Abstract
Background
Vitamin D is the one of the most common nutritional deficiencies worldwide, and insufficiency or deficiency can be associated with musculoskeletal and non-skeletal conditions such as cancer, cardiovascular disease and diabetes mellitus.
Objective
Recent data suggests that Vitamin D is relatively safe and toxicity is rarer than previously indicated. However, international guidelines regarding dosage and target plasma levels are conflicting. Moreover multiple well-designed studies of healthy older adults, unselected in terms of Vitamin D status, have revealed largely negative results (with the possible exception of older patients in care homes/hospitals) in terms of improvement in musculoskeletal and non-skeletal conditions to date.
Conclusion
On that basis, it is suggested that future trials regarding Vitamin D supplementation should be carried out in high-risk groups. The use of published criteria for evaluating the effect of nutrients and targeting of individuals with Vitamin D insufficiency and deficiency for inclusion in such studies is also proposed. The identification of specific subgroups that will benefit from supplementation and replacement, and the establishment of a scientific basis for such therapy, should be possible with this approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D deficiency is the commonest nutritional deficiency globally, however optimal dosage regimens remain uncertain (1). It is estimated that approximately one billion people worldwide have vitamin D deficiency, and vitamin D insufficiency affects nearly 50% (2).
The lack of consensus regarding supplementation has been previously highlighted (3). International guidelines are conflicting; the Institute of Medicine (IOM) recommends a a serum vitamin D (25(OH)D) of 50 nmol/L and defines a 25(OH)D concentration less than 30 nmol/L as deficiency (4), whereas the Endocrine Society recommends a target 25(OH)D of 75 nmol/L and defines deficiency as a 25(OH) D less than 50nmol/L (5). The Scientific Advisory Committee on Nutrition (SACN) also published an independent report in 2016 with recommendations regarding vitamin D and 25nmol/L defined as the “population protection level” (6). Table 1 summarises current guidelines on target levels.
Some authorities have suggested widespread supplementation with daily doses of 2,000 to 4,000 IL of vitamin D and toxicity is probably rare (7). An association of Vitamin D insufficiency with musculoskeletal and non-skeletal conditions such as cancer, cardiovascular disease, and inflammatory bowel disease is widely recognised. Many non-randomised cohort studies have produced misleading and contradictory results, and it is not proposed to dwell on that data in this review. Recent studies from Bolland (8) and Pittas (9) highlight negative results with regard to improving musculoskeletal health and preventing type 2 diabetes mellitus respectively.
This article highlights a review of intervention studies and proposes a more targeted approach to prospective vitamin D intervention research in the future.
Outcomes of Intervention Studies
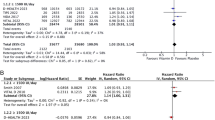
Almost all major studies of vitamin D therapy have recruited patients unselected for baseline vitamin status. In 2018, Bolland et al. carried out a systematic review and metaanalysis regarding the effects of vitamin D supplementation on musculoskeletal health (8). Eighty-one randomised controlled trials were identified which reported on falls, fractures or bone mineral density. In pooled analyses, vitamin D had no effect on total fracture (36 trials; n=44 790, relative risk 1•00, 95% CI 0•93–l•07), hip fracture (20 trials; n=36 655, 1•11, 0•97–l•26), or falls (37 trials; n=34 144, 0•97, 0•93–l•02). These results were similar in trials comparing high versus low-dose vitamin D, and in subgroup analyses of trials including daily doses exceeding 800IL.
Based on a known association between low serum 25(OH) D levels and the risk of type 2 diabetes, whether vitamin D supplementation lowers the risk of developing diabetes was investigated by Pittas et al (9). Adults with pre-diabetes were randomly assigned to receive either 4000IL per day of vitamin D3 or placebo regardless of baseline serum 25(OH)D levels. The primary outcome was time-to-event analysis of new-onset diabetes. At follow-up at 2.5 years, new-onset diabetes had occurred in 293 participants in the vitamin D group and 323 in the placebo group. It was concluded that in high risk individuals for new-onset type 2 diabetes mellitus, vitamin D supplementation did not significantly reduce the risk of diabetes compared with placebo.
In 2014 the Women’s Health Initiative (WHI) carried out a clinical trial in which over 36,000 healthy postmenopausal women >50 years (regardless of vitamin D status) were randomised to receive calcium carbonate and vitamin D (500 mg and 400 IU). Secondary analysis of this cohort was performed to address the association between vitamin D and lipid levels using a subset of 600 participants (10). In the multivariate regression model, women randomised to calcium/vitamin D had a reduction in LDL cholesterol compared to placebo, but not when Vitamin D levels were included in the analysis. Meanwhile, a small significant improvement in bone density with a trend to reduced fractures was noted in the calcium/vitamin D group in the same study (11).
Sollid et al. also analysed the effect of high-dose vitamin D supplementation on cardiovascular risk factors (and glycaemic status) in people with pre-diabetes using 20,000IU per week or placebo (12). There was a slight, but significant decrease in total and LDL cholesterol in the vitamin D group compared with the placebo group. However there was also a decrease in HDL cholesterol, and the ratio (Total Cholesterol: HDL) did not vary significantly.
The CAPS Trial (Clinical Trial of Vitamin D3 to Reduce Cancer Risk in Postmenopausal Women) randomised over two thousand healthy women >55years (regardless of Vitamin D status) to either placebo or 2000IU vitamin D/1500mg calcium daily over a four year period (13). There was no significant reduction in cancer incidence with vitamin D therapy. The VITAL (VITamin D and omegA-3 triaL) Research Group conducted a similar randomised placebo-controlled trial in men>50 years and women>55 years(again regardless of Vitamin D status)using 2000 IU vitamin D3 and 1g omega-3 fatty acids for the prevention of any cancer (and cardiovascular disease) (14). Again no reduction in cancer or cardiovascular events accrued to the supplementation group.
There are two large population-based ongoing trials at present; the FIND trial and the D-Health trial. Again, these are both unselected for vitamin D status. The FIND trial planned to study vitamin D supplementation in approximately 18,000 of the Finnish population in order to examine the relationships between vitamin D and the primary prevention of cancer and cardiovascular disease (15). Interestingly, due to recruitment and funding difficulties, the original target of 18000 participants has been revised to 2500. The D-Health trial has recruited over 21,000 participants aged between 65–84 years in Australia to receive monthly oral doses of 60,000 IU of cholecalciferol or matching placebo (16). The primary outcome is all-cause mortality. Secondary outcomes are total cancer incidence and colorectal cancer incidence.
Toxicity and Adverse Effects of Vitamin D/Calcium
Higher serum vitamin D targets (>75nmol/l) are thought to be associated with reduced falls/fractures, albeit based on somewhat controversial meta-analyses. The lower target of 50nmol/l relates to biochemical data of normalised calcium and parathyroid hormone levels at that level. The concern is raised regarding the possible toxicity of vitamin D and whether caution be exercised when supplementing or replacing it. Recent evidence suggests that concerns regarding adverse effects and toxicity may have been exaggerated.
According to Tebben et al. the definitive prevalence of vitamin D-related hypercalcaemia is unknown (17). The occurrence of vitamin D toxicity and hypercalcaemia was explored in a 16-year retrospective study of all vitamin D samples analysed in a large US teaching hospital. Lee et al. deduced that this was quite rare, with just 4 patients demonstrating clinical evidence of toxicity, one of whom was normocalcaemic (18). Table 2 highlights potential adverse events from vitamin D supplementation. Clearly large bolus therapy is not recommended due to paradoxical increases in falls and fracture rates (19–22). Prolonged excessive daily dosing (2800–100,000 IU/day) with borderline increased risk of hypercalcaemia, as demonstrated by Malihi et al (19), is not advised.
Several studies have indicated potential risk for atherosclerosis and myocardial infarction since Bolland published his meta-analysis indicating significant risk of myocardial infarction with calcium supplementation without vitamin D in 2010 (23). Some of the original cohort studies, including the seminal study of Chapuy in 1992, utilised Vitamin D and high dose calcium supplementation (24). In fact, that particular study reported a significant reduction in fractures in those prescribed that combination. However those patients were noted subsequently to have very low serum calcium, poor calcium intake and low baseline Vitamin D levels, probably not replicated in more independent community dwelling people. Meanwhile the aforementioned WHI study assessed the risk of vascular disease following calcium and vitamin D supplementation and found no increased risk (25). Many reviews showing no correlation or equivocal effects of calcium prescriptions and vascular disease had significant methodological issues (26). Therefore, in order to minimise the risk of promoting atherosclerosis and ischaemic heart disease, supplementary calcium should only be prescribed to those with low dietary calcium intake, which can be assessed with standardised questionnaires.
Suggested approach to prospective vitamin D intervention research
Approach to nutritional research
Suggested criteria for evaluation of nutrient effects have already been published (27). Heaney proposed that basal nutrient status should be measured, used as an inclusion criterion for entry into a study, and recorded in the report of the trial. Then the intervention (i.e., change in nutrient exposure or intake) should be large enough to change nutrient status and the increment quantified by suitable analyses. The hypothesis to be tested should be that a change in nutrient status (not just a change in diet) produces the sought-after effect. Finally co-nutrient status should be optimised in order to ensure that the test nutrient is the only nutrition-related limiting factor in the response.
Vitamin D studies
Translating this framework to studies of the effects of Vitamin D supplementation, baseline plasma Vitamin D levels should be measured and a sufficient dose to influence plasma levels should be given with confirmation of same by repeat plasma levels. Other deficient dietary factors (e.g. iron deficiency, which may contribute to weakness, falls, etc.) need to be optimised to avoid confounding changes in dietary factors. Ensuring adherence to study regimes and avoiding non-prescribed Vitamin D supplementation by participants is also essential.
Post-hoc analysis of some of the major intervention trials suggests that adoption of this approach a priori may have resulted in uncovering positive beneficial outcomes for participants. For example, when the subgroups which were definitely adherent to Vitamin D supplementation/placebo were analysed in the aforementioned WHI study, the risk of hip fractures was reduced by 29% (HR 0.71, 95% CI 0.52–0.97) (28). A further confounder of the WHI study was the high intake of nutritional supplements containing Vitamin D in both treatment and placebo groups of the largely middle class population studied, thus rendering identification of benefit less likely.
Vitamin D status
Inclusion of participants regardless of vitamin D status similarly compounds the evaluation of benefit from supplementation. Thus targeting of people with Vitamin D deficiency/insufficiency for prospective trials will enhance the ability to identify benefit of replacement therapy. In this regard, it is notable that the subgroup of patients studied by Pittas with Type 2 Diabetes who had documented baseline vitamin D deficiency actually had significantly reduced progression to development of diabetes (9). Moreover such individuals from high risk groups will be more likely to demonstrate benefit than broad-brush community studies of all older subjects which disregard baseline status.
Frail older people
A good example relates to frail, older adults living in institutions. A Cochrane review in 2014 inferred high quality evidence to support vitamin D and calcium as being associated with a statistically significant reduction in the incidence of new non-vertebral fractures (29). A further Cochrane review in 2018 examined interventions to prevent falls in older people in hospitals and care facilities (30). This review demonstrated moderate quality evidence (4512 participants, 4 studies) that vitamin D supplementation probably reduces the rate of falls, but likely makes little difference to the risk of falls. The population included in the analysed studies all had low vitamin D levels. On that basis, Dyer suggested that the recent conclusions by Bolland et al. (8) regarding the lack of benefit of vitamin D supplementation should not be applied to older adults in care facilities. It was further suggested that trials should target interventions to specific older populations, particularly those in long-term care (31). Higher risk individuals for insufficiency/deficiency include those with poor nutrition, inadequate housing, restricted access to outdoors, and/or chronic disease.
Other conditions
Finally, despite extensive investigation, demonstration of clear-cut benefit from vitamin D supplementation in undifferentiated groups of patients with conditions such as inflammatory bowel disease (IBD) and multiple sclerosis (MS) have likewise proved elusive despite well described associations of these conditions with vitamin D deficiency (32, 33). These review articles highlight promising studies with limited power demonstrating potential benefit regarding disease severity and response to anti-TNFs in IBD. Meanwhile possible reduction in soft outcomes like MRI plaque evolution (but not development or progression of disease) has been suggested, but not definitively established in relation to MS. Adherence to the above guidelines for further studies in at-risk individuals may help identify robust evidence of benefit in these conditions also.
Conclusion
In conclusion, future trials regarding vitamin D supplementation should be carried out using defined criteria in high-risk groups particularly with low baseline serum vitamin D levels to fully evaluate its clinical benefit in terms of major health outcomes such as fractures, falls, cancer, diabetes mellitus, cardiovascular risks, etc. Adherence to published guidelines for evaluating the effects of nutrients, including the targeting of those with Vitamin D insufficiency/deficiency for inclusion in studies is also advisable. The need for such an approach is emphasised by the largely negative publications involving studies of the general adult population to date.
References
Rosen CJ. Clinical practice. Vitamin D insufficiency. N Eng J Med 2011;364 (3):248–254. doi:https://doi.org/10.1056/NEJMcp1009570
Nair R, Maseeh A. Vitamin D: The “sunshine” vitamin. J Pharmacol Pharmacother 2012;3(2): 118–126. doi: https://doi.org/10.4103/0976-500x.95506
Gorey S, Canavan M, Robinson S, ST OK, Mulkerrin E. A review of vitamin D insufficiency and its management: a lack of evidence and consensus persists. QJM 2019;112 (3):165–167. doi:https://doi.org/10.1093/qjmed/hcy126
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 2011;96 (1):53–58. doi:https://doi.org/10.1210/jc.2010-2704
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2011;96 (7):1911–1930. doi:https://doi.org/10.1210/jc.2011-0385
England PH, 2016. SACN vitamin D and health report: The Scientific Advisory Committee on Nutrition (SACN) recommendations on vitamin D. https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report [Internet] Accessed 11 November 2019
Holick MF. Vitamin D: a d-lightful solution for health. J Investig Med 2011;59 (6):872–880. doi:https://doi.org/10.2310/JIM.0b013e318214ea2d
Bolland MJ, Grey A, Avenell A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol 2018;6 (11):847–858. doi:https://doi.org/10.1016/s2213-8587(18)30265-1
Pittas AG, Dawson-Hughes B, Sheehan P, Ware JH, Knowler WC, Aroda VR, et al. Vitamin D Supplementation and Prevention of Type 2 Diabetes. N Eng J Med 2019;381 (6):520–530. doi:https://doi.org/10.1056/NEJMoa1900906
Schnatz PF, Jiang X, Vila-Wright S, Aragaki AK, Nudy M, O’Sullivan DM, Jackson R, LeBlanc E, Robinson JG, Shikany JM, Womack CR, Martin LW, Neuhouser ML, Vitolins MZ, Song Y, Kritchevsky S, Manson JE. Calcium/vitamin D supplementation, serum 25-hydroxyvitamin D concentrations, and cholesterol profiles in the Women’s Health Initiative calcium/vitamin D randomized trial. Menopause 2014;21(8):823–833. doi:https://doi.org/10.1097/gme.0000000000000188
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Eng J Med 2006;354 (7):669–683. doi:https://doi.org/10.1056/NEJMoa055218
Sollid ST, Hutchinson MY, Fuskevag OM, Figenschau Y, Joakimsen RM, Schirmer H, Njolstad I, Svartberg J, Kamycheva E, Jorde R. No effect of high-dose vitamin D supplementation on glycemic status or cardiovascular risk factors in subjects with prediabetes. Diabetes Care 2014;37 (8):2123–2131. doi:https://doi.org/10.2337/dc14-0218
Lappe J, Watson P, Travers-Gustafson D, Recker R, Garland C, Gorham E, Baggerly K, McDonnell SL. Effect of Vitamin D and Calcium Supplementation on Cancer Incidence in Older Women: A Randomized Clinical Trial. JAMA 2017;317 (12): 1234–1243. doi:https://doi.org/10.1001/jama.2017.2115
Manson JE, Cook NR, Lee JM, Christen W, Bassuk SS, Mora S, Gibson H, Gordon D, Copeland T, D’Agostino D, Friedenberg G, Ridge C, Bubes V, Giovannucci EL, Willett WC, Buring JE. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Eng J Med 2019;380 (1):33–44. doi: https://doi.org/10.1056/NEJMoa1809944
Finnish Vitamin D Trial (2011–2018). ClinicalTrials. gov https://ClinicalTrials.gov/show/NCT01463813. [Internet] Accessed November 11 2019
Neale RE, Armstrong BK, Baxter C, Duarte Romero B, Ebeling P, English DR, Kimlin MG, McLeod DS, RL OC, van der Pols JC, Venn AJ, Webb PM, Whiteman DC, Wockner L. The D-Health Trial: A randomized trial of vitamin D for prevention of mortality and cancer. Contemp Clin Trials 2016;48:83–90. doi:10.1016/j.cct.2016.04.005
Tebben PJ, Singh RJ, Kumar R. Vitamin D-Mediated Hypercalcemia: Mechanisms, Diagnosis, and Treatment. Endocr Rev 2016;37 (5):521–547. doi:https://doi.org/10.1210/er.2016-1070
Lee JP, Tansey M, Jetton JG, Krasowski MD. Vitamin D Toxicity: A 16-Year Retrospective Study at an Academic Medical Center. Lab Med 2018;49 (2): 123–129. doi: https://doi.org/10.1093/labmed/lmx077
Malihi Z, Wu Z, Lawes CMM, Scragg R. Adverse events from large dose vitamin D supplementation taken for one year or longer. J Steroid Biochem Mol Biol 2019;188:29–37. doi:https://doi.org/10.1016/j.jsbmb.2018.12.002
Smith H, Anderson F, Raphael H, Maslin P, Crozier S, Cooper C. Effect of annual intramuscular vitamin D on fracture risk in elderly men and women—a population-based, randomized, double-blind, placebo-controlled trial. Rheumatology 2007;46 (12): 1852–1857. doi:https://doi.org/10.1093/rheumatology/kem240
Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, Nicholson GC. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA 2010;303 (18): 1815–1822. doi:https://doi.org/10.1001/jama.2010.594
Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ, Staehelin HB, Meyer OW, Theiler R, Dick W, Willett WC, Egli A. Monthly High-Dose Vitamin D Treatment for the Prevention of Functional Decline: A Randomized Clinical Trial. JAMA Intern Med 2016;176 (2):175–183. doi:https://doi.org/10.1001/jamainternmed.2015.7148
Bolland MJ, Avenell A, Baron JA, Grey A, MacLennan GS, Gamble GD, Reid IR. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ 2010;29;341:c3691. doi: https://doi.org/10.1136/bmj.c3691.
Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meunier PJ. Vitamin D3 and calcium to prevent hip fractures in elderly women. N Eng J Med 1992;327(23): 1637–42. doi:https://doi.org/10.1056/NEJM199212033272305
Hsia J, Heiss G, Ren H, Allison M, Dolan NC, Greenland P, Heckbert SR, Johnson KC, Manson JE, Sidney S, Trevisan M. Calcium/vitamin D supplementation and cardiovascular events. Circulation 2007;20;115(7):846–54. doi:https://doi.org/10.1161/CIRCULATTONAHA.106.673491
Reid IR, Birstow SM, Bolland MJ. Calcium and Cardiovascular Disease. Endocrinol Metabol 2017;32(3): 339–349. doi:https://doi.org/10.3803/EnM.2017.32.3.339
Heaney RP. Guidelines for optimizing design and analysis of clinical studies of nutrient effects. Nutr Rev 2014;72 (1):48–54. doi:https://doi.org/10.1111/nure.12090
Brunner R, Dunbar-Jacob J, Leboff MS, Granek I, Bowen D, Snetselaar LG, Shumaker SA, Ockene J, Rosal M, Wactawski-Wende J, Cauley J, Cochrane B, Tinker L, Jackson R, Wang CY, Wu L. Predictors of adherence in the Women’s Health Initiative Calcium and Vitamin D Trial. Behav Med 2009;34 (4): 145–155. doi: https://doi.org/10.3200/bmed.34.4.145-155
Avenell A, Mak JC, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst Rev 2014;(4):Cd000227. doi:https://doi.org/10.1002/14651858.CD000227.pub4
Cameron ID, Dyer SM, Panagoda CE, Murray GR, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2018;9:Cd005465. doi: https://doi.org/10.1002/14651858.CD005465.pub4
Dyer SM, Cumming RG, Hill KD, Kerse N, Cameron ID. Benefits of Vitamin D supplementation in older people living in nursing care facilities. Age Ageing 2019;48(5):761–762 doi:https://doi.org/10.1093/ageing/afz081
Fletcher J, Cooper SC, Ghosh S, Hewison M. The Role of Vitamin D in Inflammatory Bowel Disease: Mechanism to Management. Nutrients 2019; 11 (5). doi: https://doi.org/10.3390/nu11051019
Sintzel MB, Rametta M, Reder AT. Vitamin D and Multiple Sclerosis: A Comprehensive Review. Neurol Ther 2018;7 (1):59–85. doi: https://doi.org/10.1007/s40120-017-0086-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical standards: Not applicable to this type of study.
Rights and permissions
About this article
Cite this article
McGettigan, S., Mulkerrin, P., O’Shea, P.M. et al. Establishing Benefit from Vitamin D Supplementation — Adherence to Defined Criteria and Targeting of High-Risk Groups Essential?. J Nutr Health Aging 24, 827–831 (2020). https://doi.org/10.1007/s12603-020-1384-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1384-6