Abstract
Background
Sarcopenia can be characterized by European Consensus for Sarcopenia (EWGSOP2) criteria, but it methods are not easily accessible. Likewise, the Strength, Assistance with walking, Rise from a Chair, Climb stairs and Falls (SARC-F) has been proposed.
Objective
The aim of this study was i) to evaluate the prevalence for risk sarcopenia and ii) to correlate the SARC-F with components of the EWGSOP2 consensus in hemodialysis (HD) patients.
Measurements
This cross-sectional study enrolled ninety-five (male n= 59; 62%) HD older patients. Sarcopenia risk was assessed using the SARC-F, which ≥4 score indicates sarcopenia risk. Sarcopenia was confirmed through of the EWGSOP2 consensus, including the handgrip strength (HGS <27kg for men and <16kg for women) using the dynamometer, muscle mass through appendicular muscle mass (ASMI/m2 <7.0 kg/m2 for men and 5.5 kg/m2 for women) using the bioimpedance electrical, and physical performance through of gait speed (GS <0.8 m/s).
Results
From 95 patients, n=21(22%) presented sarcopenia risk. SARC-F ≥4 group are older (64.9±13.9 vs. 56.9±14.6 y, p= 0.028), presented lower ASMI (7.4±1.2 vs. 8.3±1.8 kg/m2, p=0.033), HGS (20.5±5.7 vs. 27.2±10.2 kg, p=0.005), and GS (0.5±0.1 vs. 0.7±0.1 m/s, p=0.001) than SARC-F<4 group. SARC-F score was negatively correlated with EWGSOP2 components: ASMI × SARC-F (r=−0.27, p=0.007), HGS × SARC-F (r=−0.35, p=0.0005), and GS × SARC-F (r=−0.47, p<0.0001). Although, no difference of number of patients with low or normal ASMI values was found, 62% and 95% of SARC-F≥4 group patients presented low HGS and gait speed, respectively.
Conclusions
In older HD patients, 22% presented sarcopenia risk. In addition, SARC-F is better correlated with muscle function indicators (HGS and gait speed) than muscle mass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, the European Working Group on Sarcopenia in Older People (EWGSOP2) defined the sarcopenia trough of low muscle strength (primary criteria), followed by low muscle quantity or quality and low physical performance (1). However, techniques to measure muscle quantity, quality and physical performance are not accessible in clinical practice, since same instruments are quite expensive and no accessible in large scale.
Likewise, the Strength, Assistance with walking, Rise from a Chair, Climb stairs and Falls (SARC-F) has been proposed to screening patients with sarcopenia risk (1). SARC-F is a validated and inexpensive tool which is rapidly applied and presents low-moderate sensitivity and high specificity to classify a person with sarcopenia risk (1, 2). In addition, SARC-F have been demonstrated higher sensitivity and specificity to assessment the skeletal muscle function (2). However, in chronic kidney disease (CKD) patients undergone hemodialysis (HD) this instrument has not been used yet.
Considering that HD patients suffer of protein wasting (3, 4) and based on absence of studies that find-cases sarcopenia using the SARC-F questionnaire, we hypothesized SARC-F questionnaire is correlated with HGS, gait-speed and muscle mass index. Therefore, the aim of this study was i) to evaluate the prevalence of sarcopenia risk and ii) to correlate the SARC-F score with components of the EWGSOP2 consensus in HD patients.
Materials and Methods
Design of study and patients
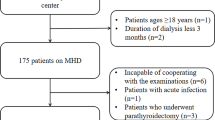
This cross-sectional study included patients diagnosed with chronic kidney disease in HD of both genders (male n= 59; 62%) and with a mean age of 60.9 years. Regarding ethical procedures, patients were informed about their participation in the research, as interested in participating in the study, were directed to read and sign the Informed Consent Form approved by the Research Ethics Committee of the Federal Lniversity of Goiâs under the number 3.384.866/2019. The recruitment of patients was done for convenience in two HD clinics. The total sample consisted of 95 patients.
Sarcopenia assessment
The assessment of the risk of sarcopenia was assessed using the SARC-F, a questionnaire for screening the risk for sarcopenia (1, 5). SARC-F contain five items, Strength, Assistance for walking, Rise from a chair, Climb stairs, and Falls. It results range from 0 to 2 points, where 0 meant better functional capacity and 2 worse functional capacity. Cut-off point with SARC-F ≥4 indicates sarcopenia risk and SARC-F <4 no sarcopenia.
In the current definition for sarcopenia, EWGSOP2 consensus includes the HGS assessment as the primary reference for sarcopenia. And it is classified into three stages: probable sarcopenia, sarcopenia and severe sarcopenia. Probable sarcopenia is identified by low muscle strength. Sarcopenia is defined by the assessment of low muscle quality or quantity. And severe sarcopenia involves the previous components plus poor physical performance (1).
In order to classify sarcopenia according to the EWGSOP, measure up i) muscle strength using the dynamometer to assess the HGS (HGS <27kg for men and <16kg for women); ii) muscle mass through appendicular muscle mass (ASM/m2 <7.0 kg/m2 for men and 5,5 kg/m2 for women) using the bioimpedance electrical, and iii) physical performance through of gait speed (GS <0.8 m/s) (1).
Statistical analyses
The normality of the data was tested using the Kolmogorov-Smirnov test and the MedCalc®, Belgium software was used for statistical analysis. Descriptive statistics were applied for absolute and relative frequencies, means and standard deviation. The comparative analysis was performed using the Student’s T test or chi-square. Correlations between the components of sarcopenia and SARC-F were performed using Pearson’s correlation test. The level of statistical significance was set at 5% (p <0.05).
Results
Our sample was divided into two groups, no sarcopenia (SARC-F <4: 0.8+0.8 score, n=74/78%) and with sarcopenia risk (SARC-F ≥ 4: 6.8+0.7 score, n=21/22%) (Table 1). Although no difference in time of HD diagnosis (p= 0.248) and calf circumference (p= 0.179), we found older patients in the SARC-F ≥4 group than in the SARC-F <4 (64.9+13.9 vs. 56.9+14.6 years, p= 0.028, respectively). Additionally, SARC-F ≥4 group presented lower ASMI (SARC-F ≥4: 7.4+1.2 kg/m2 vs. SARC-F <4: 8.3+1.8 kg/m2, p= 0.033), HGS (SARC-F ≥4: 20.5+5.7 vs. SARC-F <4: 27.2+10.2 kg, p= 0.005), and gait speed (SARC-F ≥4: 0.5+0.1 vs. SARC-F <4: 0.7+0.1 m/s, p= 0.001) when compared with SARC-F <4 group (Table 1).
Although there is not difference between groups in number of patients with low or normal appendicular muscle mass (p=0.815), was observed that the SARC-F ≥4 group have more patients with low HGS and gait speed than SARC-F <4 group (HGS: 61.9% vs. 31.1%, respectively, p= 0.020) and (gait speed: 95.2% vs. 54.0%, respectively, p= 0.001) (Table 2).
SARC-F values were negatively correlated with EWGSOP2 components: ASMI x SARC-F (r= -0.27, p= 0.007), HGS × SARC-F (r= −0.35, p= .0005), and gait speed x SARC-F (r= −0.47, p< 0.0001) (Figure 1).
Discussion
To the best of our knowledge, this is the first study to correlate the SARC-F questionnaire as a screening for sarcopenia and EWGSOP2 indicators in older hemodialysis patients. The main finding of our study was that 22% of HD patients presented sarcopenia risk and that SARC-F score was better correlated with muscle function indicators (HGS and gait speed) than muscle mass.
In previous study, we found that approximately one-third of HD patients presented pre-sarcopenia when evaluated by appendicular lean mass using the DXA (4). Although no study assessed the sarcopenia risk, using the SARC-F questionnaire was observed that 22% of HD patients may be affected by sarcopenia. Recently, an Italian study evaluated HD patients and found that presence of sarcopenia when assessed using the EWGSOP2 was associated with lower HGS, mid arm muscle circumference, and gait speed test. In addition, the prevalence of sarcopenia was similar to our study (23.8%) (6). Thus, independently of the sarcopenia definition, their components are associated with worse HD outcomes (7).
In the present study, SARC-F ≥4 patients did not show difference in calf circumference, since it evaluation was done during intermediary HD session in which patients are not affected by hydration. Indeed, calf circumference when assessed in pre-dialysis has been demonstrated highly associated with overhydration (8).
Although, there is no difference in the length of HD between the non-sarcopenia and sarcopenia risk group, is known that length of time of HD is associated with lower psosas muscle index (9) and higher mortality (10).
Although the SARC-F score was correlated with EWGSOP2 components, we did find no patients with low ASMI in the SARC-F ≥4. However, 62% and 95% of SARC-F ≥4 group patients presented low HGS and gait speed, respectively. Thus, these data suggesting that SARC-F questionnaire is better to determinate any alteration in muscle strength and physical performance rather than quantity of skeletal muscle mass. Indeed, in clinical routine the SARC-F questionnaire is useful to sarcopenia screening as well as muscle function evaluation and has been validated in Portuguese version (11).
Our main limitation was the small sample size. However, our study was the first to use SARC-F to screening the risk for sarcopenia, the specificity and sensibility of SARC-F to predict the sarcopenia remains to be tested in a major population and from different countries. Additionally, cross-sectional design does not allow to establish a cause and effect relationship. As strengths, these data provide a new evidence for HD patients, since SARC-F appear be a convenient tool for health care professionals who are encouraged to screen the muscle function loss (12), thus as in patients with others chronic diseases, such as cancer (13).
In conclusion, 22% of older patients presented sarcopenia risk when assessed by SARC-F questionnaire. In addition, SARC-F is better correlated with muscle function indicators (HGS and gait speed) than muscle mass (ASMI). However, this evidence remains to be elucidated for further studies.
References
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M, Writing Group for the European Working Group on Sarcopenia in Older P, the Extended Group for E. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:601
Bahat G, Yilmaz O, Kilic C, Oren MM, Karan MA. 2 Performance of SARC-F in Regard to Sarcopenia Definitions, Muscle Mass and Functional Measures. J Nutr Health Aging 2018;22:898–903
Marini ACB, Pimentel GD. Is body weight or muscle strength correlated with the Malnutrition Inflammation Score (MIS)? A cross-sectional study in hemodialysis patients. Clin Nutr ESPEN 2019;33:276–8
Marini AC, Motobu RD, Freitas ATV, Laviano A, Pimentel GD. Pre-sarcopenia in patients undergoing hemodialysis: Prevalence and association with biochemical parameters. Clin Nutr ESPEN 2018;28:236–8
Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc 2013;14:531–2
Vettoretti S, Caldiroli L, Armelloni S, Ferrari C, Cesari M, Messa P. Sarcopenia is Associated with Malnutrition but Not with Systemic Inflammation in Older Persons with Advanced CKD. Nutrients 2019;11
Moorthi RN, Avin KG. 2 Clinical relevance of sarcopenia in chronic kidney disease. Curr Opin Nephrol Hypertens 2017;26:219–28
Vasko R, Muller GA, Ratliff BB, Jung K, Gauczinski S, Koziolek MJ. Clinical judgment is the most important element in overhydration assessment of chronic hemodialysis patients. Clin Exp Nephrol 2013;17:563–8
Takamoto D, Kawahara T, MochizuM T, Makiyama K, Teranishi J, Uemura H. A Longer History of Hemodialysis Can Lead to Sarcopenia in Renal Transplantation Patients. Transplant Proc 2018;50:2447–50
Kittiskulnam P, Chertow GM, Carrero JJ, Delgado C, Kaysen GA, Johansen KL. Sarcopenia and its individual criteria are associated, in part, with mortality among patients on hemodialysis. Kidney Int 2017;92:238–47
Barbosa-Silva TG, Menezes AM, Bielemann RM, Malmstrom TK, Gonzalez MC, Grupo de Estudos em Composicao Corporal e N. Enhancing SARC-F: Improving Sarcopenia Screening in the Clinical Practice. J Am Med Dir Assoc 2016;17:1136–41
Bauer J, Morley JE, Schols A, Ferrucci L, Cruz-Jentoft AJ, Dent E, Baracos VE, Crawford JA, Doehner W, Heymsfield SB, Jatoi A, Kalantar-Zadeh K, Lainscak M, Landi F, Laviano A, Mancuso M, Muscaritoli M, Prado CM, Strasser F, von Haehling S, Coats AJS, Anker SD. Sarcopenia: A Time for Action. An SCWD Position Paper. J Cachexia Sarcopenia Muscle 2019;10:956–61
Borges TC, Gomes TLN, Pimentel GD. Sarcopenia as a predictor of nutritional status and comorbidities in hospitalized patients with cancer: A cross-sectional study. Nutrition 2019;73:110703
Acknowledgements
ACBM would like to thank the Capes, Brazil. GDP would like to The Brazilian National Council for Scientific and Technological Development (CNPq, Brazil, 312252/2019-6).
Author information
Authors and Affiliations
Contributions
ACBM and GDP contributed to the study design. ACBM, DRSP, and JAF participated of collection data. ACBM, DRSP, JAF, and GDP performed the literature search and discussed the paper. ACBM, DRSP, JAF, and GDP wrote the manuscript. ACBM and GDP participated of critical discussion of data and reviewed the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
All authors declare: 1. That this manuscript is not published elsewhere; 2. Any conflicts of interest; 3. They meet criteria for authorship and ensure appropriate acknowledgments made in the manuscript; 4. Appropriate funding statements in the manuscript; 5. They will inform the journal if any subsequent errors are found in the manuscript.
Additional information
Conflict of Interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Marini, A.C.B., Perez, D.R.S., Fleuri, J.A. et al. SARC-F is Better Correlated with Muscle Function Indicators than Muscle Mass in Older Hemodialysis Patients. J Nutr Health Aging 24, 999–1002 (2020). https://doi.org/10.1007/s12603-020-1510-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1510-5