Abstract
Purpose
The purpose of the current study was to evaluate the effects of pregabalin administration as an adjunct to fentanyl-based intravenous patient-controlled analgesia on opioid consumption and postoperative pain following arthroscopic shoulder surgery.
Methods
In this randomized controlled trial, 60 adult patients undergoing arthroscopic shoulder surgery were randomly assigned to receive either pregabalin 150 mg (Pregabalin group, n = 30) or placebo (Control group, n = 30) one hour before anesthetic induction. The primary outcome was the cumulative amount of fentanyl consumption during 48 hr postoperatively. Secondary outcomes were pain intensity, the number of rescue analgesics administered, and adverse effects related to the analgesic regimen, which were serially assessed during 48 hr postoperatively.
Results
The cumulative fentanyl consumption during 48 hr postoperatively was significantly lower in the Pregabalin group than in the Control group ([1,126.0 (283.6) μg vs 1,641.4 (320.3) μg, respectively; mean difference, 515.4 μg; 95% confidence interval [CI], 359.0 to 671.8; P = < 0.001). Numeric rating scores for pain (0 to 10) were significantly lower in the Pregabalin group at six hours (mean difference, 2.9; 95% CI, 1.8 to 4.0), 24 hr (mean difference, 2.9; 95% CI, 1.9 to 3.8), and 48 hr (mean difference, 1.5; 95% CI, 0.6 to 2.3). The incidence of adverse effects related to the analgesic regimens, including nausea, sedation, and dizziness, were similar between the two groups.
Conclusion
A preoperative dose of pregabalin 150 mg administered before arthroscopic shoulder surgery resulted in significant analgesic efficacy for 48 hr in terms of opioid-sparing effect and improved pain intensity scores without influencing complications. This trial was registered at: http://cris.nih.go.kr, number CT0000578.
Résumé
Objectif
L’objectif de cette étude était d’évaluer les effets d’une administration de prégabaline comme supplément à une analgésie contrôlée par le patient intraveineuse à base de fentanyl sur la consommation d’opioïdes et la douleur postopératoire après une arthroscopie de l’épaule.
Méthode
Dans cette étude randomisée contrôlée, 60 patients adultes subissant une arthroscopie de l’épaule ont été randomisés à recevoir soit 150 mg de prégabaline (groupe prégabaline, n = 30), ou un placebo (groupe témoin, n = 30) une heure avant l’induction de l’anesthésie. Le critère d’évaluation principal était la quantité cumulée de fentanyl consommée durant les premières 48 h postopératoires. Les critères secondaires comprenaient l’intensité de la douleur, le nombre d’analgésiques de sauvetage administrés et les effets secondaires liés au régime analgésique, lesquels ont été évalués en série pendant 48 h après l’intervention.
Résultats
La consommation cumulée de fentanyl pendant 48 h postopératoires était significativement plus basse dans le groupe prégabaline que dans le groupe témoin ([1126,0 (283,6) µg vs 1641,4 (320,3) µg, respectivement; différence moyenne, 515,4 µg; intervalle de confiance [IC] 95 %, 359,0 à 671,8; P = < 0,001). Les scores d’évaluation numérique de la douleur (0 à 10) étaient significativement plus bas dans le groupe prégabaline à six heures (différence moyenne, 2,9; IC 95 %, 1,8 à 4,0), 24 h (différence moyenne, 2,9; IC 95 %, 1,9 à 3,8), et 48 h (différence moyenne, 1,5; IC 95 %, 0,6 à 2,3). L’incidence d’effets secondaires néfastes liés aux régimes analgésiques, y compris la nausée, la sédation et les étourdissements, étaient semblables dans les deux groupes.
Conclusion
Une dose préopératoire de 150 mg de prégabaline administrée avant une arthroscopie de l’épaule a entraîné une efficacité analgésique significative durant 48 h en termes de réduction en besoin d’opioïdes et a amélioré les scores d’intensité de la douleur sans influencer les complications. Cette étude a été enregistrée au: http://cris.nih.go.kr, numéro CT0000578.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Apart from patient perceptions of discomfort, postoperative pain after arthroscopic shoulder surgery is also known to complicate the postoperative course by hindering patient early mobilization and rehabilitation.1 Accordingly, there have been many studies on various methods to control postoperative pain after arthroscopic shoulder surgery, including subacromial/intra-articular infiltration of local anesthetic,2,3 suprascapular and/or axillary nerve block,4 and interscalene block.5,6 Notwithstanding their analgesic efficacy, however, these methods present procedural difficulties and are accompanied by complications inherent in their invasive nature.7
Among the noninvasive methods to control postoperative pain, intravenous opioid-based patient-controlled analgesia (IV-PCA) has been widely accepted as effective and safe. Yet IV-PCA is also accompanied by a high incidence of opioid-related adverse effects, including respiratory depression, pruritus, constipation, and nausea. The use of a multimodal analgesic regimen that incorporates non-opioids in conjunction with IV-PCA has been advocated as a standard practice to reduce opioid consumption without compromising the analgesic efficacy.8,9
In the same context, pregabalin, a ligand of the α2-δ subunit of presynaptic voltage-gated calcium channels widely used for neuropathic pain, has shown promising results as an adjunct to a multimodal approach for the control of postoperative pain without any apparent side effects.10-13 Considering the need for analgesic regimens that are specific to a particular surgical procedure, evidence is lacking regarding pregabalin’s efficacy on acute postoperative pain and its ability to provide an opioid-sparing effect following arthroscopic shoulder surgery.
In this prospective randomized controlled trial, we tested our hypothesis that pregabalin would decrease opioid consumption for postoperative pain control while providing sufficient analgesia in adult patients undergoing shoulder arthroscopic surgery during 48 hr postoperatively.
Methods
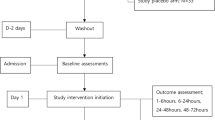
This study protocol was approved by the Ethical Committee of Kyungpook National University Hospital, a tertiary referral medical centre, in October 2012. Sixty adult patients (aged 20-65 yr) scheduled for arthroscopic shoulder surgery (Bankart or rotator cuff repair) during October 2012 to March 2013 provided their informed consent and were enrolled in the study. One day prior to the scheduled surgery, a staff member who was not involved in this study randomly assigned the patients to either the Control group (n = 30) or the Pregabalin group (n = 30) according to a computerized randomization table (without being blocked or stratified by procedure). The Control group received placebo capsules one hour before induction of anesthesia, and the Pregabalin group received pregabalin 150 mg at the same point in time. The hospital pharmacy prepared all medications in identical capsules, and an independent nurse who was not involved in this study administered the capsules orally with sips of water. Sealed envelopes were used to conceal group allocation from staff members involved in clinical care and from study participants collecting data. To ensure blinding, randomization results were not disclosed until data analysis. Exclusion criteria included patients with an American Society of Anesthesiologists physical status III or higher, those with a history of cardiovascular or respiratory disease, dizziness or frequent headaches, alcohol or substance abuse, daily intake of analgesics or intake of any analgesics within 48 hr preoperatively, impaired kidney or liver function, or an inability to use an IV-PCA device. The Figure displays the flow chart showing the patients’ enrolment for randomization.
Sedative premedication was withheld from all patients and standardized anesthetic and analgesic management was provided to all patients. Anesthesia was induced with propofol 2 mg·kg−1and remifentanil 0.5-1 μg·kg−1, and tracheal intubation was facilitated with rocuronium 0.6 mg·kg−1. Anesthesia was maintained with a continuous infusion of remifentanil 0.05-0.2 μg·kg−1·min−1 and sevoflurane 1.5-2.5 vol% to maintain a bispectral index score of 40-60. At the beginning of surgery, palonosetron 0.75 mg was administered intravenously. After surgery, the patients were turned to the supine position, sevoflurane was discontinued, and remifentanil was continued at an infusion rate of 0.02-0.05 μg·kg−1·min−1. Neuromuscular blockade was reversed with glycopyrrolate and pyridostigmine, and remifentanil was discontinued following tracheal extubation. After satisfactory recovery, the patients were taken to the postanesthesia care unit (PACU). The duration of anesthesia and surgery and the type of surgery were recorded.
After completion of the surgical procedure, IV-PCA was initiated using the AutoMed 3200® (ACE Medical, Korea). The IV-PCA regimen consisted of fentanyl 20 μg·kg−1 in 0.9% saline (total volume of 100 mL), and it was programmed to deliver a basal rate of 1 mL·hr−1 and 1 mL each time the patient pressed the activation button, with a 15 min lockout. If patients complained of pain ≥ 5 on the numeric rating scale (NRS), they were allowed to receive intravenous ketorolac 30 mg as a rescue drug according to their comfort and following the standard protocol.
The primary variable for determining efficacy was the opioid-sparing effect in terms of the total amount of cumulative fentanyl consumption during 48 hr postoperatively. Secondary variables for determining efficacy were pain intensity, the number of rescue analgesic drugs administered, and the incidence of nausea. Fentanyl consumption, pain intensity, rescue analgesic requirement, and nausea were further assessed upon arrival at the PACU and at six, 24, and 48 hr postoperatively. Adverse effects related to the multimodal analgesic regimen, including sedation, dizziness, headache, and visual disturbances, were also assessed for 48 hr postoperatively. Pain intensity was measured on a NRS for pain that ranged from 0 = no pain to 10 = worst pain imaginable. Sedation was assessed using a numeric score of 1-5 (1 = completely awake; 2 = awake but drowsy; 3 = asleep but responsive to verbal commands; 4 = asleep but responsive to tactile stimulus; 5 = asleep and not responsive to any stimulus). Patients with scores of 4 and 5 were regarded as sedated and the number of these patients was recorded. Sedated patients were closely observed with pulse oximetry and managed appropriately as necessary. An investigator blinded to group allocation evaluated all of these variables at the end of each time period.
Statistical analysis
SPSS® version 18 (SPSS Inc.; Chicago, IL, USA) was used for statistical analyses, and data were expressed as number of patients, mean [standard deviation (SD)]. Sample size was calculated based on the primary endpoint, i.e., comparison of the volume of infused IV-PCA between the groups. Based on an institutional preliminary study, the anticipated mean (SD) infused volume of IV-PCA for 48 hr was 60 (18) mL after surgery, and we considered a 30% reduction (18 mL) to be clinically significant.14 We determined that 26 patients would be required in each group to show this difference with α error of 5% and power of 90% using the independent Student’s t test. Allowing for a 10% dropout rate during the study period, 30 patients were enrolled in each group. We used the Chi square statistic or Fisher’s exact test for categorical variables and the independent Student’s t test or Mann-Whitney U test for continuous variables as appropriate. All reported P values are two sided. Values measured repeatedly were compared by repeated measures analysis of variance using the Bonferroni correction for post hoc analysis.
Results
Arthroscopic surgery was performed successfully in all patients, and none of the patients developed any complications related to perioperative anesthesia or surgery. Thus, data from all 60 patients could be collected and analyzed. The patients’ characteristics and operative data, including the type and duration of surgery, were similar between the groups (Table 1).
The mean (SD) amount of cumulative fentanyl consumption for 48 hr postoperatively was significantly less in the Pregabalin group than in the Control group [1,126.0 (283.6) μg vs 1,641.4 (320.3) μg, respectively; mean difference, 515.4 μg; 95% confidence interval [CI], 359.0 to 671.8; P = <0.001] (Table 2). The preoperative pain scores of all patients were < 3 and were similar between the groups (data not shown). Pain intensity scores expressed on the NRS at six, 24, and 48 hr after surgery were all significantly lower in the Pregabalin group than in the Control group. Also, the frequency of additional pain rescue drug (ketorolac) administered during 24-48 hr was significantly less in the Pregabalin group than in the Control group (Table 3).
The occurrence of complications related to the multimodal analgesic regimen, including sedation, headache, dizziness, and blurred vision, were similar between the groups during the study period. Also, the incidence of postoperative nausea was similar between the groups, and none of the patients experienced postoperative vomiting (Table 4).
Discussion
In this randomized controlled study, we evaluated the efficacy of administering a single preemptive dose of pregabalin 150 mg before arthroscopic shoulder surgery as an adjunct to an opioid-based IV-PCA. This resulted in a significant beneficial effect in terms of a reduction in opioid consumption, pain intensity, and requirement for pain rescue medication. In addition, these beneficial effects of pregabalin were not accompanied by any increase in side effects.
Opioid-based IV-PCA is being widely used as it is able to provide analgesia for a chosen duration of time after surgeries that accompany significant pain. Nevertheless, many studies have shown that this method is associated with several adverse effects, including sedation, respiratory depression, constipation, urinary retention, as well as nausea and vomiting. To reduce these opioid-related adverse effects, a multimodal approach to the management of acute postoperative pain has been advocated for many years.15 Accordingly, the efficacy of several drugs as adjuvants has been studied, including NSAIDs, ketamine, local anesthetics, and opioids.16-19
Recently, gabapentinoids have attracted attention in the surgical setting as an adjuvant to a multimodal postoperative pain management strategy. Gabapentinoids bind at the α2-δ subunit of presynaptic voltage-gated calcium channels and exert analgesic effects by reducing the release of several excitatory neurotransmitters such as calcitonin gene-related peptide, glutamate, noradrenaline, and substance P.20 Also, gabapentinoids administered before surgical trauma have been shown to interact with other analgesics additively or synergistically to decrease inflammatory hyperalgesia.21 These properties of gabapentinoids may be useful in decreasing opioid consumption when the agents are administered as an adjunct to a multimodal approach to postoperative pain management.22,23 Among the gabapentinoids, pregabalin shows reliable pharmacokinetic profiles across its therapeutic dose range with low intersubject variability.24 These theoretical advantages have led to clinical studies validating the analgesic efficacy of oral pregabalin for postoperative pain in various surgical settings.25,26
In the current trial, a single preoperative dose of pregabalin 150 mg was beneficial in controlling pain intensity with an opioid-sparing effect for a period of 48 hr after arthroscopic shoulder surgery. Contradictory results found in previous studies evaluating the effect of pregabalin on acute postoperative pain might be related to different doses and the type of surgery. In the case of single preoperative administration, pregabalin 150 mg was reported as being beneficial in decreasing postoperative pain and opioid consumption after laparoscopic cholecystectomy,22 while administration of pregabalin 100 mg did not result in a beneficial effect after minor gynecologic surgery.27 On the other hand, administration of pregabalin 300 mg before and after laparoscopic hysterectomy resulted in increased pregabalin-related side effects, although the agent’s analgesic efficacy was present.13 Therefore, we administered a 150 mg dose of pregabalin to patients in this study and observed significant analgesic efficacy without the cost of untoward side effects.
Most of the studies showing negative results involved minimally invasive surgery, including laparoscopic surgery, minor gynecological surgery, and surgery performed using regional anesthesia, types of procedures that are associated with relatively less postoperative pain.25-27 A recent meta-analysis recommended further studies to evaluate the analgesic effect of pregabalin in more painful surgeries, pointing to the importance of a surgery-specific analgesic regimen.28 In addition, it was suggested that pregabalin’s analgesic efficacy was evident only in patients who received general anesthesia and opioid analgesia.26 These findings are consistent with the results of the current trial, as arthroscopic shoulder surgery (Bankart or rotator cuff repair) is generally considered to be associated with severe postoperative pain.1
An additional strength of this study is our strategy to evaluate the analgesic efficacy of pregabalin for 48 hr after surgery and our finding that the drug’s beneficial influence extended beyond its elimination half-life. Many studies examining the effect of a single dose of pregabalin evaluated its analgesic effect for only 24 hr postoperatively, as it has an elimination half-life of 4.6-6.8 hr. Although acute postoperative pain is commonly recognized as nociceptive pain, surgical trauma has been established to induce hyperalgesia, which can lead to abiding postoperative pain.25 Preventive analgesia is a type of treatment that begins before surgical stimuli in order to prevent the central sensitization of the dorsal horn caused by incisional injury. Pregabalin is well known to reduce central sensitization and hyperalgesia after tissue injury by inhibiting calcium influx in voltage-gated calcium channels.29 The beneficial effect of preemptive analgesia with gabapentinoids has been reported in many other studies.30-32 In the current trial, fentanyl consumption, pain intensity, and rescue analgesic requirement during 24-48 hr postoperatively were all significantly lower in the Pregabalin group than the Control group. Thus, the extended beneficial influence of pregabalin observed in the current trial may be attributed to the abovementioned mechanism, although it is beyond the scope of this study to draw such a conclusion due to lack of mechanistic analysis and adequate statistical power for analysis of interim time points.
There are certain limitations to this study. First, caution should be exercised when generalizing the results of our study as it was carried out in a single institution in Korean patients only. Second, although our results point to clear analgesic efficacy of preemptive pregabalin administration, pain intensity scores upon PACU arrival were considerably high in both groups, requiring rescue analgesic administration in most of the patients. This observation may be attributed to the possible occurrence of acute hyperalgesia from the discontinuation of remifentanil after surgery.33 Although patients were allowed to press fentanyl bolus delivery and receive ketorolac rescue, our multimodal analgesic regimen requires further modification to improve pain control during the immediate postoperative period.
In conclusion, single administration of pregabalin 150 mg before arthroscopic shoulder surgery resulted in significant analgesic efficacy in terms of opioid-sparing effects and improved pain intensity scores without influencing side effects for 48 hr postoperatively.
References
Ilfeld BM, Morey TE, Wright TW, Chidgey LK, Enneking FK. Continuous interscalene brachial plexus block for postoperative pain control at home: a randomized, double-blinded, placebo-controlled study. Anesth Analg 2003; 96: 1089-95.
Klein SM, Nielsen KC, Martin A, et al. Interscalene brachial plexus block with continuous intraarticular infusion of ropivacaine. Anesth Analg 2001; 93: 601-5.
Ciccone WJ 2nd, Busey TD, Weinstein DM, Walden DL, Elias JJ. Assessment of pain relief provided by interscalene regional block and infusion pump after arthroscopic shoulder surgery. Arthroscopy 2008; 24: 14-9.
Price DJ. The shoulder block: a new alternative to interscalene brachial plexus blockade for the control of postoperative shoulder pain. Anaesth Intensive Care 2007; 35: 575-81.
Boezaart AP. Continuous interscalene block for ambulatory shoulder surgery. Best Pract Res Clin Anaesthesiol 2002; 16: 295-310.
Delaunay L, Souron V, Lafosse L, Marret E, Toussaint B. Analgesia after arthroscopic rotator cuff repair: subacromial versus interscalene continuous infusion of ropivacaine. Reg Anesth Pain Med 2005; 30: 117-22.
Fredrickson MJ, Krishnan S, Chen CY. Postoperative analgesia for shoulder surgery: a critical appraisal and review of current techniques. Anaesthesia 2010; 65: 608-24.
Chandrakantan A, Glass PS. Multimodal therapies for postoperative nausea and vomiting, and pain. Br J Anaesth 2011; 107(Suppl 1): i27-40.
American Society of Anesthesiologists Task Force on Acute Pain Management.. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 2012; 116: 248-73.
Stacey BR, Dworkin RH, Murphy K, Sharma U, Emir B, Griesing T. Pregabalin in the treatment of refractory neuropathic pain: results of a 15-month open-label trial. Pain Med 2008; 9: 1202-8.
Taylor CP. The biology and pharmacology of calcium channel alpha2-delta proteins Pfizer Satellite Symposium to the 2003 Society for Neuroscience Meeting. Sheraton New Orleans Hotel, New Orleans, LA November 10, 2003. CNS Drug Rev 2004; 10: 183-8.
Stahl SM. Mechanism of action of alpha2delta ligands: voltage sensitive calcium channel (VSCC) modulators. J Clin Psychiatry 2004; 65: 1033-4.
Jokela R, Ahonen J, Tallgren M, Haanpaa M, Korttila K. A randomized controlled trial of perioperative administration of pregabalin for pain after laparoscopic hysterectomy. Pain 2008; 134: 106-12.
Van Elstraete AC, Tirault M, Lebrun T, et al. The median effective dose of preemptive gabapentin on postoperative morphine consumption after posterior lumbar spinal fusion. Anesth Analg 2008; 106: 305-8.
Kehlet H, Dahl JB. The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg 1993; 77: 1048-56.
Reuben SS, Bhopatkar S, Maciolek H, Joshi W, Sklar J. The preemptive analgesic effect of rofecoxib after ambulatory arthroscopic knee surgery. Anesth Analg 2002; 94: 55-9.
Aida S, Yamakura T, Baba H, Taga K, Fukuda S, Shimoji K. Preemptive analgesia by intravenous low-dose ketamine and epidural morphine in gastrectomy: a randomized double-blind study. Anesthesiology 2000; 92: 1624-30.
Obata H, Saito S, Fujita N, Fuse Y, Ishizaki K, Goto F. Epidural block with mepivacaine before surgery reduces long-term post-thoracotomy pain. Can J Anesth 1999; 46: 1127-32.
Wilson RJ, Leith S, Jackson IJ, Hunter D. Pre-emptive analgesia from intravenous administration of opioids. No effect with alfentanil. Anaesthesia 1994; 49: 591-3.
Fink K, Dooley DJ, Meder WP, et al. Inhibition of neuronal Ca(2+) influx by gabapentin and pregabalin in the human neocortex. Neuropharmacology 2002; 42: 229-36.
Hurley RW, Chatterjea D. Rose Feng M, Taylor CP, Hammond DL. Gabapentin and pregabalin can interact synergistically with naproxen to produce antihyperalgesia. Anesthesiology 2002; 97: 1263-73.
Agarwal A, Gautam S, Gupta D, Agarwal S, Singh PK, Singh U. Evaluation of a single preoperative dose of pregabalin for attenuation of postoperative pain after laparoscopic cholecystectomy. Br J Anaesth 2008; 101: 700-4.
Frampton JE, Foster RH. Pregabalin: in the treatment of postherpetic neuralgia. Drugs 2005; 65: 111-8; discussion 119-20.
Ben-Menachem E. Pregabalin pharmacology and its relevance to clinical practice. Epilepsia 2004; 45(Suppl 6): 13-8.
Jokela R, Ahonen J, Tallgren M, Haanpaa M, Korttila K. Premedication with pregabalin 75 or 150 mg with ibuprofen to control pain after day-case gynaecological laparoscopic surgery. Br J Anaesth 2008; 100: 834-40.
Yadeau JT, Paroli L, Kahn RL, et al. Addition of pregabalin to multimodal analgesic therapy following ankle surgery: a randomized double-blind, placebo-controlled trial. Reg Anesth Pain Med 2012; 37: 302-7.
Paech MJ, Goy R, Chua S, Scott K, Christmas T, Doherty DA. A randomized, placebo-controlled trial of preoperative oral pregabalin for postoperative pain relief after minor gynecological surgery. Anesth Analg 2007; 105: 1449-53.
Zhang J, Ho KY, Wang Y. Efficacy of pregabalin in acute postoperative pain: a meta-analysis. Br J Anaesth 2011; 106: 454-62.
Shneker BF, McAuley JW. Pregabalin: a new neuromodulator with broad therapeutic indications. Ann Pharmacother 2005; 39: 2029-37.
Pande AC, Crockatt JG, Feltner DE, et al. Pregabalin in generalized anxiety disorder: a placebo-controlled trial. Am J Psychiatry 2003; 160: 533-40.
Dierking G, Duedahl TH, Rasmussen ML, et al. Effects of gabapentin on postoperative morphine consumption and pain after abdominal hysterectomy: a randomized, double-blind trial. Acta Anaesthesiol Scand 2004; 48: 322-7.
Pandey CK, Sahay S, Gupta D, et al. Preemptive gabapentin decreases postoperative pain after lumbar discoidectomy. Can J Anesth 2004; 51: 986-9.
Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth 2014; 112: 991-1004.
Acknowledgements
The authors thank Jae-Kwang Shim MD PhD (Yonsei University College of Medicine, Seoul, South Korea) for his valuable comments on the manuscript.
Funding
This study was not funded by any companies or organizations.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Sowoon Ahn and Jong Chan Kim helped design this study and analyze the data. Sowoon Ahn, Sung Hye Byun, and Jong Chan Kim helped prepare the manuscript. Sung Hye Byun, Kibum Park, Jong Lin Ha, and Byeonghun Kwon helped conduct the study. Jong Lin Ha and Byeonghun Kwon helped collect the data. All authors reviewed the manuscript.
Rights and permissions
About this article
Cite this article
Ahn, S., Byun, S.H., Park, K. et al. Analgesic efficacy of preemptive pregabalin administration in arthroscopic shoulder surgery: a randomized controlled trial. Can J Anesth/J Can Anesth 63, 283–289 (2016). https://doi.org/10.1007/s12630-015-0510-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-015-0510-0