Abstract
Organophosphorus nerve agents (NAs) irreversibly inhibit acetylcholinesterase, which results in the accumulation of acetylcholine and widespread excitotoxic seizure activity. Because current medical countermeasures (anticholinergics, AChE reactivators, and benzodiazepines) lack sufficient anti-seizure efficacy when treatment is delayed, those intoxicated are at risk for severe brain damage or death if treatment is not immediately available. Toward developing a more effective anti-seizure treatment for NA intoxication, this study evaluated the efficacy of A1 adenosine (ADO) receptor (A1AR) agonists in a rat soman seizure model. One minute after exposure to soman (1.6 × LD50, subcutaneous), rats were treated intraperitoneally with one of the following agonists at increasing dose levels until anti-seizure efficacy was achieved: N6-cyclopentaladenosine (CPA), 2-chloro-N6-cyclopentyladenosine (CCPA), and (±)-5'-chloro-5′-deoxy-ENBA (ENBA). All A1AR agonists were efficacious in preventing seizure and promoting survival. The effective doses for the A1AR agonists were 60 mg/kg CPA, 36 mg/kg CCPA, and 62 mg/kg ENBA. Whereas vehicle-treated rats experienced 100% seizure and 21% survival (N = 28), ADO treatments reduced seizure occurrence and improved survival rates: 8% seizure and 83% survival with CPA (60 mg/kg, N = 12), 17% seizure and 75% survival with CCPA (36 mg/kg, N = 12), and 8% seizure, 83% survival with ENBA (62 mg/kg, N = 12). The brains of ADO-treated rats were also protected from damage as indicated by neurohistopathological analysis. While all ADO agonists provided neuroprotection, rats receiving CCPA and ENBA experienced less severe ADO-induced side effects (e.g., sedation, hypothermia, bradycardia) than with CPA. The data from this study suggest that the ADO signaling pathway is a promising mechanism for countering seizure activity induced by NAs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
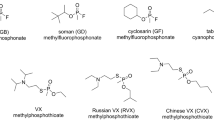
Exposure to an organophosphorus nerve agent (NA), such as soman (also known as GD), initiates a cascade of biochemical events that eventually leads to severe brain damage or death. The primary mechanism for this toxicity involves the irreversible inhibition of cholinesterase (ChE) enzymes, especially acetylcholinesterase (AChE), the enzyme responsible for clearing the excitatory neurotransmitter acetylcholine (ACh). Without adequate AChE activity, there is an excess amount of ACh at synapses, which leads to overstimulation of the downstream cells and eventually to cell death. This process leads to headache, confusion, tremors, convulsions, depression of neural respiratory centers, and seizure. Peripherally, NAs induce respiratory dysfunction via muscarinic-induced bronchorrhea and bronchoconstriction, and nicotinic-mediated respiratory paralysis. To preserve brain function and life, it is critical that both peripheral and central cholinergic symptoms are alleviated.
Many compounds with different pharmacologic mechanisms have been investigated to combat the toxic sequelae after NA exposure. Drugs that block ACh receptors, increase the effect of γ-amino-butyric acid (GABAA), and antagonize n-methyl-d-aspartic acid (NMDA) glutamatergic receptors are efficacious when administered quickly after NA exposure (Marrs 2004; Shih et al. 1991). The currently approved NA treatment system uses atropine sulfate to block ACh receptors, 2-pyridine aldoxime methyl chloride (2-PAM) to reactivate NA-inhibited AChE, and diazepam to stop seizures induced by NAs. However, after a period of sustained seizure activity, the central nervous system often becomes refractory to these treatment strategies, and seizures cannot be terminated (McDonough et al. 2010; Shih et al. 1991). Because current inhibitory- and reactivator-based strategies are unable to sufficiently control seizure activity when treatment is delayed, it is essential that victims are treated quickly so that status epilepticus and neuropathology are prevented (McDonough et al. 1995). However, in the event of an unexpected or mass casualty NA event, acute treatment may not be feasible. New medical countermeasures capable of preventing and terminating seizure activity need to be developed. Toward developing more effective anticonvulsant treatments, our team has been investigating the adenosine (ADO) signaling pathway as a potentially more effective mechanism to counter NA-induced seizure.
ADO is an endogenous purine nucleoside that has a variety of physiological effects. ADO modulates cellular activity via multiple subtype adenosine receptors (ARs). AR subtypes are classified with respect to their action on adenylyl cyclase. Stimulation of A1 adenosine receptors (A1ARs) inhibits activity via Gαi proteins, and A2A enhances activity via Gαs proteins (St Hilaire et al. 2009). Within the periphery, A1ARs are widely distributed in various tissues including heart, aorta, liver, kidney, eye, and bladder (Dixon et al. 1996). The most notable physiologic effect of peripheral A1AR activation is a decrease in heart rate and blood pressure (Schindler et al. 2005). Activation of central A1ARs has a profound inhibitory effect on neuronal activity via presynaptic inhibition of neurotransmitter release and post-synaptic hyperpolarization (Malva et al. 2003; Ribeiro et al. 2002). Therapeutic exploitation of this inhibitory effect on neuronal excitability has been investigated for neuroprotection against a variety of pathologies including drug-resistant epilepsy (Boison 2012; Gouder et al. 2003; Huber et al. 2002; Young and Dragunow 1994). Although ADO has demonstrated neuroprotective efficacy, clinical adoption of historical ADO agonists has been impeded by their modulation of cardiovascular function. Peripherally administered ADO agonists reduce cardiac output via A2AAR-induced hypotension and A1AR-induced bradycardia (Schindler et al. 2005). Despite that phenomenon, studies conducted in our laboratories demonstrated that acute intracerebroventricular (ICV) treatment with the A1AR agonist N6-cyclopentaladenosine (CPA) effectively prevented seizure and neuropathology after soman exposure (Thomas and Shih 2014). While those results were encouraging, CPA at the effective dose level produced prolonged sedation and profound hypothermia, side effects that may complicate clinical transition. Toward further developing the A1AR mechanism as a novel NA anticonvulsant, this study aimed to assess CPA’s anti-seizure efficacy and side effects when given intraperitoneally (IP). Additionally, alternative agonists with greater A1AR affinities were investigated to maximize therapeutic efficiency and to minimize off target effects. These selective A1AR agonists included 2-chloro-N6-cyclopentyladenosine (CCPA) and (±)-5′-chloro-5′-deoxy-ENBA (ENBA). While the ultimate goal is to develop a countermeasure that is capable of terminating sustained seizure activity after delayed treatment, safety and efficacy in preventing seizure with acute treatment have to be first established. Therefore, the objective of this study was to (1) determine and compare the efficacy of CPA, CCPA, and ENBA in preventing seizure and acute neurohistopathology and (2) evaluate and compare the physiological and functional responses among these A1AR agonists in a rat soman seizure model.
Material and Methods
Subjects
Male Sprague Dawley rats weighing 275–300 g were purchased from Charles River Labs (Kingston, NY). They were housed in individual cages in temperature- (21 ± 2 °C) and humidity- (50 ± 20%) controlled quarters that were maintained on a 12-h light–dark schedule (with lights on at 0600 h). Laboratory chow and tap water were freely available whenever the animals were in home cages. Animals were acclimated for 3–5 days prior to surgery.
Materials
Saline (0.9% NaCl) injection, USP, was purchased from Cutter Labs, Inc. (Berkeley, CA). Atropine methyl nitrate (AMN) was purchased from Wedgewood Pharmacy (Swedesboro, NJ). Asoxime chloride (HI-6) was synthesized by Kalexyn Medicinal Chemistry (Kalamazoo, MI). Soman (pinacolyl methylphosphonofluoridate) was obtained from the U.S. Army Edgewood Chemical Biological Center (Aberdeen Proving Ground, MD). N6-cyclopentaladenosine (CPA), 2-Chloro-N6-cyclopentyladenosine (CCPA), and (±)-5′-Chloro-5′-deoxy-ENBA (ENBA) were purchased from R&D Systems (Minneapolis, MN). All these ADO agonists were prepared in multisol vehicle (48.5% distilled H2O, 40% propylene glycol, 10% ethanol, 1.5% benzyl alcohol) on the day of treatment. Diluted preparations were sonicated until the drug was completely dissolved. During sonication, bath temperature was monitored for elevations above average ambient temperature to diminish the chance of structure degradation. CCPA readily dissolved in the solvent at all concentrations and stayed in solution until the time of treatment. CPA required additional time sonicating, but stayed in solution once dissolved. At the elevated concentrations (108 mg/ml) required for the optimal dose, ENBA did not readily dissolve and required constant sonication until time of treatment delivery. Soman was diluted in ice-cold saline prior to subcutaneous (SC) injection. AMN was injected intramuscularly (IM), while HI-6, CPA, CCPA, and ENBA were injected IP. Injection volumes were 0.5 ml/kg for nerve agent and all treatment drugs.
Experimental Procedures
Approximately 1 week before experimentation, rats were surgically prepared with the implantation of a temperature transponder for recording body temperature and cortical electrodes for recording brain electroencephalographic (EEG) activity and detecting seizure onset. After collecting baseline brain activity on the day of experimentation, the standard soman-induced seizure rat model that is used for neuroprotection studies was implemented (Shih 1990; Shih et al. 1991). Briefly, animals were pre-treated with HI-6 (125 mg/kg, IP) 30 min before a subcutaneous (SC) injection of 1.6 × LD50 (180 μg/kg) soman or saline (0.5 ml/kg). One minute later, animals were treated with an IM injection of 2 mg/kg atropine methyl nitrate (AMN). The administration of HI-6 prior to exposure and AMN immediately after, both with quaternary ammonium structures, does not affect EEG seizure onset or severity; they are used to minimize peripheral cholinergic symptoms and, thus, promote survival for adequate statistical comparisons of neuroprotection outcomes.
Since the objective of this study was to determine the anti-seizure dose efficacy of acute treatment, CPA, CCPA, ENBA, or vehicle for ADO was given IP 1 min after soman or saline (sham) exposure at increasing dose levels. The following dose ranges were administered: CPA, 0 (for vehicle control), 25, 30, 40, 50, and 60 mg/kg; CCPA, 0, 15, 18, 21, 24, 30, and 36 mg/kg; and ENBA, 0, 10, 16, 20, 28, 34, 46, 54, and 62 mg/kg. For each agonist dose level, up to 8 rats were exposed to saline to measure the effects of the A1AR agonist without soman, and 12 rats were exposed to soman to determine the dose level’s anti-seizure efficacy and rate of survival. The initial dose level for each agonist was determined from past experience and the pharmacological profiles of the new ADO agonists. To minimize the number of animals used, specific ADO dose levels were first tested in groups of 3–4 rats after soman exposure. If no seizure was detected, additional sets of 3–4 rats were tested until N = 12 for the dose level. If seizure or cholinergic symptoms were detected in any rat, the dose level was escalated.
Brain activity of each rat was monitored continuously via EEG recording for 5 h on the experimental day. The neurobehavioral responses were recorded using the functional observational battery (FOB) and toxic signs at 0, 4, 8, 15, 30, 45, and 60 min, and thereafter at 30-min increments for 5 h after soman or saline exposure. Briefly, the FOB scored the rat’s righting reflex, startle reflex, arousal, and ambulation/gait, and the presence of toxic signs, such as chewing, excessive salivation, lacrimation, head nodding, clonus, and convulsions, was recorded. Twenty-four hours after exposure, a final EEG recording (30-min duration) and neurobehavioral assessment were made. The rats were then deeply sedated and perfused for histological analysis.
Data Analysis
After perfusion, the brains were extracted, serial sectioned at 5 μm, and prepared for histology with hematoxylin and eosin (H&E) staining. Four regions associated with severe neurological deficits after NA exposure (i.e., piriform cortex, dorsal and ventral hippocampus, and thalamus) were each evaluated by a trained pathologist, who was unaware of treatment paradigm, and scored using the established standard rubric: 0 = no lesion; 1 = minimal (1–10%); 2 = mild (11–25%); 3 = moderate (26–45%); 4 = severe (> 45%) described in detail elsewhere (McDonough et al. 1995). A total neuropathology score was then calculated for each rat from 0 (normal) to 16 (severe damage), and experimental groups were then compared with their respective controls using the Kruskal-Wallis test, followed by a Dunn’s multiple comparison test if the treatment effect was significant. Differences in body temperature were also compared using the Kruskal-Wallis followed by a Dunn’s multiple comparison test. Rates of seizure and survival for soman-exposed rats that received treatment and those that did not were compared using the Fisher’s exact test. Estimation and comparison of the mean time to seizure and death were done using the Kaplan-Meier survival analysis and log rank test. Statistical significance was defined as p < 0.05. Because multiple comparisons were made to the control groups with the seizure and survival Fisher’s tests, a Bonferroni correction was implemented (p < 0.006–p < 0.01).
Results
Table 1 summarizes the dose-escalation responses (i.e., seizure and lethality rates, time to onset of EEG seizure, neuropathological scores, body temperature changes, and righting reflex) after exposure to a 1.6 × LD50 dose of soman and treatment with vehicle or an A1AR agonist.
Anticonvulsive Effects
The efficacy of each A1AR agonist was determined by comparing the agonist-treated group against the control group, which received vehicle in lieu of agonist. Seizure was readily detected from the EEG tracing; the signal associated with normal/baseline brain activity (i.e., low amplitude [< ± 100 μV], high frequency) would quickly transition to severe spiking activity with high amplitude (> ± 1000 μV) and high frequency. Behavioral signs such as convulsions and Straub tail coincided with such EEG power changes. Due to a high rate of mortality in our rat soman seizure model, a total of 28 control rats were required to generate a sufficient sample size for statistical analysis of neuropathology. Without ADO treatment, the rate of seizure prevention/absence was 0% (i.e., 100% seizure rate); the average (± standard deviation) latency to seizure was 5.28 ± 2.1 min. Of the 28 soman control rats, 6 survived to the 24-h endpoint (21%). For those rats that did survive, signs of severe neuropathology were observed with an average total score of 14.8 ± 1.8 (with a maximum score of 16).
Similar to our previous experiments involving CPA treatment via ICV, CPA via IP prevented soman-induced seizure and neurohistopathology. The anti-seizure effectiveness of CPA increased with escalating dose levels at 25, 30, 40, 50, and 60 mg/kg. A moderate level of protection was achieved even at the lowest dose of 25 mg/kg: 40% seizure rate and 20% lethality with average seizure onset of 3.7 min. Rats receiving 30 mg/kg experienced a greater rate of seizure (67% seizure, 33% survival); however, the onset of seizure was slightly delayed to 8.9 ± 4.7 min. The 40 mg/kg and 50 mg/kg groups had 100% survival with only 50% and 40% seizure rates, respectively, and for those rats that seized the average, onset was much more delayed: average seizure onset time was 19.4 and 22.7 min, respectively. The largest dose tested (60 mg/kg) provided the greatest protection. Only one of the 12 rats (8.3%) developed minimal EEG spiking/seizure activity (lower amplitude and frequency vs. control seizures) 36 min after soman exposure. The neural and physiological effect of 60 mg/kg CPA on that rat was markedly diminished compared with the other CPA-treated rats. Whereas almost all rats, even those treated with the smallest dose of CPA (25 mg/kg), experienced rapid and deep sedation, this one rat maintained consciousness and a righting reflex. Because of that aberrant response, the actual dose of CPA delivered to the IP cavity was hypothesized to be less than prescribed. The most probable cause for this observation is an error in the execution of the IP injection, not with the compound or dose. Consequently, dose escalation was not performed further, and 60 mg/kg was accepted as the minimum effective dose for CPA.
CCPA was tested against soman at 15, 18, 21, 24, 30, and 36 mg/kg. CCPA at all dose levels improved survival. From 15 to 30 mg/kg, all rats survived to the 24-h endpoint. Similar to CPA, some degree of protection from seizure was achieved at all dose levels (Table 1). All rats receiving 21 mg/kg were protected from status epilepticus; however, there were signs of toxicity. Approximately 2 h after soman exposure, rats treated with CCPA 21 mg/kg displayed brief episodes (<3 min) of tremors and minimal EEG spiking sporadically. Even though seizure/status epilepticus was not detected, we determined that the minimum effective dose was not achieved, and therefore, the dose level was increased further. At the highest dose level of 36 mg/kg, 2 of the 12 rats seized (average onset of 13 min) and later died. The remaining 10 rats were completely protected from seizure. Similar to the rationale for not escalating CPA beyond 60 mg/kg, CCPA was not escalated beyond 36 mg/kg because the lack of effect was believed to be an artifact of suboptimal IP injections. Whereas the 10 rats protected by CCPA experienced rapid unconsciousness and bradycardia, the two rats that seized maintained consciousness, reflexes, and cardiovascular function. Because that response was significantly aberrant (same vial, same day), we concluded that CCPA did not reach circulation due to suboptimal IP injections and that escalating the dose would not improve anti-seizure efficacy.
The third A1AR agonist evaluated in this study was ENBA at 10, 16, 20, 28, 34, 46, 54, and 62 mg/kg. ENBA at 10, 16, and 20 mg/kg was largely ineffective at preventing seizure onset (≤ 25%) after soman exposure. ENBA at 28 and 34 mg/kg provided statistically significant seizure protection (75% and 50%, respectively); however, lethality was high with 50% and 63% respectively. While ENBA at 46 and 54 mg/kg significantly delayed the onset of seizure to more than 2 h after soman exposure, most rats eventually seized. Significant anti-seizure and survival-promoting efficacy was only achieved with ENBA at 62 mg/kg. At that dose level, one of the 12 rats seized 155 min after exposure. That rat survived the 24-h time point. In general, ENBA had physiological and neurological effects similar to the other A1AR agonists, i.e., reduction of brain activity, bradycardia, hypothermia, and sedation; however, the duration of effect was significantly shorter. Whereas rats receiving half the effective dose of CPA and CCPA remained sedated throughout the day of treatment, all rats receiving ENBA 34 mg/kg recovered consciousness after a period of deep sedation and appeared normal by the day’s end.
Neuroprotective Effects
For all dose levels of CPA, CCPA, and ENBA, prevention of seizure translated to the absence of neuronal injury as assessed by neuropathology scoring (0 = none, 16 = severe damage). According to the Kruskal-Wallis test followed by a Dunn’s multiple comparison test, CPA at 25 and 60 mg/kg, CCPA at 21 and 36 mg/kg, and ENBA at 62 mg/kg were statistically different from the soman control group. Whereas vehicle-treated rats experienced severe neuropathology (average score = 14.8 ± 1.8), rats treated with ADO received significantly lower scores: CPA (60 mg/kg) = 0.2 ± 0.6, CCPA (36 mg/kg) = 0 ± 0, and ENBA (62 mg/kg) = 1.4 ± 4.3. Animals that experienced seizure after vehicle or ENBA at any dose level developed severe neuropathology with widespread neuronal injury and death. In contrast, the severity of neuropathology was suppressed after CPA or CCPA treatment at suboptimal dose levels, even if seizure occurred. The average neuropathology scores for seizing rats with suboptimal ADO treatments are as follows: CPA (25–50 mg/kg) = 7.5 ± 3.7, CCPA (15–30 mg/kg) = 6.2 ± 2.3, and ENBA (10–54 mg/kg) = 11.7 ± 2.8. Suppression of neuropathology with seizure activity could not be assessed for the 3 rats that seized after CPA at 60 mg/kg (N = 1) and CCPA at 36 mg/kg (N = 2) because those rats died before the study endpoint. All other rats in the soman/CPA (60 mg/kg) and soman/CCPA (36 mg/kg) groups received a neuropathology score of 0 except for one soman/CPA (60 mg/kg) rat. That rat’s dorsal and ventral hippocampus received scores of 1, which is considered normal, minor, injury. The single rat that seized after ENBA (62 mg/kg) developed severe neuropathology and received a total score of 14. All other ENBA-treated rats did not seize and received a score of 0.
Cholinergic Toxic Signs and Behavioral Effects
While CPA, CCPA, and ENBA all stimulate the A1AR with a high degree of specificity, the effects on EEG and brain activity after soman exposure varied between agonists (Fig. 1). After soman exposure and vehicle (no ADO) treatment, the rats displayed cholinergic symptoms (chewing, tremors) in less than 3 min. Within 5 min, most rats were convulsing with EEG seizure activity. That high-frequency, high-amplitude EEG signal continued throughout the day of experimental observation period (5 h). At 24 h, the spiking activity was observed, albeit at a lower frequency (Fig. 1, top row). Drastic behavioral changes correlated with CPA-, CCPA-, or ENBA-induced suppression of EEG. Animals first became lethargic and then quickly lost consciousness and a righting reflex as the EEG changed from normal (desynchronized) activity to slow-wave and flat-line. Conversely, the resumption of desynchronized EEG indicated behavioral recovery with ambulation, reflexes, and consciousness. CPA, CCPA, and ENBA effectively suppressed all cortical activity after soman exposure and, thereby, inhibited neuronal excitotoxicity. While CPA and CCPA had similar effects on EEG during the day of experimentation, rats receiving CCPA recovered more brain activity at 24 h than animals receiving CPA did. Not only had they recovered their righting reflexes and arousal, their EEG was also of higher frequency and more similar to baseline. ENBA had the most rapid and pronounced effect on EEG of all agonists tested. In rats exposed to either vehicle or soman, ENBA suppressed all cortical activity in approximately 2 min after injection. Remarkably, most rats regained all brain activity at the 24-h time point without any cholinergic symptoms. In addition to central inhibitory effects, ADO agonists also showed some inhibition of peripheral neural pathways. ADO treatments suppressed all peripheral cholinergic symptoms after soman exposure. Neither excessive salivation nor lacrimation was detected in animals receiving ADO at anti-seizure levels.
Exemplar EEG tracing for rats exposed to soman and treated with vehicle, CPA, CCPA, or ENBA. Whereas control animals (vehicle treatment) displayed severe spiking/seizure activity within 5 min of soman exposure (top row), the ADO agonists, CPA, CCPA, and ENBA, suppressed cortical activity and prevented the onset of seizure
EEG Power Analysis
The effect of soman or ADO on brain activity is further exemplified by an EEG power analysis (custom MATLAB Fast Fourier Transform script applied). As shown in Fig. 2, the power relative to baseline increased tenfold within 30 min of soman exposure without ADO treatment, a time point that corresponded to maximum EEG spiking and seizure activity. In contrast, ADO treatment rapidly suppressed EEG power and respectively all reflexes and consciousness. ENBA’s effects on brain activity were the most rapid and greatest in magnitude; EEG power was reduced to near zero in less than 10 min of treatment. EEG power then slowly increased and eventually surpassed baseline power approximately 3 h after treatment. The resumption of EEG power corresponded to an increase in body temperature from a hypothermic state, but not consciousness nor a return of a righting reflex. While EEG power was 1.5x baseline 5 h post-treatment, that power resided within low frequency bands (i.e., very low frequency, delta, and theta) that are associated with sleep. CPA and CCPA also reduced total EEG power but at a slower rate than ENBA. The effects of CPA and CCPA on the day of treatment were similar; both reduced power to approximately half of baseline within 30 min of treatment and suppressed EEG power at that level for the remainder of the experimental day.
A power analysis of the EEG brain activity after soman (GD) exposure and treatment with vehicle, CPA, CCPA, or ENBA is shown. Whereas there is a dramatic increase in EEG power 7 min after soman exposure and 6 min after vehicle treatment (top panel), ADO treatments decreased EEG power and suppressed cortical brain activity (bottom panel)
Lethality
After vehicle treatment, only 6 of the 28 rats survived to the 24-h time point. Death occurred 6.9 ± 9.3 h after exposure on average without ADO treatment. The lethal effects of soman were significantly minimized with all ADO treatment at the highest dose levels according to the Kaplan-Meier survival analysis with log rank (Mantel-Cox), p < 0.005, with a mean survival time for CPA of 20.7 ± 7.9 h, for CCPA of 18.8 ± 9.6 h, and for ENBA of 21.7 ± 7.4 h, after GD exposure. The ability to promote survival was similar for CPA, CCPA, and ENBA; differences between agonists were not statistically different. Two deaths occurred after CPA, one within 1 h of exposure and one overnight. The rat that died during the day was the only rat that seized with CPA at 60 mg/kg. Two of the 12 rats receiving CCPA at 36 mg/kg died at 0.8 and 1.0 h post-exposure with seizure. The other CCPA death occurred overnight without seizing. ENBA protected most rats at 62 mg/kg; however, two rats died at 0.8 and 0.6 h after exposure without seizure or cholinergic symptoms. While 100% survival was achieved with CPA (40–50 mg/kg), CCPA (15–30 mg/kg), and ENBA (46 mg/kg) at sub-anti-seizure dose levels, those groups had small sample sizes, and, therefore, significant differences among dose level groups could not be detected.
Effects on Body Temperature and Heart Rate
Beyond suppression of neuronal activity in the central nervous system, A1AR agonists had significant peripheral effects. All ADO treatments with and without soman exposure induced some degree of hypothermia and bradycardia (i.e., reduction of heart rate). CPA, CCPA, and ENBA by themselves (i.e., no soman exposure) significantly reduced body temperatures with increasing magnitude at 0.5× and 1.0× their respective minimum effect doses. CCPA produced the greatest reduction in body temperature on the day of exposure; rats receiving 36 mg/kg decreased from a baseline of 38.1 ± 0.2 °C to 28.6 ± 1.6 °C at 5 h (300 min) after treatment, a reduction of 24.9%. That group continued to experience a decrease in body temperature overnight; the 24-h average temperature was 27.8 ± 7.7 °C. Rats receiving 18 mg/kg of CCPA experienced a similar decline in temperature on the day of treatment (29.1 ± 0.8 °C); however, their body temperatures increased to 37.1 ± 0.0 °C at 24 h (97.6% of baseline). CPA at 30 mg/kg and 60 mg/kg had similar effects on body temperature on the day of treatment (84.0 ± 4.9% and 86.8 ± 4.6% of baseline, respectively). As with CCPA, body temperatures in rats receiving the high dose of CPA further decreased to 77.1 ± 13.3% of baseline at 24 h. Only CPA and CCPA effects were statistically different at 24 h in vehicle-exposed animals (Fig. 3a). ENBA also decreased body temperature but with less severity and for a shorter period of time. Rats receiving 34 mg/kg experienced maximum hypothermic effect 3 h after treatment and slightly recovered to 88.4 ± 1.7% of baseline at 24 h. The magnitude of reduction with ENBA at 62 mg/kg was comparable with CPA on the day of treatment; however, rats receiving ENBA demonstrated improved recovery with temperatures rebounding to 95.3 ± 4.2% of baseline at 24 h.
For rats exposed to soman, ADO treatment reduced the body temperature in rats if seizure was prevented; otherwise, seizing rats did not develop hypothermia and maintained a temperature comparable to baseline. At the anti-seizure dose levels, CPA had the greatest effect on 24-h body temperature (Fig. 3b). The body temperature of rats receiving CPA (60 mg/kg) after soman exposure decreased to 67.7 ± 10.0% of baseline. Soman-exposed rats that received CCPA (36 mg/kg) and ENBA (62 mg/kg) also experienced hypothermia on the day of exposure but had recovered to 89.2 ± 7.6% and 97.2 ± 3.1%, respectively, of their baseline body temperatures at the 24-h time point. The improvement in 24-h body temperature after soman exposure and ENBA treatment was statistically significant from soman-exposed CPA-treated animals. As evidenced by high rates of survival and seizure prevention in both hypothermic (CPA and CCPA) and normothermic (ENBA) rats, body temperature does not appear to be beneficial or deleterious to their outcomes at 24 h.
In addition to lowering body temperature, A1AR agonists rapidly reduced heart rate at all dose levels. This phenomenon was reliably observed within 60 s of treatment, quickly accompanied by lethargy and pallor. Unlike the severity of hypothermia, the magnitude and rate of heart rate reduction were not dependent on the ADO dose level. That is, the lowest dose of each agonist had the same acute effect on the heart rate as the highest dose tested. However, the duration of heart rate depression was dose dependent; the recovery of baseline physiological parameters was quicker in rats receiving lower ADO doses. At the optimal/anti-seizure dose levels, depression of heart rate relative to baseline persisted until the 24-h endpoint for all treatments after saline exposure with statistical significance. The effect was, however, smallest with ENBA (Fig. 4a). For soman-exposed animals (Fig. 4b), CPA at 60 mg/kg induced the greatest bradycardia of all ADO treatments: heart rates at 24 h averaged 33.6 ± 20.4% of baseline. CCPA and ENBA at anti-seizure dose levels also depressed heart rate, but to a significantly less degree than CPA at 24 h. Heart rates for CCPA-treated (36 mg/kg) rats were 67.9 ± 17.0%, and ENBA-treated (62 mg/kg) rats had 78.7 ± 13.4% relative to baseline.
Effects on Behavior
A functional observational battery (FOB), including assessments for startle reflex, righting reflex, arousal, and gait, was performed on each animal at regular intervals after soman exposure and treatment. Of the various functional assessments, the presence or absence of a righting reflex was the most representative measure of function or incapacitation for these rats. That is, the ability to right themselves after being placed on their sides indicated at least a moderate degree of cognitive and motor function. Rats receiving CPA at 60 mg/kg experienced the greatest immobility and depth of sedation: only 2 of the 10 surviving rats recovered their righting reflex and some ability to walk at 24 h; the remaining animals were unconscious and unable to ambulate. The functional recovery after CCPA (36 mg/kg) and ENBA (62 mg/kg) was markedly better than after CPA; all rats except for one CCPA-treated rat were able to ambulate at 24 h. Overall, approximately 33% of soman/vehicle, 80% of soman/CPA, 22% of soman/CCPA, and 0% of soman/ENBA rats were unable to ambulate at the 24-h endpoint.
Discussion
The use of NAs poses a severe threat to civilian and military personnel. Because current medical countermeasures have limited efficacy in preventing or terminating NA-induced seizure, we are investigating novel treatment strategies that utilize the ADO signaling pathway to suppress excitotoxic neuronal activity. Van Helden and his associates (van Helden et al. 1998) from the Netherlands Organization for Applied Scientific Research (TNO, Netherlands) first recognized adenosine’s potential as a pathway to medically counter NA. CPA at 2 mg/kg (IM) was shown to reduce nerve agent lethality and diminish cholinergic toxicity in rats challenged with soman (van Helden et al. 1998). Subsequent experiments performed by TNO continued to examine ADO as a NA countermeasure and proposed that ADO’s observed effect on mitigating NA-induced pathology was an artifact of the cardiovascular output; i.e., CPA reduced cardiac output and, therefore, minimized the nerve agent’s bioavailability in the body and brain (Bueters et al. 2002; Bueters et al. 2003; Compton 2004; Joosen et al. 2004). While TNO discontinued their development of ADO due to that conclusion, the mechanism of ADO’s protection has not been fully established. It is possible that ADO’s full neuroprotective potential was not realized due to the low doses that were tested by TNO. In 2012, we rekindled the development of ADO as a neuroprotective pathway against NA. To examine ADO’s ability to limit central excitotoxic activity via central pre- and post-synaptic inhibitory effects, CPA was directly injected into the brains in rats exposed to seizure-inducing doses of soman. The results from that study demonstrated that CPA does have a direct effect on central neuronal activity that provided neuroprotection against NAs (Thomas and Shih 2014). This study builds upon that previous work to evaluate the efficacy of not only CPA at much higher doses, but also two newer ADO candidates that have great specificity for the A1AR in a rat soman seizure model. We demonstrated that acute ADO treatment effectively prevented the onset of seizure and promoted survival with statistical significance. CPA at 60 mg/kg, CCPA at 36 mg/kg, and ENBA at 62 mg/kg were determined to be effective anti-seizure dose levels.
Of the three A1AR agonists tested in this study, ENBA at 62 mg/kg was the most efficacious treatment and that it was anti-seizure, was survival promoting, and allowed for ambulation at the study endpoint of 24 h. CPA and CCPA also promoted survival and prevented seizure; however, those animals had not recovered consciousness nor a righting reflex at 24 h. While protective sedation is a much better outcome than status epilepticus after NA exposure, the ideal countermeasure would allow the treated victim to return to combat or at least ambulate so that medical resources could be directed elsewhere. In addition to enabling a faster recovery, ENBA’s suppression of neuronal activity was more rapid and pronounced than that of CPA and CCPA. Consequently, ENBA may offer better protection since cholinergic and glutamatergic excitotoxicity would have less opportunity to develop. Furthermore, ENBA’s pharmacological profile would allow the first responder or clinician to better control the course of treatment and maintain seizure prevention with additional doses while minimizing side effects.
While the primary motivation for investigating ADO was to leverage the A1AR’s profound inhibitory effect on cortical brain activity, data from this study suggest that ADO’s protective efficacy can also be attributed to inhibition of peripheral neural pathways. Soman-induced hypersecretions (bronchorrhea and alveolar edema) often lead to high rates of mortality (Hulse et al. 2014). In this study, ADO treatments suppressed all peripheral cholinergic symptoms after soman exposure. Neither excessive salivation nor lacrimation was detected in animals receiving ADO at anti-seizure levels. This peripheral phenomenon in addition to reduction in seizure activity is likely the driving mechanisms of ADO’s promotion of survival after soman exposure.
ADO treatments had significant cognitive and physiological effects at all dose levels. While others have reported that ADO’s peripheral effects (i.e., cardiac depression) limit clinical utility (Biaggioni 1992; Dunwiddie and Masino 2001), the data from the present study clearly demonstrated that acute ADO-induced bradycardia is not lethal regardless of whether the animal was exposed to soman or not. There was zero lethality for all saline-exposed (no soman) and ADO-treated rats at any dose level. Moreover, all ADO treatments promoted survival after soman exposure with great statistical significance concomitant to bradycardia and hypothermia. Although these results suggest that A1AR stimulation is a promising mechanism for countering NA intoxication, further study is needed to establish acute toxicity and long-term safety and efficacy of relatively high ADO doses. In-depth assessment of ADO’s acute safety and toxicity with pharmacokinetic/pharmacodynamic and LD50 studies with multiple routes of administration will be performed in the near-term for pre-clinical development. Since ADO receptors are expressed in many different types of tissues (e.g., liver, heart, spleen, and kidney) and modulate a variety of physiologic functions (Yaar et al. 2005), robust long-term behavioral and histological analyses are required to verify that effective dose levels do not induce deleterious side effects.
The ultimate goal for any NA medical countermeasure is to provide neuroprotection. However, neuroprotection is a difficult phenomenon to define and quantify. A common and relatively straightforward approach is to associate histologically quantified neuronal health or injury with neuroprotection. That is, the presence of spongiform changes, rarefaction, and aberrant neuronal staining/morphology indicates severe damage and likely poor functional outcomes. Conversely, brain sections that lack such indicators typically correlate to normal behavior and positive outcomes. From this definition, CPA (60 mg/kg), CCPA (36 mg/kg), and ENBA (62 mg/kg) provided significant neuroprotection against a high-dose soman exposure. In general, that neuroprotection closely correlated with seizure prevention. However, CPA and CCPA surprisingly provided moderate, yet not significant, neuroprotection even after soman-induced seizure. CPA-treated rats that seized received an average neuropathology score of 7.5 ± 3.7 (maximum score of 16), and CCPA-treated rats that seized received an average score of 6.2 ± 2.3. In contrast, all ENBA-treated rats that seized displayed greater neuropathology, with an average score of 11.7 ± 2.8. CPA’s and CCPA’s greater duration of effect may explain this partial protection. Whereas ENBA at a suboptimal dose level may have suppressed excitotoxic activity for a short period of time, that effect likely subsided overnight. However, CPA’s and CCPA’s effects were longer lasting than ENBA’s, and their suppression of the excitotoxic magnitude may have persisted overnight and consequently minimized neuronal damage. Further study into the mechanism of partial neuroprotection is required.
In this study, there were several aberrant cases of subdued or absent responses to ADO injection. At the optimal dose levels, CPA, CCPA, and ENBA produced rapid sedation, inhibition of EEG, and bradycardia after saline or soman exposure in the majority of rats. However, the responses of 1 CPA rat, 2 CCPA rats, and 1 ENBA rat were fundamentally different. Those rats displayed minimal reaction to ADO, i.e., lack of sedation, minimal bradycardia, and insignificant EEG power effects. While biological variability and sensitivity to A1AR stimulation may lead to slight differences in the duration of neuronal inhibition, the pronounced absence of central effects indicates other causative factors when strain, weight, age, and sex are controlled. One plausible explanation is variability in the exact location of the treatment injection. Whether it was from deformation of the IP cavity from improper animal holding or a misplacement in the injection site, clearly the amount of ADO agonist reaching the circulation was less. Consequently, the lack of anti-seizure and neuroprotection in the rats receiving ADO agonists at the high dose levels could be attributed to human error and not to the countermeasure. In follow-up experiments, alternative routes of administration such as IM should be evaluated not only to minimize injection error but also to assess the efficacy of a more clinically relevant delivery technique.
The anti-seizure and neuroprotective efficacy that was demonstrated by these ADO compounds motivates further development of this promising mechanism. Because the induction of hypothermia can be neuroprotective in itself during a number of pathological states, future experiments will isolate and evaluate the effect that hypothermia has on nerve agent-induced seizure and neuropathology. Additionally, the efficacy of ADO agonists will be evaluated when administrated via more clinically relevant routes, e.g., intramuscular.
In summary, three candidate A1AR agonists were evaluated for anti-seizure and neuroprotective efficacy in a rat soman seizure model. After completing a dose-escalation study, CPA at 60 mg/kg, CCPA at 36 mg/kg, and ENBA at 62 mg/kg were determined to be effective anti-seizure doses. Suppression of soman-induced seizure activity translated to protection of brain tissue from neuropathology. Moreover, all ADO treatments promoted survival with great statistical significance. While CPA, CCPA, and ENBA concomitantly induced bradycardia and hypothermia in soman-exposed rats, those peripheral side effects did not negatively affect outcomes. Of the three agonists tested, ENBA displayed the most beneficial pharmacological profile. Not only did that agonist produce the most rapid and profound suppression of neuronal activity, but also rats treated with ENBA after soman were fully functional 24 h later. These data strongly suggest that A1AR agonists are promising NA medical countermeasures. Toward further developing this novel treatment strategy, future studies will comprehensively evaluate CPA, CCPA, and ENBA against a broad set of threat agents including sarin, cyclosarin, and VX, and in combination with currently approved oximes and benzodiazepines. Additionally, longer term studies will be conducted to better assess physiological and functional recovery after ADO treatment with and without preceding NA exposure.
References
Biaggioni I (1992) Contrasting excitatory and inhibitory effects of adenosine in blood pressure regulation. Hypertension 20(4):457–465
Boison D (2012) Adenosine augmentation therapy. In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV (eds) Jasper’s basic mechanisms of the epilepsies, 4th edn, Bethesda
Bueters TJ, Groen B, Danhof M, AP IJ, Van Helden HP (2002) Therapeutic efficacy of the adenosine A1 receptor agonist N6-cyclopentyladenosine (CPA) against organophosphate intoxication. Arch Toxicol 76(11):650–656. https://doi.org/10.1007/s00204-002-0395-x
Bueters TJ, Joosen MJ, van Helden HP, Ijzerman AP, Danhof M (2003) Adenosine A1 receptor agonist N6-cyclopentyladenosine affects the inactivation of acetylcholinesterase in blood and brain by sarin. J Pharmacol Exp Ther 304(3):1307–1313. https://doi.org/10.1124/jpet.102.044644
Compton JR (2004) Adenosine receptor agonist Pd 81,723 protects against seizure/status epilepticus and neuropathology following organophosphate exposure. Walter reed army inst of research silver spring md published by wrair and available through dtic
Dixon AK, Gubitz AK, Sirinathsinghji DJ, Richardson PJ, Freeman TC (1996) Tissue distribution of adenosine receptor mRNAs in the rat. Br J Pharmacol 118(6):1461–1468
Dunwiddie TV, Masino SA (2001) The role and regulation of adenosine in the central nervous system. Annu Rev Neurosci 24(1):31–55. https://doi.org/10.1146/annurev.neuro.24.1.31
Gouder N, Fritschy JM, Boison D (2003) Seizure suppression by adenosine A1 receptor activation in a mouse model of pharmacoresistant epilepsy. Epilepsia 44(7):877–885
Huber A, Guttinger M, Mohler H, Boison D (2002) Seizure suppression by adenosine A(2A) receptor activation in a rat model of audiogenic brainstem epilepsy. Neurosci Lett 329(3):289–292
Hulse EJ, Davies JOJ, Simpson AJ, Sciuto AM, Eddleston M (2014) Respiratory complications of organophosphorus nerve agent and insecticide poisoning. Implications for respiratory and critical care. Am J Respir Crit Care Med 190(12):1342–1354. https://doi.org/10.1164/rccm.201406-1150CI
Joosen MA, Bueters TH, Helden HM (2004) Cardiovascular effects of the adenosine A1 receptor agonist N6-cyclopentyladenosine (CPA) decisive for its therapeutic efficacy in sarin poisoning. Arch Toxicol 78(1):34–39. https://doi.org/10.1007/s00204-003-0513-4
Malva JO, Silva AP, Cunha RA (2003) Presynaptic modulation controlling neuronal excitability and epileptogenesis: role of kainate, adenosine and neuropeptide Y receptors. Neurochem Res 28(10):1501–1515. https://doi.org/10.1023/a:1025618324593
Marrs TC (2004) The role of diazepam in the treatment of nerve agent poisoning in a civilian population. Toxicol Rev 23(3):145–157
McDonough JH Jr, Dochterman LW, Smith CD, Shih TM (1995) Protection against nerve agent-induced neuropathology, but not cardiac pathology, is associated with the anticonvulsant action of drug treatment. Neurotoxicology 16(1):123–132
McDonough JH, McMonagle JD, Shih TM (2010) Time-dependent reduction in the anticonvulsant effectiveness of diazepam against soman-induced seizures in guinea pigs. Drug Chem Toxicol 33(3):279–283. https://doi.org/10.3109/01480540903483417
Ribeiro JA, Sebastiao AM, de Mendonca A (2002) Adenosine receptors in the nervous system: pathophysiological implications. Prog Neurobiol 68(6):377–392
Schindler CW, Karcz-Kubicha M, Thorndike EB, Müller CE, Tella SR, Ferré S, Goldberg SR (2005) Role of central and peripheral adenosine receptors in the cardiovascular responses to intraperitoneal injections of adenosine A1 and A2A subtype receptor agonists. Br J Pharmacol 144(5):642–650. https://doi.org/10.1038/sj.bjp.0706043
Shih TM (1990) Anticonvulsant effects of diazepam and MK-801 in soman poisoning. Epilepsy Res 7(2):105–116
Shih TM, Koviak TA, Capacio BR (1991) Anticonvulsants for poisoning by the organophosphorus compound soman: pharmacological mechanisms. Neurosci Biobehav Rev 15(3):349–362
St Hilaire C, Carroll SH, Chen H, Ravid K (2009) Mechanisms of induction of adenosine receptor genes and its functional significance. J Cell Physiol 218(1):35–44. https://doi.org/10.1002/jcp.21579
Thomas TP, Shih T-M (2014) Stimulation of central A1 adenosine receptors suppresses seizure and neuropathology in a soman nerve agent seizure rat model. Toxicol Mech Methods 24(6):385–395. https://doi.org/10.3109/15376516.2014.920450
van Helden HP, Groen B, Moor E, Westerink BH, Bruijnzeel PL (1998) New generic approach to the treatment of organophosphate poisoning: adenosine receptor mediated inhibition of ACh-release. Drug Chem Toxicol 21 Suppl 1(s1):171–181. https://doi.org/10.3109/01480549809007409
Yaar R, Jones MR, Chen JF, Ravid K (2005) Animal models for the study of adenosine receptor function. J Cell Physiol 202(1):9–20. https://doi.org/10.1002/jcp.20138
Young D, Dragunow M (1994) Status epilepticus may be caused by loss of adenosine anticonvulsant mechanisms. Neuroscience 58(2):245–261
Acknowledgements
The authors wish to thank the technical assistance of Cindy Acon-Chen, Jeff Koenig, Kristy Meads, and Justin Moreno.
Funding
The authors would like to thank the generous financial support by the National Institutes of Health (NIH) via an NIH-USAMRICD Interagency Agreement (AOD16024-001-00000/A120-B.P2016-02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimers
The views expressed in this report are those of the author(s) and do not reflect the official policy of the Department of Army, Department of Defense, or the U.S. Government. The experimental protocol was approved by the Institutional Animal Care and Use Committee at the U.S. Army Medical Research Institute of Chemical Defense, and all procedures were conducted in accordance with the principles stated in the Guide for the Care and Use of Laboratory Animals and the Animal Welfare Act of 1966 (P.L. 89-544), as amended. The facility where this research was conducted is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International. The use of trade names does not constitute an official endorsement or approval of the use of such commercial hardware or software. This document may not be cited for purposes of advertisement.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thomas, T.P., Wegener, A. & Shih, TM. In Vivo Evaluation of A1 Adenosine Agonists as Novel Anticonvulsant Medical Countermeasures to Nerve Agent Intoxication in a Rat Soman Seizure Model. Neurotox Res 36, 323–333 (2019). https://doi.org/10.1007/s12640-019-00034-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-019-00034-w