Abstract
Purpose
There is a paucity of data on the effect of intraoperative end-tidal carbon dioxide (EtCO2) levels on postoperative mortality. The purpose of this study was to investigate the relationship between intraoperative EtCO2 and 90-day mortality in patients undergoing major abdominal surgery under general anesthesia.
Methods
We conducted a historical cohort study of patients undergoing major abdominal surgery under general anesthesia at Kyoto University Hospital. We measured the intraoperative EtCO2, and patients with a mean EtCO2 value < 35 mm Hg were classified as low EtCO2. The time effect was determined based on minutes below an EtCO2 of 35 mm Hg, and cumulative effects were evaluated by measuring the area under the threshold of 35 mm Hg for each patient.
Results
Of 4,710 patients, 1,374 (29%) had low EtCO2 and 55 (1.2%) died within 90 days of surgery. Multivariable Cox regression analysis—adjusted for age, American Society of Anesthesiologists Physical Status classification, sex, laparoscopic surgery, emergency surgery, blood loss, mean arterial pressure, duration of surgery, type of surgery, and chronic obstructive pulmonary disease—revealed an association between low EtCO2 and 90-day mortality (adjusted hazard ratio, 2.2; 95% confidence interval [CI], 1.2 to 3.8; P = 0.006). In addition, severity of low EtCO2 was associated with an increased 90-day mortality (area under the threshold; adjusted hazard ratio; 2.9, 95% CI, 1.2 to 7.4; P =0.02); for long-term exposure to an EtCO2 < 35 mm Hg (≥ 226 min), the adjusted hazard ratio for increased 90-day mortality was 2.3 (95% CI, 0.9 to 6.0; P = 0.08).
Conclusion
A mean intraoperative EtCO2 < 35 mm Hg was associated with increased postoperative 90-day mortality.
Résumé
Objectif
Il n’existe que très peu de données s’intéressant à l’effet du niveau peropératoire télé-expiratoire du dioxyde de carbone (EtCO2) sur la mortalité postopératoire. L’objectif de cette étude était d’examiner la relation entre l’EtCO2 peropératoire et la mortalité à 90 jours chez des patients subissant une chirurgie abdominale majeure sous anesthésie générale.
Méthode
Nous avons réalisé une étude de cohorte historique portant sur des patients subissant une chirurgie abdominale majeure sous anesthésie générale à l’Hôpital universitaire de Kyoto. Nous avons mesuré l’EtCO2 peropératoire, et les patients avec une valeur moyenne d’EtCO2 < 35 mmHg ont été catégorisés comme EtCO2 faible. L’effet temps a été déterminé en fonction de la durée, en minutes, avec une EtCO2 inférieure à 35 mmHg, et les effets cumulatifs ont été évalués en mesurant l’aire sous le seuil de 35 mmHg pour chaque patient.
Résultats
Sur 4710 patients, 1374 (29 %) avaient une EtCO2 faible et 55 (1,2 %) sont décédés dans les 90 jours suivant la chirurgie. Une analyse de régression multivariée de Cox, ajustée pour tenir compte des facteurs suivants : âge, statut physique selon l’American Society of Anesthesiologists, sexe, chirurgie par laparoscopie, chirurgie d’urgence, pertes de sang, tension artérielle moyenne, durée de la chirurgie, type de chirurgie et maladie pulmonaire obstructive chronique, a révélé une association entre une EtCO2 faible et la mortalité à 90 jours (rapport de risque ajusté, 2,2; intervalle de confiance [IC] à 95 %, 1,2 à 3,8; P = 0,006). De plus, la sévérité de l’EtCO2 basse était associée à une augmentation de la mortalité à 90 jours (aire sous le seuil; rapport de risque ajusté; 2,9, IC 95 %, 1,2 à 7,4; P =0,02); pour une exposition à long terme à une EtCO2 < 35 mmHg (≥ 226 minutes), le rapport de risque ajusté pour une mortalité accrue à 90 jours était de 2,3 (IC 95 %, 0,9 à 6,0 ; P = 0,08).
Conclusion
Une EtCO2 peropératoire moyenne < 35 mmHg était associée à une augmentation de la mortalité postopératoire à 90 jours.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
With an increasing number of surgeries worldwide, approximately 4.2 million people die within 30 days of surgery each year, accounting for 7% of all deaths globally.1
The International Standards for a Safe Practice of Anesthesia recommend monitoring of end-tidal carbon dioxide (EtCO2) with a capnograph during general anesthesia.2 Although mild hypocapnia, defined as an EtCO2 of 30-35 mm Hg, was traditionally used to reduce the requirements for sedatives, analgesics, and neuromuscular blocking drugs,3 a recent review suggested that mild hypercapnia (EtCO2 ≥ 40 mm Hg) should be the standard for anesthesia management,3 based on evidence of the risks of hypocapnia4,5 and the benefits of mild hypercapnia.6,7,8,9 Nevertheless, most of these studies were conducted in animals,8 patients undergoing neurosurgery,10 and intensive care patients with traumatic brain injury11 or acute respiratory distress syndrome (ARDS).9,12 Furthermore, an eight-year observational study of 317,445 adult patients receiving general anesthesia reported that EtCO2 levels varied significantly between hospitals and providers.13 Thus, there is no consensus on the recommended target intraoperative EtCO2 level in clinical practice.
In the general surgery literature, three studies have shown an association between low EtCO2 and poor postoperative outcomes, including higher mortality14 and prolonged postoperative length of stay (PLOS).14,15,16 Nevertheless, no studies have evaluated the association between duration and degree of low EtCO2 and postoperative outcomes. In addition, the one study that investigated the association between EtCO2 and postoperative mortality did not adjust for important confounding factors like laparoscopic surgery, chronic obstructive pulmonary disease (COPD) status, and surgery type.14
Therefore, we explored the effects of the duration and degree of hypocapnia exposure after adjusting for important confounding factors. We aimed to investigate the relationship between intraoperative EtCO2 levels and 90-day mortality (the primary outcome) and in-hospital mortality and PLOS (secondary outcomes).
Methods
Ethics
The Kyoto University Certified Review Board (Kyoto, Japan) approved the study protocol (approval number: R1272-3, 23 January 2020) and waived the requirement for informed consent because of the retrospective nature of the study.
Study design, setting, and population
This retrospective single-centre historical cohort study included data from the Kyoto University Hospital Improve Anesthesia Care and Outcomes (Kyoto-IMPACT) database. The Kyoto-IMPACT database was designed to identify the relationships between intraoperative respiratory and circulatory parameters and postoperative outcomes. We selected patients who underwent surgery under the supervision of an anesthesiologist at the Kyoto University Hospital—a Japanese teaching hospital with 1,121 beds. We have published several papers using data from the Kyoto-IMPACT database.17,18 We included consecutive patients aged 18 yr or older who underwent major abdominal surgery under general anesthesia at Kyoto University Hospital from March 2008 to December 2017. We targeted the abdominal surgery population because we assumed that there would be a large number of cases in the database, long surgical durations, and a high incidence of recorded outcomes. The major abdominal surgeries in this study included liver, colorectal, gastric, pancreatic, or esophageal resections by either laparoscopic or non-laparoscopic approaches. We excluded cases with missing EtCO2 data or one-lung ventilation.
Data collection
We collected data from the Kyoto-IMPACT database, which was built from an anesthesia information management system and an electronic medical records system. We measured EtCO2 by continuously using a sidestream gas analyzer (GF-220R Multigas/Flow Unit, Nihon Kohden®, Japan) that automatically uploaded data to the anesthesia information management system every 60 sec. The intraoperative EtCO2 was defined as the mean EtCO2 level from skin incision to closure. If the EtCO2 level was less than 20 mm Hg, it was deleted as an artifact (occurring, for example, during aspiration or position change). Definitions of variables, including minimum and maximum EtCO2, are listed in eTable 1 in the Electronic Supplementary Material (ESM). We obtained data on causes of all deaths that occurred within 90 days from the date of surgery by reviewing all clinical data contained within the electronic medical record.
Exposure
To determine how EtCO2 is related to postoperative mortality, we defined exposure by calculating the dose, time, and cumulative effects of EtCO2. Dose effects were evaluated using the mean EtCO2. We divided patients into two groups based on a cut-off level of 35 mm Hg, as suggested by Way and Hill3. Patients with low EtCO2 were defined as patients with a mean EtCO2 < 35 mm Hg, whereas patients with normal EtCO2 had a mean EtCO2 ≥ 35 mm Hg. Classification into one of these groups was used as the main exposure for further analysis. Furthermore, we considered that the relationship between EtCO2 and mortality may not be linear, so we categorized the mean EtCO2 into quartiles (i.e., < 35, 35-37, 37-39, and ≥ 39 mm Hg). To assess the effects of the duration and degree of low EtCO2 exposure, the time effect was determined based on minutes below an EtCO2 of 35 mm Hg, and cumulative effects were evaluated by measuring the area under the threshold of an EtCO2 of 35 mm Hg. We further categorized minutes and area under the threshold of an EtCO2 of 35 mm Hg into quartiles, with the lowest quartile as the reference category.
Outcomes
We focused on three outcome variables. The primary outcome was 90-day mortality, which was defined as any mortality within 90 days of surgery, because it includes postoperative deaths occurring after 30 days or after discharge.19,20,21 For patients who were discharged within 90 days of surgery, post-discharge survival was confirmed from the outpatient visit records. In addition, follow-up information registered by the surgeon was used for patients whose outpatient visit records were discontinued within 90 days. Secondary outcomes were defined as in-hospital mortality and PLOS. In-hospital mortality was defined as any mortality during the index hospitalization. Postoperative length of stay was defined as the duration of hospitalization after surgery for patients who survived until hospital discharge.
Statistical analysis
Analyses of the relationship between EtCO2 and postoperative mortality were planned before data collection. We compared groups using the Mann-Whitney test and the Chi square test. We expressed continuous variables as medians [interquartile ranges (IQRs)] and categorical variables as counts and proportions (%).
First, we performed a Cox proportional hazard regression model to calculate the hazard ratios for low EtCO2 (mean EtCO2 < 35 mm Hg) and 90-day mortality, with the reference category of normal EtCO2 (mean EtCO2 ≥ 35 mm Hg). In addition, the hazard ratios for the mean EtCO2 of the first quartile (mean EtCO2 < 35 mm Hg), third quartile (mean EtCO2 37-39 mm Hg), and fourth quartile (mean EtCO2 ≥ 39 mm Hg), were compared with the reference category of the second quartile (mean EtCO2 35-37 mm Hg) because the latter is considered as normocapnia. Furthermore, to examine the cumulative and time effects, we evaluated how each quartile affected 90-day mortality, with the first quartile of the area below the threshold EtCO2 of 35 mm Hg and minutes under an EtCO2 of 35 mm Hg as the reference category. We created a directed acyclic graph (eFigure, ESM), and further created a model using covariates that affect both EtCO2 and 90-day mortality to show the relationship between EtCO2 and 90-day mortality. In the model, we adjusted for age, sex, American Society of Anesthesiologists Physical Status (I or II vs III or VI), laparoscopic surgery, emergency surgery, COPD, blood loss (mL), type of surgery, mean of mean arterial pressure (MAP) (mm Hg), and surgery duration (hr). Moreover, we used a logistic regression model to investigate whether dose, time, or cumulative effects of EtCO2 affected in-hospital mortality, adjusted using the model above. Further, to evaluate the relationship between EtCO2 and PLOS, a linear regression analysis was performed with adjustment for the possible confounders in the model above.
The relationship between EtCO2 and postoperative outcomes may depend on patient characteristics and surgical factors. Thus, we performed subgroup analysis to assess this potential heterogeneity. In addition, we used the same Cox proportional hazard regression model in the following subgroups: (i) type of surgery (hepato-pancreatic surgery or gastrointestinal surgery); (ii) blood loss (≥ 500 or < 500 mL); (iii) laparoscopic surgery (yes or no); (iv) emergency surgery (yes or no); (v) COPD (yes or no); (vi) duration of surgery (≥ or < 4 hr) and (vii) epidural anesthesia (yes or no). We calculated the crude hazard ratio for 90-day mortality in each subgroup and tested the interaction between subgroups and EtCO2. When performing subgroup analysis, subgroup covariates were included in the model as covariates.
A sensitivity analysis was used to assess the robustness of our findings. We used sensitivity models as a Cox proportional 90-day regression model after adjusting for the aforementioned confounders to assess the veracity of the primary analysis: (i) patients limited to a single surgery during the follow-up period; (ii) excluded patients whose follow-up information was registered by surgeons; and (iii) where the outcome was defined as 30-day mortality. We also added an analysis of the partial pressure of arterial carbon dioxide (PaCO2)-EtCO2 gradient and 90-day mortality for patients who had arterial gas measurements taken during surgery. Finally, propensity score matching analysis was performed to balance the aforementioned confounders and further potentially important confounders.
To maximize statistical power, we included all eligible patients in the Kyoto-IMPACT database. To determine study power, we predicted 4,500 eligible surgeries in our database in the nine-year time period, a hazard ratio of 2.5 with a postoperative 90-day mortality of 1%22,23 and low EtCO2 proportion of 50%,13 resulting in an estimated power of 87%. We carried out a complete case analysis because the missing data were 0.1%. All statistical tests were two-tailed. We used Stata/SE 15.1 (StataCorp LLC, College Station, TX, USA) for statistical analyses.
Results
Baseline patient characteristics
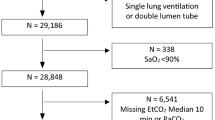
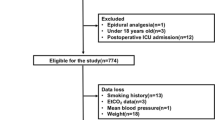
From the 4,781 major abdominal surgical patients treated between 2008 and 2017, 4,718 met our inclusion criteria and were included in the analyses (4,710 had complete case report forms; Figure).
Flow chart for the study. We consecutively included patients aged ≥ 18 yr who underwent major abdominal surgery under general anesthesia at the Kyoto University Hospital from March 2008 to December 2017. Then, we selected the cases that met the eligibility criteria and analyzed them as complete cases.
Low EtCO2 (defined as a mean EtCO2 of less than 35 mm Hg) was found in 29% of the patients. Table 1 displays the characteristics of the study participants. The median [IQR] EtCO2 level was 33 [32-34] mm Hg for patients with low EtCO2 and 38 [36-40] mm Hg for patients with normal EtCO2.
Association between low EtCO2 and 90-day mortality
Table 2 presents the main results of the study. The overall 90-day mortality was 1.2% (55 of 4,710), compared with 2.2% (30 of 1,374) in the low EtCO2 group and 0.8% (25 of 3,336) in the normal EtCO2 group. The adjusted hazard ratio for the low EtCO2 group (mean EtCO2 < 35 mm Hg) after multivariable adjustments indicated an association between low EtCO2 and 90-day mortality (adjusted hazard ratio, 2.2; 95% confidence interval [CI], 1.2 to 3.8; P = 0.006) compared with the normal EtCO2 group. For further analysis, EtCO2 was divided into quartiles, and the second quartile (mean EtCO2 35-37 mm Hg) was used as the reference. The first quartile (mean EtCO2 < 35 mm Hg) was associated with an increased 90-day mortality (adjusted hazard ratio, 2.9; 95% CI, 1.3 to 6.4; P = 0.008; Table 2). Nevertheless, the third quartile (mean EtCO2 37-39 mm Hg) and fourth quartile (mean EtCO2 ≥ 39 mm Hg) were not associated with increased 90-day mortality.
Regarding the cumulative effects of EtCO2, the fourth quartile (408-7,206) of the area under the threshold EtCO2 of 35 mm Hg was associated with an increased 90-day mortality compared with the first quartile (0-13; adjusted hazard ratio, 2.9; 95% CI, 1.2 to 7.4; P = 0.02). Finally, regarding the time effects of EtCO2 on 90-day mortality, the adjusted hazard ratio for long-term exposure to EtCO2 levels < 35 mm Hg (the fourth quartile of exposure time to EtCO2 < 35 mm Hg, 226-1,069 min) compared with short-term exposure (the first quartile of exposure time to EtCO2 < 35 mm Hg, 0-21 min) was 2.3 (95% CI, 0.9 to 6.0; P = 0.08). We reported the causes of death in patients who died within 90 days after surgery in the ESM, eTable 2.
Association between low EtCO2 and in-hospital mortality
The in-hospital mortality was 1.3% (61 of 4,710) overall, 2.3% (32 of 1,374) in the low EtCO2 group, and 0.9% (29 of 3,336) in the normal EtCO2 group. Compared with the patients with normal EtCO2, patients with low EtCO2 were more likely to have higher in-hospital mortality rates (adjusted odds ratio, 2.0; 95% CI, 1.2 to 3.5; P = 0.01, Table 3). In addition, both time and cumulative effects of low EtCO2 (< 35 mm Hg) were associated with increased in-hospital mortality (Table 3).
Association between low EtCO2 and PLOS
The median [IQR] PLOS was 21 [5-33] days (Table 4). The median [IQR] PLOS in patients with low EtCO2 was longer than in patients with normal EtCO2 (24 [17-39] days vs 20 [15-30] days; P < 0.001). Linear regression analysis revealed a significant association between low EtCO2 and PLOS (adjusted difference in PLOS, 1.7; 95% CI, 0.2 to 3.1; P = 0.02).
Subgroup analysis
Subgroup analysis involved type of surgery, blood loss, laparoscopic surgery, emergency surgery, COPD diagnosis, duration of surgery, and epidural anesthesia. These broadened the CIs but did not significantly alter the effects of low EtCO2 on 90-day mortality. There were no interactions between these variables and 90-day mortality (Table 5).
Sensitivity analysis
In the sensitivity analysis, we observed the relationship between low EtCO2 and 90-day mortality (eTable 3, ESM) as well as the relationship between low EtCO2 and 30-day mortality (eTable 4, ESM). The PaCO2-EtCO2 gradient was also significantly associated with increased 90-day mortality (eTable 5, ESM). In the propensity score matched analysis, low EtCO2 was also associated with increased 90-day mortality (eTable 6, ESM).
Discussion
Overview of results
In this retrospective cohort study of over 4,000 abdominal surgery patients undergoing general anesthesia, we found that low intraoperative EtCO2 was associated with a 2.2-fold increase in postoperative 90-day mortality. In addition, low EtCO2 was associated with increased in-hospital mortality and prolonged PLOS.
Possible mechanisms
There are two hypotheses regarding the mechanisms underlying an association between low intraoperative EtCO2 and increased postoperative mortality. One hypothesis is that a low EtCO2 reflects hypocapnia, which has deleterious effects including hypotension due to peripheral vasodilation,24 reduced tissue perfusion4, arrhythmia,25 cerebral vasoconstriction,26,27 cognitive decline,28,29 increased intrapulmonary shunt, and pulmonary cellular dysfunction.5 Another hypothesis is that low EtCO2 may reflect an increased PaCO2-EtCO2 gradient, which indicates pathological conditions such as increased V/Q mismatch, increased alveolar dead space, increased shunting rates, reduced pulmonary blood flow, and hemodynamic instability, rather than systemic hypocapnia. An increase in the PaCO2-EtCO2 gradient above 10 mm Hg is associated with increased ARDS severity,30 increased mortality in patients with trauma,31,32 and poor outcomes in patients with sepsis.33 Furthermore, low EtCO2 may reflect lower cardiac output and lower pulmonary blood flow when ventilation is constant during surgery.34,35,36,37 Whether systemic hypocapnia itself is associated with worse outcomes needs to be clarified in future studies.
Clinical implications
In our study, 29% of the patients had low mean intraoperative EtCO2 levels. A previous study indicated that more than half of the patients who underwent general anesthesia had a low intraoperative EtCO2.13 Extremely low EtCO2 should be observed carefully as it may be associated with higher postoperative mortality and longer hospital stays. If the PaCO2-EtCO2 gradient increases, before targeting a lower EtCO2, anesthesiologists should consider assessing and stabilizing the circulatory and respiratory status. In addition, our results suggested that a low EtCO2 is associated with poor outcomes independent of blood pressure, which may reflect a condition that compensates for low cardiac output by increasing peripheral vascular resistance and stabilizing blood pressure. Low EtCO2 without low MAP may indicate a decreased cardiac output and pulmonary blood flow; therefore, cardiovascular stabilization should be considered in this scenario.
Hypercapnia can elicit beneficial effects, including increased cardiac index,6 increased tissue perfusion,6,7 decreased postoperative surgical site infection,38 and lung protection.8,9 A review revealed that mild hypercapnia (EtCO2 ≥ 40 mm Hg) was beneficial and should be accepted as a standard treatment.3 Conversely, some recent reports show deleterious effects of hypercapnia, including immunosuppression,39,40 decreased diaphragm contractility41 and skeletal muscle atrophy.42 The effects of hypercapnia on postoperative mortality are unclear since it has both beneficial and harmful effects. We did not observe beneficial effects of mild hypercapnia (mean EtCO2 ≥ 39 mm Hg) compared with an EtCO2 of 35-37 mm Hg. We, therefore, recommend that further studies should be undertaken on the effect of hypercapnia on surgical outcomes.
Strengths
Our research has several strengths. First, our research extends beyond EtCO2 by exploring the effects of duration and degree of exposure to a low intraoperative EtCO2 < 35 mm Hg (median duration > 225 min) and an increased 90-day mortality and in-hospital mortality. The two studies that have examined the association between low EtCO2 and outcome have both evaluated the dose effect only,14,15 whereas only one study assessed the association between the dose effect of low EtCO2 and postoperative mortality.14 Second, we designed a regression model to adjust for important confounding factors related to postoperative mortality, including type of surgery, laparoscopic surgery, COPD, and blood loss. Third, we effectively captured 90-day mortality data in 98.9% of the patients. We did this by accessing 90-day follow-up outpatient records (4,553/4,710, 96.7%) and information registered by surgeons for patients whose outpatient visit records were discontinued within 90 days (99/4,710, 2.1%), leaving loss of follow-up in 53/4,710 (1.1%) of patients.
Limitations
There are several limitations to our study. First, there are likely unknown or unmeasured confounders. These may include the potential reasons for anesthesiologists to aim for a specific EtCO2 level and the missing source data on smoking status, hypothermia, anesthetic depth, and ventilation parameters. Second, this study evaluated the effect of the PaCO2-EtCO2 gradient on 90-day mortality using the first intraoperative measured PaCO2 level, but it did not consider the effect of variations over time in either PaCO2 level or PaCO2-EtCO2 gradient. Third, the study design employed was observational so could not infer causality. Furthermore, it is not clear whether the association between EtCO2 and 90-day mortality is due to hypocapnia or the PaCO2-EtCO2 gradient. Therefore, future randomized controlled trials are needed.
Conclusions
In patients undergoing major abdominal surgery, intraoperative low EtCO2 was associated with increased postoperative 90-day mortality, in-hospital mortality, and hospital stay.
References
Nepogodiev D, Martin J, Biccard B, et al. Global burden of postoperative death. Lancet 2019; DOI: https://doi.org/10.1016/S0140-6736(18)33139-8.
Merry AF, Cooper JB, Soyannwo O, Wilson IH, Eichhorn JH. International Standards for a Safe Practice of Anesthesia 2010. Can J Anesth 2010; 57: 1027-34.
Way M, Hill GE. Intraoperative end-tidal carbon dioxide concentrations: what is the target? Anesthesiol Res Pract 2011; DOI: https://doi.org/10.1155/2011/271539.
Pinsky MR. Cardiovascular effects of ventilatory support and withdrawal. Anesth Analg 1994; 79: 567-76.
Lele EE, Hantos Z, Bitay M, et al. Bronchoconstriction during alveolar hypocapnia and systemic hypercapnia in dogs with a cardiopulmonary bypass. Respir Physiol Neurobiol 2011; 175: 140-5.
Enoki T, Tsuchiya N, Shinomura T, Nomura R, Fukuda K. Effect of hypercapnia on arterial hypotension after induction of anaesthesia. Acta Anaesthesiol Scand 2005; 49: 687-91.
Fleischmann E, Herbst F, Kugener A, et al. Mild hypercapnia increases subcutaneous and colonic oxygen tension in patients given 80% inspired oxygen during abdominal surgery. Anesthesiology 2006; 104: 944-9.
Contreras M, Ansari B, Curley G, et al. Hypercapnic acidosis attenuates ventilation-induced lung injury by a nuclear factor-kappaB-dependent mechanism. Crit Care Med 2012; 40: 2622-30.
Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 1998; 338: 347-54.
Akkermans A, van Waes JA, Peelen LM, Rinkel GJ, van Klei WA. Blood pressure and end-tidal carbon dioxide ranges during aneurysm occlusion and neurologic outcome after an aneurysmal subarachnoid hemorrhage. Anesthesiology 2019; 130: 92-105.
Muizelaar JP, Marmarou A, Ward JD, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg 1991; 75: 731-9.
Nin N, Muriel A, Peñuelas O, et al. Severe hypercapnia and outcome of mechanically ventilated patients with moderate or severe acute respiratory distress syndrome. Intensive Care Med 2017; 43: 200-8.
Akkermans A, van Waes JA, Thompson A, et al. An observational study of end-tidal carbon dioxide trends in general anesthesia. Can J Anesth 2019; 66: 149-60.
Dony P, Dramaix M, Boogaerts JG. Hypocapnia measured by end-tidal carbon dioxide tension during anesthesia is associated with increased 30-day mortality rate. J Clin Anesth 2017; 36: 123-6.
Wax DB, Lin HM, Hossain S, Porter SB. Intraoperative carbon dioxide management and outcomes. Eur J Anaesthesiol 2010; 27: 819-23.
Park JH, Lee HM, Kang CM, et al. Correlation of intraoperative end-tidal carbon dioxide concentration on postoperative hospital stay in patients undergoing pylorus-preserving pancreaticoduodenectomy. World J Surg 2021; DOI: https://doi.org/10.1007/s00268-021-05984-x.
Mizota T, Dong L, Takeda C, et al. Invasive respiratory or vasopressor support and/or death as a proposed composite outcome measure for perioperative care research. Anesth Analg 2019; 129: 679-85.
Mizota T, Dong L, Takeda C, et al. Transient acute kidney injury after major abdominal surgery increases chronic kidney disease risk and 1-year mortality. J Crit Care 2019; 50: 17-22.
Bryant AS, Rudemiller K, Cerfolio RJ. The 30- versus 90-day operative mortality after pulmonary resection. Ann Thorac Surg 2010; 89: 1717-23.
Joung RH, Merkow RP. Is it time to abandon 30-day mortality as a quality measure? Ann Surg Oncol 2021; 28: 1263-4.
Damhuis RA, Wijnhoven BP, Plaisier PW, Kirkels WJ, Kranse R, van Lanschot JJ. Comparison of 30-day, 90-day and in-hospital postoperative mortality for eight different cancer types. Br J Surg 2012; 99: 1149-54.
Shaw AD, Bagshaw SM, Goldstein SL, et al. Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to Plasma-Lyte. Ann Surg 2012; 255: 821-9.
Myles PS, Bellomo R, Corcoran T, et al. Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med 2018; 378: 2263-74.
Burnum JF, Hickam JB, McIntosh HD. The effect of hypocapnia on arterial blood pressure. Circulation 1954; 9: 89-95.
Wong KC, Schafer PG, Schultz JR. Hypokalemia and anesthetic implications. Anesth Analg 1993; 77: 1238-60.
Curley G, Kavanagh BP, Laffey JG. Hypocapnia and the injured brain: more harm than benefit. Crit Care Med 2010; 38: 1348-59.
Takahashi CE, Brambrink AM, Aziz MF, et al. Association of intraprocedural blood pressure and end tidal carbon dioxide with outcome after acute stroke intervention. Neurocrit Care 2014; 20: 202-8.
Hovorka J. Carbon dioxide homeostasis and recovery after general anaesthesia. Acta Anaesthesiol Scand 1982; 26: 498-504.
Wollman SB, Orkin LR. Postoperative human reaction time and hypocarbia during anaesthesia. Br J Anaesth 1968; 40: 920-6.
Abdalrazik FS, Elghonemi MO. Assessment of gradient between partial pressure of arterial carbon dioxide and end-tidal carbon dioxide in acute respiratory distress syndrome. Egypt J Bronchol 2019; 13: 170-5.
Tyburski JG, Carlin AM, Harvey EH, Steffes C, Wilson RF. End-tidal CO2-arterial CO2 differences: a useful intraoperative mortality marker in trauma surgery. J Trauma 2003; 55: 892-6.
Campion EM, Robinson CK, Brant N, et al. End-tidal carbon dioxide underestimates plasma carbon dioxide during emergent trauma laparotomy leading to hypoventilation and misguided resuscitation: a Western Trauma Association Multicenter Study. J Trauma Acute Care Surg 2019; 87: 1119-24.
Shetty A, Sparenberg S, Adams K, et al. Arterial to end-tidal carbon dioxide tension difference (CO2 gap) as a prognostic marker for adverse outcomes in emergency department patients presenting with suspected sepsis. Emerg Med Australas 2018; 30: 794-801.
Isserles SA, Breen PH. Can changes in end-tidal PCO2 measure changes in cardiac output? Anesth Analg 1991; 73: 808-14.
Jin X, Weil MH, Tang W, et al. End-tidal carbon dioxide as a noninvasive indicator of cardiac index during circulatory shock. Crit Care Med 2000; 28: 2415-9.
Maslow A, Stearns G, Bert A, et al. Monitoring end-tidal carbon dioxide during weaning from cardiopulmonary bypass in patients without significant lung disease. Anesth Analg 2001; 92: 306-13.
Shibutani K, Muraoka M, Shirasaki S, Kubal K, Sanchala VT, Gupte P. Do changes in end-tidal PCO2 quantitatively reflect changes in cardiac output? Anesth Analg 1994; 79: 829-33.
Akça O, Kurz A, Fleischmann E, et al. Hypercapnia and surgical site infection: a randomized trial. Br J Anaesth 2013; 111: 759-67.
Coakley RJ, Taggart C, Greene C, McElvaney NG, O'Neill SJ. Ambient pCO2 modulates intracellular pH, intracellular oxidant generation, and interleukin-8 secretion in human neutrophils. J Leukoc Biol 2002; 71: 603-10.
Marhong J, Fan E. Carbon dioxide in the critically ill: too much or too little of a good thing? Respir Care 2014; 59: 1597-605.
Jaber S, Jung B, Sebbane M, et al. Alteration of the piglet diaphragm contractility in vivo and its recovery after acute hypercapnia. Anesthesiology 2008; 108: 651-8.
Jaitovich A, Angulo M, Lecuona E, et al. High CO2 levels cause skeletal muscle atrophy via AMP-activated kinase (AMPK), FoxO3a protein, and muscle-specific Ring finger protein 1 (MuRF1). J Biol Chem 2015; 290: 9183-94.
Author contributions
Li Dong conceptualized the study. Li Dong, Chikashi Takeda, Toshiyuki Mizota, and Yosuke Yamamoto designed the study. Li Dong and Toshiyuki Mizota collected data. All authors analyzed and interpreted data. Li Dong drafted the manuscript. All authors edited and approved the manuscript.
Acknowledgements
We are grateful to Mr Yoshihiro Kinoshita, Ms Tomoko Hosoya, and Mr Yohei Taniguchi (Medical Information Systems Section, Management Division, Kyoto University Hospital, Kyoto, Japan) for their assistance in data collection for this study.
Disclosures
None.
Funding statement
This work was supported in part by the Japan Society for the Promotion of Science KAKENHI program (grant number: 20K09242, principal investigator: Toshiyuki Mizota) and the 2019 Kyoto University ISHIZUE Research Development Program (principal investigator: Toshiyuki Mizota).
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is accompanied by an editorial. Please see Can J Anesth 2021; this issue.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dong, L., Takeda, C., Yamazaki, H. et al. Intraoperative end-tidal carbon dioxide and postoperative mortality in major abdominal surgery: a historical cohort study. Can J Anesth/J Can Anesth 68, 1601–1610 (2021). https://doi.org/10.1007/s12630-021-02086-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-02086-z