Abstract
Objectives
To investigate the association of three muscle mass adjustment methods with low muscle strength (MS) and low physical function (PF) defined by the Asian Working Group for Sarcopenia (AWGS) 2019 criteria.
Design
Cross-sectional study.
Setting
Clinical setting.
Participants
We included 361 outpatients (77.9 ± 5.9 years) without scheduled orthopedic surgery or activities of daily living disability.
Measurements
Appendicular skeletal muscle mass (ASM) was measured by dual-energy X-ray absorptiometry, then divided by height-square (ht2), body weight, and body mass index (BMI) to calculate the ASM indexes. We assessed grip strength, gait speed, short physical performance battery, and five-time chair stand test. Low MS and low PF were defined by the AWGS2019 criteria. To compare the association of three muscle mass adjustments with low MS and low PF, multiple logistic regression analysis was performed, adjusted for age in each sex.
Results
Participants with low MS was 31.5%, low PF was 50.1%. After adjustment, only ASM/BMI was significantly associated with all independent variables, such as low MS, low PF, and either of these, with the odds ratios of 2.09, 2.08, and 2.50 for males; and 1.87, 2.43, and 2.71 for females, respectively.
Conclusion
Our findings suggest that ASM/BMI is best associated with low MS and low PF in older Japanese outpatients. Longitudinal outcome studies are needed to confirm our findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sarcopenia has been described by Rosenberg and Roubenoff (1) as aging-related muscle mass loss and is currently recognized as a disease associated with low muscle mass and reduced muscle function (2, 3).
In recent years, low muscle strength has been suggested as a better predictor of adverse health outcomes than muscle mass loss (2, 3). Thus, in the revised sarcopenia diagnostic criteria of the European Working Group on Sarcopenia in Older People (EWGSOP), measurement of muscle strength is prioritized over assessment of muscle mass in the diagnostic process (2). However, muscle mass loss is essential for definitive diagnosis, and dual-energy X-ray absorptiometry (DXA) is recommended for quantifying muscle mass in the clinical setting (2, 3).
The EWGSOP 2 and Asian Working Group for Sarcopenia (AWGS) 2019 consensus reports set the cutoff value of muscle mass by dividing appendicular skeletal muscle mass (ASM) by height squared (ASM/ht2) (2–4). However, a previous study has suggested that obese older adults have lower fat-free mass (FFM) per body weight than non-obese older adults, despite the fact that absolute FFM was greater in obese older adults in that study (5). This suggests an important limitation of ASM/ht2 for assessing muscle mass. In fact, previous studies have shown that ASM/ht2 does not have a strong relationship with physical disability (6, 7). Other methods of assessing muscle mass using body weight (ASM/weight) (8) or body mass index (BMI, ASM/BMI) (9) have been proposed in addition to ASM/ht2. EWGSOP 2 recognizes that it is unclear which method is best and whether those methods are applicable to all populations (2), and AWGS 2019 also states that there is lack of evidence about applicability of these methods to Asian people (3). Although it has been established that proper diagnosis of sarcopenia is essential in medical care, there is no consensus on the usefulness of other measuring methods apart from DXA, such as computed tomography and D3-creatine dilution (2, 3, 10).
Therefore, we investigated the association of three methods of muscle mass adjustment (i.e., ASM/ht2, ASM/weight, and ASM/BMI) with low muscle strength and low physical function in Japanese older outpatients.
Methods
Study setting and participants
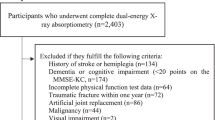
Data for this cross-sectional study was obtained from the Frail Registry Study, which included outpatients in a general geriatric hospital in Aichi, Obu, Japan, between June 2017 and July 2019. All 497 participants were outpatients of the frailty clinic, and physical composition and function were measured at the first visit to the clinic. There was no patient with activities of daily living (ADL) disability, as defined by Katz index score <5 (11).
We excluded participants aged <65 years (n=28), those who were planning orthopedic surgery (n=87), those who had missing DXA data (n=3), and those in whom muscle function was not measured (n=18). Finally, data from 361 patients (134 males, 37.1%) were analyzed.
All participants provided written informed consent before being included in the study. The study was conducted in accordance with the Declaration of Helsinki, and the Ethics Committee of Human Research of the National Center for Geriatrics and Gerontology, Japan, approved the study protocol (No. 881-7).
Independent variables: three methods of muscle mass adjustment
Body composition was measured using DXA (Lunar iDXA; GE Healthcare, Chicago, IL) and ASM was calculated by summing the values of lean soft-tissue mass in the arms and legs as described by Heymsfield et al. (12).
-
1)
ASM/ht2 was calculated as follows: ASM/ht2 = ASM (kg)/[height (m)]2 (4).
-
2)
ASM/weight was calculated as follows: ASM/weight = ASM (kg) / body weight (kg) x 100 (8).
-
3)
ASM/BMI was proposed by the Foundation for the National Institutes of Health (FNIH) Sarcopenia Project in 2014 (9). BMI was calculated from anthropometric data, using the following formula: BMI = weight (kg) / [height (m)]2. ASM/BMI was calculated as follows: ASM/BMI = ASM (kg) / BMI (kg/m2).
Outcome measures: muscle strength and physical function
Low muscle strength was defined as grip strength <28 kg for males and <18 kg for females, based on the AWGS 2019 criteria (3). Maximal grip strength was measured twice in each hand with the patient in sitting position, using a new hand dynamometer developed in our institute (13).
Low physical function was defined as low performance in one or more of three functional assessment parameters (i.e., gait speed, short physical performance battery (SPPB), and five-time chair stand test (5CS)), based on the AWGS 2019 criteria (3). Low gait speed was defined as usual gait speed <1.0 m/s as measured using the detection plate walkway (Anima Co., Ltd., Tokyo, Japan). Low SPPB was defined as score ≤9, and low 5CS was defined as ≥12 seconds. These functions were measured by trained physiotherapists.
Statistical analysis
The mean and standard deviation (SD) were calculated. T-test or chi-square test was used to compare patients with or without low muscle strength, and patients with or without low physical function.
We compared the age-adjusted odds ratios (ORs) of ASM/ht2, ASM/weight, and ASM/BMI for low muscle strength and low physical function using multiple logistic regression analysis. The SDs of ASM/ht2, ASM/weight, and ASM/BMI were calculated for both males and females. We set the -1SDs of these three methods as the independent variables and set low muscle strength, low physical function, and either of the two as the outcome measures.
The receiver-operating characteristic (ROC) curves and the area under the curve (AUC) of ASM/ht2, ASM/weight, and ASM/BMI were obtained. The Youden indexes (YIs) of ASM/ht2, ASM/weight, and ASM/BMI were calculated as sensitivity + specificity −1.
Analyses were performed with Statistical Analysis System version 9.3 (SAS Institute, Cary, NC), and only the ROC analysis was performed with the Statistical Package for Social Sciences version 23.0 (IBM Japan, Tokyo, Japan). Statistical significance was indicated by a two-sided P-value <0.05. We repeated the analysis for the three independent measures; however, multiplicity correction of statistical significance was not considered because we judged by the statistical results. This interpretation coincides with the view of the American Statistical Association (14).
Results
Table 1 shows the characteristics of the study participants. Of 361 participants, 31.5% had low muscle strength, and 50.1% had low physical function. ASM (kg) and ASM/BMI in participants with low muscle strength were significantly lower than in participants with normal muscle strength, and these observations were also detected in participants with or without low physical function (all P <0.01), in both males and females; however, ASM/ht2 was not significantly different between groups. Table 2 shows the comparisons of the ORs of the three muscle mass adjustment methods for both low muscle strength and low physical function. In both males and females, only ASM/BMI was associated with low muscle strength, low physical function, and either of these. Figure 1 shows the ROC curves for low muscle strength and low physical function based on the three muscle mass adjustment methods. ASM/BMI showed the highest AUCs for low muscle strength, low physical function, and either of these, in both males and females.
ROC curves of the three muscle mass adjustment methods for low muscle strength and low physical function
(A) to (F) show the ROC curves, AUCs, cut-off points based on maximum YIs, sensitivities, and specificities of the three methods of muscle mass assessment (i.e., ASM/BMI, ASM/ht2, and ASM/weight) for low muscle strength and function, as defined by AWGS 2019 criteria, in both males and females. (A) and (B) show the results for low muscle strength, which was defined as maximal grip strength <28 kg for males and <18 kg for females. (C) and (D) show the results for low physical function, which was defined as gait speed <1.0 m/s, SPPB ≤9 scores, and 5CS ≥12 seconds, and participants were described as having low physical function when they had low function based on any of these measures. (E) and (F) show the results for patients who had either low muscle strength or low physical function; ROC, receiver operating characteristic; AUC, area under the curve; YI, Youden index; ASM, appendicular skeletal muscle mass; BMI, body mass index; AWGS, Asian Working Group for Sarcopenia; SPPB, short physical performance battery; 5CS, five-time chair stand test
Discussion
We investigated the cross-sectional association of three methods of muscle mass adjustment (i.e., ASM/ht2, ASM/weight, and ASM/BMI) with low muscle strength and physical function in order to determine which of these methods is suitable for discriminating low muscle strength and low physical function. After age adjustment, in both males and females, only ASM/BMI was significantly associated with low strength and function, which were defined by the AWGS 2019 criteria. Besides, the AUC of ASM/BMI for these outcomes was the highest. AWGS 2019 criteria have defined sarcopenia as low muscle mass with low muscle strength or physical function (3). Low muscle strength and physical function predict adverse outcomes such as mobility limitation, falls, ADL disability, and mortality (15). Thus, our findings suggest that ASM/BMI can detect sarcopenia and may more accurately predict prognosis.
In the definitive criteria for sarcopenia, the measurement of muscle mass is important, but various problems have been identified (2, 3). Villareal et al. showed that muscle function in obese older adults was similar to that in non-obese frail older adults (5). Zoico et al. reported that high body fat status significantly predicted functional limitation in older women, whereas low muscle mass status was not significant (16). These previous studies suggest that adjustment of muscle mass by height misses obese individuals who are at high risk for poor health outcomes (5, 16).
ASM/weight was also proposed by Janssen et al. because mobility and ADL are influenced by body size (8). However, ASM/BMI may be superior to ASM/weight in adjusting for body size. Previous studies have suggested that ASM/BMI is an effective method for obese, diabetic, and pre-diabetic patients (9, 17, 18). Bahat et al. investigated the cutoff points of ASM/weight and ASM/BMI for Turkish populations and observed that ASM/BMI was the best predictor of low grip strength (19). These findings support our study results.
The FNIH Sarcopenia Project proposed ASM/BMI as the best adjustment method that discriminated low grip strength in Westerners (9). Our findings showed similar results to the FNIH study. On the other hand, a pooled data analysis by the Sarcopenia Definitions and Outcomes Consortium found no remarkable differences between methods of muscle mass adjustment for discriminating slow walking speed (20). One possible explanation for the discrepancy in results would be ethnic differences in body composition and walking speed (21–23). It has been reported that Asians have a higher rate of body fat and a greater amount of intramuscular fat than Westerners, even if their BMI is comparable (21, 22). A previous study comparing walking speed between older Japanese and Caucasians suggested that the Japanese had faster walking speeds despite having lower BMIs (23). These findings indicate that ASM/ht2 may underestimate the relationship between physical performance and muscle mass, which may partly explain our study results.
So far, few studies have found an association between ASM/BMI and low muscle strength and function in older Asians (3, 9, 24). In addition, the Asian sarcopenia criteria have just been revised in 2019 (3). Our findings suggest that ASM/BMI is also applicable to Asian older adults and is useful for future clinical care and study.
This study has several limitations. First, this was a small cross-sectional study; thus, longitudinal association of the three muscle mass adjustment methods with adverse outcomes such as mortality should be investigated in a future study. Second, the study participants were Japanese outpatients in a frailty clinic, and it is possible that there were more functionally declined participants among this cohort than community-dwellers.
In conclusion, our findings suggest that ASM/BMI is best associated with low muscle strength and function in Japanese older patients and may be able to identify sarcopenia, regardless of body size. Future studies that clarify the optimal cutoff of ASM/BMI for Asian older adults in all settings are needed.
Abbreviations
- ADL:
-
activities of daily living
- ASM:
-
appendicular skeletal muscle mass
- AUC:
-
area under the curve
- AWGS:
-
Asian Working Group for Sarcopenia
- BMI:
-
body mass index
- CI:
-
confidence interval
- DXA:
-
dual-energy X-ray absorptiometry
- EWGSOP:
-
European Working Group on Sarcopenia in Older People
- FFM:
-
fat-free mass
- 5CS:
-
five-time chair stand test
- FNIH:
-
Foundation for the National Institutes of Health
- ROC:
-
receiver-operating characteristic
- OR:
-
odds ratios
- SPPB:
-
short physical performance battery
- SD:
-
standard deviation
References
Rosenberg IH, Roubenoff R. Stalking sarcopenia. Ann Intern Med 1995;123:727–728.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16–31.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, Jang HC, Kang L, Kim M, Kim S, Kojima T, Kuzuya M, Lee JSW, Lee SY, Lee WJ, Lee Y, Liang CK, Lim JY, Lim WS, Peng LN, Sugimoto K, Tanaka T, Won CW, Yamada M, Zhang T, Akishita M, Arai H. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc 2020;21:300–307.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 1998;147:755–763.
Villareal DT, Banks M, Siener C, Sinacore DR, Klein S. Physical frailty and body composition in obese elderly men and women. Obes Res 2004;12:913–920.
Delmonico MJ, Harris TB, Lee JS, Visser M, Nevitt M, Kritchevsky SB, Tylavsky FA, Newman AB. Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc 2007;55:769–774.
Newman AB, Kupelian V, Visser M, Simonsick E, Goodpaster B, Nevitt M, Kritchevsky SB, Tylavsky FA, Rubin SM, Harris TB. Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc 2003;51:1602–1609.
Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc 2002;50:889–896.
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, Ferrucci L, Guralnik JM, Fragala MS, Kenny AM, Kiel DP, Kritchevsky SB, Shardell MD, Dam TT, Vassileva MT. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 2014;69:547–558.
Bauer JM, Morley JE. Editorial: Body composition measurements in older adults. Curr Opin Clin Nutr Metab Care 2020;23:1–3.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963;185:914–919.
Heymsfield SB, Smith R, Aulet M, Bensen B, Lichtman S, Wang J, Pierson RN, Jr. Appendicular skeletal muscle mass: measurement by dual-photon absorptiometry. Am J Clin Nutr 1990;52:214–218.
Matsui Y, Fujita R, Harada A, Sakurai T, Nemoto T, Noda N, Toba K. Association of grip strength and related indices with independence of activities of daily living in older adults, investigated by a newly-developed grip strength measuring device. Geriatr Gerontol Int 2014;14:77–86.
Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. Am Stat 2016;70:129–133.
Bhasin S, Travison TG, Manini TM, Patel S, Pencina KM, Fielding RA, Magaziner JM, Newman AB, Kiel DP, Cooper C, Guralnik JM, Cauley JA, Arai H, Clark BC, Landi F, Schaap LA, Pereira SL, Rooks D, Woo J, Woodhouse LJ, Binder E, Brown T, Shardell M, Xue QL, D’Agostino RB, Sr., Orwig D, Gorsicki G, Correa-De-Araujo R, Cawthon PM. Sarcopenia definition: the position statements of the Sarcopenia Definition and Outcomes Consortium. J Am Geriatr Soc 2020;68:1410–1418.
Zoico E, Di Francesco V, Guralnik JM, Mazzali G, Bortolani A, Guariento S, Sergi G, Bosello O, Zamboni M. Physical disability and muscular strength in relation to obesity and different body composition indexes in a sample of healthy elderly women. Int J Obes Relat Metab Disord 2004;28:234–241.
Dabak MR, Sevinç E, Tüzün S, Gün E. Evaluation of muscle mass in obesity, prediabetes and diabetes mellitus by different equations used for the measurement of muscle mass. Diabetes Metab Syndr 2019;13:2148–2151.
Kim KM, Jang HC, Lim S. Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean J Intern Med 2016;31:643–650.
Bahat G, Tufan A, Kilic C, Öztürk S, Akpinar TS, Kose M, Erten N, Karan MA, Cruz-Jentoft AJ. Cut-off points for weight and body mass index adjusted bioimpedance analysis measurements of muscle mass. Aging Clin Exp Res 2019;31:935–942.
Manini TM, Patel SM, Newman AB, Travison TG, Kiel DP, Shardell MD, Pencina KM, Wilson KE, Kelly TL, Massaro JM, Fielding RA, Magaziner J, Correa-de-Araujo R, Kwok TCY, Hirani V, Karlsson MK, D’Agostino RB, Sr., Mellström D, Ohlsson C, Ribom E, Jordan JM, Bhasin S, Cawthon PM. Identification of Sarcopenia Components That Discriminate Slow Walking Speed: A Pooled Data Analysis. J Am Geriatr Soc 2020; 68:1419–1428.
Nazare JA, Smith JD, Borel AL, Haffner SM, Balkau B, Ross R, Massien C, Alméras N, Després JP. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the International Study of Prediction of Intra-Abdominal Adiposity and Its Relationship With Cardiometabolic Risk/Intra-Abdominal Adiposity. Am J Clin Nutr 2012; 96:714–726.
Wulan SN, Westerterp KR, Plasqui G. Ethnic differences in body composition and the associated metabolic profile: a comparative study between Asians and Caucasians. Maturitas 2010; 65:315–319.
Aoyagi K, Ross PD, Nevitt MC, Davis JW, Wasnich RD, Hayashi T, Takemoto T. Comparison of performance-based measures among native Japanese, Japanese-Americans in Hawaii and Caucasian women in the United States, ages 65 years and over: a cross-sectional study. BMC Geriatr 2001; 1:3.
Moon JH, Kim KM, Kim JH, Moon JH, Choi SH, Lim S, Lim JY, Kim KW, Park KS, Jang HC. Predictive values of the new sarcopenia index by the Foundation for the National Institutes of Health Sarcopenia Project for mortality among older Korean adults. PLoS One 2016;11:e0166344.49.
Fougere B, Goisser S, Cantet C, Soriano G, Guyonnet S, De Souto Barreto P, et al. Omega-3 fatty acid levels in red blood cell membranes and physical decline over 3 years: longitudinal data from the MAPT study. Geroscience. 2017;39(4):429–37.
Acknowledgments
We would like to thank all study participants and all staff at the frailty clinic in the Center for Frailty and Locomotive Syndrome, National Center for Geriatrics and Gerontology, for their cooperation and contribution to this study. We also thank Editage (https://www.editage.com) for English language editing. This study was supported in part by Research Funding for Longevity Sciences from the National Center for Geriatrics and Gerontology, Japan (grant number 29-12, 30-6). No grant provider played any role in the design, analysis, or writing of this article.
Author information
Authors and Affiliations
Contributions
Authors’ contributions: Kaori Kinoshita conceived the study design, performed the data analysis, interpreted the results, and drafted the initial manuscript. Shosuke Satake collected the data, conceived the study design, interpreted the results, contributed to discussions, and had primary responsibility for the final content. Yasumoto Matsui performed project management, collected the data, interpreted the results, and contributed to discussions. Hidenori Arai collected the data, interpreted the results, contributed to discussions, and supervised the study. All authors critically revised the manuscript for intellectual content and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest: All authors declare no conflict of interest in the present study.
Additional information
Sources of Support: This study was supported in part by Research Funding for Longevity Sciences from the National Center for Geriatrics and Gerontology, Japan (grant number 29-12, 30-6). No grant provider played any role in the design, analysis, or writing of this article.
Rights and permissions
About this article
Cite this article
Kinoshita, K., Satake, S., Matsui, Y. et al. Quantifying Muscle Mass by Adjusting for Body Mass Index Is the Best for Discriminating Low Strength and Function in Japanese Older Outpatients. J Nutr Health Aging 25, 501–506 (2021). https://doi.org/10.1007/s12603-020-1557-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1557-3