Abstract
In this article, we will review the current recommendations for screening breast ultrasound along with its role as an adjunct to mammography and as a primary screening tool. We will discuss the most recent literature pertaining to breast ultrasound screening in high-risk, intermediate-risk, and average-risk women and compare it with other breast screening modalities including breast MRI, tomosynthesis or 3D mammography, and automated breast ultrasound. The current obstacles to screening breast ultrasound’s more widespread implementation will also be covered in our discussion. These will include ultrasound’s high false positive rate when compared to mammography, overdiagnosis, and cost-effectiveness. Our target audience encompasses breast surgeons, oncologists, and breast radiologists with an interest in screening breast ultrasound.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a leading cause of death in women in the USA [1]. Cancer will become a major cause of morbidity and mortality in the coming years for the entire world. With continuing trends, the incidence for all cancer cases will increase to 22.2 million by the year 2030. Breast and cervical cancers are the most common malignancies in women, with breast cancer being the most common in most countries [2]. It is therefore relevant to develop prevention strategies for population screening and early intervention. While there are new and improved treatment options available, it is the tumor stage and nodal status at diagnosis, which in the long run significantly impacts overall survival [3, 4].
Therefore, diagnosis of breast cancer at an early stage is essential, and a screening program that provides early detection of breast cancer improves breast cancer outcomes. There are multiple studies with data supporting that screening mammography in women ages 40 thru 69 years old is associated with a reduction in mortality. Current guidelines for breast cancer screening from the American Cancer Society (ACS), the United States Preventive Services Task Force (USPSTF), the American College of Radiology (ACR), and the Society of Breast Imaging (SBI) are reviewed here (Table 1)[1, 5–8].
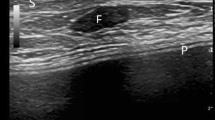
Screening Ultrasound and Mammography
Screening mammography is the only modality proven to reduce mortality from breast cancer. Nonetheless, it has limitations. Its sensitivity has been reported to vary between 85 % and as low as 48 %, depending on breast density [9, 10]. Adjunct screening modalities are being explored for women with a high risk of developing breast cancer and for women with intermediate risk for breast cancer and dense breasts.
Density in the breasts is currently subjectively identified on mammography based on an estimation of the amount of radio-opaque tissue and radiolucent fatty tissue. Dense breasts are defined by most researchers, using the Breast Imaging Reporting and Data System (BI-RADS classification [11]), as heterogeneously dense (category C) and extremely dense (category D) of the four density categories [11]. Women with mammograms showing dense breasts (categories C and D) are associated with a marked increased risk and with a modest individual risk for invasive breast cancer. The association between mammographic density and an increased risk of breast cancer is due not only to a masking effect, but as an independent risk factor itself, due to a biologic connection between breast density and breast cancer [12–14]. Approximately 27 US states have legislation with regards to patient notification about their breast density after screening mammography has been completed and interpreted [15]. Increased breast density is not associated with reduced survival among women diagnosed with breast cancer, after adjusting for stage at diagnosis and mode of detection [16].
With the coming of digital mammography, the sensitivity of mammography improved, but the overall sensitivity remained at only 55 % [17]. The majority of breast cancers detected with screening ultrasound remained occult on mammography as noted in a retrospective review from Bae et al. where the causes for non-detection were discussed [18]. Bae et al. stated that of 106,856 women who had screening ultrasounds in addition to mammograms, 356 cancers were detected only by ultrasound. Eighty-one percent of these cancers were still occult on mammography even in retrospect. These cancers were apparent on ultrasound and not on mammography because 258 were obscured by overlapping dense breast tissue on mammography, 62 were interpretive errors, and the lesions were not included on mammography in 9 [18].
Currently available modalities used for supplemental screening include handheld ultrasound (HHUS) and automated breast ultrasound (ABUS), digital breast tomosynthesis (DBT), and magnetic resonance imaging (MRI). Table 2 shows a comparative review on some recently published studies performed to date.
Mammography with adjunct screening MRI or whole breast ultrasound increases the rate of detection of early-stage breast cancer in women with dense breasts [19]. The addition of ultrasound to screening mammography has been shown to increase the screening detection rate from 0.3 to 7.7 additional breast cancers per 1000 women screened [20]. A recent retrospective study from Connecticut was demonstrated detecting an additional 2.3 cancers per 1000 women screened with adjunct ultrasound for dense breast tissue [21]. Similar studies have shown that the use of screening ultrasound detects breast cancer at early stages [20, 22, 23], and demonstrated low interval cancer rates (ICR of 1.07 per 1000 negative screens) as well [22–24]. Screening ultrasound is associated with increased false positive findings [20, 25] when compared to mammography alone. Because ultrasound and MRI are not limited by breast density like mammography is [26], they can detect breast cancer at an early stage and can improve sensitivity even in dense breast parenchyma, as is seen in most premenopausal women [27].
Automated Breast Ultrasound
ABUS has been studied for the potential to be implemented as an adjunct screening tool in breast imaging with a standardized acquisition of images using an automated transducer. A recent study showed that the mean interpretation time for a normal bilateral ABUS was 9 min [28]. In comparison, HHUS averages less than 0.5-min mean interpretation time for a normal bilateral breast ultrasound study [29]. Another study of 173 women, who had 206 suspicious lesions and scheduled for US-guided or stereotactic guided biopsy, compared the performance of HHUS to that of ABUS [30]. ABUS detected 83.0 % of the lesions biopsied while HHUS detected 94.2 % of the total lesions biopsied. ABUS detected less lesions, but did not miss any malignant lesions; only smaller size and benign lesions were not detected with ABUS [30]. The recall rate has been shown to decrease with experience and training from 25 to 13 % in 3 months [31].
The SomoInsight study [32•] was an observational, prospective multicenter trial to determine if the cancer detection rate increased when ABUS was added to mammographic screening in women with dense breast tissue (BI-RADS density C or D). A wide footprint transducer was used. A total of 15,318 women were studied. Results showed that an additional 1.9 cancers were detected per 1000 women screened with the added use of ABUS. A total of 112 cancers were detected, of which 30 were detected with ultrasound alone. Of the 30 cancers detected on ultrasound alone, most of the cancers were invasive carcinoma (28, 93.3 %). Cancer staging at the time of detection was low (stages 1A and 1B) in 67 % of the ultrasound-only detected malignancies. There was an increase in the recall rate of 13 % and an increase in the biopsy rate of 37 % when compared with mammography. Mortality was not assessed in this study, and there was no control group.
USPSTF
In February 2016, USPSTF published reviewed research on supplemental screening of women with dense breasts [8]. The task force looked at 24 studies that met their criteria, and evaluated reproducibility of BI-RADS breast density classification, test performance, and outcomes of supplemental breast screening tools in women with dense breasts. Only six of these studies were considered of good quality. The studies reviewed included the use of HHUS, ABUS, MRI, and DBT as a supplemental screening tool.
The results of the review showed that HHUS and MRI found additional breast cancers (most of them invasive), but with an increase in the false positive rates. ABUS studies were of fair quality, and only one study was shown to have similar performance characteristics to HHUS studies [33]. DBT was the only modality that did not increase the recall rates and the number of additional biopsies, and may actually reduce recall rates; however, only a few studies were available to conclusively conclude such. None of the studies took into consideration the effect of supplemental screening, while randomizing women with and without this supplemental screening, on breast cancer morbidity or mortality. The need for assessment on whether the diagnosis of additional breast cancers will lead to improved clinical outcomes, and what proportion of the additional cancers detected represents overdiagnosis was commented on. To address these issues, the task force recommended well-designed, long-term, prospective, and comparative studies.
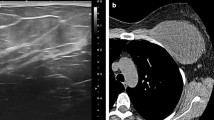
Screening Ultrasound and Digital Breast Tomosynthesis
DBT acquires multiple images of the breast at different angles creating a three-dimensional (3D) image of the breast. At present, DBT promises improved screening sensitivity in dense breasts. It remains unclear if the improved sensitivity would eliminate the requirement of additional adjunct screening ultrasound, or if the combination of DBT and screening ultrasound would provide the best screening regimen.
The STORM trial [34], a prospective comparative trial, showed that integrated two-dimensional (2D) and 3D mammographic screening significantly improved detection of breast cancer and reduced false positive recalls when compared to standard 2D mammography alone. The supplemental cancer detection rate was 2.7 cancers per 1000 screens. In this study, 3D mammograms were not interpreted independently of the 2D mammograms; therefore, 3D mammography only (without the 2D images) might not provide the same results.
The Oslo trial [35] was a prospective trial that screened women with both 2D and 3D mammography. The Oslo trial randomized reading strategies (with vs without 3D mammograms) and adjusted for the different screen readers using a Wald test in the context of a log-linear binary regression model. Analysis showed a 27 % increase in the cancer detection rate: 8 cancers per 1000 exams for combined 2D and 3D imaging compared to 6.1 cancers per 1000 for 2D. Both studies (STORM and Oslo) showed that 3D mammography reduced false positive recalls when used in addition to standard (2D) mammography [34, 35]. Screening ultrasound was not assessed in either study.
The recently published multicenter adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense trial (ASTOUND) compared DBT to US for adjunct screening in the same women with a negative screening mammogram and dense breasts [36••]. Interim results of the trial showed 3231 women with negative mammograms and dense breasts had additional 24 breast cancer detected: 1 with tomosynthesis only, 11 with ultrasound only, and 12 with both modalities. Of the 24 cancers detected, 23 were invasive carcinoma. These results show an increase in the cancer detection rate (CDR) of 7.4 cancers per 1000 screens for both modalities. The risk profile for these women was not quantified; therefore, the CDR may be higher because of higher risk patients were inadvertently included in the study. The ultrasound CDR was higher at 7.1 cancers per 1000 screens when compared to the DBT CDR, which was 4 cancers per 1000 screens. Out of 3231 women, 131 were recalled. The false positive recall rate was similar for both modalities (US, 2.0 % and DBT, 1.7 %) as was the biopsy recall rate of 0.7 % for both modalities. These findings may be due to the experience and the expertise of the interpreting radiologists and that the ultrasound screening included both prevalent and incident screens [37].
Most Recent Study
The Japan strategic anti-cancer randomized trial or J-Start [38•] is a randomized controlled multicenter study comparing the use of mammography, clinical breast exam, and ultrasound versus mammography and clinical breast exam in 72,998 women ages 40–49 years with dense breasts in Japan. It is the first large randomized trial to address the quality and effectiveness of US as a screening tool. The results showed increased sensitivity in the intervention group (mammography (MG) + clinical breast exam (CBE) + US) of 91 % when compared to the control group (MG + CBE) of 77 %. The number of interval cancers identified was lower in the intervention group (18 vs 35) than that in the control group. The screening detection rate increased by 0.17 % with the addition of ultrasound, and 67 additional breast cancers were detected by sonography alone. Of the cancers detected by sonography, 78 % were early stage (0–1), and most were invasive. Specificity was lower in the intervention group due to an increased recall rate (12.6 % in the intervention group vs 8.8 % in the control group) with a combined (both intervention and control group) recall rate of 10.7 %. The biopsy rate was 4.5 % in the intervention group compared to 1.8 % in the control group. Continued screening may decrease the recall rate and the biopsy rate, therefore increasing specificity [26]. The study allowed a comparison of the interval cancer rate between the intervention and the control groups, and the intervention group was lower. These findings are consistent with other studies, which showed that the incidence rate of interval cancers was lower when ultrasound was used as a supplemental screening tool [23, 24]. Of the women in the study, 57.7 % had BI-RADS breast density C or D, comparable to Western women in their 40s whose breast density is also BI-RADS C or D in more than 50 % [25].
Screening Ultrasound in Selective Population
High-Risk Population
Women who are at high risk for developing breast cancer have a higher prevalence of disease, and therefore, additional screening should result in a higher yield. Because they have a higher prevalence, they should be screened at an earlier age. Screening mammograms of younger women usually demonstrate dense breast tissue, decreasing the sensitivity of mammography even further. Therefore, additional screening modalities for high-risk patients are needed.
At present, contrast-enhanced breast MRI is recommended as adjunct screening to mammography for women at high risk (20 % or greater lifetime risk of breast cancer) including a family history of breast or ovarian cancer and mantle radiation to the chest [5]. The supplemental yield of mammography plus breast MRI ranges from 11 to 18.15 cancers per 1000 [39, 40]. Ultrasound is mostly used as a screening test in women who are at high risk for developing breast cancer when they cannot tolerate MRI or when MRI is contraindicated.
The American College of Radiology Imaging Network (ACRIN) 6666 trial [24] was a multicenter study to assess the use of screening ultrasound in patients with dense breasts and intermediate to high risk for developing breast cancer. The ACRIN 6666 trial demonstrated that by adding a single screening ultrasound to the screening mammogram, there was an increase in the cancer detection rate of small cancers and node-negative cancers. The study included women with additional risk factors such as a personal history of breast cancer and a family history of breast cancer, in addition to dense breasts. The targeted population has been shown to have a higher interval cancer rate than the average-risk population, and mammographic sensitivity was lower than in the average-risk population [41]. The ACRIN 6666 trial also included a mix of film screen and digital mammography, resulting in lower mammographic sensitivity in women with dense breasts. Results also showed an increase in the false positive rate with false positive rates for mammography at 4.4 % and for ultrasound at 8.1 %. The combined (mammography and ultrasound) false positive rate was 10.4 % [24]. The number of false positives should be minimized since false positives add to the overall costs of a screening program, and false positive assessments may cause unnecessary anxiety.
A recent multicenter randomized controlled trial in high-risk Chinese women ages 30–65 (mean age 46) years, compared ultrasound to mammography for breast cancer screenings [57]. The study included 12,519 women in the first year and 8692 in the second year. The patients were randomized for screening with mammography, ultrasound, or both. Their results showed that mammography detected 5 cancers (CDR 0.072/1000), ultrasound detected 11 cancers (CDR 1.51/1000), and the combined group (mammography and ultrasound) detected 14 cancers (CDR 2.02/1000) for a total of 30 cancers, of which 82 % were stages 0 and 1. In the combined group, ultrasound detected all cancers (100 % sensitivity) vs 8 detected by mammography (57.1 % sensitivity) (P = 0.04). The specificity and positive predictive value (PPV) between mammography and ultrasound was the similar at 100 vs 99.9 %, (P = 0.51) and 72.7 vs 70 %, (P = 0.87). Interestingly, the cost to detect one cancer per modality used was $7876 for ultrasound alone, $45,253 for mammography alone, and $21,599 for the combined approach. Even though the peak age for breast cancer in Asian women (40–55 years old) is different than that in Western women (60–70 years old) [42–44], we can see how for increased breast density and premenopausal women, ultrasound evaluation can be more sensitive than mammography.
Average-Risk Population
Gartlehner and colleagues [45] did a meta-analysis and systematic review of studies evaluating mammography with ultrasound vs mammography alone for breast cancer screening in average-risk women. They found no methodologically sound evidence to justify the routine addition of ultrasound to mammography in average-risk women. Results of a recent study in average-risk women indicated that MRI has a higher cancer detection rate than US or tomosynthesis [46]. In a more recent study, an abbreviated MRI protocol could provide for a screening tool without compromising sensitivity or specificity. The reduced acquisition and interpretation time may render the study more accessible and less costly [40]. The use of intravenous contrast in breast MRI remains a risk.
Ultrasound as Primary Screening for Breast Cancer
Ultrasound’s lack of radiation exposure, relatively low cost of implementation, and portability make it an attractive screening tool for breast cancer. Based on the ACRIN 6666 study, the cancer detection rate for ultrasound is similar to mammography, but a higher percentage of the cancers detected by sonography were invasive (91 %) and more likely to be node negative as well [24, 26]. The false positive rate on ultrasound was higher than that for mammography, though it was reduced with incidence screening. With adequate technologist and sonographer training, ultrasound may be a screening tool that can be used in countries where mammography is not widely available. However, appropriate validation is needed. [47]
Harms from Screening Breast Ultrasound
Potential harms noticed from supplemental screening breast ultrasound false positive results should be equivalent to the ones seen from mammography screening with the exception of the radiation exposure [48]. Possible harms include recommendations for biopsy, anxiety and distress, pain during the procedures, and overdiagnosis [26, 49]. Most of these are short-term and have shown no lasting effects [50]. Overdiagnosis means that women will have their cancer treated by surgery, radiation therapy, and possibly chemotherapy, but it is unknown if the cancer would have become apparent without screening and lead to death, or if it would have remained undetected. According to some estimates, overdiagnosis can range from 10 to 54 %, depending on whether lead time bias was compensated for or not and how it was compensated for [51–54]. It was noted that you would need at least 30 years of follow-up to compensate for the effects of lead time. Another controversy with overdiagnosis is the use of ductal carcinoma in situ (DCIS) cases and whether they have been included in the data used for estimations, as not all DCIS will represent overdiagnosis. Whether DCIS will progress to invasive cancer and cause symptoms in the patient’s lifetime is a question that has yet to be answered [52]. We do know that ultrasound screening has consistently shown that the majority of cancers detected are invasive [55••]. Overdiagnosis experts agree that some malignancies detected will likely not result in mortality, and therefore, women will be undergoing unnecessary treatment regimens. Ultrasound has shown to increase the recall rate and biopsy rates as well. However, the risk of false positives decreases with annual screening as was seen with both mammography and MRI [26].
Sprague et al. [25] used microsimulation models to determine the cost-effectiveness ratio of supplemental screening breast ultrasound per quality-adjusted life-years (QALY) gained in women with dense breasts. The analysis showed that the supplemental use of screening sonography for women ages 50–74 with dense breasts (BI-RADS C and D) would decrease cancer deaths by 0.36 per 1000 women screened. It would also cost more than $100,000 per QALY, increasing costs while producing relatively small benefits in prevented breast cancer deaths. Sprague et al. agreed that additional studies are needed to justify the use of supplemental screening breast ultrasound in dense breasts [25].
Conclusions
Mammography continues to be the gold standard as a screening tool for breast cancer detection. Due to limitations related to this imaging modality, additional screening modalities have been investigated, and some have shown improved cancer detection rates and other benefits as discussed. For example, in the high-risk population, the CDR of adjunct MRI is significantly higher that mammography or ultrasound, making it the tool of choice for screening. Supplemental ultrasound can be offered if MRI is not tolerated. For intermediate risk and/or dense breasts, adjunct ultrasound has a higher CDR than mammography alone. Recent studies have concluded that DBT in addition to 2D mammography reduces the recall rate in most instances. However, ultrasound has a better CDR than DBT in dense breasts. Breast ultrasound is also widely available, has no ionizing radiation and no adverse side effects, and is better tolerated by the patients than mammography or MRI. Ultrasound does have a higher false positive rate than mammography with a positive predictive value of approximately 11 % [56]. There is no proof that screening ultrasound can reduce the mortality rate from breast cancer, even though most of the cancers detected by ultrasound are invasive, small, and node-negative [24].
Ultrasound exam is operator-dependent. Therefore, one obvious limitation is the difficulty to maintain standardization of scanning techniques and training among technologists and sonographers in different centers and countries. In addition, this exam can be time-consuming. By adding ultrasound to mammography screening, the cost of screening would increase. Finding a balance between screening benefits and the costs of the additional adjunct exams to screening mammography requires additional studies and long-term follow-up.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Oeffinger KC, Fontham ET, Etzioni R, Herzig A, Michaelson JS, Shih Y-CT, et al. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–614.
Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008–2030): a population-based study. The Lancet Oncology. 2012;13(8):790–801. doi:10.1016/S1470-2045(12)70211-5.
Saadatmand S, Bretveld R, Siesling S, Tilanus-Linthorst MMA. Influence of tumour stage at breast cancer detection on survival in modern times: population based study in 173 797 patients. BMJ. 2015;351. doi:10.1136/bmj.h4901.
Tabár L, Vitak B, Chen HH, Duffy SW, Yen MF, Chiang CF, et al. The Swedish two-county trial twenty years later: updated mortality results and new insights from long-term follow-up. Radiol Clin N Am. 2000;38(4):625–51.
Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89. doi:10.3322/canjclin.57.2.75.
Siu AL. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016;164(4):279–96. doi:10.7326/M15-2886.
Lee CH, Dershaw DD, Kopans D, Evans P, Monsees B, Monticciolo D, et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol. 2010;7(1):18–27. doi:10.1016/j.jacr.2009.09.022.
Melnikow J, Fenton JJ, Whitlock EP, Miglioretti DL, Weyrich MS, Thompson JH, et al. Supplemental screening for breast cancer in women with dense breasts: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164(4):268–78. doi:10.7326/M15-1789.
Rosenberg RD, Hunt WC, Williamson MR, Gilliland FD, Wiest PW, Kelsey CA, et al. Effects of age, breast density, ethnicity, and estrogen replacement therapy on screening mammographic sensitivity and cancer stage at diagnosis: review of 183,134 screening mammograms in Albuquerque, New Mexico. Radiology. 1998;209(2):511–8.
Kolb TM, Lichy J, Newhouse JH. Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: an analysis of 27,825 patient evaluations. Radiology. 2002;225(1):165–75.
Radiology ACo, Committee B-R. ACR BI-RADS breast imaging and reporting data system: breast imaging atlas. American College of Radiology. 2013.
Boyd NF. Mammographic density and risk of breast cancer. American Society of Clinical Oncology educational book / ASCO American Society of Clinical Oncology Meeting. 2013. doi:10.1200/EdBook_AM.2013.33.e57.
Kerlikowske K. The mammogram that cried Wolfe. N Engl J Med. 2007;356(3):297–300. doi:10.1056/NEJMe068244.
Freer PE. Mammographic breast density: impact on breast cancer risk and implications for screening. Radiographics. 2015;35(2):302–15.
DenseBreast-info: legislation and regulations—what is required? http://densebreast-info.org/legislation.aspx.
Gierach GL, Ichikawa L, Kerlikowske K, Brinton LA, Farhat GN, Vacek PM, et al. Relationship between mammographic density and breast cancer death in the breast cancer surveillance consortium. J Natl Cancer Inst. 2012;104(16):1218–27. doi:10.1093/jnci/djs327.
Pisano ED, Hendrick RE, Yaffe MJ, Baum JK. Diagnostic accuracy of digital versus film mammography: exploratory analysis of selected population subgroups in DMIST 1. Radiology. 2008. doi:10.1148/radiol.2461070200.
Bae MS, Moon WK, Chang JM, Koo HR, Kim WH, Cho N, et al. Breast cancer detected with screening US: reasons for nondetection at mammography. Radiology. 2014;270(2):369–77. doi:10.1148/radiol.13130724.
Parris T, Wakefield D, Frimmer H. Real world performance of screening breast ultrasound following enactment of Connecticut Bill 458. Breast J. 2012;19:1. doi:10.1111/tbj.12053.
Scheel JR et al. Screening ultrasound as an adjunct to mammography in women with mammographically dense breasts. Am J Obstet Gynecol. 2015;212(1):9–17.
Weigert J, Steenbergen S. The Connecticut experiments second year: ultrasound in the screening of women with dense breasts. Breast J. 2015;21(2):175–80. doi:10.1111/tbj.12386.
Corsetti V, Houssami N, Ferrari A, Ghirardi M, Bellarosa S, Angelini O, et al. Breast screening with ultrasound in women with mammography-negative dense breasts: evidence on incremental cancer detection and false positives, and associated cost. Eur J Cancer. 2008;44(4):539–44.
Corsetti V, Houssami N, Ghirardi M, Ferrari A, Speziani M, Bellarosa S, et al. Evidence of the effect of adjunct ultrasound screening in women with mammography-negative dense breasts: Interval breast cancers at 1 year follow-up. Eur J Cancer. 2011;47(7):1021–6.
Berg WA, Blume JD, Cormack JB, Mendelson EB, Lehrer D, Böhm-Vélez M, et al. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA - Journal of the American Medical Association. 2008;299(18):2151–63. doi:10.1001/jama.299.18.2151.
Sprague BL, Stout NK, Schechter C, van Ravesteyn NT, Cevik M, Alagoz O, et al. Benefits, harms, and cost-effectiveness of supplemental ultrasonography screening for women with dense breasts supplemental ultrasonography screening for women with dense breasts. Ann Intern Med. 2015;162(3):157–66. doi:10.7326/M14-0692.
Berg WA, Zhang Z, Lehrer D, Jong RA, Pisano ED, Barr RG, et al. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012;307(13):1394–404. doi:10.1001/jama.2012.388.
Suzuki A, Ishida T, Ohuchi N. Controversies in breast cancer screening for women aged 40–49 years. Jpn J Clin Oncol. 2014;44(7):613–8. doi:10.1093/jjco/hyu054.
Skaane P, Gullien R, Eben EB, Sandhaug M, Schulz-Wendtland R, Stoeblen F. Interpretation of automated breast ultrasound (ABUS) with and without knowledge of mammography: a reader performance study. Acta Radiologica (Stockholm, Sweden : 1987). 2015;56(4):404–12. doi:10.1177/0284185114528835.
Berg WA, Mendelson EB. Technologist-performed handheld screening breast US imaging: how is it performed and what are the outcomes to date? Radiology. 2014;272(1):12–27.
Jeh SK, Kim SH, Choi JJ, Jung SS, Choe BJ, Park S, et al. Comparison of automated breast ultrasonography to handheld ultrasonography in detecting and diagnosing breast lesions. Acta Radiologica (Stockholm, Sweden : 1987). 2016;57(2):162–9. doi:10.1177/0284185115574872.
Arleo EK, Saleh M, Ionescu D, Drotman M, Min RJ, Hentel K. Recall rate of screening ultrasound with automated breast volumetric scanning (ABVS) in women with dense breasts: a first quarter experience. Clin Imaging. 2014;38(4):439–44. doi:10.1016/j.clinimag.2014.03.012.
Brem RF, Tabár L, Duffy SW, Inciardi MF, Guingrich JA, Hashimoto BE, et al. Assessing improvement in detection of breast cancer with three-dimensional automated breast US in women with dense breast tissue: the SomoInsight Study. Radiology. 2015;274(3):663–73. doi:10.1148/radiol.14132832. Multicenter prospective trial to determine changes in the cancer detection rate when automated breast ultrasound (ABUS) is added to mammographic screening in women with dense breast tissue.
Kelly KM, Dean J, Comulada WS, Lee S-JJ. Breast cancer detection using automated whole breast ultrasound and mammography in radiographically dense breasts. Eur Radiol. 2010;20(3):734–42. doi:10.1007/s00330-009-1588-y.
Ciatto S, Houssami N, Bernardi D, Caumo F, Pellegrini M, Brunelli S, et al. Integration of 3D digital mammography with tomosynthesis for population breast-cancer screening (STORM): a prospective comparison study. The Lancet Oncology. 2013;14(7):583–9. doi:10.1016/S1470-2045(13)70134-7.
Skaane P, Bandos AI, Gullien R, Eben EB, Ekseth U, Haakenaasen U, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013;267(1):47–56. doi:10.1148/radiol.12121373.
Tagliafico AS, Calabrese M, Mariscotti G, Durando M, Tosto S, Monetti F, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial. J Clin Oncol. 2016. doi:10.1200/JCO.2015.63.4147. Prospective multicenter trial comparing DBT to US as adjunct screening in the same women with a negative screening mammogram and dense breasts.
Berg WA. Current status of supplemental screening in sense breasts. J Clin Oncol. 2016. doi:10.1200/jco.2015.65.8674.
Ohuchi N, Suzuki A, Sobue T, Kawai M, Yamamoto S, Zheng Y-F, et al. Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for breast cancer in the Japan Strategic Anti-cancer Randomized Trial (J-START): a randomised controlled trial. Lancet. 2016;387(10016):10016. doi:10.1016/S0140-6736(15)00774-6. Randomised controlled trial evaluating screening breast ultrasound in dense breasts.
Berg WA. Tailored supplemental screening for breast cancer: what now and what next? Am J Roentgenol. 2009;192(2):390–9.
Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers R-D, Bieling HB. Abbreviated breast magnetic resonance imaging: first postcontrast subtracted images and maximum-intensity projection—a novel approach to breast cancer screening with mri. J Clin Oncol. 2014;32(22):2304–10.
Houssami N, Abraham LA, Miglioretti DL, Sickles EA, Kerlikowske K, Buist DS, et al. Accuracy and outcomes of screening mammography in women with a personal history of early-stage breast cancer. JAMA. 2011;305(8):790–9. doi:10.1001/jama.2011.188.
Leong SP, Shen Z-Z, Liu T-J, Agarwal G, Tajima T, Paik N-S, et al. Is breast cancer the same disease in Asian and Western countries? World J Surg. 2010;34(10):2308–24.
DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64(1):52–62.
Fan L et al. Breast cancer in China. The Lancet Oncology. 2014;15(7):e279–89.
Gartlehner G, Thaler K, Chapman A, Kaminski-Hartenthaler A, Berzaczy D, Van Noord MG, et al. Mammography in combination with breast ultrasonography versus mammography for breast cancer screening in women at average risk. Cochrane Database Syst Rev. 2013;4:CD009632.
Schrading S, Strobel K, Kuhl C. Abstract S1-09: MRI screening of women at average risk of breast cancer. Cancer Res. 2013;73(24 Supplement):S1–09-S1-.
Berg WA, Bandos AI, Mendelson EB, Lehrer D, Jong RA, Pisano ED. Ultrasound as the primary screening test for breast cancer: analysis from ACRIN 6666. J Natl Cancer Inst. 2016;108:4. doi:10.1093/jnci/djv367.
Nelson HD, Cantor A, Humphrey L, Fu R, Pappas M, Daeges M, et al. Screening for breast cancer: a systematic review to update the 2009 U.S. Preventive Services Task Force Recommendation. Agency for Healthcare Research and Quality (US). 2016.
Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L, et al. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151(10):727. doi:10.7326/0003-4819-151-10-200911170-00009.
Tosteson AA, Fryback DG, Hammond CS, et al. Consequences of false-positive screening mammograms. JAMA Intern Med. 2014;174(6):954–61. doi:10.1001/jamainternmed.2014.981.
Jørgensen K, Gøtzsche PC. Overdiagnosis in publicly organised mammography screening programmes: systematic review of incidence trends. BMJ. 2009;339:b2587. doi:10.1136/bmj.b2587.
Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. The Lancet. 2012;380(9855):1778–86.
Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367(21):1998–2005. doi:10.1056/NEJMoa1206809.
Puliti D, Duffy SW, Miccinesi G, De Koning H, Lynge E, Zappa M, et al. Overdiagnosis in mammographic screening for breast cancer in Europe: a literature review. J Med Screen. 2012;19 suppl 1:42–56.
Molleran VM. Will supplemental screening ultrasound increase breast cancer overdiagnosis? Acad Radiol. 2015;22(8):967–72. doi:10.1016/j.acra.2014.10.012. Review article describing the advantages and disadvantages of screening breast ultrasound and overdiagnosis.
Chae EY, Kim HH, Cha JH, Shin HJ, Kim H. Evaluation of screening whole-breast sonography as a supplemental tool in conjunction with mammography in women with dense breasts. J Ultrasound Med. 2013;32(9):1573–8.
Shen S, Zhou Y, Xu Y, Zhang B, Duan X, Huang R, et al. A multi-centre randomised trial comparing ultrasound vs mammography for screening breast cancer in high-risk Chinese women. Br J Cancer. 2015;112(6):998–1004. doi:10.1038/bjc.2015.33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Elsa M. Arribas, Gary J. Whitman, and Nanette De Bruhl declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Screening and Imaging
Rights and permissions
About this article
Cite this article
Arribas, E.M., Whitman, G.J. & De Bruhl, N. Screening Breast Ultrasound: Where Are We Today?. Curr Breast Cancer Rep 8, 221–229 (2016). https://doi.org/10.1007/s12609-016-0223-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-016-0223-6