Abstract
Purpose of Review
Panel testing is increasingly being offered to patients. Currently, women may be offered a panel of up to 80 genes. Oncologists are tasked with understanding the indications for this testing as well as the potential implications. In this review, we outline which patients should undergo genetic testing for hereditary breast cancer, when this testing should be performed, and which genes should be tested for.
Recent Findings
Our understanding of hereditary breast cancer has drastically changed with the advent of next generation sequencing (NGS), and many additional genes have been associated with increased breast cancer risk. Some have advocated for genetic testing of all women with breast cancer.
Summary
Routine genetic testing for all women with breast cancer is not warranted. Women with a phenotype associated with hereditary breast cancer, with a family history of cancer, or for whom a positive genetic test would change management should be offered genetic testing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The next generation sequencing (NGS) technology and a landmark ruling in 2013 by the Supreme Court prohibiting patents on genes [1, 2] has advanced our understanding of hereditary breast cancer (HBC) and led to the use of expanded panel testing. Genes that increase an individual’s risk for breast cancer account for an estimated 10% of all breast cancer cases [3, 4•, 5•, 6], with about 40–50% of these cases having a mutation in BRCA 1 or BRCA 2 [7, 8•, 9]. Most guidelines recommend a targeted approach when deciding which genes to test [10••, 11,12,13,14,15]; however, recent studies have identified limitations of current testing guidelines in identifying patients with a mutation and recommend testing all patients with breast cancer [5•, 16]. In addition to the uncertainty of deciding which patients to offer genetic testing, questions may also arise regarding when to order genetic testing as well as how many genes to test for. Finding a BRCA 1 or BRCA 2 mutation at the time of a breast cancer diagnosis can be critical to guiding decisions about treatment, whereas identification of other breast cancer risk genes may be less relevant to the patient’s clinical course at that time, but would affect cancer screening recommendations. Multigene panels continue to expand, and genetic testing is becoming increasingly more complex. Challenges remain in interpretation of such broad panel testing, and the significance of positive results is not always clear.
Who to Test?
Professional organizations and expert panels, including the American Society of Clinical Oncology [11], the National Comprehensive Cancer Network (NCCN) [13, 17], the National Society of Genetic Counselors [15], and the US Preventive Services Task Force [10••] have developed clinical criteria and practice guidelines to identify who to offer genetic testing and which individuals may have a BRCA1 or BRCA2 pathogenic variant. These guidelines are largely based on personal and family history of cancer [10••, 11,12,13, 17]. To address the expanding field of genetic testing, these recommendations are continually updated in response to developments in the field and help guide clinicians in using this technology effectively. Studies have found that selecting patients who meet more than one NCCN criterion, such as diagnosis of breast cancer at ≤ 45 years of age and ≥ 1 close blood relative with breast cancer at ≤ 50 years of age, has good sensitivity when predicting BRCA1 or 2 variants [18].
Other studies highlight the limitations of current testing criteria in identifying patients with a positive mutation and recommend testing all patients with breast cancer [5•, 16] or all healthy Ashkenazi Jewish women regardless of their cancer history [19]. In a prospective series of 1000 enrolled patients with breast cancer, all of whom underwent genetic testing using an 80-gene panel, there was not a statistically significant difference in pathogenic/likely pathogenic mutation rates between women who did and did not meet guidelines for genetic testing (9.39% vs 7.9% respectively) [5•]. The authors conclude that their findings support expanded panel testing in all patients with a diagnosis of breast cancer. It is important to note, however, testing in patients who did not meet guideline criteria identified many low to moderate risk variants, including mutations in MUTYH, CHEK2, and ATM. While screening guidelines do exist for ATM and CHEK2 mutation carriers [13, 17], the cancer risk associated with these genes varies and depends on family history, and data to inform the management of breast cancer risk and treatment is lacking [20,21,22,23,24,25]. For CHEK2, the breast cancer risk for the relatively frequent 1100delC mutation is better understood, but for other mutations, the data are conflicting [22, 26, 27]. The cancer risk associated with a heterozygous MUTYH mutation may be no different than risk based on family history alone [28, 29]. In line with a test all approach, the American Society of Breast Surgeons recently published a recommendation to make genetic testing for “BRCA1/BRCA2, and PALB2, with other genes as appropriate for the clinical scenario and family history” available to all breast cancer patients [30].
The unintended consequences of a test all approach must be considered. For patients with unanticipated positive genetic testing results, the exact cancer risk and most appropriate management plan may not be known and the benefits of testing will be limited. Furthermore, it is also important to think about patient-level factors and how the results of genetic testing will benefit the patient’s clinical course. For instance, if a patient is unlikely to tolerate surgeries or chemotherapy, then a positive genetic test result may cause more anxiety and cost than benefit. On the other hand, a positive test result may be important to inform the patient’s family members of a HBC diagnosis. The benefits and risks need to be weighed for each individual.
Given the risk and benefits and limitations of testing, we need to recommend a thoughtful approach in selecting patients for genetic testing. For those affected by cancer, early age at diagnosis increases the likelihood of finding a mutation [8•]. Cancer pathology is also an important characteristic when considering whether to undergo genetic testing. For example, a diagnosis of triple-negative breast cancer under 60 years of age should prompt consideration of genetic testing. Family history of other cancers, including prostate, pancreas, and ovarian, should also be considered. Likewise, a male or a patient with Ashkenazi Jewish ancestry with breast cancer should also prompt consideration of genetic testing [11, 13].
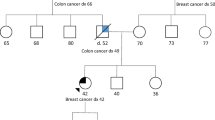
Individuals who have not been diagnosed with cancer can benefit from genetic testing as well. Identification of a pathogenic mutation associated with increased cancer risk is critical to guiding screening recommendations and primary cancer prevention. In individuals without a breast cancer history, identifying a family history with early-onset cancer or multiple primary cancers is the main factor for consideration of genetic testing [11, 13]. Testing of an affected family member is always preferred, as a negative test is considered uninformative.
As discussed, current guidelines may fall short in identifying all individuals with HBC [5•]. Despite comprehensive criteria, genetic testing is underutilized and only a small percentage of patients are referred for genetic testing based on current guidelines, suggesting the need for a new approach [4, 31,32,33,34]. As the field of genetics continues to expand, new genes associated with HBC are being identified and our understanding of the associated phenotypes and cancer risks is improving. As we gain more knowledge regarding risk profiles and management guidelines, the indications for genetic testing will likely continue to expand. Rather than rush to a “test all” approach that will lead to many uncertainties for patients and providers, efforts should instead focus on improving our understanding of HBC syndromes through family-based segregation studies and timely guideline updates.
When to Test?
The benefits of genetic testing at the time of breast cancer diagnosis include the possible identification of an inherited susceptibility gene that may influence surgical or medical treatment decisions of a patient’s breast cancer. For example, a young patient with an early-stage breast cancer may elect to undergo bilateral mastectomies rather than a lumpectomy, if found to have a pathogenic mutation in BRCA 1 or BRCA 2. Surgical risk reduction with bilateral prophylactic mastectomy offers substantial risk reduction for breast cancer and has been shown to improve breast cancer-specific mortality and overall survival benefit in BRCA mutation carriers [35,36,37]. Rates of bilateral mastectomy are higher for patients with a BRCA mutation known prior to surgery, and identification of a BRCA mutation after surgery may lead to additional breast surgeries for patients [38].
Genetic testing results may also guide chemotherapy selection, such as the use of PARP inhibitors for patients with metastatic HER2-negative breast cancer with germline BRCA1 and BRCA2 pathogenic variants [39, 40]. Also, platinum agents have been shown to be effective in treatment of breast cancer for BRCA 1 and 2 mutation carriers [41]. Identification of a TP53 mutation carrier may influence radiation treatment decisions, as these individuals have been shown to experience higher risks from radiation, including increased risk for second primary cancers in the radiation field [42, 43]. For example, a young woman with an early-stage breast cancer and family history consistent with Li-Frameni syndrome may elect to undergo mastectomy to avoid radiation if a germline TP53 mutation is identified.
Genetic testing during cancer surveillance is another option. Women with a history of breast cancer and a positive pathogenic mutation are at increased risk for additional cancers. For example, a positive CHEK2 mutation may not inform surgical or medical treatment but would impact screening recommendations. Current expert guidelines recommend that women with a pathogenic CHEK2 mutation consider breast MRI beginning at age 40 and initiate colonoscopy early [13]. Furthermore, identification of a hereditary cancer syndrome may have implications for the cancer risk of family members through the use of cascade testing.
For patients without a history of breast cancer, it is important to consider the patient’s age and family history. Genetic testing prior to cancer diagnosis should be the goal, because effective interventions can prevent cancer altogether or detect cancer earlier and improve survival. For example, adding screening MRI to annual mammogram markedly increases the likelihood of early cancer detection in high-risk individuals, including those who carry a pathogenic BRCA1 or BRCA2 mutation [37, 44,45,46]. Additionally, risk-reducing surgeries such as mastectomy and bilateral salpingo-oophorectomy have been shown to improve survival for BRCA mutation carriers [47, 48].
What Genes to Test?
Testing should always be offered in the context of genetic counseling. A tailored approach to selecting which genes to test, based on a patient’s personal cancer history and a detailed family history, remains the preferred approach. Cascade testing in families where a pathogenic mutation has been identified is critical to identify additional mutation carriers at significant risk for cancer. In these instances, testing specifically for a known gene may often be the most appropriate first step. Testing for additional genes is usually not necessary unless there is a suspicion for another hereditary cancer syndrome. For instance, if a BRCA 1 mutation is identified on the maternal side of a patient’s family, the paternal family history should still be collected and assessed for suspicion of a hereditary cancer syndrome.
At the time of a breast cancer diagnosis, we recommend starting with BRCA 1 and BRCA 2, as these are the genes with the clearest risk of a second primary breast cancer and may affect surgical decision-making. If testing is negative, providers may later assess for HBC risk with a 12-gene panel. Based on the NCCN guidelines, the most clinically relevant (highly and moderately penetrant) genes contributing to risk of breast cancer development include BRCA1, BRCA2, PTEN, TP53, ATM, CDH1, CHEK2, NBN, NF1, PALB2, and STK11 [17]. While this panel is a good starting point, a detailed family history must be collected and this information should ultimately guide the gene selection. For example, testing of Lynch syndrome genes should be included in the panel if there are several cases of early-onset colorectal and endometrial cancer.
While some studies propose expedited multigene panel testing prior to surgery [49•], it is important to remember that reflex testing to a larger panel is an option. Multigene panel testing will result in identification of more germline mutations [4•, 5•, 9], including clinically relevant genes. However, clear management recommendations or improvements in outcomes with possible interventions for these genes are often lacking or not well studied [50]. Furthermore, challenges remain in the interpretation of broad panel testing. In two studies of women who had previously tested negative for BRCA1 and BRCA2, reflex testing with a multigene panel identified pathogenic variants in additional genes among 8 to 11% of cases [51, 52•]. Additionally, Oleary and colleagues examined test results for women with breast cancer who underwent genetic testing through a single clinical laboratory and found that 13.7% of test results were unexpected findings unrelated to personal or family history [8•].
With limited information about the associated cancer risk and lack of clear guidelines conferred by many germline mutations, broad panel testing may have unanticipated consequences. Genetic testing results may impact a patient’s anxiety, quality of life, and decision-making. There is a valid concern that routine, expanded panel testing leads to increased rates of potentially unnecessary surgeries. Studies have shown rates of contralateral prophylactic mastectomy (CPM) in women who have non-BRCA mutations approaching that for BRCA mutation carriers [53], and for many of these genes, contralateral prophylactic mastectomy is not recommended [17]. High rates of CPM have also been reported among women noted to carry a variant of uncertain significance (VUS) [32], which is particularly concerning given the uncertainty of any cancer risk associated with a VUS and the high detection rate of a VUS with multigene panel testing [5•]. Given the rapid expansion of genetic testing and the shortage of counseling resources, many women are making life-altering surgical decisions without the recommendation of a genetic counselor [32]. Thus, the utility of large multigene panel testing is further limited by the lack of sufficient genetic counseling support to facilitate discussion with patients around these complex issues.
Conclusion
Panel testing for germline mutations in breast cancer patients has rapidly advanced in recent years, and many patients are being offered an increasingly larger panel of genes to test. We recommend that a rational approach should be taken in selecting which patients are most appropriate for genetic testing, and careful attention should be given by providers to obtaining a detailed family history. Given the uncertainties in cancer risk and lack of recommendations associated with many of the genes now available for testing, we conclude that routine, expanded genetic testing for all women with newly diagnosed breast cancer is not warranted. Women with a phenotype associated with HBC, with a family history of cancer, or for whom a positive genetic test would change management should be offered genetic testing.
When to offer genetic testing and which genes to test for depends on a patient’s diagnosis, family history, and readiness for genetic testing. For most women, the benefits of broad panel testing are limited. There are important implications to consider regarding the potential consequences of genetic testing, including changes in risk assessment, screening recommendations, and treatment decisions, and they should be considered prior to testing. Finally, genetic testing should always be offered in the context of genetic counseling. These resources, however, are becoming more limited as the demand for genetic testing continues to rise. Clinicians in community or more rural practices should be aware of tele-counseling services, as this may help alleviate the stress of incorporating genetic counseling into their practices and/or assist in making sure that the right referral or test is performed. Improved awareness of who to offer genetic testing as well as thoughtful panel selections will help ensure access to this valuable resource for patients who have the most potential benefit.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Metzker ML. Sequencing technologies-the next generation. Nat Rev Genet. 2010;11(1):31–46.
Supreme Court of the United States syllabus. Association for Molecular Pathology et al. v. Myriad Genetics, Inc., et al. certiorari to the United States Court of Appeals for the Federal Circuit. Rev Derecho Genoma Hum. 2013 (38):217–9.
Tung N, Lin NU, Kidd J, Allen BA, Singh N, Wenstrup RJ, et al. Garber JE Frequency of germline mutations in 25 cancer susceptibility genes in a sequential series of patients with breast cancer. J Clin Oncol. 2016;34(13):1460–8.
• Kurian AW, Ward KC, Howlader N, Deapen D, Hamilton AS, Mariotto A, et al. Genetic testing and results in a population-based cohort of breast cancer patients and ovarian cancer patients. J Clin Oncol. 2019;37(15):1305–15 An important paper which identified important gaps and disparities in testing for hereditary breast and ovarian cancer.
• Beitsch PD, Whitworth PW, Hughes K, Patel R, Rosen B, Compagnoni G, et al. Underdiagnosis of Hereditary breast cancer: are genetic testing guidelines a tool or an obstacle? J Clin Oncol. 2019;37(6):453–60 An important paper which demonstrates that guidelines do identifiy women with BRCA mutations, but expanding testing guidelines may reach more mutation carriers.
Couch FJ, Shimelis H, Hu C, Hart SN, Polley EC, Na J, et al. Associations between cancer predisposition testing panel genes and breast cancer. JAMA Oncol. 2017;3(9):1190–6.
Suszynska M, Klonowska K, Jasinska AJ, Kozlowski P. Large-scale meta-analysis of mutations identified in panels of breast/ovarian cancer-related genes-providing evidence of cancer predisposition genes. Gynecol Oncol. 2019;153(2):452–62.
• Buys SS, Sandbach JF, Gammon A, Patel G, Kidd J, Brown KL, et al. A study of over 35,000 women with breast cancer tested with a 25-gene panel of hereditary cancer genes. Cancer. 2017;123(10):1721–30 An important paper which demonstrates featues most consistent with BRCA related cancers.
O'Leary E, Iacoboni D, Holle J, Michalski ST, Esplin ED, Yang S. Ouyang K Expanded gene panel use for women with breast cancer: identification and intervention beyond breast cancer risk. Ann Surg Oncol. 2017;24(10):3060–6.
•• Force USPST, Owens DK, Davidson KW, Krist AH, Barry MJ, Cabana M, et al. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer: US Preventive Services Task Force recommendation statement. JAMA. 2019;322(7):652–65 Very important and up to date guidelines for genetic testing.
Lu KH, Wood ME, Daniels M, Burke C, Ford J, Kauff ND, et al. American Society of Clinical Oncology Expert statement: collection and use of a cancer family history for oncology providers. J Clin Oncol. 2014;32(8):833–40.
Lancaster JM, Powell CB, Chen LM, Richardson DL, Committee SGOCP. Society of Gynecologic Oncology statement on risk assessment for inherited gynecologic cancer predispositions. Gynecol Oncol. 2015;136(1):3–7.
Daly MB, Pilarski R, Berry M, Buys SS, Farmer M, Friedman S, et al. NCCN guidelines insights: genetic/familial high-risk assessment: breast and ovarian, version 2.2017. J Natl Compr Cancer Netw. 2017;15(1):9–20.
Robson ME, Bradbury AR, Arun B, Domchek SM, Ford JM, Hampel HL, et al. Lindor NM American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol. 2015;33(31):3660–7.
Hampel H, Bennett RL, Buchanan A, Pearlman R, Wiesner GL, Guideline Development Group ACoMG, et al. A practice guideline from the American College of Medical Genetics and Genomics and the National Society of Genetic Counselors: referral indications for cancer predisposition assessment. Genet Med. 2015;17(1):70–87.
Espenschied CR, LaDuca H, Li S, McFarland R, Gau CL, Hampel H. Multigene panel testing provides a new perspective on Lynch syndrome. J Clin Oncol. 2017;35(22):2568–75.
Genetic/Familial High-Risk Assessment (2019): Breast O, and Pancreatic. In: NCCN Clin, Pract. Guidel. Oncol. https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf Accessed 12.6.2019.
Cropper C, Woodson A, Arun B, Barcenas C, Litton J, Noblin S, et al. Daniels M Evaluating the NCCN clinical criteria for recommending BRCA1 and BRCA2 genetic testing in patients with breast cancer. J Natl Compr Cancer Netw. 2017;15(6):797–803.
Gabai-Kapara E, Lahad A, Kaufman B, Friedman E, Segev S, Renbaum P, et al. Levy-Lahad E Population-based screening for breast and ovarian cancer risk due to BRCA1 and BRCA2. Proc Natl Acad Sci U S A. 2014;111(39):14205–10.
Ahmed M, Rahman N. ATM and breast cancer susceptibility. Oncogene. 2006;25(43):5906–11.
Swift M, Morrell D, Massey RB, Chase CL. Incidence of cancer in 161 families affected by ataxia-telangiectasia. N Engl J Med. 1991;325(26):1831–6.
Weischer M, Bojesen SE, Ellervik C, Tybjaerg-Hansen A, Nordestgaard BG. CHEK2*1100delC genotyping for clinical assessment of breast cancer risk: meta-analyses of 26,000 patient cases and 27,000 controls. J Clin Oncol. 2008;26(4):542–8.
Consortium CBCC-C. CHEK2*1100delC and susceptibility to breast cancer: a collaborative analysis involving 10,860 breast cancer cases and 9,065 controls from 10 studies. Am J Hum Genet. 2004;74(6):1175–82.
Jerzak KJ, Mancuso T, Eisen A. Ataxia-telangiectasia gene (ATM) mutation heterozygosity in breast cancer: a narrative review. Curr Oncol. 2018;25(2):e176–e80.
Southey MC, Goldgar DE, Winqvist R, Pylkas K, Couch F, Tischkowitz M, et al. PALB2, CHEK2 and ATM rare variants and cancer risk: data from COGS. J Med Genet. 2016;53(12):800–11.
Schmidt MK, Hogervorst F, van Hien R, Cornelissen S, Broeks A, Adank MA, et al. Age- and tumor subtype-specific breast cancer risk estimates for CHEK2*1100delC carriers. J Clin Oncol. 2016;34(23):2750–60.
Schutte M, Seal S, Barfoot R, Meijers-Heijboer H, Wasielewski M, Evans DG, et al. Variants in CHEK2 other than 1100delC do not make a major contribution to breast cancer susceptibility. Am J Hum Genet. 2003;72(4):1023–8.
Win AK, Dowty JG, Cleary SP, Kim H, Buchanan DD, Young JP, et al. Risk of colorectal cancer for carriers of mutations in MUTYH, with and without a family history of cancer. Gastroenterology. 2014;146(5):1208–11 e1 5.
Jenkins MA, Croitoru ME, Monga N, Cleary SP, Cotterchio M, Hopper JL, et al. Risk of colorectal cancer in monoallelic and biallelic carriers of MYH mutations: a population-based case-family study. Cancer Epidemiol Biomark Prev. 2006;15(2):312–4.
Manahan ER, Kuerer HM, Sebastian M, Hughes KS, Boughey JC, Euhus DM, et al. Taylor WA Consensus guidelines on genetictesting for hereditary breast cancer from the American Society of Breast Surgeons. Ann Surg Oncol. 2019;26(10):3025–31.
Wood ME, Kadlubek P, Pham TH, Wollins DS, Lu KH, Weitzel JN, et al. Quality of cancer family history and referral for genetic counseling and testing among oncology practices: a pilot test of quality measures as part of the American Society of Clinical Oncology Quality Oncology Practice Initiative. J Clin Oncol. 2014;32(8):824–9.
Kurian AW, Li Y, Hamilton AS, Ward KC, Hawley ST, Morrow M, et al. Gaps in incorporating germline genetic testing into treatment decision-making for early-stage breast cancer. J Clin Oncol. 2017;35(20):2232–9.
Kurian AW, Griffith KA, Hamilton AS, Ward KC, Morrow M, Katz SJ. Jagsi R Genetic testing and counseling among patients with newly diagnosed breast cancer. JAMA. 2017;317(5):531–4.
Childers CP, Childers KK, Maggard-Gibbons M, Macinko J. National estimates of genetic testing in women with a history of breast or ovarian cancer. J Clin Oncol. 2017;35(34):3800–6.
Carbine NE, Lostumbo L, Wallace J, Ko H. Risk-reducing mastectomy for the prevention of primary breast cancer. Cochrane Database Syst Rev. 2018;4:CD002748.
Ingham SL, Sperrin M, Baildam A, Ross GL, Clayton R, Lalloo F, et al. Evans DG Risk-reducing surgery increases survival in BRCA1/2 mutation carriers unaffected at time of family referral. Breast Cancer Res Treat. 2013;142(3):611–8.
Padamsee TJ, Wills CE, Yee LD, Paskett ED. Decision making for breast cancer prevention among women at elevated risk. Breast Cancer Res. 2017;19(1):34.
Chiba A, Hoskin TL, Hallberg EJ, Cogswell JA, Heins CN, Couch FJ. Boughey JC Impact that timing of genetic mutation diagnosis has on surgical decision making and outcome for BRCA1/BRCA2 mutation carriers with breast cancer. Ann Surg Oncol. 2016;23(10):3232–8.
Litton JK, Rugo HS, Ettl J, Hurvitz SA, Goncalves A, Lee KH, et al. Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N Engl J Med. 2018;379(8):753–63.
Robson M, Im SA, Senkus E, Xu B, Domchek SM, Masuda N, et al. Conte P Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377(6):523–33.
Mylavarapu S, Das A, Roy M. Role of BRCA mutations in the modulation of response to platinum therapy. Front Oncol. 2018;8(16):16.
Heymann S, Delaloge S, Rahal A, Caron O, Frebourg T, Barreau L, et al. Radio-induced malignancies after breast cancer postoperative radiotherapy in patients with Li-Fraumeni syndrome. Radiat Oncol. 2010;5:104.
Bougeard G, Renaux-Petel M, Flaman JM, Charbonnier C, Fermey P, Belotti M, et al. Frebourg T Revisiting Li-Fraumeni syndrome from TP53 mutation carriers. J Clin Oncol. 2015;33(21):2345–52.
Kuhl C, Weigel S, Schrading S, Arand B, Bieling H, Konig R, et al. Prospective multicenter cohort study to refine management recommendations for women at elevated familial risk of breast cancer: the EVA trial. J Clin Oncol. 2010;28(9):1450–7.
Passaperuma K, Warner E, Causer PA, Hill KA, Messner S, Wong JW, et al. Narod SA Long-term results of screening with magnetic resonance imaging in women with BRCA mutations. Br J Cancer. 2012;107(1):24–30.
Warner E, Hill K, Causer P, Plewes D, Jong R, Yaffe M, et al. Prospective study of breast cancer incidence in women with a BRCA1 or BRCA2 mutation under surveillance with and without magnetic resonance imaging. J Clin Oncol. 2011;29(13):1664–9.
Domchek SM, Friebel TM, Singer CF, Evans DG, Lynch HT, Isaacs C, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304(9):967–75.
Finch AP, Lubinski J, Moller P, Singer CF, Karlan B, Senter L, et al. Impact of oophorectomy on cancer incidence and mortality in women with a BRCA1 or BRCA2 mutation. J Clin Oncol. 2014;32(15):1547–53.
• Theobald KA, Susswein LR, Marshall ML, Roberts ME, Mester JL, Speyer D, et al. Utility of expedited hereditary cancer testing in the surgical management of patients with a new breast cancer diagnosis. Ann Surg Oncol. 2018;25(12):3556–62 An important paper which demonstrates the importance of expanded panels when testing for hereditary breast cancer.
Mandelker D, Zhang L, Kemel Y, Stadler ZK, Joseph V, Zehir A, et al. Mutation detection in patients with advanced cancer by universal sequencing of cancer-related genes in tumor and normal DNA vs guideline-based germline testing. JAMA. 2017;318(9):825–35.
Yadav S, Reeves A, Campian S, Paine A, Zakalik D. Outcomes of retesting BRCA negative patients using multigene panels. Familial Cancer. 2017;16(3):319–28.
• Crawford B, Adams SB, Sittler T, van den Akker J, Chan S, Leitner O, et al. Multi-gene panel testing for hereditary cancer predisposition in unsolved high-risk breast and ovarian cancer patients. Breast Cancer Res Treat. 2017;163(2):383–90 An important study which shows the benefits of expanded testing when considering hereditary breast cancer.
Elsayegh N, Webster RD, Gutierrez Barrera AM, Lin H, Kuerer HM, Litton JK, et al. Arun BK Contralateral prophylactic mastectomy rate and predictive factors among patients with breast cancer who underwent multigene panel testing for hereditary cancer. Cancer Med. 2018;7(6):2718–26.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Breast Cancer Genetics
Rights and permissions
About this article
Cite this article
Landry, K.K., Wood, M.E. Panel Testing for Hereditary Breast Cancer: More or Less?. Curr Breast Cancer Rep 12, 45–50 (2020). https://doi.org/10.1007/s12609-020-00361-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-020-00361-4