Abstract
Toxocariasis is an underestimated geohelminthic infection which shows respiratory changes concurrent with larval migration. The purpose of the present study was to detect Toxocara seropositivity in asthmatic and pneumonic children, and in turn to evaluate its association with the children clinical manifestations, laboratory test results, and sociodemographic risk factors. A total of 50 asthmatic, 50 pneumonic children and 50 healthy controls were subjected to stool analysis by direct wet mount and concentration techniques to exclude possible cross reactivity. Blood samples were collected for complete blood count and assessment of eosinophil count. Sera were examined for anti-Toxocara IgG antibodies, and measurement of total IgE level. Anti Toxocara IgG was detected in 27.3% (41/150) of the studied children. It was significantly higher in asthmatic group compared to controls (26%. p value = 0.033) and significantly highest in pneumonia group compared to both bronchial asthma group (46%. p value = 0.030) and control group (10%. p value = 0.001). There was a significant association between anti Toxocara IgG seroprevalence and each of eosinophilia, total IgE and both combined. Anti Toxocara IgG showed significant higher percentage in asthmatic children who recorded history of soil contact and pets contact as compared to control and pneumonic groups. Toxocara IgG seropositivity was highly associated with fever, cough, wheezes and dyspnea with statistical significance. Toxocara seropositivity has to be considered as a vital associated factor for asthmatic and pneumonic children, and eventually better to be considered in differential diagnosis by pediatricians. Further studies are still needed to explore the correlation between toxocariasis and different patient categories.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human toxocariasis is a worldwide neglected zoonotic disease caused by helminthic infection of Toxocara canis (T. canis) and Toxocara cati (T. cati), the ascarid worms in dogs and cats, respectively (Temsah et al. 2021). The seroprevalence of human toxocariasis varies from 0.6% in Canada to 86% in Nigeria in either developing or developed countries (Ma et al. 2018). In Egypt, Toxocara infection occurs specially in low-income populations with poor hygienic practices where stray and household dogs and cats have an important role in the spread of toxocariasis among Egyptians (Farghly et al. 2016).
Toxocara infection occurs through ingestion of embryonated eggs in raw vegetables, or contaminated soil, or by accidental consumption of Toxocara larvae in raw or insufficiently cooked meat or liver of paratenic hosts (Fialho and Corrêa 2016). Children are the most susceptible group to Toxocara infection owing to their common behaviors, such as geophagia, contact with soil while playing, direct contact with animals having eggs in their fur, poor personal hygiene, and absence of parents’ supervision (Despommier 2003; El-Tantawy et al. 2013).
In humans, the parasite can't develop beyond the larval stage and the migrating larvae cause allergic reactions and intense local inflammatory response in different organs such as liver, lungs, eye and brain causing visceral, covert, ocular, and cerebral toxocariasis (Despommier 2003). In the first two conditions, children may be asymptomatic or develop asthma symptoms (Smith et al. 2009). Infected children may also suffer from fever, cough, hepatomegaly, abdominal pain, or dermatological lesions (Nash 2005). However, the severity of infection depends on the intensity of infection, the site of migrating larvae, age of the child, and the host’s immune system qualification (Pawlowski 2001).
Bronchial asthma (BA) is a global health problem that seems to be the most widespread chronic disease in children. In last decades, it increased progressively due to new lifestyle and different environmental risk factors (Nunes et al. 2017). The relationship between asthma and toxocariasis has always been an issue of research.
Toxocariasis could be risk factor for the inception of allergic diseases including asthma, or may accelerate pulmonary symptoms in asthmatic patients as well (Cooper 2008; Aghaei et al. 2018). Moreover, asthma is described in various studies as a toxocariasis-associated factor (Cooper 2009; Cadore et al. 2016).
Pulmonary involvement in toxocariasis is common and manifests by wheezing, coughing, and dyspnea (Despommier 2003), while some lung diseases can also occur as asthma, acute bronchiolitis or pneumonitis (Lassmann et al. 2007). Yet, there are rare reports recording severe clinical manifestations in children like acute severe asthma and diffuse interstitial pneumonia (Demirci et al. 2012). The presumptive mechanism of pulmonary infiltration is assumed to the larval allergic reaction in the lung (Yoshikawa et al. 2011).
Since human toxocariasis is largely unknown and uncommon to health professionals, it is still a poorly diagnosed disease in Egypt. Direct techniques can't diagnose the disease and thus ELISA is usually used for this purpose especially during epidemiologic studies. ELISA gives highly sensitive and specific results with minor degrees of cross-reactivity in case of using second-stage T. canis larvae excretory and secretory (E/S) antigens (Magnaval et al. 2001).
The purpose of the present study was to investigate Toxocara seropositivity in diagnosed asthmatic and pneumonic children in comparison to healthy children in Beni-Suef University Hospital, and to evaluate its association with the children clinical manifestations, laboratory test results and sociodemographic risk factors.
Subjects and methods
Study design and population
A case control hospital-based study was conducted from May 2020 to January 2022 on a total of 150 children aged between 2 and 15 years. The studied cases (n. = 100) were categorized into 50 asthmatic children diagnosed clinically and according to GINA recommendations (GINA 2019), and 50 pneumonic children diagnosed clinically and radiologically by finding of nodules or, ground glass opacities, or areas of consolidations or all of them. The studied cases were attending Allergy and Immunology Outpatient Clinic and Pediatric Department of Beni-Suef University Hospital, while the controls (n. = 50) were sex/age-matched healthy children with no respiratory manifestations.
Exclusion criteria for cases included children aged < 2 years old, children with malignancy, autoimmune diseases, or taking systemic steroid therapy, children positive for helminthic infections by stool analysis to exclude the cross reactivity with toxocariasis. In asthmatic cases, genetic and allergic asthma were ruled out from the study as well.
A structured questionnaire was obtained from each child parent/legal guardian to assess the possible association with Toxocara seropositivity including socio-epidemiological, environmental, and clinical data. Also, all children were subjected to full clinical examination.
Samples collection
Stool samples
Three consecutive fecal samples were collected from each child 1 day apart, and examined for parasitic infections at Medical Parasitology Department, Faculty of Medicine, Beni-Suef University. Samples were subjected to direct microscopic examination and formalin-ethyl acetate concentration technique. Positive samples (ova/larvae) of helminthic infections (fascioliasis, ascariasis, strongyloidiasis, trichuriasis, ancylostomiasis) were excluded to get out of possible cross reactions.
Blood samples
Two venous blood samples were collected individually from studied children. The first blood sample (3 ml) was collected on EDTA anticoagulant for complete blood count (CBC) and assessment of eosinophil count where values > 400/mm3 was expressed as eosinophilia (Figueiredo et al. 2005). The second sample of blood was centrifuged, and serum samples were separated and stored at -20 °C until used for detection of anti‐Toxocara IgG antibodies and measurement of total IgE level.
Serological tests
Detection of anti‐Toxocara IgG antibodies
Serum samples of all children were analyzed for IgG anti-Toxocara antibodies against (E/S) Toxocara larval antigens using the commercial Human Toxocara Canis Antibody ELISA kit (Bioassay England, Cat # ED4450) according to the manufacturer’s instructions. The optical density (OD) was read at a wavelength of 450 nm with a microplate ELISA reader and calculation of cut-off value was done as mean of negative controls OD value plus 0.15.
Measurement of total IgE level
The measurement of total IgE was performed quantitively using the commercial Human IgE ELISA kit (ThermoFisher Scientific) following manufacturer instructions. OD was determined at 450 nm. Construction of the standard curve was done as well as calculation of samples concentration in relation to the mean absorbance from the standard curve.
Statistical analysis
Statistical analysis was done using statistical package for social sciences (SPSS) computer software (version 25), IBM software, USA. All the studied variables were categorical, that were described as the total number and percentage for each category and were compared to the chi-square χ2 test. p value equal to or < 0.05 was considered of significant value.
Results
A total of 150 children participated in this study were distributed as follows: 100 cases (50 children with BA and 50 children with pneumonia), and 50 controls without respiratory manifestations. Table 1 provides the sociodemographic characteristics of the cases and controls children showing a single statistical difference among all participants in pets contact variable (p value = 0.037). Participants’ age ranged from 2 to 11 years old; the mean age of the case patients was 4.05 ± 1.98 years and that of the control group was 4.28 ± 2.01 years old.
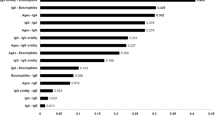
As demonstrated in Table 2, anti Toxocara IgG was detected in 27.3% (41/150) of the studied children. It was significantly higher in BA cases (26%) as compared to controls (10%)/(p value = 0.033). Also, anti Toxocara IgG was significantly highest in pneumonia cases group (46%) as compared to both BA cases (p value = 0.030) and control group (p value = 0.001). Eosinophil count was higher in BA cases as compared to controls, though it was not statistically significant (p value > 0.05). Eosinophil count was significantly higher in the pneumonia cases group as compared to both normal control (p value = 0.011) and BA cases (p value = 0.032). Total IgE in the BA cases group was significantly higher than in control group (p value = 0.008), while there was non-statistically significant difference between pneumonia group versus controls (p value > 0.05). Non-statistically significant difference was observed in IgE level between BA and pneumonia cases (p value > 0.05).
There was a statistically significant association between anti Toxocara IgG seroprevalence and each of eosinophilia, IgE seropositivity, and combined eosinophilia with IgE seropositivity. Nineteen out of forty-one (46.3%) children with positive anti Toxocara IgG had eosinophilia (p value = 0.031), and fifteen (36.6%) of positive anti Toxocara IgG showed positive total IgE (p value = 0.013). Also, nine (22%) children with positive anti Toxocara IgG had combined eosinophilia with IgE seropositivity with statistical significance (p value = 0.008) as shown in Table 3.
There was non-statistically significant association between Toxocara IgG seropositivity, with some studied variables such as sex, residence and socioeconomic level (p values > 0.05). We couldn’t detect any statistically significant difference in each group separately compared to control and compared to the other group. However, seropositivity of Toxocara IgG in children with positive soil contact showed higher percentages in BA cases as compared to both controls (p value = 0.040), and pneumonic cases (p value = 0.043) with statistical significance. Also, Toxocara IgG seropositivity was significantly higher in children with positive pets contact in the BA cases group as compared to control group (p value = 0.045) as shown in Table 4.
Table 5 demonstrates some important statistical differences regarding associated clinical manifestations. All studied children with positive Toxocara IgG in BA cases didn’t have fever (p value < 0.001), and complained of chronic cough (p value = 0.016). Anti Toxocara IgG was more prevalent among pneumonia cases who have dyspnea as compared to BA cases (p value = 0.032). Also, anti Toxocara IgG was higher in most of asthmatic cases who have wheezes (92.3%) with statistical significance (p value = 0.042).
Discussion
Generally, human toxocariasis are difficult to diagnose due to asymptomatic infection in most of cases and inaccessibility of the parasite (Hotez and Wilkins 2009). The main diagnosis is based on direct detection of Toxocara sp. larvae in tissues. However, identification of larvae seems to be difficult due to their extended allocation and tiny size. Moreover, tissue biopsy is considered an invasive procedure (Ma et al. 2018). PCR-based approaches are not commonly used for toxocariasis routine diagnosis, but they are used for gene analysis and identification of species (Gasser 2013). Serological diagnoses by ELISA techniques and CT scan for chest lesions can diagnose toxocariasis without risk of invasiveness (Despommier 2003).
Serodiagnosis of toxocariasis may cross reacts with other helminthic infections, in particular, geohelminthic ones. To rule out geohelminthic parasites in our study, we examined three consecutive fecal samples from each child using direct microscopic examination and formalin-ethyl acetate concentration technique, and any positive results were excluded. Hence, the ELISA test using (E/S) antigen derived from T. canis second-stage larvae was the most suitable screening diagnostic approach for human toxocariasis in our study with acceptable 91% sensitivity and 86% specificity (Jacquier et al. 1991).
As regards results analysis of the present study, the overall anti Toxocara IgG seropositivity in all studied children was 27.3%. Anti Toxocara IgG was found in 13 (26%) of asthmatic children as referred to 5 (10%) of healthy control children. These results were accepted with that reported in Egypt by Badawey et al. (2018), and Shahat et al. (2019) who detected 17%, 22.2% of toxocariasis in asthmatic children compared to 10%, 6.9% in controls from Zagazig and Damietta cities, respectively. Meanwhile, El-Tantawy et al. (2013) observed higher seropositivity of toxocariasis in 42% of asthmatic children compared to 8% in controls from Dakahlia, Egypt. Temsah et al. (2021) reported lower anti Toxocara IgG level in 15% of asthmatic children in Damietta, Egypt. Variable seroprevalence results were illustrated worldwide such as Iran (45%, 9.8%), Cuba (40.1%), and Brazil (63.6%) (Momen et al. 2018; Salemi et al. 2021; Kanobana et al. 2013; Mendonca et al. 2013) respectively. Other researches didn’t detect anti Toxocara IgG in sera of control group (Sadri et al. 2019). Previous variable Toxocara seropositivity may be due to the different ecological conditions of environments in these studied areas, and methods used for diagnosis in each study.
Our obtained results showed significant association between anti Toxocara IgG seropositivity and BA. This was consistent with previous observations (Fernando et al. 2009; El-Tantawy et al. 2013; Shahat et al. 2019). Contrarily, some authors hadn’t found any correlation between them (Sadri et al. 2019; Shamsian et al. 2019; Salemi et al. 2021).
In the preceding literature, eosinophil count was higher in BA cases (28%) as compared to controls (24%), though it was not statistically significant. This obtained result went in hand with previous results that revealed no significant association between eosinophilia level in asthmatic children (Badawey et al. 2018; Shahat et al. 2019) and in contrast with others who reported a statistical difference between BA children and control group as regards eosinophilia (El-Tantawy et al. 2013).
Regarding pneumonia cases, seropositivity of anti Toxocara IgG (46%) and eosinophil count (48%) were significantly highest as compared to both control group and BA cases. Among positive anti Toxocara IgG pneumonic children, eosinophilia was detected in (47.8%) so that eosinophilic pneumonia cases showed statistically significant association in our study. Roig et al. (1992) recorded 64% eosinophilia and diffuse lung infiltration in patient with toxocariasis. They declared that the diagnosis of pulmonary infiltration with high eosinophilia best performed by routine ELISA of toxocariasis as it detected unsuspected and undetermined numbers of cases of toxocariasis with lung involvement. Bouchard et al. (1994) diagnosed case report of acute severe eosinophilic pneumonia positive for anti Toxocara IgG. Another case report of toxocariasis with eosinophilic pneumonia was detected using serological test (Demirci et al. 2012).
Estimation of total IgE level provides evidence of atopy, which is almost a general finding in asthmatic children and described as a capability to produce excessive amount of IgE when exposed to allergens (Burrowset al. 1989). Increased reactivity of the airway to variable stimuli such as irritants, cold air, allergens, viruses, and exercise frequently tends to occur in asthmatic patients (Borish et al. 2005).
Total IgE in the BA cases was significantly higher than in control group (34% vs. 12%), and this is completely in accordance with El-Tantawy et al. (2013). These data agreed with other researches suggesting that elevation of total IgE and eosinophilia in asthmatic patients are highly related to toxocariasis (Figueiredo et al. 2005; Bahnea et al. 2008). Concerning our observations, total IgE was higher (22%) in pneumonia group versus controls (12%) and this result was confirmed by other studies reporting that young children having pulmonary lesions with hyperimmunoglobulinemia E and high eosinophilia could be suggestive of toxocariasis (Mazur-Melewska et al. 2015).
Based on our findings, there was a statistically significant association between anti Toxocara IgG seroprevalence in BA (26%), and each of eosinophilia (28%) and total IgE (34%). This was agreed with the results of Mendonca et al. (2012) who reported that toxocariasis was an important provocative of eosinophilia and IgE. Anti Toxocara IgG seropositivity (46.3%) was detected among (33.3%) of positive eosinophilia individuals. This result agreed with Gueglic et al. (1994) who suggested that patients with eosinophilia were at 149 times higher risk of having toxocariasis compared to other patients with negative eosinophilia. Martin et al. (2008) and Espinoza et al. (2008) had previously demonstrated higher rates of eosinophilia in nearly 87% of toxocariasis positive cases. El-Shazly et al. (2013), Shahat et al. (2019) and Song et al (2020) detected lower Toxocara IgG seropositivity in 29%, 36.4%, and 22.2% eosinophilic cases in Egypt and Korea, respectively.
In the present work, behavioral, and sociodemographic data, were debatable. The obtained result revealed non statistically significant association between anti Toxocara IgG seropositivity with studied variables regarding sex, and socioeconomic level in the total studied groups together. This agrees with Badawey et al. (2018), Shahat et al. (2019) Guadalupe et al. (2021) and Temsah et al. (2021). Other researches related between toxocariasis and sex (Silva et al. 2016), socioeconomic status (Souza et al. 2011; Alvarado 2013).Meanwhile, Toxocara IgG seropositivity was significantly higher in asthmatic children with positive pets contact (61.5%) as compared to control group, which is similar to other studies (Badawey et al. 2018; Shahat et al. 2019; Temsah et al. 2021).
Our results revealed non statistical significance between Toxocara IgG seropositivity and residence, although percentages were higher in rural areas (80.5%) than urban areas (19.5%) which is parallel to findings with variable statistical values observed by Nyan et al. (2001), Badawey et al. (2018), and Shahat et al. (2019). Also, higher anti-Toxocara IgG (70.7%) was detected in children that had positive soil contact and showed statistical significance which matches with others (El-Tantawy et al. 2013; Badawey et al. 2018; Shahat et al. 2019).
Regarding the outcome of respiratory manifestations in BA children, all studied cases with positive Toxocara IgG in their sera (100%) didn’t have fever and complained of chronic cough and this showed high significant statistical difference. Dyspnea was more prevalent among positive anti Toxocara IgG pneumonic cases (60.9%) as compared to BA cases (23.1%) with significant statistical difference. Wheezes were observed in most of asthmatic cases (92.3%) with statistical significance. The obtained results revealed significant association between Toxocara seropositivity and respiratory symptoms in BA patients in the same way illustrated previously by Shahat et al. (2019).
Fever in pneumonic children was (56.5%) which may be owed to hyper-reaction of T. canis larvae in systemic or pulmonary involvement (Park et al. 2014). All children in pneumonia group (asymptomatic and symptomatic) underwent classical chest radiography screening. Children who revealed abnormalities in their chest X ray were subjected to anti Toxocara IgG test, that was previously approved by others (Park et al. 2014; Mazur-Melewska et al. 2015).
Pulmonary symptoms are the most frequent clinical respiratory manifestations recorded in toxocariasis (Gueglic et al. 1994). Respiratory manifestations occur in toxocariasis are owed to migration of larvae and infected subjects are most probably start to wheeze in response to larval invasion (Nash 2005).
In the preceding literature, Toxocara IgG seropositivity had no significant association with GIT manifestations, which was in contrast to Bahnea et al. (2008), and Shahat et al. (2019) results at this point.
In conclusion, the present study illustrated a potential significant association between Toxocara seropositivity, BA and pneumonia in pediatric children in our Governorate confirming the role of toxocariasis as a vital associated factor for this category of children. It’s necessary to evaluate the impact of this neglected parasitic infection on the public health. Pediatricians should keep in mind to consider toxocariasis as a common differential diagnosis in BA and eosinophilic pneumonia especially in our country Egypt. Further studies are still needed to explore the correlation between toxocariasis and different patient categories. Extended researches from different localities in Egypt as well as larger sample size are recommended.
References
Aghaei S, Riahi SM, Rostami A, Mohammadzadeh I, Javanian M, Tohidi E, Foroutan M, Esmaeili Dooki M (2018) Toxocara spp. infection and risk of childhood asthma: a systematic review and meta-analysis. Acta Trop 182:298–304. https://doi.org/10.1016/j.actatropica.2018.03.022
Alvarado E (2013) Toxocariasis in waste pickers: a case control seroprevalence study. PLoS ONE 8:e54897. https://doi.org/10.3389/fpsyt.2019.00766
Badawey M, Fathy G, Abdelrahman S, Dalia A (2018) Relation between Toxocara infection, atopy and asthmatic bronchitis children in Zagazig University Hospitals. J Egy Soc Parasitol 48:93–100. https://doi.org/10.12816/jesp.77030
Bahnea RG, Ivan A, Cârdei E, Luca MC, Stoica O (2008) Retrospective clinical and laboratory study of the toxocariasis cases hospitalized between 2005 and 2008. Rev Med Chir Soc Med Nat Iasi 112:938–941
Borish L, Chipps B, Deniz Y, Gujrathi S, Zheng B, Dolan CM (2005) Total serum IgE levels in a large cohort of patients with severe or difficult-to-treat asthma. Ann Allergy Asthma Immunol 95:247–253. https://doi.org/10.1016/S1081-1206(10)61221-5
Bouchard O, Arbib F, Paramelle B, Brambilla C (1994) Acute eosinophilic pneumonia and the larva migrans syndrome: apropos of a case in an adult. Rev Mal Respir 11:593–595
Burrows B, Martinez FD, Halonen M, Barbee RA, Cline MG (1989) Association of asthma with serum IgE levels and skin test reactivity to allergens. New Engl J Med. 320:270–277. https://doi.org/10.1056/NEJM198902023200502
Cadore PS, Linjie Zhang MD, Lemos LL, Lorenzi C, Telmo PL, Santos PC, Mattos GT, Vignol FS, Prietsch SOM, Berne MEA, Scaini CJ (2016) Toxocariasis and childhood asthma: a case-control study. J Asthma. https://doi.org/10.3109/02770903.2015.1064951
Cooper PJ (2008) Toxocara canis infection: an important and neglected environmental risk factor for asthma? Clin Exp Allergy 38:551–553. https://doi.org/10.1111/j.1365-2222.2008.02934.x
Cooper PJ (2009) Interactions between helminth parasites and allergy. Curr Opin Allergy Clin Immunol 9:29–37
Demirci M, Unlü M, Fidan F, Kaya S (2012) Eosinophilic pneumonia due to toxocariasis: an adult case report. Turkiye Parazitol Derg 36:258–259. https://doi.org/10.5152/tpd.2012.61
Despommier D (2003) Toxocariasis: clinical aspects, epidemiology, medical ecology, and molecular aspects. Clin Microbiol Rev 16:265–272. https://doi.org/10.1128/cmr.16.2.265-272.2003
El-Shazly A, Abdel Baset A, Khairy A, Mohammed TI, Hammad S (2013) Seroprevalence of human toxocariasis (visceral larva migrans) AAMJ 11
El-Tantawy NL, ElNahas HA, El-Assmy MM, Alsalem AM (2013) Clinicosero-epidemiological evaluation of toxocariasis in asthmatic pediatric children in Mansoura city in Egypt. Arch Clin Microbiol 4:3. https://doi.org/10.3823/271
Espinoza YA, Huapaya PH, Roldan WH, Jimenez S, Arce Z et al (2008) Clinical and serological evidence of Toxocara infection in school children from Morrope district, Lambayeque, Peru. Rev Inst Med Trop Sao Paulo 50:101–105. https://doi.org/10.1590/s0036-46652008000200007
Farghly AM, Mohamed SM, Abdel-Rahman SA, Mohammed FE, El-Bahaie ES, El-Shafey MA (2016) The relation between the prevalence of soil transmitted parasites in the soil and among school children in Zagazig district, Sharkyia Governorate. Egypt J Parasit Dis 40:1021–1029. https://doi.org/10.1007/s12639-014-0627-z
Fernando D, Wickramasinghe P, Kapilananda G, Dewasurendra RL, Amarasooriya M, Dayaratne A (2009) Toxocara seropositivity in Sri Lankan children with asthma. Pediatr Int 51:241–245. https://doi.org/10.1111/j.1442-200X.2008.02687.x
Fialho PM, Corrêa CR (2016) A systematic review of toxocariasis: a neglected but high-prevalence disease in Brazil. Am J Trop Med Hyg 94:1193–1199. https://doi.org/10.4269/ajtmh.15-0733
Figueiredo SD, Taddei JA, Menezes J, Novo NF, Silva EO, Cristóvão HL, Cury MC (2005) Clinical-epidemiological study of toxocariasis in a pediatric population. J Pediatr (rio J) 81:126–132
Gasser RB (2013) A perfect time to harness advanced molecular technologies to explore the fundamental biology of Toxocara species. Vet Parasitol 193:353–364. https://doi.org/10.1016/j.vetpar.2012.12.031
GINA (2019) Global initiative for asthma. Global Strategy for Asthma Management and Prevention. www.ginasthma.org
Guadalupe S, Noé M, Esteban G et al (2021) Detection of antigens and anti-Toxocara canis antibodies in children with different asthma severities. Immun Inflamm Dis 9:435–442. https://doi.org/10.1002/iid3.403442
Gueglic B, de Gentile L, Nguyen JM, Achard J, Cha-basse D, Marjolet M (1994) Epidemiologic approach to human toxocariasis in western France. Parasitol Res 80:531–536
Hotez PJ, Wilkins PP (2009) Toxocariasis: America’s most common neglected infection of poverty and a helminthiasis of global importance? PLoS Negl Trop Dis 3:e400. https://doi.org/10.1371/journal.pntd.0000400
Jacquier P, Gottstein B, Stingelin Y et al (1991) Immunodiagnosis of toxocarosis in humans: evaluation of a new enzyme-linked immunosorbent assay kit. J Clin Microbiol 29:1831–1835
Kanobana K, Vereecken K, Junco Diaz R, Sariego I, Rojas L (2013) Toxocara seropositivity, atopy and asthma: a study in Cuban school children. Trop Med Int Health 18:403–406. https://doi.org/10.1111/tmi.12073
Lassmann B, Tsigrelis C, Virk A (2007) 33-Year-old woman with marked eosinophilia. Mayo Clin Proc 82:103–106. https://doi.org/10.4065/82.1.103
Ma G, Holland CV, Wang T, Hofmann A, Fan CK, Maizels RM, Hotez PJ, Gasser RB (2018) Human toxocariasis. Lancet Infect Dis 18:e14-24. https://doi.org/10.1016/S1473-3099(17)30331-6
Magnaval JF, Glickman LT, Dorchies P, Morassin B (2001) Highlights of human toxocariasis. Korean J Parasitol 39:1–11. https://doi.org/10.3347/kjp.2001.39.1.1
Martin UO, Machuca PB, Demonte MA, Contini L (2008) Analysis of children with a presumptive diagnosis of toxocariasis in Santa Fe, Argentina. Medicina (b Aires) 68:353–357
Mazur-Melewska K, Katarzyna J-P, Paweł K, Anna M, Magdalena F, Wojciech S (2015) Pulmonary presentation of Toxocara sp. infection in children. Pneumonol Alergol Pol 83:250–255. https://doi.org/10.5603/PiAP.a2015.0043
Mendonca LR, Veiga RV, Dattoli VC, Figueiredo CA, Fiaccone R et al (2012) Toxocara seropositivity, atopy and wheezing in children living in poor neighborhoods in urban Latin American. PLoS Negl Trop Dis 6:e1886. https://doi.org/10.1371/journal.pntd.0001886
Mendonca LR, Figueiredo C, Esquivel R, Fiaccone R, Carvalho L (2013) Seroprevalence and risk factors for Toxocara infection in children from an urban large setting in Northeast Brazil. Acta Trop 128:90–95. https://doi.org/10.1016/j.actatropica.2013.06.018
Momen T, Esmaeil N, Reisi M (2018) Seroprevalence of Toxocara canis in asthmatic children and its relation to the severity of diseases—a case-control study. Med Arch Jun 72:174–177. https://doi.org/10.5455/medarh.2018.72.174-177
Nash TE (2005) Visceral larva migrans and other unusual helminth infections. In: Mandell GR, Bennett JE, Dolin R (eds) Principles and practice of infectious diseases, 6th edn. Elsevier Churchill Livingstone, Philadelphia
Nunes C, Pereira AM, Morais-Almeida M (2017) Asthma costs and social impact. Asthma Res Pract 3:1. https://doi.org/10.1186/s40733-016-0029-3
Nyan OA, Walraven GE, Banya WA (2001) Atopy, intestinal helminth infection and total serum IgE in rural and urban adult Gambian communities. Clin Exp Allergy 31:1672–1678. https://doi.org/10.1046/j.1365-2222.2001.00987.x
Park BM, Jeong SO, Park HS, Jung SS, Kim SY, Kim JO, Lee JE (2014) Differences in the clinical and radiological characteristics of lung-involved toxocariasis between toxocariasis with eosinophilia and those without eosinophilia. J Thorac Dis 6:1757–1764. https://doi.org/10.3978/j.issn.2072-1439.2014.12.24
Pawlowski Z (2001) Toxocariasis in humans: clinical expression and treatment dilemma. J Helminthol 75:299–305. https://doi.org/10.1017/s0022149x01000464
Roig J, Romeu J, Riera C, Texido A, Domingo C, Morera J (1992) Acute eosinophilic pneumonia due to toxocariasis with broncho-alveolar lavage findings. Chest 102:294–296
Sadri H, Gharavi MJ, Arjmand R, Zibaei M, Elahimehr N et al (2019) Toxocara infection in asthmatic children: a case-control study in Karaj district, Iran. Arch Pediatr Infect Dis 7:e82370. https://doi.org/10.5812/pedinfect.82370
Salemi AM, Arefkhah N, Mikaeili F, Rabbani H, Nabavizadeh H (2021) Seroprevalence of Toxocara infection among asthmatic children in Shiraz City, Southern Iran. Iran J Parasitol 16:587–592. https://doi.org/10.18502/ijpa.v16i4.7871
Shahat SA, Mohammad KA, Saad MY, Emran TM, Mohamed SA, Elshahat ME (2019) A clinico-sero-epidemiological evaluation of toxocariasis in asthmatic Egyptian children. Egypt J Hosp Med 76:4195–4201
Shamsian SA, Sayedi SJ, Zibaei M, Vaghei S, Moghaddas E (2019) Frequency of toxocariasis among asthmatic children in Northeastern Iran. Arch Clin Infect Dis 14:e82967. https://doi.org/10.5812/archcid.82967
Silva MB, Amor AL, Santos LN, Galvão AA, OviedoVera AV (2016) Risk factors for Toxocara spp. seroprevalence and its association with atopy & asthma phenotypes in school age children in a small town and semi-rural areas of Northeast Brazil. Acta Trop 9:425–428. https://doi.org/10.1016/j.actatropica.2016.04.005
Smith H, Celia H, Mervyn T, Magnaval J, Peter S, Rick M (2009) How common is human toxocariasis? Towards standardizing our knowledge. Trends Parasitol 25:182–188. https://doi.org/10.1016/j.pt.2009.01.006
Song HB, Lee D, Jin Y, Kang J, Cho SH et al (2020) Prevalence of toxocariasis and its risk factors in patients with eosinophilia in Korea. Korean J Parasitol 58:413–419. https://doi.org/10.3347/kjp.2020.58.4.413
Souza RF, Dattoli VC, Mendonca LR, Jes- us JR, Baqueiro T, (2011) Prevalence and risk factors of human infection by Toxocara canis in Salvador, State of Bahia, Brazil. Rev Soc Bras Med Trop 44:516–519. https://doi.org/10.1590/S0037-86822011000400024
Temsah KA, Mostafa ME, El-Khaleegy H, El Rifai AW, Al shazly SM, Abd Rabbo MAD (2021) Toxocariasis; a neglected tropical disease. Association with asthma, chronic urticaria and unexplained neurologic manifestations among children. IJMA 3:922–929. https://doi.org/10.21608/ijma.2020.46359.1192
Yoshikawa M, Koyama N, Hontsu S, Yamamoto Y, Mikasa K, Kimura H (2011) Lessons from eight cases of adult pulmonary toxocariasis: abridged republication. Respirology 16:1014–1015. https://doi.org/10.1111/j.1440-1843.2011.02000.x
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
All manuscript authors contributed to every aspect of it; idea of the research, study design and conception, collection of materials, methodology, writing the paper, revising/editing and approving it.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The study was approved by Research Ethical Committee of Beni-Suef University, Faculty of Medicine, Egypt. Ethical approval certificate is registered under number FMBSUREC/08052022. Written informed consent was obtained from children's parents/guardians after detailed description of the study's purpose. Pediatricians were informed with children positive results to describe appropriate treatment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abd El Wahab, W.M., Ali, M.I., Ibrahim, S.S. et al. Toxocariasis: potential association with bronchial asthma, and pneumonia among pediatric children. J Parasit Dis 47, 93–100 (2023). https://doi.org/10.1007/s12639-022-01543-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12639-022-01543-w