Abstract
Purpose of Review
Enhanced recovery after surgery (ERAS) protocols have become common for patients undergoing breast reconstruction, catalyzed by the recent opioid crisis. Here, we review standard ERAS protocol structure and the supporting evidence.
Recent Findings
A perioperative multidisciplinary team and multimodal pain management appropriately are the two critical factors for ERAS success. Preoperative counseling, both antibiotic and venous thromboembolic prophylaxis, and multimodal antiemetics are crucial to optimize results. Regional nerve blocks provide an alternative to oral and intravenous opioids. Intraoperative minimization of inhaled anesthetics and complete IV analgesia is recommended along with team communication. A postoperative opioid-sparing approach with medications such as acetaminophen, NSAIDs, and gabapentin is needed along with an early diet, patient mobilization, and IV fluid and Foley catheter discontinuation.
Summary
ERAS protocols for breast reconstruction have shown a decrease in length of stay, intraoperative and postoperative narcotic use, and perioperative costs while simultaneously increasing patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past two decades, the opioid epidemic in the United States (US) has become a highly discussed topic among medical professionals, the media, and the general public. In 2018 alone, over 46,000 individuals died from opioid overdose in the US, with 32% directly linked to prescription opioids [1]. In an effort to simultaneously reduce opioid prescriptions while maximizing postoperative recovery, surgeons began developing and implementing enhanced recovery after surgery (ERAS) protocols [2].
The term “ERAS” was first introduced in the early twenty-first century [3]. Prior to 2001, several publications had used the term “fast-track” surgery that described a similar approach to current ERAS protocols [4, 5]. Both terms describe evidence-based protocols that utilize a multidisciplinary team for a multimodal pain management approach with patient engagement and ongoing protocol evaluation and evolution with the ultimate goal of optimizing quality of care [6].
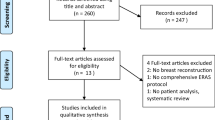
In 2011, the first ERAS protocol for breast reconstruction was published and since then, multiple series have been published and provide the evidence for current protocols (Fig. 1) [7]. With over 101,000 breast reconstruction cases in 2018, there is an exceptionally large patient population who can benefit from ERAS protocol implementation [8]. The protocols for breast reconstruction have shown a decrease in length of stay (LOS), decrease in intraoperative and postoperative narcotic use, and an overall decrease in perioperative costs, with a simultaneous increase in patient satisfaction [7, 9•, 10••]. Here we review the current evidence for perioperative ERAS protocol management for patients undergoing breast reconstruction after mastectomy.
Preoperative Protocols
Days Prior to Surgery
The preoperative phase of ERAS begins in the clinic with extensive preoperative counseling to set realistic expectations for both the perioperative and postoperative period. Preoperative education leads to earlier achievement of postoperative milestones for discharge, reduction in patient anxiety, and improvements in patient satisfaction [11•, 12]. Additionally, preoperative medical optimization such as smoking and alcohol cessation for at least 4 weeks prior to surgery, weight loss, and tight glucose control for diabetic patients can all help minimize postoperative complications [11•, 12]..
Day of Surgery
Pain Management
Opioid-sparing pain management plans are initiated preoperatively using a combination of both oral medications and regional anesthesia [11•, 13, 14•, 15••, 16•]. Oral medications include acetaminophen, gabapentin, and celecoxib [11•, 17•]. Acetaminophen is utilized in all three phases of the ERAS protocol and its use is well established across all surgical specialties as an effective drug for both pain control and reduction of opioid use in the perioperative period [11•]. Preoperative use of gabapentin has been shown to significantly decrease postoperative pain, postoperative opioid use, and postoperative nausea and vomiting (PONV) [11•, 13, 14•, 18,19,20,21,22] The available regional anesthesia techniques for breast reconstruction have all led to significant reductions in postoperative pain, opioid use, and PONV along with an associated decreased LOS [11•, 22, 23••, 24]. The reduction in PONV is likely secondary to both lower opioid and inhaled gas requirements during general anesthesia [23••, 24, 25]..
There are several regional anesthesia techniques that can be utilized based on the planned approach for breast reconstruction (Table 1). For alloplastic (implant)-based reconstruction, paravertebral (PVB), pectoral nerve (which includes PEC I and PEC II), serratus anterior plane (SAP), and erector spinae plane (ESP) blocks can be used [12, 23••, 24, 25, 26]. Additional regional anesthesia options for patients undergoing abdominal-based autologous reconstruction include blocks to the transversus abdominis plane (TAP), quadratus lumborum block (QLB), and ESP planes [27,28,29,30]. All blocks, except the PVB, are considered intrafascial plane blocks because they rely on anesthetic spread throughout their respective fascial compartment to reach the targeted nerve(s) [28,29,30]. Intrafascial plane blocks are more superficial injections with a lower risk for the serious complications that can occur with a PVB including vascular perforation, pneumothorax, and hypotension [19, 24, 25, 29]. Lastly, an injection of liposomal bupivacaine is an option for an increased duration of analgesia obtained from either a preoperative block or can be directly injected into the surgical wound intraoperatively [31].
Antiemetics
Multimodal antiemetics targeting different receptors have been shown to significantly reduce the incidence of PONV [15••, 19]. In the preoperative phase, scopolamine patches, ondansetron, and gabapentin can be utilized to minimize PONV [17, 32•].
Venous Thromboembolism
Venous thromboembolism (VTE) rates in patients undergoing breast reconstruction are double that of patients undergoing lumpectomy or mastectomy alone [15••, 33]. Preoperative mechanical prophylaxis with sequential compression devices should be used and pharmacological VTE prophylaxis should be considered for all reconstruction cases [15••].
Intraoperative Protocols
Cleaning and Antibiotic Prophylaxis
Infectious complications are known to be higher in breast reconstruction surgery when compared with other breast surgeries [15••]. Skin preparation with aqueous-based chlorhexidine gluconate (CHG) solution with a minimum of 3-min dry time is preferred [34, 35]. In line with national surgery guidelines including the Surgical Care Improvement Project (SCIP), intravenous antibiotics targeting common skin bacterial flora should be infused within 1 h of the skin incision [15••, 36]. There is currently no evidence supporting continued antibiotic use beyond 24 h after breast reconstruction surgery, regardless of surgical drain status [15••, 37].
Temperature Management
Maintaining the patient at a euthermic core temperature of 36 °C or higher has been shown to reduce a multitude of complications including infection and wound healing [38, 39]. Forced-air measures are needed for appropriate patient warming and include forced-air warming blankets, which are the most effective, along with underbody warming and circulating water garments [38, 40]. Warmed intravenous fluids and humified air should be considered by the anesthesia team, while the surgical team should consider warm fluid for surgical irrigation [41].
Intravenous Fluid Management
Aggressively maintaining euvolemia is critical to prevent adverse events. An inability to maintain euvolemia has been shown to result in increased risks for cardiopulmonary events, wound infection, and healing and has been shown to be prothrombic in tissue-based reconstruction [42, 43]. Warm fluids with balanced crystalloids should be used whenever possible to maintain appropriate electrolyte balance. The administration of vasopressor support in euvolemic patients has been shown to be safe and effective [44•]. Foley catheters should be considered for operations lasting longer than 3 h and should be removed promptly at the completion of the operation or as soon as possible prior to hospital discharge [17•].
Analgesia and Anesthetic Management
Multimodal intraoperative analgesia and anesthetic management are crucial to postoperative outcomes in ERAS patients. Communication between the surgical and anesthesia teams is imperative and reviewing analgesia management should be considered as part of the standard time-out [17•].
Nitrous oxide and inhalation agents should be avoided, and total intravenous analgesia management should be employed when possible. For sedation, a propofol infusion should be used in the absence of any contraindications. Ketamine and dexmedetomidine may also be used; however, both can cause hypotension and bradycardia [17•, 32•]. To minimize PONV, dexamethasone may be given after induction and a dose of ondansetron should be given prior the end of the case. Promethazine can also be added if needed [17•, 32•].
Multimodal pain control is achieved by using several medications. Intravenous or oral acetaminophen is given preoperatively every 6 h thereafter. Ketorolac and other NSAIDs can be used with no increase in risks for postoperative bleeding complications [45,46,47,48,49]. As-needed intravenous pushes of fentanyl and/or hydromorphone are given for breakthrough pain [17•]. At the completion of the operation, the surgically placed wound catheters for postoperative anesthetic infusion may also be considered; however, the current evidence does not strongly support their use [50, 51].
Postoperative Protocols
Pain Management
Optimal perioperative pain management requires an opioid-sparing multimodal pain protocol to reduce total opioid consumption [15••, 52•, 53•, 54•, 55]. This includes an inpatient and outpatient pain management regimen that is weaned over the course of 1–2 weeks and includes scheduled acetaminophen, NSAIDs, gabapentin, as-needed opioids, and rarely muscle relaxants [15••]. The combination of acetaminophen and NSAIDs is more effective than either alone in managing postoperative pain [56]. Intravenous acetaminophen is more costly while not necessarily more effective compared with oral administration [57].
Diet and PONV
Patients are advanced to a regular diet as soon as possible with early discontinuation of intravenous fluids to minimize the risk of complications [42, 43]. Early advancement to a regular diet and reduction in PONV all serve to improve patient satisfaction after surgery. Early refeeding within 24 h after surgery is safe and associated with improved healing, reduced infection rates, and reduced hospital LOS [58].
Mobilization and Length of Stay
Barriers to discharge for breast reconstruction are most often mobilization and pain control. Early mobilization has been shown to increase muscle strength, improve pulmonary function, and decrease venous thromboembolism [59, 60]. ERAS postoperative protocols improve early mobilization and decrease hospital LOS [61••]. Recent analyses have found a significant reduction in LOS for ERAS patients to be on average 1.0–1.35 days shorter compared with standard protocols without an increased rate of postoperative complications or hospital readmission rates [32•, 52•, 53•]..
For implant-based reconstruction, patients using an ERAS protocol are more likely to be discharged the same day (58.6%) compared with the standard (7.2%) without an increased risk of complications [62]. Patients undergoing microvascular autologous breast reconstruction in an ERAS protocol have been shown to be discharged an average of 2 days earlier compared with the standard average of 5–6 days [55].
Conclusion
ERAS protocols involve a multidisciplinary and multimodal approach to perioperative care. Key elements include preoperative counseling and education, multimodal pain management using regional blocks and opioid-sparing techniques, VTE and PONV prophylaxis, and early mobilization. Complete protocol implementation requires close collaboration between anesthesia providers, the surgical team, and patients. ERAS protocols for breast reconstruction are both safe and effective and allow for a decreased LOS, decreased narcotic usage, and an economic benefit by decreasing hospital costs. Future research should address long-term outcomes and patient-reported satisfaction using validated procedure-specific surveys. This data can be used to further expand and improve upon the current ERAS protocol recommendations to optimize patient safety, quality, and satisfaction.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
National Institute on Drug Abuse. Overdose death rates. 2020. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed 3 Apr 2020.
Etemadi K. Tackling the opioid epidemic: using the enhanced recovery after surgery principles to manage gynecological post-op pain. Harvard Public Health Rev. 2019;25. http://harvardpublichealthreview.org/surgeryrecoveryopioids/. Accessed 7 Aug 2020.
Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2004;24(3):466–77. https://doi.org/10.1016/j.clnu.2005.02.002.
Engelman RM, Rousou JA, Flack JE, Deaton DW, Humphrey CB, Ellison LH, et al. Fast-track recovery of the coronary bypass patient. Ann Thorac Surg. 1994;58(6):1742–6. https://doi.org/10.1016/0003-4975(94)91674-8.
Bardram L, Funch-Jensen P, Jensen P, Crawford ME, Kehlet H. Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet. 1995;345(8952):763–4. https://doi.org/10.1016/s0140-6736(95)90643-6.
Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017;152(3):292–8. https://doi.org/10.1001/jamasurg.2016.4952.
Arsalani-Zadeh R, ElFadl D, Yassin N, MacFie J. Evidence-based review of enhancing postoperative recovery after breast surgery. Br J Surg. 2011;98(2):181–96. https://doi.org/10.1002/bjs.7331.
The American Society of Plastic Surgeons. (2018) Plastic Surgery Statistics Report. 2019. https://www.plasticsurgery.org/documents/News/Statistics/2018/plastic-surgery-statistics-full-report-2018.pdf . Accessed 1 Apr 2020.
• Oh C, Moriarty J, Borah BJ, Mara KC, Harmsen WS, Saint-Cyr M, et al. Cost analysis of enhanced recovery after surgery in microvascular breast reconstruction. J Plast Reconstr Aesthet Surg. 2018;71(6):819–26. https://doi.org/10.1016/j.bjps.2018.02.018This analysis from the Mayo Clinic highlights the cost-benefit and improved quality with ERAS implementation.
•• Mericli AF, McHugh T, Kruse B, DeSnyder SM, Rebello E, Offodile AC. Time-driven activity-based costing to model cost utility of enhanced recovery after surgery pathways in microvascular breast reconstruction. J Am Coll Surg. 2020;S1072–7515(20):30219–2. https://doi.org/10.1016/j.jamcollsurg.2020.01.035A decision-analytic model of 5 studies found that ERAS patients had a lower cost of care with superior outcomes compared to the standard in microvascular breast reconstruction.
• Barker JC, DiBartola K, Wee C, Andonian N, Abdel-Rasoul M, Lowery D, et al. Preoperative multimodal analgesia decreases post-anesthesia care unit narcotic use and pain scores in outpatient breast surgery. Plast Reconstr Surg. 2018;142(4):443e–50e. https://doi.org/10.1097/PRS.0000000000004804Retrospective review at The Ohio State found that pre-operative oral multimodal analgesia reduced post-operative narcotic use and improved breast pain scores.
Parikh RP, Myckatyn TM. Paravertebral blocks and enhanced recovery after surgery protocols in breast reconstructive surgery: patient selection and perspectives. J Pain Res. 2018;11:1567–81. https://doi.org/10.2147/JPR.S148544.
Rai AS, Khan JS, Dhaliwal J, Busse JW, Choi S, Devereaux PJ, et al. Preoperative pregabalin or gabapentin for acute and chronic postoperative pain among patients undergoing breast cancer surgery: a systematic review and meta-analysis of randomized controlled trials. J Plast Reconstr Aesthet Surg. 2017;70(10):1317–28. https://doi.org/10.1016/j.bjps.2017.05.054.
• Fan KL, Luvisa K, Black CK, Wirth P, Nigam M, Camden R, et al. Gabapentin decreases narcotic usage: enhanced recovery after surgery pathway in free autologous breast reconstruction. Plast Reconstr Surg Glob Open. 2019;7(8):e2350. https://doi.org/10.1097/GOX.0000000000002350Prospective study from MedStar Georgetown University Hospital which found post-operative gabapentin use resulted in significant reduction in postoperative opioid use, pain, and PONV.
•• Temple-Oberle C, Shea-Budgell MA, Tan M, Semple JL, Schrag C, Barreto M, et al. Consensus review of optimal perioperative care in breast reconstruction: enhanced recovery after surgery (ERAS) society recommendations. Plast Reconstr Surg. 2017;139(5):1056e–71e. https://doi.org/10.1097/PRS.0000000000003242Consensus review of ERAS care in breast reconstruction from the ERAS Society.
• Kennedy GT, Hill CM, Huang Y, So A, Fosnot J, Wu L, et al. Enhanced recovery after surgery (ERAS) protocol reduces perioperative narcotic requirement and length of stay in patients undergoing mastectomy with implant-based reconstruction. Am J Surg. 2019;S0002–9610(19):31154–7. https://doi.org/10.1016/j.amjsurg.2019.10.007Prospective study from University of Pennsylvania found that patients receiving perioperative gabapentin, acetaminophen, and NSAIDs used significantly fewer narcotics and had a shorter LOS.
• Persing S, Manahan M, Rosson G. Enhanced recovery after surgery pathways in breast reconstruction. Clin Plast Surg. 2020;47(2):221–43. https://doi.org/10.1016/j.cps.2019.12.002A review of ERAS protocols in breast reconstruction with a comprehensive report of the protocol used at Johns Hopkins Hospital.
Batdorf NJ, Lemaine V, Lovely JK, Ballman KV, Goede WJ, Martinez-Jorge J, et al. Enhanced recovery after surgery in microvascular breast reconstruction. J Plast Reconstr Aesthet Surg. 2015;68(3):395–402. https://doi.org/10.1016/j.bjps.2014.11.014.
Chiu C, Aleshi P, Esserman LJ, Inglis-Arkell C, Yap E, Whitlock EL, et al. Improved analgesia and reduced post-operative nausea and vomiting after implementation of an enhanced recovery after surgery (ERAS) pathway for total mastectomy. BMC Anesthesiol. 2018;18(1):41. https://doi.org/10.1186/s12871-018-0505-9.
Seib RK, Paul JE. Preoperative gabapentin for postoperative analgesia: a meta-analysis. Can J Anaesth. 2006;53:461–9.
Engelman E, Cateloy F. Efficacy and safety of perioperative pregabalin for post-operative pain: a meta-analysis of randomized-controlled trials. Acta Anaesthesiol Scand. 2011;55:927–43.
Zhang J, Ho KY, Wang Y. Efficacy of pregabalin in acute postoperative pain: a meta-analysis. Br J Anaesth. 2011;106:454–62.
•• Calì Cassi L, Biffoli F, Francesconi D, Petrella G, Buonomo O. Anesthesia and analgesia in breast surgery: the benefits of peripheral nerve block. Eur Rev Med Pharmacol Sci. 2017;21(6):1341–5 Review of thoracic nerve blocks in patients undergoing breast surgery and their added benefit in better pain control, lower narcotic use, and decrease in both LOS and PONV.
Kulhari S, Bharti N, Bala I, Arora S, Singh G. Efficacy of pectoral nerve block versus thoracic paravertebral block for postoperative analgesia after radical mastectomy: a randomized controlled trial. Br J Anaesth. 2016;117(3):382–6. https://doi.org/10.1093/bja/aew223.
Jones MR, Hadley GR, Kaye AD, Lirk P, Urman RD. Paravertebral blocks for same-day breast surgery. Curr Pain Headache Rep. 2017;21(8):35. https://doi.org/10.1007/s11916-017-0637-5.
Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107–13. https://doi.org/10.1111/anae.12344.
Wheble GA, Tan EK, Turner M, Durrant CA, Heppell S. Surgeon-administered, intra-operative transversus abdominis plane block in autologous breast reconstruction: a UK hospital experience. J Plast Reconstr Aesthet Surg. 2013;66(12):1665–70. https://doi.org/10.1016/j.bjps.2013.07.017.
Akerman M, Pejčić N, Veličković I. A review of the quadratus lumborum block and ERAS. Front Med (Lausanne). 2018;5:44. https://doi.org/10.3389/fmed.2018.00044.
Altıparmak B, Korkmaz Toker M, Uysal Aİ, Turan M, Gümüş Demirbilek S. Comparison of the effects of modified pectoral nerve block and erector spinae plane block on postoperative opioid consumption and pain scores of patients after radical mastectomy surgery: a prospective, randomized, controlled trial. J Clin Anesth. 2019;54:61–5. https://doi.org/10.1016/j.jclinane.2018.10.040.
Gürkan Y, Aksu C, Kuş A, Yörükoğlu UH, Kılıç CT. Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: a randomized controlled study. J Clin Anesth. 2018;50:65–8. https://doi.org/10.1016/j.jclinane.2018.06.033.
Dasta J, Ramamoorthy S, Patou G, Sinatra R. Bupivacaine liposome injectable suspension compared with bupivacaine HCl for the reduction of opioid burden in the postsurgical setting. Curr Med Res Opin. 2012;28:1609–15.
• Sharif-Askary B, Hompe E, Broadwater G, Anolik R, Hollenbeck ST. The effect of enhanced recovery after surgery pathway implementation on abdominal-based microvascular breast reconstruction. J Surg Res. 2019;242:276–85. https://doi.org/10.1016/j.jss.2019.04.062Retrospective review of 276 patients at Duke University Hospital who underwent abdominal free-flap breast reconstruction both before and after ERAS implementation, showing the ERAS group had significantly lower postoperative opioid use.
Nwaogu I, Yan Y, Margenthaler JA, Myckatyn TM. Venous thromboembolism after breast reconstruction in patients undergoing breast surgery: an American College of Surgeons NSQIP analysis. J Am Coll Surg. 2015;220(5):886–93. https://doi.org/10.1016/j.jamcollsurg.2015.01.031.
Hemani ML, Lepor H. Skin preparation for the prevention of surgical site infection: which agent is best? Rev Urol. 2009;11(4):190–5.
Dumville JC, McFarlane E, Edwards P, Lipp A, Holmes A, Liu Z. Preoperative skin antiseptics for preventing surgical wound infections after clean surgery. Cochrane Database Syst Rev. 2015;4:CD003949. https://doi.org/10.1002/14651858.CD003949.pub4.
Prantl L, Momeni A, Brebant V, Kuehlmann B, Heine N, Biermann N, et al. Recommendations for the use of antibiotics in primary and secondary esthetic breast surgery. Plast Reconstr Surg Glob Open. 2020;8(1):e2590. https://doi.org/10.1097/GOX.0000000000002590.
Monroig K, Ghosh K, Marquez JE, Medrano C, Marmor WA, McAuliffe P, et al. Do postoperative prophylactic antibiotics reduce highly virulent infections?: an analysis of 660 tissue expander breast reconstructions. Ann Plast Surg. 2020;85:S50–3. https://doi.org/10.1097/SAP.0000000000002325.
Nieh HC, Su SF. Meta-analysis: effectiveness of forced-air warming for prevention of perioperative hypothermia in surgical patients. J Adv Nurs. 2016;72(10):2294–314. https://doi.org/10.1111/jan.13010.
Torossian A, Bräuer A, Höcker J, Bein B, Wulf H, Horn EP. Preventing inadvertent perioperative hypothermia. Dtsch Arztebl Int. 2015;112(10):166–72. https://doi.org/10.3238/arztebl.2015.0166.
Deren ME, Machan JT, DiGiovanni CW, Ehrlich MG, Gillerman RG. Prewarming operating rooms for prevention of intraoperative hypothermia during total knee and hip arthroplasties. J Arthroplast. 2011;26(8):1380–6. https://doi.org/10.1016/j.arth.2010.12.019.
Campbell G, Alderson P, Smith AF, Warttig S. Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia. Cochrane Database Syst Rev. 2015;4:CD009891. https://doi.org/10.1002/14651858.CD009891.pub2.
Booi DI. Perioperative fluid overload increases anastomosis thrombosis in the free TRAM flap used for breast reconstruction. Eur J Plast Surg. 2011;34(2):81–6. https://doi.org/10.1007/s00238-010-0466-9.
Nelson JA, Fischer JP, Grover R, Mirzabeigi MN, Nelson P, Wes AM, et al. Intraoperative perfusion management impacts postoperative outcomes: an analysis of 682 autologous breast reconstruction patients. J Plast Reconstr Aesthet Surg. 2015;68(2):175–83. https://doi.org/10.1016/j.bjps.2014.10.002.
• Anker AM, Prantl L, Strauss C, Brébant V, Heine N, Lamby P, et al. Vasopressor support vs. liberal fluid administration in deep inferior epigastric perforator (DIEP) free flap breast reconstruction - a randomized controlled trial. Clin Hemorheol Microcirc. 2018;69(1-2):37–44. https://doi.org/10.3233/CH-189129Randomized-controlled trial that did not detect any negative effect of vasopressor use on flap survival or overall patient outcome.
Rojas KE, Fortes TA, Flom P, Manasseh DM, Andaz C, Borgen P. Intraoperative ketorolac use does not increase the risk of bleeding in breast surgery. Ann Surg Oncol. 2019;26(10):3368–73. https://doi.org/10.1245/s10434-019-07557-8.
Gobble RM, Hoang HL, Kachniarz B, Orgill DP. Ketorolac does not increase perioperative bleeding: a meta-analysis of randomized controlled trials. Plast Reconstr Surg. 2014;133(3):741–55. https://doi.org/10.1097/01.prs.0000438459.60474.b5.
Hall PE, Derry S, Moore RA, McQuay HJ. Single dose oral lornoxicam for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;2009(4):CD007441. https://doi.org/10.1002/14651858.CD007441.pub2.
Gaskell H, Derry S, Wiffen PJ, Moore RA. Single dose oral ketoprofen or dexketoprofen for acute postoperative pain in adults. Cochrane Database Syst Rev. 2017;5(5):CD007355. https://doi.org/10.1002/14651858.CD007355.pub3.
Legeby M, Sandelin K, Wickman M, Olofsson C. Analgesic efficacy of diclofenac in combination with morphine and paracetamol after mastectomy and immediate breast reconstruction. Acta Anaesthesiol Scand. 2005;49(9):1360–6. https://doi.org/10.1111/j.1399-6576.2005.00811.x.
Raghavendra GK, Sreenivasa RH, Ashok K, Chitsabesan P, McLean NR, Youssef M, et al. Surgically placed wound catheters (SPWC) and local anaesthetic infusion in breast surgery: efficacy and safety analysis. Breast Dis. 2011;33(1):1–8. https://doi.org/10.3233/BD-2010-0316.
Giordano S, Veräjänkorva E, Koskivuo I, Suominen E. Effectiveness of local anaesthetic pain catheters for abdominal donor site analgesia in patients undergoing free lower abdominal flap breast reconstruction: a meta-analysis of comparative studies. J Plast Surg Hand Surg. 2013;47(6):428–33. https://doi.org/10.3109/2000656X.2013.788508.
• Offodile AC, Gu C, Boukovalas S, Coroneos CJ, Chatterjee A, Largo RD, et al. Enhanced recovery after surgery (ERAS) pathways in breast reconstruction: systematic review and meta-analysis of the literature. Breast Cancer Res Treat. 2019;173(1):65–77. https://doi.org/10.1007/s10549-018-4991-8Systematic review that included 9 studies demonstrating that ERAS protocols reduce opioid use and LOS with no increase in complication rate.
• Tan YZ, Lu X, Luo J, Huang ZD, Deng QF, Shen XF, et al. Enhanced recovery after surgery for breast reconstruction: pooled meta-analysis of 10 observational studies involving 1,838 patients. Front Oncol. 2019;9:675. https://doi.org/10.3389/fonc.2019.00675Systematic review that included 10 studies demonstrating that ERAS protocols reduce opioid use and LOS with no increase in complication rate.
• Rendon JL, Hodson T, Skoracki RJ, Humeidan M, Chao AH. Enhanced recovery after surgery protocols decrease outpatient opioid use in patients undergoing abdominally based microsurgical breast reconstruction. Plast Reconstr Surg. 2020;145(3):645–51. https://doi.org/10.1097/PRS.0000000000006546Prospective study of patients undergoing abdominal based reconstruction before and after ERAS implementation. ERAS benefits were found to extend well into the outpatient setting.
Astanehe A, Temple-Oberle C, Nielsen M, de Haas W, Lindsay R, Matthews J, et al. An enhanced recovery after surgery pathway for microvascular breast reconstruction is safe and effective. Plast Reconstr Surg Glob Open. 2018;6(1):e1634. https://doi.org/10.1097/GOX.0000000000001634.
Derry CJ, Derry S, Moore RA. Single dose oral ibuprofen plus paracetamol (acetaminophen) for acute postoperative pain. Cochrane Database Syst Rev. 2013;2013(6):CD010210. https://doi.org/10.1002/14651858.CD010210.pub2.
McNicol ED, Ferguson MC, Haroutounian S, Carr DB, Schumann R. Single dose intravenous paracetamol or intravenous propacetamol for postoperative pain. Cochrane Database Syst Rev. 2016;2016(5):CD007126. https://doi.org/10.1002/14651858.CD007126.pub3.
Lambert E, Carey S. Practice guideline recommendations on perioperative fasting: a systematic review. JPEN J Parenter Enteral Nutr. 2016;40(8):1158–65. https://doi.org/10.1177/0148607114567713.
Henriksen MG, Jensen MB, Hansen HV, Jespersen TW, Hessov I. Enforced mobilization, early oral feeding, and balanced analgesia improve convalescence after colorectal surgery. Nutrition. 2002;18(2):147–52. https://doi.org/10.1016/s0899-9007(01)00748-1.
Brower RG. Consequences of bed rest. Crit Care Med. 2009;37(10 Suppl):S422–8. https://doi.org/10.1097/CCM.0b013e3181b6e30a.
•• Soteropulos CE, Tang SYQ, Poore SO. Enhanced recovery after surgery in breast reconstruction: a systematic review. J Reconstr Microsurg. 2019;35(9):695–704. https://doi.org/10.1055/s-0039-1693699Systematic review of 11 ERAS protocols, including both autologous and alloplastic protocols, that highlights the core elements that make these protocols successful.
Jogerst K, Thomas O, Kosiorek HE, Gray R, Cronin P, Casey W, et al. Same-day discharge after mastectomy: breast cancer surgery in the era of ERAS. Ann Surg Oncol. 2020. https://doi.org/10.1245/s10434-020-08386-w.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Chandler Cortina, Caitlin Patten, Karri Adamson, and Erin Doren declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cortina, C.S., Patten, C.R., Adamson, K. et al. Enhanced Recovery After Surgery (ERAS): Protocols in Post-Mastectomy Breast Reconstruction. Curr Breast Cancer Rep 12, 398–404 (2020). https://doi.org/10.1007/s12609-020-00378-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-020-00378-9