High center traveled distance and number of entries and high center time ratio (center/total time) are reported parameters of a low level of anxiety. Total and closed arm traveled distance and also the number of entries are variables of motor activity in EPM. High open-arm traveled distance and number of entries and high open-arms time ratio (open arms/total time) indicate low anxiety-like behavior. Between tasks, the mazes were cleaned with 70% ethanol to remove the residual odor (Gamberini et al. 2015; Sevastre Berghian et al. 2017; Walf and Frye 2007).
Biochemical Investigations of Oxidative Stress
For the oxidative stress evaluation, the malondialdehyde (MDA) was measured as a marker of lipid peroxidation from the hippocampus, frontal lobe, and cerebellum. The MDA levels were determined by spectrofluorimetry, using the 2-thiobarbituric acid method. The values were expressed as nmoles/mg of protein (Conti et al. 1991).
Quantitative Estimation of MAPK Level
The total p44/42 MAPK (ERK 1/2) protein level was evaluated by Path Scan Sandwich ELISA tests according to the manufacturer’s protocol (Cell Signaling Technology Inc.). Results were expressed in terms of OD units/mg protein of different treatment samples.
Evaluation of MCP1, γH2AX, NFkB, and pNFkB Proteins Expressions in Hippocampus
MCP1, γH2AX, NFkB, and pNFkB proteins quantification were performed by western blot technique. Lysates (20 µg protein/lane) were separated by electrophoresis on 8% SDS PAGE gels under reducing conditions, then transferred to polyvinylidenedifluoride membranes (BioRad), using Biorad Miniprotean system (BioRad). Blots were then blocked and incubated with antibodies against MCP1, γH2AX NFkB and phospho-NFkB, diluted 1:500 and corresponding secondary HRP-linked antibodies (1:1500). Proteins were visualized and detected using Supersignal West Femto Chemiluminescent substrate (Thermo Fisher Scientific, Rockford IL, USA) and a Gel Doc Imaging system equipped with a XRS camera and quantity one analysis software (Biorad). GAPDH was used as a protein loading control.
Histological Investigation of the Hippocampus
Hippocampus slices were harvested for histological investigation. Brain samples were fixed in 10% neutral buffered formalin, then embedded in paraffin in order to produce 5-mm thick sections which were stained with hematoxylin–eosin (HE) for light microscopy (Optika B-383LD2 microscope).
Statistical Analysis
All statistical analyses were conducted using ANOVA GraphPad Prism software, version 6.0 (GraphPad, San Diego, CA, USA), and SPSS v.11.5 for Windows. The results were expressed as the mean ± standard deviation (SD). One-way analysis of variance (ANOVA) was used, either followed by Tukey’s post hoc test, to determine statistically significant among four groups or followed by Bonferonni’s post hoc test, to determine statistically significant among two groups. A p-value lower than 0.05 was considered statistically significant.
Results
Behavioral Studies
The effect of melatonin preadministration on rat’s “locomotion, tested in OFT,” was illustrated in Fig. 2. Our results showed that BPA exerted an inhibitory effect on general locomotion. Even though MEL tended to maintain the general locomotion, there were no statistically significant differences between the groups.
The effects of MEL preadministration on total (A) and peripheral (B) traveled distance and total (C) and peripheral (D) number of entries in OFT in BPA-treated rats BPA administration significantly decreased the locomotor activity (the total distance (A), the distance in periphery (B), the total entries (C), and the entries in periphery (D)) compared to control group. Twenty-eight days of MEL treatment, before BPA administration, slightly improved the locomotor activity (total entries and entries in the periphery), but without a statistical significance (p > 0.05) compared to the BPA group (C, D). Each group consisted of 6 rats. Control vs BPA, #; BPA vs BPA + Mel 1,*; BPA vs BPA + Mel 2,*; BPA + Mel 1 vs BPA + Mel 2, α; results were expressed as mean ± SD; #,* α, p < 0.05; ##, **, α α, p < 0.01; ###, ***, ααα p < 0.001
The effect of MEL on rats’ locomotion, tested in EPM, was illustrated in Fig. 3. According to Walf and Frye (2007), EPM may be used to assess general locomotor activity levels (total and closed arms entries). In the EPM, MEL pretreatment tended to maintain general locomotion close to the control group, but without any statistical significance (p > 0.05). BPA-treated rats significantly made fewer entries in the EPM test as compared to the control group (p < 0.001 and p < 0.01).
The effects of MEL preadministration on the total (A) and peripheral (B) traveled distance and the total (C) and peripheral (D) number of entries in EPM. In the EPM, BPA-treated rats significantly made fewer entries (C, D) in the EPM test as compared to the control group (p < 0.001 and p < 0.01). MEL pretreatment tended to maintain general locomotion, but without any statistical significance (p > 0.05) (C, D). Each group consisted of 6 rats. Control vs BPA, #; BPA vs BPA + Mel 1,*; BPA vs BPA + Mel 2,*; BPA + Mel 1 vs BPA + Mel 2, α; results were expressed as mean ± SD; #,* α, p < 0.05; ##, **, α α, p < 0.01; ###, ***, ααα, p < 0.001
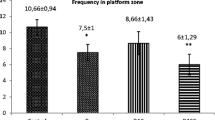
Regarding the emotionality (Fig. 4), our results showed that 28 days of MEL administration significantly reversed the inhibitory effect of BPA on central locomotion (the traveled distance in the center (A), the time spent in the center of the arena (C) in OFT (p < 0.001; p < 0.05), and the number of made entries in open arms (E) in EPM (BPA + MEL II vs BPA, p < 0.05). BPA significantly diminished the central locomotion both in OFT (A, C) and EPM (D, E, F) as compared to the control group (p < 0.001, p < 0.05 in OFT and EPM p < 0.01; p < 0.001 and p < 0.05).
The effects of MEL pretreatment on emotionality in OFT (A, B, C) and in EPM (D, E, F). In OFT, BPA exerted an inhibitory effect on the treated animals as compared to the control group (A, C). MEL-treated rats traveled a significantly greater distance (A) and spent more time (C), in the central part of the OFT arena as compared to the BPA group (BPA + MEL II vs BPA). In the EPM, the BPA group significantly traveled less (D), made fewer entries (E), and spent less time (F) in the open arms of the maze, as compared to the control. The BPA + MEL II group made significantly more entries in the open arms as compared to the BPA group (E). Each group consisted of 6 rats. Control vs BPA, #; BPA vs BPA + Mel 1,*; BPA vs BPA + Mel 2,*; BPA + Mel 1 vs BPA + Mel 2, α; results were expressed as mean ± SD; #,* α, p < 0.05; ##, **, α α, p < 0.01; ###, ***, ααα, p < 0.001
Oxidative Stress Assessment in Brain
MDA levels in the brain of rats treated with MEL before BPA administration were illustrated in Fig. 5. MDA displayed lower levels in the hippocampus (BPA + MEL II vs BPA, p < 0.05) and frontal lobe (BPA + MEL I vs BPA, p < 0.05) of the MEL-treated groups.
The effects of MEL preadministration on malondialdehyde (MDA) levels (A, B, C) in the hippocampus, frontal lobe, and cerebellum of BPA-treated rats both doses of MEL diminished the MDA in the hippocampus (BPA + MEL II vs BPA, p < 0.05), (A) and frontal lobe (BPA + MEL I vs BPA, p < 0.05) (B). Each group consisted of 6 rats. Control vs BPA, #; BPA vs BPA + Mel 1,*; BPA vs BPA + Mel 2,*; BPA + Mel 1 vs BPA + Mel 2, α; results were expressed as mean ± SD; #,* α, p < 0.05; ##, **, α α, p < 0.01; ###, ***, ααα, p < 0.001
The effects of MEL preadministration on the MAPK levels in the brain in different areas of the brain were exemplified in Fig. 6A–C. In the hippocampus and frontal lobe, BPA stimulated the MAPK activation (A, B) as compared to the control group (p < 0.01 and p < 0.05). Both MEL I and II doses diminished the MAPK levels in the hippocampus, as compared to BPA groups (p < 0.01) (A). In the frontal lobe, the MAPK levels were downregulated by MEL II treatment (p < 0.05) (B).
The effect of MEL preadministration on the MAPK levels in the brain, both in the hippocampus and frontal lobe, was that BPA administration significantly increased the MAPK protein as compared to the control group (BPA vs control, p < 0.01) in (A). In the hippocampus, MAPK level was significantly lower in the MEL-treated groups as compared to BPA (BPA + MEL I/ BPA + MEL II vs BPA, p < 0.01; A). In the frontal lobe, BPA and MEL II treatment reduced the MAPK activation (BPA + MEL II vs BPA p < 0.05; (B). Each group consisted of 6 rats. Control vs BPA, #; BPA vs BPA + Mel 1,*; BPA vs BPA + Mel 2,*; BPA + Mel 1 vs BPA + Mel 2, α; results were expressed as mean ± SD; #,* α, p < 0.05; ##, **, α α, p < 0.01; ###, ***, ααα, p < 0.001
The effects of MEL preadministration on the expression of MCP1, γH2AX, NFkB, and pNFkB proteins in the hippocampus were exemplified in Fig. 7. MCP1 expression, measured by western blot, decreased in the BPA group and BPA + MEL II groups (p < 0.001) compared to control and increased significantly in BPA + MEL I group compared to BPA (p < 0.001, B). Both doses of MEL significantly decreased the γH2AX expression (BPA + MEL I vs BPA, p < 0.01; BPA + MEL II vs BPA, p < 0.05; C). The NFkB (p < 0.001) and pNFkB (p < 0.001) protein expression was significantly upregulated by both MEL I and MEL II treatment as compared to BPA (D, E). BPA administration significantly increased the expression of pNFkB (p < 0.001) as compared to control, in the hippocampus (E). MEL II increased the NFkB expression in comparison to MEL I (D).
The effects of MEL preadministration on the expression of MCP1, γH2AX, NFkB, and pNFkB in the hippocampus. Expression of MCP1, γH2AX, NF-kB, and pNF-kB in the hippocampus were analyzed by western blot (WB) (A). Image analysis of western blot bands was done by densitometry; results were normalized to GAPDH (B, C, D, E). Each group consisted of 3 samples. Control vs BPA, #; BPA vs BPA + Mel 1,*; BPA vs BPA + Mel 2,*; BPA + Mel 1 vs BPA + Mel 2, α; results were expressed as mean ± SD; #,* α, p < 0.05; ##, **, α α, p < 0.01; ###, ***, ααα, p < 0.001
Histopathological analysis of the hippocampus showed that BPA-treated groups presented cellular edema, necrosis, and polymorphic cellular inflammatory infiltrate that enlarge the intercellular spaces. MEL I and MEL II administration diminished the cellular edema and necrosis and reduced the inflammatory cell formation, but without any statistical significance between the groups (Fig. 8). The histological subtle changes can be difficult to define between the groups; therefore, more sensitive visualization methods of the neuronal death induced by the administration of BPA may be necessary in this context.
Representative photomicrographs of the hippocampus of the four experimental groups. A, B, C, and D showed the histological features of the CA3 field in the hippocampus (the first column—I) and micromorphology (the second column—II) in the same experimental conditions for the four groups. Magnification: × 200. H&E staining. Scale bar = 20 µm
Discussions
BPA, a synthetic compound with estrogenic endocrine activity, is widely used in the manufacture of polycarbonate plastics and epoxy resins. There is scientific evidence that humans are continuously exposed to this chemical. Some in vivo and in vitro studies suggest that BPA accumulates in various tissues (brain, heart, liver, pancreas, testis), thus causing diseases, both in humans and animals (Amjad et al. 2020; Kobroob et al. 2018; Mączka et al. 2022). Some studies have stated the link between oxidative stress and the negative effect of BPA (Babu et al. 2013; Hassan et al. 2012; Kobroob et al. 2018). Other papers indicated that BPA can alter neurogenesis, therefore representing a risk factor for neurological disorders and cognitive impairments in humans (Ishtiaq et al. 2021; Negri-Cesi 2015).
BPA may induce neurotoxicity by several mechanisms: it reduces synaptic plasticity, inhibits neurogenesis, generates oxidative stress, and induces autophagy and apoptosis. There are experimental research data sustaining that BPA may suppress neuroepithelial progenitor cells proliferation and thus, affecting the normal dentate gyrus (DG) formation, or may induce apoptotic cell death in the DG, hilus, and molecular layer of the hippocampus, by enhanced expression of the autophagy proteins (Agarwal et al. 2015; Kim et al. 2009; Li et al. 2018; Santoro et al. 2019). Therefore, in this particular study, we have chosen a chemical model to induce experimental neurotoxicity in animals, such as BPA. Moreover, in 2021, the European Food Safety Authority’s (EFSA’s) expert panel on food contact materials, enzymes, and processing aids (CEP) will have established a tolerable daily intake (TDI) of 0.04 ng/kg b.w./day for BPA (https://www.efsa.europa.eu/en/news/bisphenol-efsa-draft-opinion-proposes-lowering-tolerable-daily-intake).
In addition, to limit the BPA intake, current protection strategies could include the use of compounds with known neuroprotective effects such as natural compounds, including MEL. Our results demonstrated that MEL, especially in high dose, improved the emotionality of animals, reduced oxidative stress, and MAPK levels, decreased DNA damage, and upregulated the NFkB and the pNFkB expressions in the hippocampus.
In the present research, we provide evidence that BPA administration (1 mg/kg b.w.) induced redox imbalance. Thus, we noticed increased amounts of MDA in the hippocampus and frontal lobe. These observations are consistent with the literature. Several studies reported that BPA enhanced nitric oxide levels and protein carbonyl content, decreased glutathione (GSH), as well as decreased antioxidant enzymatic activity (glutathione S-transferase (GST), glutathione peroxidase (GPx), superoxide dismutase enzyme (SOD), catalase (CAT)) in the kidneys, pancreas or blood, in animal models (Kobroob et al. 2018; Mączka et al. 2022). Oxidative stress, a result of an imbalance between reactive oxygen species (ROS) generation and antioxidant systems, may have a strong, negative impact on central nervous system functions. As known, the brain tissue is highly vulnerable to oxidative stress, due to its high oxygen consumption and lipid-rich content. Therefore, oxidative damage may be an essential factor in the onset of disorders associated with glial cell injuries and neuronal damage (Aranarochana et al. 2021; Galano et al. 2018; Salim 2017).
So, based on the above-mentioned data, the comparative effects of two doses of MEL (20 mg/kg b.w. and 40 mg/kg b.w.) on the BPA effect were considered. MEL doses were chosen based on previously published data (Chabra et al. 2014; Tavakoli et al. 2022). As MEL is reported to be a potent neuroprotective molecule, due to its antioxidant, anti‐excitotoxic, anti‐inflammatory, and anti‐misfolding effects, we have chosen to test its ability to counteract the BPA’s effect (Alghamdi 2018; Lee et al. 2019).
In our study, MEL II diminished lipid peroxidation in the hippocampus, whereas MEL I exerted protective effects in the frontal lobe of the BPA-treated rats, data which are comparable with other reports. Mączka et al. (2022) reported the efficiency of antioxidants, such as curcumin, lycopene, luteolin, and melatonin on various organs (liver, lungs, brain, and prostate) by modulation of the ROS, mitochondrial dysfunction, and cell signaling pathways. The positive impact of MEL as an antioxidant has been deeply documented in the literature. Some authors consider that MEL can exert its antioxidant activity directly, by scavenging free radicals (⋅OH, alkoxy radicals (RO⋅), peroxy radicals (ROO⋅), and ⋅NO, hydrogen peroxide (H2O2), singlet oxygen (1O2), and ONOO−)) and indirectly by inhibiting metal-induced DNA damage (chelating several metal ions: iron, copper, aluminum, lead, cadmium, and zinc, and thus preventing •OH generation) or by protection through its metabolites (N-acetylserotonin, N1-acetyl-N2-formyl-5-methoxykynuramine, N1-acetyl-5-methoxykynuramine, cyclic 3-hydroxymelatonin, 6-hydroxymelatonin, 4-hydroxymelatonin, and 2-hydroxymelatonin). MEL can also act by activating antioxidative enzymes (CAT, GPx, and SOD) and inhibiting pro-oxidant enzymes (xanthine oxidase), or by reducing DNA damage (Davanipour et al. 2009; Galano et al. 2018; Wu et al. 2012).
Accordingly, some authors sustained the beneficial effect of MEL on BPA-treated rats by increased antioxidant enzymes activity (SOD, CAT, ascorbate peroxidase, Px), and by attenuated brain apoptosis (normalized p53, p53 upregulated modulator of apoptosis (PUMA), and dynamin-related protein 1 (Drp-1) expression), both at the transcriptional and translational levels (Ishtiaq et al. 2021; Mączka et al. 2022). Apart from these mechanisms, the MEL’s antioxidant–receptor-dependent mechanisms have also been also mentioned (Hardeland 2019; Xia et al. 2012). Similarly, Won et al. (2021) mentioned that MEL decreased oxidative stress damage and reduced Nox2 and Nox4 expression via MT2 receptors (Won et al. 2021). MEL can exert its effects after binding to MEL receptors, T1 (MT1) and T2 (MT2), broadly distributed in the nervous system, such as in the neurons and glial cells of CA3 subfield of the hippocampus, cerebral cortex, cerebellar cortex, thalamus, or pineal gland (Won et al. 2021). Based on the various distribution of the MEL receptors and different expression profiles of signal transduction pathways, in diverse tissues and cell types, the rapid effect of MEL, such as antioxidant activity and cell signaling, may differ, depending on the target tissue (Lee et al. 2019; Yapislar et al. 2022). Hence, MEL’s neuroprotective action may be explained by its antioxidant effect (Lee et al. 2019; Won et al. 2021).
As oxidative stress is reported to trigger neuroinflammation, we evaluated the MAPK levels in various brain areas and the expression of NFkB, pNFkB, and MCP1 in the hippocampus of the rats. In our study, one dose of BPA increased the MAPK (ERK ½) levels, both in the hippocampus and frontal lobe, along with the activation of pNFkB in the hippocampus, as compared to the control group. Furthermore, MEL diminished the MAPK levels, in the hippocampus and frontal lobe of BPA-treated rats. However, in the hippocampus, our results showed the excitatory effect of MEL upon NFkB, pNFkB activity, and MCP 1 expression. Contrarily, some earlier reports have provided evidence that MEL reduced the secretion of pro-inflammatory cytokines (IL-6, TNF-α, CRP, and IL-1β), thus modulating the inflammatory response in the central nervous system (Favrais et al. 2021; Madhu et al. 2021; Yapislar et al. 2022). Monocyte chemoattractant protein-1 (MCP1), expressed by neurons, astrocytes, microglia, and capillary endothelium in the brain, may alter the permeability of blood–brain barrier (BBB) and modulate various neuronal lesions (excitotoxic injury, ischemia, or hemorrhage) (Yao and Tsirka 2014). The discordant effect of MEL on MCP1 expression is dose-dependent. The higher the dose of Mel, the lower the secretion of MCP1.
Nuclear factor-κB consists of a family of transcription factors, highly involved in synaptic processes, neurotransmission, neuroprotection, brain inflammation, or neural stem cell proliferation (Mattson and Meffert 2006). In CNS, various factors, such as inflammatory cytokines, antigen receptor engagement, UV- or γ-irradiation, ischemia, hyperosmotic shock, or oxidative stress, can activate the NFkB factor, thus allowing the cells to adapt to the ongoing changing conditions (Oeckinghaus and Ghosh 2009). Some authors indicated that constitutively activated NFkB is found mostly in glutamatergic neurons of the CNS (layers 2, 4, and 5 of the cerebral cortex, granule cells, and pyramidal neurons of the hippocampus in the CA1 and CA3 areas, amygdala, cerebellum, hypothalamus, and olfactory lobes), but in the glial cells and cerebral blood vessels as well (Kaltschmidt and Kaltschmidt 2009; Schmidt-Ullrich et al. 1996; Shih et al. 2015). Solid evidence suggested that the transcription factor NFkB may exert promoting or suppressive functions in a cell- and tissue-dependent context, such as NFkB inhibition in glia may ameliorate disease while its activation in neurons may improve memory (Kaltschmidt and Kaltschmidt 2009; Markopoulos et al. 2018). Therefore, the contradictory findings of our study can be partially explained by the vast cell-type heterogeneity within the CNS and the interplay between cell-type specific roles of NFkB (Dresselhaus and Meffert 2019).
Numerous authors reported that MEL administration reduced the expression of NFkB in various organs or cells (kidneys, liver, lungs, heart, sciatic nerve, testicular cells, macrophages, T cells, neuronal tissue, and cell culture) (Cristofanon et al. 2009; Guo et al. 2017; Li et al. 2009; Negi et al. 2011). Moreover, it is likely that MEL may inhibit the NFkB expression by p38MAPK signaling pathway suppression and antioxidants upregulation. Furthermore, MEL is indicated to inhibit the transcriptional activation of TNF-α and IL1β, by blocking NFkB binding to DNA (Bantounou et al. 2022; Yapislar et al. 2022). Conversely, other studies indicated the stimulatory effect of MEL on NFkB in U937 cells, a lineage derived from monocytic human cells. In respect of the above-mentioned, the dual effect, both inhibitory and stimulatory, of MEL on NFkB in various cell types, depending on the quantification moment or experimental design, is hypothesized (Dresselhaus and Meffert 2019; Markus et al. 2013; Pugazhenthi et al. 2008; Yapislar et al. 2022). Therefore, the specific functions of NFkB in the nervous system and in neuroinflammation remain to be fully understood.
Exposure to BPA can also lead to DNA damage, which is believed to be mediated by increased free radicals. Therefore, γH2AX expression in the hippocampus of the rats was additionally evaluated (Wu et al. 2012). In our study, MEL I and MEL II significantly downregulated the expressions of γH2AX in the hippocampus of the BPA-treated groups suggesting protective effects on DNA damage induction. Gamma H2A histone family member X (γH2AX), a phosphorylated H2AX on serine 139, is a marker of DNA double-strand breaks (DS) in non-neuronal cells and in immature neurons (Crowe et al. 2011). γH2AX induction is associated with exposure of cells to cigarette smoke, polycyclic aromatic compounds, dinitrobenzo[e] pyrene, norethindrone, chromium, crude oil, electromagnetic fields, microwaves from mobile phones, or extreme heat (Dickey et al. 2009). In the CNS, γH2AX is involved both in the proliferation and apoptosis of neuronal precursors. Furthermore, γH2AX may also play a role in various neuropsychological disorders (neurotoxicity induced by glutamate receptor activation, in seizures, in Alzheimer’s disease, in Huntington’s disease, in depression-related cellular senescence, or in the regulation of necrosis in glioblastoma after irradiation (Merighi et al. 2021; Tang et al. 2021). Merighi et al. (2021) detected high levels of γH2AX, particularly in the subventricular zone of the lateral ventricles, the rostral migratory stream, the olfactory bulb or cerebellum, the prefrontal cortex, and the hippocampus, known as classical neurogenetic areas. Based on the literature, neurotoxic substances and oxidative stress induce γ phosphorylation of H2AX in the nervous system (Merighi et al. 2021). Moreover, oxidative stress-induced DNA damage has been identified as an important factor to neurodegeneration. Therefore, MEL’s beneficial effect against oxidative stress-induced DNA damage may be explained by its antioxidant activity (Galano et al. 2018).
Regarding the behavioral tests, our findings showed that BPA significantly decreased general, peripheral, and central locomotion, both in OFT and EPM tests. MEL II administration demonstrated an anxiolytic-like effect in OFT as it enhanced the traveled distance and the time spent in the central part of the arena. Additionally, MEL II improved the traveled central traveled distance as compared to the MEL I group, in OFT. Furthermore, the MEL I-treated rats made more entries in the open arms of the EPM as compared to BPA treated group. Our results are in agreement with previously published data (Fan et al. 2018). On the other hand, Mahdavinia et al. (2019) reported no effect of chronic BPA administration on locomotor activity in comparison with the control rats (Mahdavinia et al. 2019). Hence, MEL’s neuroprotective action may be explained by its antioxidant effect. Histopathologically, no significant microscopic differences were found in all groups. However, cellular edema, necrosis, and polymorphic cellular inflammatory infiltrate that enlarge the intercellular spaces were predominantly found in BPA-treated animals while MEL I and MEL II diminished the cellular changes.
In conclusion, MEL diminished the MDA and the MAPKs levels, both in the hippocampus and frontal lobe, downregulated the expressions of γH2AX and MCP1, upregulated the NFkB and the pNFkB expressions in the hippocampus, improved the central locomotion both in OFT and EPM. Thus, the present study provides evidence about the neuroprotective effect of MEL against BPA-induced toxicity, at least partially explained by diminished lipid peroxidation, cell signaling, and immune response modulation. MEL can also mediate the neuroprotection against BPA-induced neurotoxicity by improving behavioral changes suggesting a real potential as a protective agent in brain toxicity.
Availability of Data and Materials
All data and materials are available on the authors.
References
Agarwal S, Tiwari SK, Seth B et al (2015) Activation of autophagic flux against xenoestrogen bisphenol-A-induced hippocampal neurodegeneration via AMP kinase (AMPK)/mammalian target of Rapamycin (mTOR) pathways. J Biol Chem 290(34):21163–21184. https://doi.org/10.1074/jbc.M115.6489987
Alghamdi BS (2018) The neuroprotective role of melatonin in neurological disorders. J Neurosci Res 96(7):1136–1149. https://doi.org/10.1002/jnr.24220
Ali et al (2017) Protection against neurobehavioral changes induced by bisphenol a during development in rats. Res Rev Neurosci 2:1–21
Amjad S, Rahman MS, Pang MG (2020) Role of antioxidants in alleviating bisphenol a toxicity. Biomolecules 10(8):1105. https://doi.org/10.3390/biom10081105
Aranarochana A, Sirichoat A, Pannangrong W, Wigmore P, Welbat JU (2021) Melatonin ameliorates valproic acid-induced neurogenesis impairment: the role of oxidative stress in adult rats. Oxid Med Cell Longev 2021:9997582. https://doi.org/10.1155/2021/9997582
Babu S, Uppu S, Claville MO, Uppu RM (2013) Prooxidant actions of bisphenol A (BPA) phenoxyl radicals: implications to BPA-related oxidative stress and toxicity. Toxicol Mech Methods 23(4):273–280. https://doi.org/10.3109/15376516.2012.753969. Epub 2013 Jan 18 PMID: 23193990
Bantounou M, Plascevic J, Galley HF (2022) Melatonin and related compounds: antioxidant and anti-inflammatory actions. Antioxidants 11:532. https://doi.org/10.3390/antiox11030532
Bittner GD, Yang CZ, Stoner MA (2014) Estrogenic chemicals often leach from BPA-free plastic products that are replacements for BPA-containing polycarbonate products. Environ Health 13(1):41. https://doi.org/10.1186/1476-069X-13-41. PMID:24886603
Carr RL, Bertasi FR, Betancourt AM, Bowers SD, Gandy BS, Ryan PL, Willard ST (2003) Effect of neonatal rat bisphenol a exposure on performance in the morris water maze. J Toxicol Environ Heal – Part A. https://doi.org/10.1080/71385398
Chabra A, Shokrzadeh M, Naghshvar F, Salehi F, Ahmadi A (2014) Melatonin ameliorates oxidative stress and reproductive toxicity induced by cyclophosphamide in male mice. Hum Exp Toxicol. https://doi.org/10.1177/0960327113489052
Chouhan S, Yadav SK, Prakash J et al (2014) Effect of Bisphenol A on human health and its degradation by microorganisms: a review. Ann Microbiol 64:13–21. https://doi.org/10.1007/s13213-013-0649-2
Conti M, Morand PC, Levillain P, Lemonnier A (1991) Improved fluorometric determination of malonaldehyde. Clin Chem 37(7):1273–1275
Cristofanon S, Uguccioni F, Cerella C, Radogna F, Dicato M, Ghibelli L, Diederich M (2009) Intracellular prooxidant activity of melatonin induces a survival pathway involving NF-kappaB activation. Ann N Y Acad Sci 1171:472–478
Crowe S et al (2011) Phosphorylation of histone H2A.X as an early marker of neuronal endangerment following seizures in the adult rat brain. J Neurosci 31(21):7648–7656. https://doi.org/10.1523/JNEUROSCI.0092-11.2011
Davanipour Z, Poulsen HE, Weimann A, Sobel E (2009) Endogenous melatonin and oxidatively damaged guanine in DNA. BMC Endocr Disord 9:22. https://doi.org/10.1186/1472-6823-9-22
Dickey JS, Redon CE, Nakamura AJ, Baird BJ, Sedelnikova OA, Bonner WM (2009) H2AX: functional roles and potential applications. Chromosoma 118(6):683–692. https://doi.org/10.1007/s00412-009-0234-4
Dresselhaus EC, Meffert MK (2019) Cellular specificity of NF-κB function in the nervous system. Front Immunol 10:1043. https://doi.org/10.3389/fimmu.2019.01043
Fan Y, Tian C, Liu Q, Zhen X, Zhang H, Zhou L, Li T, Zhang Y, Ding S, He D, Jin X, Liu J, Zhang B, Wu N, Manyande A, Zhu M (2018) Preconception paternal bisphenol A exposure induces sex-specific anxiety and depression behaviors in adult rats. PLoS ONE 13(2):e0192434. https://doi.org/10.1371/journal.pone.0192434
Favrais G, Saliba E, Savary L et al (2021) Partial protective effects of melatonin on developing brain in a rat model of chorioamnionitis. Sci Rep 11:22167. https://doi.org/10.1038/s41598-021-01746-w
Galano A, Tan DX, Reiter RJ (2018) Melatonin: a versatile protector against oxidative DNA damage. Molecules 23(3):530. https://doi.org/10.3390/molecules23030530
Gamberini MT, Rodrigues DS, Rodrigues D, Pontes CV (2015) Effects of the aqueous extract of Pimpinella anisum L. seeds on exploratory activity and emotional behavior in rats using the open field and elevated plus maze tests. J Ethnopharmacol 168:45–49
Guo Y, Sun J, Li T, Zhang Q, Bu S, Wang Q, Lai D (2017) Melatonin ameliorates restraint stress-induced oxidative stress and apoptosis in testicular cells via NF-κB/iNOS and Nrf2/ HO-1 signaling pathway. Sci Rep 7(1):9599. https://doi.org/10.1038/s41598-017-09943-2
Hardeland R (2019) Aging, melatonin, and the pro- and anti-inflammatory networks. Int J Mol Sci 20:1223
Hass AM, Christiansen S, Boberg J, Rasmussen MG, Mandrup K (2016) Low-dose effect of developmental bisphenol A exposure on sperm count and behaviour in rats. Andrology. https://doi.org/10.1111/andr.12176
Hassan ZK, Elobeid MA, Virk P, Omer SA, ElAmin M, Daghestani MH, AlOlayan EM (2012) Bisphenol A induces hepatotoxicity through oxidative stress in rat model. Oxid Med Cell Longev 2012:194829. https://doi.org/10.1155/2012/194829
Homberg R et al (2016) Understanding autism and other neurodevelopmental disorders through experimental translational neurobehavioral models. Neurosci Biobehav Rev 65:292–312. https://doi.org/10.1016/j.neubiorev.2016.03.013. https://www.efsa.europa.eu/en/news/bisphenol-efsa-draft-opinion-proposes-lowering-tolerable-daily-intake
Inadera H (2015) Neurological effects of bisphenol A and its analogues. Int J Med Sci 12(12):926–936. https://doi.org/10.7150/ijms.13267
Ishido M, Masuo Y (2014) Temporal effects of bisphenol A on dopaminergic neurons: an experiment on adult rats. Open Environ Sci 8:9–17. https://doi.org/10.2174/1876325101408010009
Ishtiaq A, Ali T, Bakhtiar A, Bibi R, Bibi K, Mushtaq I, Li S, Khan W, Khan U, Anis RA, Anees M, Sultan A, Murtaza I (2021) Melatonin abated bisphenol A-induced neurotoxicity via p53/PUMA/Drp-1 signaling. Environ Sci Pollut Res Int 28(14):17789–17801. https://doi.org/10.1007/s11356-020-12129-5
Kaltschmidt B, Kaltschmidt C (2009) NF-kappaB in the nervous system. Cold Spring Harb Perspect Biol 1(3):a001271. https://doi.org/10.1101/cshperspect.a001271. Erratum.In:ColdSpringHarbPerspectBiol.2010Jan;2(1):a001271
Kim K, Son TG, Park HR, Kim SJ, Kim HS, Kim HS, Kim TS, Jung KK, Han SY, Lee J (2009) Potencies of bisphenol A on the neuronal differentiation and hippocampal neurogenesis. J Toxicol Environ Health A 72(21–22):1343–1351. https://doi.org/10.1080/15287390903212501
Kobroob A, Peerapanyasut W, Chattipakorn N, Wongmekiat O (2018) Damaging effects of bisphenol A on the kidney and the protection by melatonin: emerging evidences from in vivo and in vitro studies. Oxid Med Cell Longev 2018:3082438. https://doi.org/10.1155/2018/3082438
Lee JG, Woo YS, Park SW, Seog DH, Seo MK, Bahk WM (2019) The neuroprotective effects of melatonin: possible role in the pathophysiology of neuropsychiatric disease. Brain Sci 9(10):285. https://doi.org/10.3390/brainsci9100285. Erratum.In:BrainSci25;9(12)
Li Z, Nickkholgh A, Yi X, Bruns H, Gross ML, Hoffmann K, Mohr E, Zorn M, Büchler MW, Schemmer P (2009) Melatonin protects kidney grafts from ischemia/reperfusion injury through inhibition of NF-kB and apoptosis after experimental kidney transplantation. J Pineal Res 46(4):365–372. https://doi.org/10.1111/j.1600-079X.2009.00672.x
Li Z, Zhao K, Lv X, Lan Y, Hu S, Shi J, Guan J, Yang Y, Lu H, He H, Gao F, He W (2018) Ulk1 governs nerve growth factor/trka signaling by mediating Rab5 GTPase activation in porcine hemagglutinating encephalomyelitis virus-induced neurodegenerative disorders. J Virol 92(16):e00325–e18. https://doi.org/10.1128/JVI.00325-18
Mączka W, Grabarczyk M, Wińska K (2022) Can antioxidants reduce the toxicity of bisphenol? Antioxidants (Basel) 11(2):413. https://doi.org/10.3390/antiox11020413
Madhu LN, Kodali M, Attaluri S, Shuai B, Melissari L, Rao X, Shetty AK (2021) Melatonin improves brain function in a model of chronic Gulf War illness with modulation of oxidative stress, NLRP3 inflammasomes, and BDNF-ERK-CREB pathway in the hippocampus. Redox Biol 43:101973
Mahdavinia M, Ahangarpour A, Zeidooni L, Samimi A, Alizadeh S, Dehghani MA, Alboghobeish S (2019) Protective effect of Naringin on bisphenol A-induced cognitive dysfunction and oxidative damage in rats. Int J Mol Cell Med 8(2):141–153. https://doi.org/10.22088/IJMCM.BUMS.8.2.141
Markopoulos GS, Roupakia E, Tokamani M, Alabasi G, Sandaltzopoulos R, Marcu KB, Kolettas E (2018) Roles of NF-κB signaling in the regulation of miRNAs impacting on inflammation in cancer. Biomedicines 6:40. https://doi.org/10.3390/biomedicines6020040
Markus RP, Cecon E, Pires-Lapa MA (2013) Immune-pineal axis: nuclear factor κB (NF-kB) mediates the shift in the melatonin source from pinealocytes to immune competent cells. Int J Mol Sci 14(6):10979–10997. https://doi.org/10.3390/ijms140610979. PMID:23708099
Mattson M, Meffert M (2006) Roles for NF-κB in nerve cell survival, plasticity, and disease. Cell Death Differ 13:852–860. https://doi.org/10.1038/sj.cdd.4401837
Merighi A, Gionchiglia N, Granato A, Lossi L (2021) The phosphorylated form of the histone H2AX (γH2AX) in the brain from embryonic life to old age. Molecules 26(23):7198. https://doi.org/10.3390/molecules26237198
Morrice JR, Gregory-Evans CY, Shaw CA (2006) Modeling environmentally-induced motor neuron degeneration in zebrafish. Sci Rep 8:4890. https://doi.org/10.1038/s41598-018-23018-w
Nakamura K, Itoh K, Yaoi T, Fujiwara Y, Sugimoto T, Fushiki S (2006) Murine neocortical histogenesis is perturbed by prenatal exposure to low doses of bisphenol A. J Neurosci Res 84(6):1197–1205. https://doi.org/10.1002/jnr.21020
Negi G, Kumar A, Sharma SS (2011) Melatonin modulates neuroinflammation and oxidative stress in experimental diabetic neuropathy: effects on NF-κB and Nrf2 cascades. J Pineal Res 50(2):124–131. https://doi.org/10.1111/j.1600-079X.2010.00821
Negri-Cesi P (2015) Bisphenol a interaction with brain development and functions. Dose Response 13(2):1559325815590394. https://doi.org/10.1177/1559325815590394
Oeckinghaus A, Ghosh S (2009) The NF-kappaB family of transcription factors and its regulation. Cold Spring Harb Perspect Biol 1(4):a000034. https://doi.org/10.1101/cshperspect.a000034
Pugazhenthi K, Kapoor M, Clarkson AN, Hall I (2008) Appleton I. Melatonin accelerates the process of wound repair in full-thickness incisional wounds. J Pineal Res 44:387–396
Rebolledo-Solleiro D, Castillo Flores LY, Solleiro-Villavicencio H (2021) Impact of BPA on behavior, neurodevelopment and neurodegeneration. Front Biosci (Landmark Ed) 26(2):363–400. https://doi.org/10.2741/4898
Rehman SU, Ikram M, Ullah N et al (2019) Neurological enhancement effects of melatonin against brain injury-induced oxidative stress, neuroinflammation, and neurodegeneration via AMPK/CREB signaling. Cells 8(7):760. https://doi.org/10.3390/cells8070760
Rochester JR (2013) Bisphenol A and human health: a review of the literature. Reprod Toxicol 42:132–155
Salim S (2017) Oxidative stress and the central nervous system. J Pharmacol Exp Ther 360(1):201–205. https://doi.org/10.1124/jpet.116.237503
Santoro A, Chianese R, Troisi J, Richards S, Nori SL, Fasano S, Guida M, Plunk E, Viggiano A, Pierantoni R, Meccariello R (2019) Neuro-toxic and reproductive effects of BPA. Curr Neuropharmacol 17(12):1109–1132. https://doi.org/10.2174/1570159X17666190726112101. PMID:31362658; PMCID:PMC7057208
Schmidt-Ullrich R, Memet S, Lilienbaum A, Feuillard J, Raphael M, Israel A (1996) NF-kappaB activity in transgenic mice: developmental regulation and tissue specificity. Development 122:2117–2128. https://doi.org/10.1101/cshperspect.a001271
Sevastre Berghian A et al (2017), Curcumin reverses the Diazepam-induced cognitive impairment by modulation of oxidative stress and ERK 1/2/NF-κB pathway in brain. Oxid Med Cell Longev 2017:16. https://doi.org/10.1155/2017/3037876
Shafei A, Matbouly M, Mostafa E et al (2018) Stop eating plastic, molecular signaling of bisphenol A in breast cancer. Environ Sci Pollut Res 25:23624–23630. https://doi.org/10.1007/s11356-018-2540-y
Shih RH, Wang CY, Yang CM (2015) NF-kappaB signaling pathways in neurological inflammation: a mini review. Front Mol Neurosci 8:77. https://doi.org/10.3389/fnmol.2015.00077
Tang FR, Liu L, Wang H, Ho KJN, Sethi G (2021) Spatiotemporal dynamics of γH2AX in the mouse brain after acute irradiation at different postnatal days with special reference to the dentate gyrus of the hippocampus. Aging (Albany NY) 13(12):15815–15832. https://doi.org/10.18632/aging.203202
Tavakoli M et al (2022) Protective effect of melatonin on nonylphenol-induced reproductive and behavioral disorders in first-generation adult male rats. Behav Neurol 2022(1877761):13. https://doi.org/10.1155/2022/1877761
Walf A, Frye CA (2007) The use of the elevated plus maze as an assay of anxiety-related behavior in rodents. Nat Protoc 2(2):322–328
Won E, Na KS, Kim YK (2021) Associations between melatonin, neuroinflammation, and brain alterations in depression. Int J Mol Sci 23(1):305. https://doi.org/10.3390/ijms23010305
Wu ZH, Zhang H, Wang XY, Yang R, Liu B, Liu Y, Zhao WP, Feng HY, Xue LG, Hao JF, Niu BT, Wang ZH (2012) Protective effects of melatonin against12C6+beam irradiation-induced oxidative stress and DNA injury in the mouse brain. Adv Space Res 49:196–203. https://doi.org/10.1016/j.asr.2011.09.007
Xia MZ, Liang YL, Wang H, Chen X, Huang YY et al (2012) Melatonin modulates TLR4-mediated inflammatory genes through MyD88- and TRIF-dependent signaling pathways in lipopolysaccharide-stimulated RAW264.7 cells. J Pineal Res 53:325–334
Yao Y, Tsirka SE (2014) Monocyte chemoattractant protein-1 and the blood-brain barrier. Cell Mol Life Sci 71(4):683–697
Yapislar H, Haciosmanoglu E, Sarioglu T, Degirmencioglu S, Sogut I, Poteser M, Ekmekcioglu C (2022) AntiInflammatory effects of melatonin in rats with induced type 2 diabetes mellitus. Life 12:574. https://doi.org/10.3390/life12040574
Acknowledgements
We thank Mr. Remus Moldovan for handling the animals and Mrs. Nicoleta Decea for the biochemical analysis.
Funding
The present work received financial support through the grant of the Ministry of Research, Innovation and Digitization, CNCS—UEFISCDI, project number PN-III-P1-1.1-TE-2021–0159, within PNCDI III (TE60/2022).
Author information
Authors and Affiliations
Contributions
ACSB and GAF wrote the main manuscript, contributed to acquisition, analysis, or interpretation of data; CC performed the experiments and statistical data analysis; DG and LR performed the histopathological analysis, and MCOVV, DO, and IB made western blot investigation and critically revised the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Experimental procedures were approved by the Animal Ethics Board of “Iuliu Hatieganu” University on animal welfare according to Directive 2010/63/EU on the protection of animals used for scientific purposes.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sevastre-Berghian, A.C., Casandra, C., Gheban, D. et al. Neurotoxicity of Bisphenol A and the Impact of Melatonin Administration on Oxidative Stress, ERK/NF-kB Signaling Pathway, and Behavior in Rats. Neurotox Res 40, 1882–1894 (2022). https://doi.org/10.1007/s12640-022-00618-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-022-00618-z