Abstract
Background
The objective of this study was to determine the clinical usefulness of videolaryngoscopes (VLs) by comparing the time to intubation (TTI) and the ease of intubation of McGrath MAC VL (MVL), Pentax Airway Scope VL (PVL), and Macintosh direct laryngoscope (DL) during nasotracheal intubation using manual in-line stabilization to simulate difficult airways.
Methods
One hundred and twenty patients were randomly assigned to the MVL group (n = 40), the PVL group (n = 40), and the DL group (n = 40). Nasotracheal intubation was performed using MVL, PVL, or DL, according to group assignments. The primary outcome was TTI and secondary outcomes were glottic view, ease of intubation, and bleeding.
Results
The TTI was significantly shorter in the MVL group than in the DL group (45 sec vs 57 sec; difference in means: − 12; 95% confidence interval [CI], − 21 to − 3; P = 0.01). The percentage of glottic opening and Cormack Lehane grade were significantly superior in the MVL and the PVL groups compared with the DL group (both P < 0.001). The intubation difficulty scale and numeric rating scale regarding ease of intubation were also significantly lower in the MVL and PVL groups than in the DL group (all P < 0.007). The incidence of bleeding was significantly lower in the MVL group than in the DL group (3 vs 15, relative risk 0.2; 95% CI, 0.06 to 0.64; P = 0.001).
Conclusion
This study showed that both MVL and PVL provided better visualization of the glottis and easier intubation, with less additional manipulation than DL during nasotracheal intubation in simulated difficult airways. Additionally, use of the MVL significantly shortened the TTI compared with the DL.
Trial registration
www.clinicaltrials.gov (NCT02647606); registered 6 January, 2016.
Résumé
Contexte
L’objectif de cette étude était de déterminer l’utilité clinique des vidéolaryngoscopes (VL) en comparant le temps jusqu’à intubation (TTI) et la facilité d’intubation du VL McGrath MAC (MVL), du VL Pentax Airway Scope (PVL), et du laryngoscope avec lame Macintosh (DL) pour une intubation nasotrachéale avec stabilisation manuelle en ligne simulant des voies aériennes difficiles.
Méthode
Cent vingt patients ont été aléatoirement alloués au groupe MVL (n = 40), au groupe PVL (n = 40) ou au groupe DL (n = 40). L’intubation nasotrachéale a été réalisée à l’aide du MVL, du PVL ou du DL selon l’attribution de groupe. Le critère d’évaluation principal était le TTI et les critères secondaires comprenaient la visualisation glottique, la facilité d’intubation et les saignements.
Résultats
Le TTI était significativement plus court dans le groupe MVL que dans le groupe DL (45 sec vs 57 sec; différence de moyennes : -12; intervalle de confiance [IC] 95 %, -21 à -3; P = 0,01). Le pourcentage d’ouverture glottique et le grade de Cormack et Lehane étaient significativement supérieurs dans les groupes MVL et PVL par rapport au groupe DL (P < 0,001 pour les deux). L’échelle de difficulté d’intubation et l’échelle d’évaluation numérique concernant la facilité d’intubation étaient également significativement plus basses dans les groupes MVL et PVL que dans le groupe DL (tous P < 0,007). L’incidence de saignements était significativement plus basse dans le groupe MVL que dans le groupe DL (3 vs 15, risque relatif 0,2; IC 95 %, 0,06 à 0,64; P = 0,001).
Conclusion
Cette étude a démontré que le MVL et le PVL procuraient tous deux une meilleure visualisation glottique et une intubation plus facile, avec moins de manipulations supplémentaires qu’un DL pendant l’intubation nasotrachéale de voies aériennes difficiles simulées. En outre, l’utilisation d’un MVL a significativement réduit le TTI par rapport à un DL.
Enregistrement de l’étude
www.clinicaltrials.gov (NCT02647606); enregistrée le 6 janvier 2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A variety of videolaryngoscopes (VLs) have been developed since the early 2000s to solve difficult airway problems.1 Several types of VLs are available, each with different strengths and weaknesses, which are useful for a variety of situations. Many studies are ongoing to evaluate the usefulness of VLs under a variety of clinical situations.2,3
The McGrath MAC VL (Covidien, Mansfield, MA, USA) (MVL) is a non-channelled Macintosh direct laryngoscope (DL)-shaped VL.1 It has a display monitor at the top of the handle and can present superior glottis views in both normal and difficult airways compared with the DL.4,5 Because the MVL is structurally similar to the DL, an anesthesiologist familiar with DLs may prefer the device. In addition, direct glottic views can be obtained at any time during intubation, even when the glottis is not visible because of secretions or fog.3,6
The Pentax Airway Scope VL (Pentax Co., Tokyo, Japan) (PVL) is a channelled indirect VL. It has a disposable blade with two channels, a monitor, and an image tube containing a camera. The endotracheal tube (ETT) is inserted into the channel of a curved blade, which resembles the curvature of the pharynx and the larynx. After inserting the blade into the mouth and targeting the glottic opening on the monitor, an ETT can be inserted through the vocal cords.7 The PVL can improve the glottic view and difficulty of intubation, thus increasing the success rate of intubation during management of difficult airways. It may be especially helpful in cases where the oral-pharyngeal-laryngeal axis is not aligned, such as in cases of limited cervical motion.8
Videolaryngoscopes can be quite useful for nasotracheal intubations, as well as for orotracheal intubations. A few studies have evaluated their strengths during nasotracheal intubations in normal airways and found that VLs can offer better glottic view, easier intubation, shorter time to intubation (TTI), and less additional manipulations.9,10,11,12,13 Nevertheless, a randomized-controlled study examining the efficacy of VLs during nasotracheal intubation in difficult airway situations has not yet been published. Thus, the objective of this study was to determine the clinical usefulness of VLs by comparing the TTI and the ease of intubation using intubation difficulty scale (IDS) and numeric rating scale (NRS) for MVL, PVL, and DL in nasotracheal intubations performed under manual in-line stabilization (MILS) to simulate difficult airways.
Methods
After obtaining approval from the Institutional Review Board of Ajou University Hospital, Suwon, Korea (approval number: AJIRB-MED-DE1-15-334), the study was registered at ClinicalTrials.gov (NCT02647606). Patients aged between 19 and 60 yr with an American Society of Anesthesiologist physical status of I or II, scheduled for dental or maxillofacial surgery requiring nasotracheal intubation between January 2016 and February 2017 were screened and enrolled following written informed consent. Patients with anticipated difficult airways (Mallampati scores, class IV), requiring rapid sequence induction, with cervical spine injuries, and with bleeding tendencies were excluded. According to the randomization table obtained from www.random.org, patients were assigned to one of three groups (MVL, PVL, and DL groups) at a ratio of 1:1:1. During preoperative evaluation, airway assessment, including Mallampati score, inter-incisor distance with mouth opening, thyromental distance, neck mobility (normal, reduced, or fixed), and upper incisor status (normal, absent, or loose) was performed by one physician blinded to the group assignment.
Patients entered the operating room without premedication. In the operating room, standard monitoring devices, including electrocardiogram, non-invasive blood pressure monitor, pulse oximeter, and bispectral index (BIS; Covidien, Mansfield, MA, USA) were applied. After three minutes of preoxygenation, anesthesia was induced with propofol (effect site concentration [Ce] of 5.0 μg·mL−1) and remifentanil (Ce of 4.0 ng·mL−1) using an Orchestra® target-controlled infusion pump (Fresenius Vial, Brezins, France). When the BIS value dropped below 60, 0.6 mg·kg−1 of rocuronium was administered and cotton swabs soaked with 0.1 % epinephrine were packed into the right nasal cavity to prevent nasal bleeding. After two minutes of manual ventilation with 100% oxygen, the neuromuscular block was confirmed by a loss of train-of-four response with a peripheral nerve stimulator. An assistant removed the pillow and applied MILS by grasping the patient’s mastoid processes and occiput to minimize head and neck mobility during nasotracheal intubation.14 Two physicians (K.J.Y. and R.G.) who had experienced more than 50 intubations with three different laryngoscopes performed nasotracheal intubations with the Polar™ Preformed Tracheal Tube (Smith Medical International Ltd., UK), pre-warmed and lubricated with a water-soluble jelly. A 6.5 mm tracheal tube used for males and a 6.0 mm tube was used for females. The nasotracheal tube was inserted into the nostril until its tip passed through the posterior naris. If significant bleeding obscured the glottis view and hindered intubation, the patient was excluded from the study at that time. MVL, PVL, or DL was introduced into the mouth and the nasotracheal tube was advanced according to group assignments. In the PVL group, the blade tip of PVL was positioned posteriorly to the epiglottis to directly elevate the epiglottis, according to the manufacturer’s recommendation for standard orotracheal intubation.
The primary outcome measure was TTI. An observer faced the monitor located on the right side of the patient. A screen between the patient and the monitor blinded the observer to the device assignment. The observer constantly watched the monitor and measured TTI from the intranasal placement of the tube to the detection of carbon dioxide by capnography. Intubation was considered a failure if peripheral capillary oxygen saturation (SpO2) dropped below 95% during intubation. It was also considered a failure if the intubation took more than 90 sec, even if there was no desaturation during the intubation. The latter was included in the analysis. If SpO2 dropped below 95% during intubation, a second trial was performed without MILS by manipulating the head–neck position after manual ventilation. During the intubation, intubation physicians assessed Cormack Lehane grade (CL grade), percentage of the glottic opening (POGO), and the use of external laryngeal manipulation (ELM) or Magill forceps. Magill forceps were used if the nasal tube tip did not align with the glottis during either left or right rotation of the tube at the external nostrils or ELM. After nasotracheal intubation, the ease of intubation was assessed using IDS15 and NRS (ten-point scale: 0 = easy and 10 = difficult). Oropharyngeal bleeding was checked using Yankauer suction and was graded as none, trace, moderate, or severe.11 Hemodynamics and BIS values were recorded before induction, one minute after induction, before intubation, and one minute after intubation. Bleeding and vital signs were recorded by the observer recording the TTI.
Statistical analysis
The sample size was calculated based on previous studies using DLs, in which the mean (standard deviation) duration of nasotracheal intubation ranged from 38.3–44.9 (6.2–15.6) sec.9,16 Under the assumption that a ten-second between-group difference was clinically significant, the sample size was calculated to be 37 patients for each group, based on conservative numbers from previous reports at 80% power and a significance level of 0.05.12,13 Considering the possibility of participant drop-out during the study, 40 patients were recruited for each group. Statistical analyses were performed with IBM SPSS statistics version 21.0 (Armonk, NY, USA). Continuous variables were evaluated with one-way analysis of variance. Post-hoc comparisons were performed to detect any significant pairwise differences between the groups. Categorical variables were analyzed using Chi-square test or Fisher’s exact test with the Bonferroni correction for multiple comparisons. P values less than 0.0167 (0.05/3) were considered statistically significant.
Results
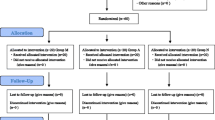
One hundred and twenty patients were enrolled, and follow-up evaluations were conducted on all patients during the study (Figure). Patients’ characteristics were comparable among groups (Table 1).
Intubation-related profiles are listed in Tables 2 (continuous outcomes) and 3 (categorical outcomes). Time to intubation was significantly shorter in the MVL group than in the DL group (45 s vs 57 sec; difference in means, −12; 95% CI, −21 to −3; P = 0.01). Percentage of the glottic opening scores in the MVL and PVL groups were significantly superior to those in the DL group. Intubation difficulty scale scores were significantly lower in the MVL and PVL groups than in the DL group. Numeric rating scale scores were also significantly lower in the MVL and PVL groups than in the DL group (Table 2).
The number of patients with CL grade 1 was significantly higher in the MVL and PVL groups than in the DL group. The need for an ELM was lower in the MVL and PVL groups than in the DL group. The use of Magill forceps was lower in the MVL and PVL groups than in the DL group (Table 3). No patient presented with significant bleeding during insertion of the nasotracheal tube into the nostril. The incidence of bleeding was significantly lower in the MVL group than in the DL group (none/trace/moderate, 37/3/0 vs 25/13/2) (Table 3). Hemodynamic variables, including mean arterial pressure and heart rate, and BIS values were not significantly different between the groups throughout this study (data not shown).
Discussion
This study showed that both MVL and PVL could provide better glottic views and easier intubation during nasotracheal intubation under MILS compared with DL. Use of the MVL also significantly reduced the TTI and the incidence of bleeding during intubation compared with DL.
It is well known that VLs can provide a better view of the glottis than DL. They are especially helpful during the management of difficult airways.17,18 In this study, MVL and PVL showed improved glottic views during nasotracheal intubation of patients with simulated difficult airways, compared with DL. These results were consistent with previous reports on patients with normal airways.9,10 According to Jones’s report comparing GlideScope with DL for nasotracheal intubation, GlideScope provides superior glottis view, easier intubation, and shorter TTI.11 In other studies of orotracheal intubation, MVL and PVL showed improved POGO scale and CL grade in patients with simulated difficult airways,8,14 consistent with our results. In the present study, POGO scales were over 75% and more than 50% of the patients showed a CL grade of 1 in both the MVL and PVL groups. On the other hand, patients in the DL group showed an average POGO scale of 25% and only one patient had a CL grade of 1. Therefore, VL might be a better choice than DL to obtain superior glottic views for nasotracheal intubation in cases where a difficult airway is expected.
In this study, the ease of intubation was significantly better in the MVL and PVL groups than in the DL group, based on evaluations using IDS and NRS. These results could be due to the better glottic views provided by these two VLs. In most orotracheal intubation studies comparing VLs with DL, the glottic views and ease of intubation tended to be better,18 consistent with our results. Nevertheless, a superior glottic view does not always guarantee successful intubation,19 and vice versa, a poor glottic view does not always result in a failed intubation. Studies have reported that most physicians successfully intubated over 95% of patients using DLs.20,21 A previous study with the GlideScope reported that persistent attempts to achieve a full glottic view resulted in slower and more difficult intubations than accepting a restricted glottic view.22 The authors suggested that obtaining a full laryngeal view might not be desirable during intubation using the GlideScope.22
In this study, VLs showed a slight discrepancy in the time and success rate of intubation at the first attempt, despite providing better glottic views. Only the MVL group significantly shortened the TTI and the first attempt failure numbers were similar among the groups in this study. An earlier study comparing MVL, PVL, and DL in normal airways during routine nasotracheal intubations reported that only MVL shortened the TTI, although PVL showed better glottic views compared with MVL.23 Several factors might explain these results. First, PVL has a curved blade resembling the anatomy of the upper airway with two channels. It is much bigger than the blade of traditional DL or MVL.24 The bulky blade of PVL can make it difficult to insert a PVL into the mouth, which might increase the TTI. In a previous study comparing MVL and PVL during orotracheal intubation, although PVL provided superior glottic view over MVL, the TTI and ease of intubation were similar between the two devices.25 Second, it may be difficult to direct the tube tip into the glottis. PVL is designed for orotracheal intubation, while the ETT is inserted into the channel during intubation. Nevertheless, because the ETT cannot be preloaded into the channel of PVL for nasotracheal intubation, even if the glottic visualization is excellent, insertion might be difficult when the tube is located posteriorly or laterally to the glottis.26,27 When the tube is located posteriorly in the pharynx, positioning of the PVL blade close to the anterior commissure of the vocal cords with direct elevation of the epiglottis may not provide enough space for ETT manipulation towards the glottis.10 In addition, when using PVL, there might not be enough space to efficiently manipulate the tube with Magill forceps.23 In this study, Magill forceps were used in two cases in the PVL group to advance the tube tip into the glottic inlet. Nevertheless, Magill forceps did not immediately advance the tube tip. Therefore, repeated attempt to redirect the tube tip into the glottis inlet increased the TTI. On the other hand, only one case needed Magill forceps in the MVL group, which may have reduced the TTI in this group as less time was spent manipulating with the forceps.11 In addition, PVL has a hyper-curved, angulated blade, while MVL has a less angulated blade, similar to DL.1 In a study of the GlideScope with a hyper-curved blade, an intentionally restricted glottic view was associated with faster and easier intubations compared with cases with full glottic views.22 During the use of GlideScope, the full view of the glottis may interfere with tube insertion by increasing the mismatch of the tube tip and the trachea.22
Patients in the MVL group had significantly less bleeding than those in the DL group in this study. A previous study comparing three laryngoscopes in routine nasotracheal intubations reported no bleeding in any group.23 In another study comparing MVL and DL, the incidence of bleeding was 14% and 31%, respectively, without a significant difference.9 In the DL group of this study, poor glottic view increased the difficulty of intubation by MILS,28 and additional manipulations, such as ELM and Magill forceps might have resulted in additional trauma to the oral cavity and upper airway. On the contrary, in the MVL group, better glottic view and less manipulation would together reduce the bleeding significantly. In the PVL group, the bulky blade might have caused trauma during insertion and removal. Pentax Airway Scope VL has been associated with more dental clicks and compression, representing trauma to patient airways.29 Additionally, repeated attempts to advance the ETT into the glottic opening and readjusting the PVL and ETT might be causes of bleeding.
During nasotracheal intubation, the overall TTI of this study was about 10–20 sec longer than those of previous reports in normal airways.9,10,23 This discrepancy might be due to the difficult airway simulation using MILS in the present study. Restriction of cervical motion can make laryngoscopy more difficult because the oral-pharyngeal-laryngeal axes are not aligned, which could prolong the TTI.28
Because awake fibreoptic intubation is recommended as a standard technique in difficult airway management, it would be considered the first choice of technique when difficult airway is anticipated. On the other hand, in unexpected difficult airway situations, VLs might be helpful because they can be applied quickly and easily.18 In addition, various VLs can be used during awake intubation.30 This study is helpful because it explores the usefulness of various types of VLs in nasotracheal intubation with simulated difficult airway situations.
This study has several limitations. First, it was not possible to blind the intubating physicians to which laryngoscope was used. Second, the intubating physicians had sufficient experience with VL intubations, but were more familiar with non-channelled blades, like those used in MVL or DL, than channelled blades used in PVL. The physicians’ familiarity with MVL might have reduced the intubation times, especially in patients with MILS that simulated difficult airway conditions. Since experienced anesthetists were able to achieve similar intubation times and ease of intubations with PVL and MVL in patients with normal airways,25 further studies about the experience of intubation with VLs are needed. Third, the blade tip of PVL was positioned behind the epiglottis for direct elevation in our study. If an indirect technique with the blade tip placed in the vallecula for elevation of the epiglottis had been used, it could have affected the results.10 Fourth, the bleeding was assessed after ETT insertion into the nostril and there was no significant bleeding related to ETT insertion. Nevertheless, bleeding can be disastrous if encountered before confirming that a glottic view can be obtained. Therefore, it would be more reasonable to verify glottic view before inserting the ETT into the nostril.31 Lastly, this study did not include the GlideScope, one of the most popular VLs in current clinical practice,1,11,12,13 because of its limited availability at our institute.
In conclusion, both MVL and PVL provided better visualization of the glottis and easier intubation with less additional manipulation than DL during nasotracheal intubation with MILS as a simulation of a difficult airway. Additionally, use of the MVL significantly shortened the TTI compared with the DL.
References
Pieters BM, Eindhoven GB, Acott C, van Zundert AA. Pioneers of laryngoscopy: indirect, direct and video laryngoscopy. Anaesth Intensive Care 2015; 43(Suppl): 4-11.
Niforopoulou P, Pantazopoulos I, Demestiha T, Koudouna E, Xanthos T. Video-laryngoscopes in the adult airway management: a topical review of the literature. Acta Anaesthesiol Scand 2010; 54: 1050-61.
Pieters BM, Wilbers NE, Huijzer M, Winkens B, van Zundert AA. Comparison of seven videolaryngoscopes with the Macintosh laryngoscope in manikins by experienced and novice personnel. Anaesthesia 2016; 71: 556-64.
Shippey B, Ray D, McKeown D. Case series: the McGrath videolaryngoscope–an initial clinical evaluation. Can J Anesth 2007; 54: 307-13.
Shippey B, Ray D, McKeown D. Use of the McGrath videolaryngoscope in the management of difficult and failed tracheal intubation. Br J Anaesth 2008; 100: 116-9.
Komasawa N, Kido H, Mihara R, Minami T. Comparison of cricoid pressure effect between McGRATH(R) MAC and Pentax-AWS Airwayscope(R): a prospective randomized trials. Am J Emerg Med 2017; 35: 576-8.
Asai T, Enomoto Y, Shimizu K, Shingu K, Okuda Y. The Pentax-AWS video-laryngoscope: the first experience in one hundred patients. Anesth Analg 2008; 106: 257-9.
Malik MA, Maharaj CH, Harte BH, Laffey JG. Comparison of Macintosh, Truview EVO2, Glidescope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth 2008; 101: 723-30.
Kwak HJ, Lee SY, Lee SY, Cho SH, Kim HS, Kim JY. McGrath video laryngoscopy facilitates routine nasotracheal intubation in patients undergoing oral and maxillofacial surgery: a comparison with Macintosh laryngoscopy. J Oral Maxillofac Surg 2016; 74: 256-61.
Suzuki A, Onodera Y, Mitamura SM, et al. Comparison of the Pentax-AWS airway scope with the Macintosh laryngoscope for nasotracheal intubation: a randomized, prospective study. J Clin Anesth 2012; 24: 561-5.
Jones PM, Armstrong KP, Armstrong PM, et al. A comparison of Glidescope videolaryngoscopy to direct laryngoscopy for nasotracheal intubation. Anesth Analg 2008; 107: 144-8.
Hirabayashi Y. GlideScope® videolaryngoscope facilitates nasotracheal intubation. Can J Anesth 2006; 53: 1163.
Xue F, Zhang G, Liu J, et al. A clinical assessment of the Glidescope videolaryngoscope in nasotracheal intubation with general anesthesia. J Clin Anesth 2006; 18: 611-5.
Taylor AM, Peck M, Launcelott S, et al. The McGrath® Series 5 videolaryngoscope vs the Macintosh laryngoscope: a randomised, controlled trial in patients with a simulated difficult airway. Anaesthesia 2013; 68: 142-7.
Adnet F, Borron SW, Racine SX, et al. The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology 1997; 87: 1290-7.
Lili X, Zhiyong H, Jianjun S. A comparison of the GlideScope with the Macintosh laryngoscope for nasotracheal intubation in patients with ankylosing spondylitis. J Neurosurg Anesthesiol 2014; 26: 27-31.
Asai T. Videolaryngoscopes: do they truly have roles in difficult airways? Anesthesiology 2012; 116: 515-7.
Lewis SR, Butler AR, Parker J, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation. Cochrane Database Syst Rev 2016; 11: CD011136.
Hwang SM. A good laryngeal view does not guarantee perfectly successful tracheal intubation. Korean J Anesthesiol 2016; 69: 111-2.
Koh LK, Kong CE, Ip-Yam PC. The modified Cormack-Lehane score for the grading of direct laryngoscopy: evaluation in the Asian population. Anaesth Intensive Care 2002; 30: 48-51.
Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology 2005; 103: 429-37.
Gu Y, Robert J, Kovacs G, et al. A deliberately restricted laryngeal view with the GlideScope® video laryngoscope is associated with faster and easier tracheal intubation when compared with a full glottic view: a randomized clinical trial. Can J Anesth 2016; 63: 928-37.
Sato Boku A, Sobue K, Kako E, et al. The usefulness of the McGrath MAC laryngoscope in comparison with Airwayscope and Macintosh laryngoscope during routine nasotracheal intubation: a randomaized controlled trial. BMC Anesthesiol 2017; 17: 160.
Tseng KY, Lu IC, Shen YC, Lin CH, Chen PN, Cheng KI. A comparison of the video laryngoscopes with Macintosh laryngoscope for nasotracheal intubation. Asian J Anesthesiol 2017; 55: 17-21.
Lee J, Kwak HJ, Lee JY, Chang MY, Lee SY, Kim JY. Comparison of the Pentax AirwayScope and McGrath MAC videolaryngoscope for endotracheal intubation in patients with a normal airway. Medicine (Baltimore) 2017; 96: e8713.
Xue FS, Liu JH, Liao X, Yuan YJ. Use of cuff inflation to facilitate nasotracheal intubation with the Airway Scope. Anaesthesia 2011; 66: 754.
Li RP, Xue FS, Wang SY. Nasotracheal intubation with airway scope. J Anesth 2016; 30: 360.
Heath KJ. The effect of laryngoscopy of different cervical spine immobilisation techniques. Anaesthesia 1994; 49: 843-5.
Hoshijima H, Kuratani N, Hirabayashi Y, Takeuchi R, Shiga T, Masaki E. Pentax Airway Scope® vs Macintosh laryngoscope for tracheal intubation in adult patients: a systematic review and meta-analysis. Anaesthesia 2014; 69: 911-8.
Alhomary M, Ramadan E, Curran E, Walsh SR. Videolaryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation: a systematic review and meta-analysis. Anaesthesia 2018; 73: 1151-61.
Piepho T, Thierbach A, Werner C. Nasotracheal intubation: look before you leap. Br J Anaesth 2005; 94: 859-60.
Conflicts of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Associate Editor, Canadian Journal of Anesthesia.
Author contributions
Go Un Roh and Jong Yeop Kim were involved in the study design, acquisition and interpretation of data, and writing of the manuscript. Hyun Jeong Kwak wrote the manuscript. Kyung Cheon Lee interpreted the data. Sun Young Lee analyzed the data.
Funding
No external funding, solely departmental source.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roh, G.U., Kwak, H.J., Lee, K.C. et al. Randomized comparison of McGrath MAC videolaryngoscope, Pentax Airway Scope, and Macintosh direct laryngoscope for nasotracheal intubation in patients with manual in-line stabilization. Can J Anesth/J Can Anesth 66, 1213–1220 (2019). https://doi.org/10.1007/s12630-019-01409-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-019-01409-5