Abstract
Background
Sarcopenia, the age-related decrease in muscle mass and function can result in adverse health outcomes and subsequent loss of independence. Inadequate nutrition is an important contributor to the aetiology of sarcopenia, and dietary strategies are studied to prevent or delay this geriatric syndrome.
Objective
The present study investigated whether there is an association between biochemical nutrient status markers, muscle parameters and sarcopenia in community-dwelling older adults.
Design
Data from the cross-sectional Maastricht Sarcopenia study (MaSS) were used, in which skeletal muscle index (SMI), 4 meter gait speed, 5 times chair stand and handgrip strength were assessed among older adults (n=227). Sarcopenia was defined following the algorithm of the European Working Group on Sarcopenia in Older People. Fasted blood samples were analyses on amino acids levels, RBC phospholipid profile, 25-hydroxyvitamin D (25(OH)D), α-tocopherol, magnesium and homocysteine were determined in fasted blood levels. Generalized linear modelling and logistic regression were used for data analysis.
Results
Lower blood levels of essential amino acids (EAA), total branched-chain amino acids (BCAA) and leucine were associated with lower SMI (P<0.001), strength (P<0.001) and longer time to complete the chair stand (P<0.05), whereas no association was found for total amino acids (TAA). Lower levels of eicosapentaenoic acid (EPA), 25(OH)D and homocysteine were associated with lower muscle parameter values (P<0.05). No significant associations were found for SFA, MUFA, PUFA, n-3 and n-6 fatty acids, docosahexaenoic acid (DHA), α-tocopherol-cholesterol ratio and magnesium. Sarcopenia was more frequent among those with lower levels of leucine, BCAA, EAA, EPA, 25(OH)D and higher levels of homocysteine (P<0.05). Age and BMI were identified as relevant covariates. A robust association was only found for lower gait speed and lower 25(OH)D levels.
Conclusion
Compromised muscle parameters are associated with low blood values of specific amino acids, fatty acids, vitamin D and high homocysteine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With age, muscle mass, strength and function decline (1-3). This age-related low muscle mass and function is defined as sarcopenia, and may result in adverse health outcomes, such as, mobility disability and subsequent loss of independence (4). As the world population is aging (5), there is a need for strategies that prevent or delay the onset and progression of sarcopenia (6) and support active aging.
Inadequate nutrition is seen as an important contributor to the aetiology of sarcopenia and several nutritional guidelines have been published in recent years on the management of sarcopenia. The SCWD expert group and the PROT-AGE study group recommend sufficient dietary intake of vitamin D and adequate amounts of protein, rich in essential amino acids (EAA) and leucine (7, 8). Recently, we published data on the difference between sarcopenic and non-sarcopenic older adults in their nutrient intake and biochemical nutrient status (9, 10). Data from the Health, Aging, and Body Composition Study indicated that older adults consuming lower amounts of dietary protein lose more lean mass, compared to those consuming higher amounts (11), and were at greater risk of developing mobility limitations (12). A lower intake of the amino acid leucine was found to be associated with lean body mass loss, whereas those with a high intake experienced lean body mass maintenance over a 6-year period (13). This association was only observed for adults > 65 years of age (13). In addition to dietary intake of protein and leucine, vitamin D and nutrients such as omega-3 fatty acid, antioxidants and B-vitamins were also found to be associated with muscle parameters (14, 15).
Although previous studies have indicated associations between dietary nutrient intake and muscle mass and function (11-13), few studies have explored the biochemical nutrient status. Examples are the observed association between vitamin D deficiency and an increase in functional limitations, and plasma fatty acid and muscle performance in community-dwelling older adults (16, 17). With age, certain changes in nutrient absorption and metabolism occur. Examples of these changes are an increased splanchnic extraction of protein and a diminished metabolic response to ingested protein (8, 18). Another example is the less efficient formation of vitamin D3 in the skin of older adults (19), and a reduced sun exposure in this population (20). To better understand the association between nutrient intake and muscle, it is therefore of importance to study not only dietary intake, but also markers of the biochemical nutrient status. Combining these nutrient status markers may help to strengthen the predictability of biological markers to detect sarcopenia.
The present study investigated the association between biochemical nutrient status markers and muscle parameters in community-dwelling older adults. In addition, the association between the nutrient status markers and the presence of sarcopenia was explored. In contrast to previous studies, the current study analysed a range of amino acids and fatty acids, as well as 25-hydroxyvitamin D (25(OH)D), α-tocopherol, homocysteine and magnesium. These post-hoc analyses were performed with data from the cross-sectional Maastricht Sarcopenia study (MaSS) (21).
Material and methods
Data were used from the MaSS study in older adults that was designed to identify the characteristics, prevalence and consequences of sarcopenia (21). For details on the study design (clinicaltrials.gov #NCT01820988) see the original publication by Mijnarends et al. (21). MaSS was performed among community dwelling adults aged ≥65 years, in the Maastricht area in The Netherlands. Participants were found eligible when living at home or living in assisted/residential living facilities, understood the Dutch language, had a Mini-Mental State Examination score of ≥24, and were not wheelchair bound or bedridden. Participants were recruited in the period of May 2013-March 2014 and assessments took place during a 1–2 hour home visit. Informed consent was obtained from all participants before the study visit and ethics approval was obtained from the Medical Ethics Committee of the Academic Hospital Maastricht and Maastricht University, Maastricht, The Netherlands.
Muscle parameters and sarcopenia
Muscle mass was measured with bio-electrical impedance (Aker BIA 50 kHz; Akern Srl, Florence, Italy). Skeletal muscle mass (SMM) was calculated based on the Janssen equation (22) and used to calculate the skeletal muscle index (SMI = SMM / height (in m2)). Handgrip strength was assessed with a handheld Jamar dynamometer (Sammons Preston, Inc, Warrenville, IL). For muscle function the four meter gait speed and the five times chair stand were used.
Sarcopenia was defined following the algorithm of the European Working Group on Sarcopenia in Older People (EWGSOP) (6), including low muscle mass and poor grip strength and/or slow gait speed. Muscle mass was defined as low when SMI ≤6.75 kg/m2 in women and ≤10.75 kg/m2 in men (23). Muscle strength was poor if <20 kg or <30 kg for women and men respectively (24). Gait speed was defined as slow when ≤0.8 m/s (24, 25).
Biochemical markers of nutrient status
Blood samples were obtained after an overnight fast, centrifuged and aliquots were stored at -80°C until analysis. For the analysis of serum amino acids, first proteins and large peptides were precipitated with perchloric acid. After filtration, the amount of the free amino acids in the supernatant was determined by ultra-fast liquid chromatography (Shimadzu Benelux BV, Den Bosch) using a pre-column derivatization with o-phtaldialdehyde and fluorimetry as detection (26). Serum 25(OH)D was analysed with the chemiluminescence IDS-iSYS 25-Hydroxy Vitamin Ds assay (Immunodiagnostic Systems Ltd, Boldon, England). Serum α-tocopherol was analysed with ultra-fast liquid chromatography (Shimadzu Benelux,’ s-Hertogenbosch, The Netherlands) and corrected for cholesterol. Cholesterol was analysed with the colorimetric method Cholesterol Gen.2 (COBAS, Roche Diagnostics GmbH). Serum magnesium was assessed photometrically with Magnesium Gen.2 (COBAS, Roche Diagnostics GmbH, Mannheim, Germany). Blood for the homocysteine analysis was collected in S-Monovette® HCY/Z-gel tubes (Sarstedt, Nümbrecht, Germany) and plasma levels were analysed with a Quattro Premier tandem mass spectrometer (Waters Chromatography B.V., Etten-Leur, The Netherlands). The red blood cell (RBC) phospholipid profile was assessed with gas chromatography (Shimadzu Benelux,’ s-Hertogenbosch, The Netherlands), and expressed as a percentage of the total fatty acids.
Calculations
The following sum scores were calculated for amino acids: branched chain amino acids (BCAA: isoleucine, leucine and valine), EAA (histidine, threonine, valine, methionine, tryptophan, phenylalanine, isoleucine, leucine, lysine), proteinogenic total amino acids (TAA: alanine, arginine, asparagine, aspartic acid, cysteine, glutamic acid, glutamine, glycine, histidine, isoleucine, leucine, lysine, methionine, phenylalanine, proline, serine, threonine, tryptophan, tyrosine, valine). For fatty acids, the following sum scores were calculated: mono-unsaturated fatty acids (MUFA: 16:1n-7, 18:1n-9, 18:1n-7, 20:1n-9, 22:1n-9, 24:1n-9), poly-unsaturated fatty acids (PUFA: 18:2n-6, 18:3n-6, 20:2n-6, 20:3n-6, 20:4n-6, 22:4n-6, 22:5n-6, 24:2n-6, 18:3n-3, 18:4n-3, 20:3n-3, 20:5n- 3, 22:3n-3, 22:5n-3, 22:6n-3, 20:3n-9), saturated fatty acids (SFA: 8:0, 10:0, 12:0, 14:0, 15:0, 16:0, 17:0, 18:0, 20:0, 22:0, 23:0, 24:0), n-3 fatty acids (18:2n-3, 18:4n-3, 20:3n-3, 20:5n-3 (EPA), 22:3n-3, 22:5n-3 (docosahexaenoic acid, DHA), 22:6n- 3) and n-6 fatty acids (18:2n-6, 18:3n-6, 20:2n-6, 20:3n-6, 20:4n-6, 22:4n-6, 22:5n-6, 24:2n-6).
Statistical analyses
The nutrient status marker levels were divided into quartiles, and difference between quartiles for muscle parameters were compared with generalized linear modelling and post-hoc Tukey’s test. Visual inspection of the residuals was used to determine whether the models deviated from a normal distribution. Chair stand was found to deviate from a normal distribution and was therefore log-transformed for analysis. As covariates: sex, age, BMI, the number of comorbidities and the number of medicines were included, as these may affect the nutrient status markers and hence their relation with the muscle parameters and sarcopenia (27-29). The analyses were performed in three steps: first the simple model was run without the inclusions of covariates, secondly the main model was run including the 5 covariates. If the covariate had a P<0.05, first order interaction was explored in a third analysis step. First order interaction was defined as P<0.10. Binary logistic regression was used to examine the associations between the nutrient status markers and the presence of sarcopenia. The nutrient status markers were analysed as continuous variables and the same 3-step approach as described above for the covariates was applied.
Results were considered statistical significant when the P value was below 0.05, and stated as medians (95% confidence interval) or as means (standard deviations). Analyses were performed in IBM SPSS Statistics Version 19.0.0 (IBM SPSS Inc.).
Results
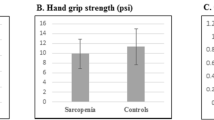
In total, 227 participants were included in the MaSS study. The median age of the MaSS population was 74 (66-89) years within the age range of 65–95 years. About half of the population was female (117, 52%). The median BMI and SMI were 27 (21-33) kg/m2 and 8.3 (5.9-10.8) kg/m2 respectively. The median number of comorbidities and medicines used was 2 (0-5) and 4 (0-11) respectively. The median handgrip strength was 25 (11-42) kg, the mean gait speed was 1.0 (0.5-1.4) m/s and the mean five times chair stand was 12 (9-22) s. For more details on the participant descriptives, see ter Borg et al. (10).
Quartiles one till four of the nutrient status markers are stated in table 1. Participants in the lowest quartile of leucine, BCAA, EAA had a lower SMI (P<0.001) and lower handgrip strength (P<0.001) and needed more time to complete the chair stand test (P<0.05), compared to those with higher levels (see table 1). In addition, a significant difference was observed in gait speed between the quartiles of EAA (P=0.028). No significant differences were observed for TAA.
No significant differences were observed between the quartiles of SFA, MUFA, PUFA, n-3, n-6 fatty acids and DHA. Participants in the lowest quartile of EPA had a lower gait speed (P=0.043) and needed more time to complete the chair stand test (P=0.041), compared to those in the higher quartiles of EPA.
Participants in the lower quartiles of 25(OH)D had a lower gait speed (P<0.001) and handgrip strength (P=0.002) compared to those in the higher quartiles. No significant difference was observed between quartiles of α-tocopherolcholesterol ratio. Participants in the higher homocysteine quartiles had higher SMI (P=0.001), lower gait speed (P=0.001) and needed more time to complete their chair stand test (P=0.049), than those in the lower quartiles of homocysteine. Those in the lowest quartile of magnesium had a lower gait speed (P=0.013) than those in the higher quartiles.
After adjustment for the potential covariates age, BMI, sex, number of comorbidities and the number of medicines, only the observed significant differences in gait speed between the quartiles of 25(OH)D remained significant (P=0.002). No first order interactions were observed for this association. The other significant differences were no longer statistically significant after adjustment for the covariates.
The binary logistic regression analysis indicated that those with lower levels of leucine were at higher odds of being sarcopenic (P<0.05) (see table 2). Similar results were observed for BCAA, EAA, EPA and 25(OH)D (P<0.05). Participants with lower homocysteine levels had lower odds of being sarcopenic (P<0.05). No significant associations were found for TAA, SFA, MUFA, PUFA, n-3 and n-6 fatty acids, DHA, α-tocopherol-cholesterol ratio and magnesium. When adjusted for the covariates, the observed associations were no longer significant. BMI and age were identified as significant covariates within the models.
Discussion
To our knowledge, this is the first study in which multiple biochemical nutrient status markers were explored with regards to their relation to muscle parameters and sarcopenia. Leucine, BCAA and EAA as well as magnesium, homocysteine and 25(OH)D were found to be associated with muscle parameters. EPA was the only fatty acid, which showed associations with muscle parameters. No association was observed for α-tocopherol. Those with lower levels of leucine, BCAA, EAA, EPA and 25(OHD) were more frequently sarcopenic, whereas those with lower levels of homocysteine were less frequently sarcopenic. After adjustment for the potential covariates, a robust association was only found between gait speed and quartiles of 25(OH)D.
Our observations on serum leucine and TAA are in line with a recent study on dietary amino acid intake (13). Among older adults, there was a significant difference in lean body mass between quartiles of dietary leucine intake while no significant differences were observed for TAA (13). Our study also identified muscle parameter differences between quartiles of serum EAA. Unfortunately, we could not determine the leucine and EAA dietary intake in our study. As leucine and EAA are anabolic amino acids (30), and dietary protein EAA reflect protein quality (31), these results may indicate that dietary protein quality is important for muscle health and the prevention of sarcopenia. This is in line with published recommendations (8, 32). Although amino acid levels can reflect long term dietary intake (33), the question is to what extent serum leucine and EAA levels are influenced by other non-dietary factors such as insulin. As an example, a strong association between blood levels of specifically BCAA and the incidence, progression and remission of insulin resistance, type 2 diabetes, and cardiovascular disease is described (34, 35). But, although diabetes was present in 11.5% of the MaSS population (21), this does not explain the association observed for EAA. Blood levels of amino acids are in general in steadystate and are the result of a balance between rate of appearance (Ra) and rate of disappearance (Rd). Hypoaminoacidemia can be the result of a decrease in Ra due to low protein intake or a decrease in mobilization of amino acid stores, which is typical for states of chronic (protein) undernutrition and mainly concerns EAA (36). To better understand the underlying mechanism of our observation, it is of interest to study the effects of sarcopenia and aging on muscle protein turnover.
The present study indicates an association between blood RBC phospholipid levels of EPA and muscle function (chair stand and gait speed). These results are in line with previous studies indicating less physical function decline over time in those with higher EPA levels (37). Although the present study did not detect a significant association between SFA and muscle parameters, the InChianti study (37) found a significant negative association for SFA and the 7m walk and physical function. This may indicate that not only EPA, but also other fatty acids and hence dietary fat quality could play a role in muscle function.
In the MaSS population, lower vitamin D status was found to be associated with lower gait speed, strength and the presence of sarcopenia. For gait speed, quartile one (≤41 nmol/l), significantly differed from the other quartiles (>41 nmol/l). Quartile one corresponds to the cut-off value of inadequacy of 50nmol/l (38). Previous studies have also identified the association between vitamin D inadequacy and muscle function (39, 40).
The MaSS study results indicate negative associations between homocysteine status and muscle function and sarcopenia. Earlier studies also identified a negative association between homocysteine and muscle function (41, 42). Homocysteine was included as an indirect nutrient status marker for the B-vitamins. However, homocysteine itself may also induce muscle protein damage and reduces blood flow through an increase in oxidative stress (43).
A difference between quartiles of magnesium was observed for gait speed in our study, but no association was found with the other muscle parameters and with sarcopenia. A possible explanation could be that magnesium is not a suitable nutrient status marker. This is because magnesium metabolism is strictly regulated, and only one percent of the overall magnesium is present in the blood (29).
As MaSS is a cross-sectional study, additional studies are needed to identify the causality of the observed associations. In addition, because of the observational nature of MaSS it is unclear which mechanisms are involved in the associations between nutrients and (the parameters of) sarcopenia. As sarcopenia is a multifactorial syndrome it can be argued that other aspects such as age and comorbidities contribute to the observed associations. To test the robustness of the results a covariate analysis was included. Since sarcopenia is the agerelated loss of muscle mass, strength and function, it was not surprising to find that age is a strong contributor to the models. BMI was also an important covariate, and sarcopenic obese older adults may have their own specific nutrient needs. The MaSS population was unfortunately too small to explore age and BMI subgroups. Future cohort studies may, therefore, want to consider matching participants for age and BMI or explore these subgroups of the sarcopenic population.
Although we observed associations between several nutrient status markers and the presence of sarcopenia, it is unlikely that a single marker or specific cut-off level can serve as a predictive biomarker. As sarcopenia is a multifactorial geriatric syndrome and is also influenced by non-nutritional factors (6), it is advised to combine nutrient status markers with other relevant markers to predict sarcopenia. Another implication of these results is that nutritional interventions may best be designed to include multiple nutrients. The present data indicates that those subjects in a lower quartile of one status marker were also frequently low in other status markers, e.g. EPA and leucine shows a significant correlation (r=0.229; P=0.001). This suggests that not a single nutrient, but a combination of nutrients (diet quality), is of importance for sarcopenia.
In combination with previous observational studies on nutrient intake, the present study helps to better understand the relation between nutrients and sarcopenia that may contribute to the development of an optimal intervention strategy.
Conclusion
Low blood levels of EAA, BCAA and leucine are associated with lower muscle mass, strength and function in older adults, whereas no association was found for TAA. Lower blood levels of EPA, 25(OH)D and homocysteine were found to be associated with lower muscle parameters. A robust association was only found for gait speed and 25(OH)D. Lower levels of leucine, BCAA, EAA, EPA, 25(OH)D and higher levels of homocysteine were associated with sarcopenia. Age and BMI were identified as significant covariates in the observed associations and should be taken into account in the design of future studies. The results of the present study show that muscle parameters are associated with blood values of specific amino acids, fatty acids, vitamin D and homocysteine. Although further investigation on the cause-effect relationship is required, this research suggests that diet quality, i.e. quality of the protein and fat source and adequate micronutrients, may be relevant for muscle health and in the prevention of sarcopenia.
Acknowledgements: We would like to thank those involved in the MaSS and the subsequent analyses, in particular Donja Mijnarends, for their dedicated work on the MaSS study. In addition, we would like to thank Egbert Biesheuvel and Elleny Balder for their support in the statistical analyses.
Financial Support: This study was financially supported by Danone Nutricia Research, Nutricia Advanced Medical Nutrition.
Conflict of Interest: StB was employed by Danone Nutricia Research at the time of the study. AvH and YL are employees of Danone Nutricia Research. YB, JS, LdG have no conflicts of interest to declare.
Authorship: The author’s contribution is as follows: StB drafted the manuscript. StB, YL, AvH, YB, JS, LdG. were involved in the study design and data interpretation. All authors critically reviewed the manuscript.
Ethical standards: The Medical Ethics Committee of the Academic Hospital Maastrichtand Maastricht University approved the MaSS study. The MaSS study was registered at www.clinicaltrials.gov (NCT01820988).
References
Koopman R, van Loon LJ. Aging, exercise, and muscle protein metabolism. Journal of applied physiology 2009;106: 2040–2048
Short KR, Nair KS. Mechanisms of sarcopenia of aging. Journal of endocrinological investigation 1999;22: 95–105
Lindle RS, Metter EJ, Lynch NA et al. Age and gender comparisons of muscle strength in 654 women and men aged 20–93 yr. Journal of applied physiology 1997;83: 1581–1587
Landi F, Calvani R, Cesari M et al. Sarcopenia: an overview on current definitions, diagnosis and treatment. Curr Protein Pept Sci, 2017
United Nations. Department of Economic and Social Affairs. Population Division Worlds Population Ageing: 1950–2050. https://doi.org/www.un.org/esa/population/publications/worldageing19502050/, accessed 16–07–2017.
Cruz–Jentoft AJ, Baeyens JP, Bauer JM et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age and ageing 2010;39: 412–423
Morley JE, Argiles JM, Evans WJ et al. Nutritional recommendations for the management of sarcopenia. Journal of the American Medical Directors Association 2010;11: 391–396
Bauer J, Biolo G, Cederholm T et al. Evidence–based recommendations for optimal dietary protein intake in older people: a position paper from the PROT–AGE Study Group. Journal of the American Medical Directors Association 2013;14: 542–559
Verlaan S, Aspray TJ, Bauer JM et al. Nutritional status, body composition, and quality of life in community–dwelling sarcopenic and non–sarcopenic older adults: A case–control study. Clin Nutr 2017;36: 267–274
Ten Borg S, de Groot LC, Mijnarends DM et al. Differences in Nutrient Intake and Biochemical Nutrient Status Between Sarcopenic and Nonsarcopenic Older Adults–Results From the Maastricht Sarcopenia Study. Journal of the American Medical Directors Association 2016;17: 393–401
Houston DK, Nicklas BJ, Ding J et al. Dietary protein intake is associated with lean mass change in older, community–dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr 2008;87: 150–155
Houston DK, Tooze JA, Garcia K et al. Protein Intake and Mobility Limitation in Community–Dwelling Older Adults: the Health ABC Study. J Am Geriatr Soc 2017;65: 1705–1711
McDonald CK, Ankarfeldt MZ, Capra S et al. Lean body mass change over 6 years is associated with dietary leucine intake in an older Danish population. The British journal of nutrition 2016;115: 1556–1562
Mithal A, Bonjour JP, Boonen S et al. Impact of nutrition on muscle mass, strength, and performance in older adults. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 2013;24: 1555–1566
Robinson S, Cooper C, Aihie Sayer A. Nutrition and sarcopenia: a review of the evidence and implications for preventive strategies. Journal of aging research 2012;2012: 510801
Sohl E, van Schoor NM, de Jongh RT et al. Vitamin D status is associated with functional limitations and functional decline in older individuals. The Journal of clinical endocrinology and metabolism 2013;98: E1483–1490
Frison E, Boirie Y, Peuchant E et al. Plasma fatty acid biomarkers are associated with gait speed in community–dwelling older adults: The Three–City–Bordeaux study. Clin Nutr 2017;36: 416–422
Boirie Y. Fighting sarcopenia in older frail subjects: protein fuel for strength, exercise for mass. Journal of the American Medical Directors Association 2013;14: 140–143
Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocrine reviews 2001;22: 477–501
Brouwer–Brolsma EM, Vaes AM, van de Zwaluw NL et al. Relative importance of summer sun exposure, vitamin D intake, and genes to vitamin D status in Dutch older adults: The B–PROOF study. The Journal of steroid biochemistry and molecular biology 2016;164: 168–176
Mijnarends DM, Schols JM, Meijers JM et al. Instruments to assess sarcopenia and physical frailty in older people living in a community (care) setting: similarities and discrepancies. Journal of the American Medical Directors Association 2015;16: 301–308
Janssen I, Heymsfield SB, Baumgartner RN et al. Estimation of skeletal muscle mass by bioelectrical impedance analysis. Journal of applied physiology 2000;89: 465–471
Janssen I, Baumgartner RN, Ross R et al. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. American journal of epidemiology 2004;159: 413–421
Lauretani F, Russo CR, Bandinelli S et al. Age–associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. Journal of applied physiology 2003;95: 1851–1860
Guralnik JM, Simonsick EM, Ferrucci L et al. A short physical performance battery assessing lower extremity function: association with self–reported disability and prediction of mortality and nursing home admission. Journal of gerontology 1994;49: M85–94
Terrlink T, van Leeuwen PA, Houdijk A. Plasma amino acids determined by liquid chromatography within 17 minutes. Clin Chem 1994;40: 245–249
Olia Araghi S, van Dijk SC, Ham AC et al. BMI and Body Fat Mass Is Inversely Associated with Vitamin D Levels in Older Individuals. The journal of nutrition, health & aging 2015;19: 980–985
Sohl E, de Jongh RT, Swart KM et al. The association between vitamin D status and parameters for bone density and quality is modified by body mass index. Calcified tissue international 2015;96: 113–122
Elin RJ. Magnesium metabolism in health and disease. Disease–a–month: DM 1988;34: 161–218
Katsanos CS, Kobayashi H, Sheffield–Moore M et al. A high proportion of leucine is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. Am J Physiol Endocrinol Metab 2006;291: E381–387
World Health Organization. Food and Agriculture Organization of the United Nations. United Nations University, 2007. Protein and amino acid requirements in human nutrition. Report of a joint FAO/WHO/UNU expert consultation (WHO Technical Report Series 935). World Health Organization.
Paddon–Jones D, Rasmussen BB. Dietary protein recommendations and the prevention of sarcopenia. Curr Opin Clin Nutr Metab Care 2009;12: 86–90
Schmidt JA, Rinaldi S, Scalbert A et al. Plasma concentrations and intakes of amino acids in male meat–eaters, fish–eaters, vegetarians and vegans: a cross–sectional analysis in the EPIC–Oxford cohort. European journal of clinical nutrition 2016;70: 306–312
Newgard CB, An J, Bain JR et al. A branched–chain amino acid–related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab 2009;9: 311–326
Shah SH, Svetkey LP, Newgard CB. Branching out for detection of type 2 diabetes. Cell Metab 2011;13: 491–492
Darmann and Cynober. Chapter 3: Approaches to study amino acid metabolism: from quantitative assays to flux assessment using stable isotopes. In: [Luc A Cynober, (ed)]] Metabolic and therapeutic aspects of amino acids in clinical nutrition, 2nd edition ed. CRC Press LLC, Washington DC, 2004
Abbatecola AM, Cherubini A, Guralnik JM et al. Plasma polyunsaturated fatty acids and age–related physical performance decline. Rejuvenation Res 2009;12: 25–32
Ross AC, Manson JE, Abrams SA et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. The Journal of clinical endocrinology and metabolism 2011;96: 53–58
Wicherts IS, van Schoor NM, Boeke AJ et al. Vitamin D status predicts physical performance and its decline in older persons. The Journal of clinical endocrinology and metabolism 2007;92: 2058–2065
Tieland M, Brouwer E, Nienaber–Rousseau C et al. Compromised vitamin D status in frail elderly people is associated with reduced muscle mass and physical performance in “Dietary strategies to augment muscle mass in the elderly”. Dissertation, Wageningen University, 2013.
Kado DM, Bucur A, Selhub J et al. Homocysteine levels and decline in physical function: MacArthur Studies of Successful Aging. The American journal of medicine 2002;113: 537–542
Swart KM, van Schoor NM, Heymans MW et al. Elevated homocysteine levels are associated with low muscle strength and functional limitations in older persons. The journal of nutrition, health & aging 2013;17: 578–584
Weiss N, Keller C, Hoffmann U et al. Endothelial dysfunction and atherothrombosis in mild hyperhomocysteinemia. Vascular medicine 2002;7: 227–239
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
ter Borg, S., Luiking, Y.C., van Helvoort, A. et al. Low Levels of Branched Chain Amino Acids, Eicosapentaenoic Acid and Micronutrients are Associated with Low Muscle Mass, Strength and Function in Community-Dwelling Older Adults. J Nutr Health Aging 23, 27–34 (2019). https://doi.org/10.1007/s12603-018-1108-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-018-1108-3