Abstract
Background
Abdominal obesity is related to the disability process in older adults, however, little is known about this relationship when adjusted for important confounders such as depression and physical performance measures in a diverse international aged population.
Objectives
To explore the longitudinal relationship between abdominal obesity and mobility disability controlling for physical performance and depression.
Design and Setting
Longitudinal observational study using data from the International Mobility in Aging Study (IMIAS) Study.
Participants
1104 out of 2002 older adults aged 64–74 years old free of mobility disability at baseline (2012) and then reassessed in 2016.
Measurements
Mobility disability was defined as reporting difficulty in walking 400 m or climbing stairs. Activities of daily living (ADL) disability was based on any self-reported difficulty in five mobility-related ADLs. Abdominal obesity was defined as waist circumference ≥ 88cm for women or ≥ 102 cm for men. Four meters gait speed, handgrip strength and depressive symptoms (CES-D) were assessed. Generalized Estimating Equations (GEE) and multinomial regressions were used to estimate associations between disability and abdominal obesity.
Results
1104 free of disability participants were followed over 4 years, the mean age was 68.9 (±2.9) years among men and 68.7 (±2.6) years among women. Prevalence and incidence rates of mobility disability varied widely across research site and sex. The longitudinal associations between mobility disability and abdominal obesity remained significant even when adjusted by depressive symptoms, handgrip strength, gait speed, age, sex, education and research site. Participants with abdominal obesity had higher mobility disability (OR=1.68, 95% CI 1.23-1.76, p-value=0.01) and also increased risk for ADL disability (OR: 1.47, 95% CI 1.23-1.76, p-value=0.01). Abdominal obesity in baseline was also predictor of mobility disability in 2016 (OR: 1.93, 95% CI 1.17-3.17, p-value <0.01) but not for ADL disability (OR: 1.59, 95% CI 0.93-2.71, p-value =0.09) with accounting mortality.
Conclusion
Abdominal obesity is associated longitudinally and predicts mobility disability, even over a short period (4 years) in community-dwelling older adults from different epidemiological contexts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disability in old age is a major public health concern due to global population aging (1). The current literature provide that higher disability rates among older people reflect an accumulation of health risks across a lifespan of disease, injury, chronic illness, environmental risk, and social and economic adversity (2). Thus, studies that compare populations of older adults with diversity in terms of demographic, economics, social and cultural characteristics, could be helpful to improve the knowledge about disability in the ageing process.
In older adults, important risk factors for disability are depression (3–6), declines in gait speed and muscle strength (7, 8), and obesity (9, 10). Obesity is a contemporary public health problem receiving increasing attention in older adult populations due to its associations with increased risk for comorbidities, cardiovascular disease and earlier death (9). The presence of obesity is linked to an increased risk for disability in older adults (9). In a systematic review, Vincent et al. (2010) reported that obesity was a consistent predictor of mobility disability in the older population (10).
Waist circumference has emerged as a possible better measure of obesity than BMI in older adults since it is strongly related to visceral fatness, while BMI is considered an inadequate measure particularly in aged subjects due do not reflect the age related changes in body composition (11). Some longitudinal studies have recently shown the predictive value of abdominal obesity (AO) for disability in older adults (12–14). Additionally, the literature from longitudinal studies also demonstrates the strong negative impact of depression on disability health status of older adults’ life (3, 4) and its relationship with obesity (15–18). Similarly, physical performance measures (such as gait speed and handgrip strength) are longitudinally associated with both obesity (19, 20) and disability (8, 21–23).
As far as we are aware, there are no longitudinal studies that have focused on the relationship between disability and abdominal obesity adjusting for depression and physical performance, which are considered important confounders of this association (16, 17, 21, 24). For this study, we hypothesized that the disablement process is influenced by abdominal obesity in its development, even in the presence of other important known risk factors. Moreover, we used data from the International Mobility Aging Study (IMIAS), a multicentre cohort study that provided a good opportunity to study this relationship in older adults aging in different contexts and with very distinct aging profiles. Thus, the current study had two objectives: (a) to estimate the prevalence and 4-year incidence of mobility and mobility-related Activities of Daily Living (ADL) disability in men and women participants in the IMIAS study; and (b) to explore the longitudinal relationship between abdominal obesity with mobility and mobility-related ADL disability controlling for physical performance and depression in older adults who are free from disability.
Methods
Study design and participants
IMIAS is a population-based longitudinal study that involved five sites with different epidemiological contexts: Kingston (Ontario, Canada) and Saint-Hyacinthe (Quebec, Canada), Tirana (Albania), Manizales (Colombia) and Natal (Brazil). IMIAS’ main purpose was understanding the differences in mobility disability among older adults from diverse settings, that differed in social, cultural, socioeconomics aspects and of health care systems (25). For instance, these countries had different demographic aging with percentage population over 65 years ranging from 7 in Colombia to 16 in Canada, also show disparities in term of gender inequalities, where Canada have a better position in Gender Inequality Index Rank (18) than their counterparts from Albania (51), Colombia (89) and Brazil (92) (25). The study design and data collection methods have been described earlier (25, 26).
IMIAS participants were community-dwelling men and women aged 64–74 years old at the time of the first assessment wave. Older adults from Tirana, Manizales, and Natal were randomly recruited through neighborhood primary care centers. Canadian participants were invited to participate in the study by an invitation letter from their primary care physicians (26). Briefly, only older adults without severe cognitive decline were included (defined as four or more errors in the orientation scale of the Leganes Cognitive Test) (25, 27).The assessments were performed by health professionals in Latin America cities and Tirana, and by teachers and other lay professionals in Canada (25).
In 2012, 2002 participants were recruited and followed for four years, with reassessments in 2014 and 2016. In 2016, 1527 of the 1891 subjects known to have not died participated in the follow-up assessment (81%). For this data analysis, we included only participants without any disability at baseline (n=1104).
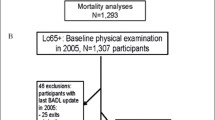
Figure 1 describes the sampling strategy of this study.
Measurements
Disability Status
Disability status was defined by self-reported difficulties in mobility tasks and also in difficulties in performing ADL related to mobility following definitions used by Guralnik et al. (1995) (28). Mobility disability was defined as self-reported difficulty in walking 400 m or climbing a flight of stairs without resting (26, 29, 30); ADL disability was defined by reporting difficulties in performing at least one of five mobility-related activities of daily living (ADL): going to the bathroom, bathing, dressing, getting out of bed, walking across a small room (26, 30, 31). Furhtermore, we used a three-level hierarchical variable for disability status definition as follows: complete function (those individuals without disability); mobility disability (have difficulty walking 400 m or climbing a flight of stairs); and mobility-related ADL disability (including those with mobility disability plus difficulty to perform one or more mobilityrelated ADL) (31, 32).
Abdominal obesity
Waist circumference (cm) was assessed using a non-elastic tape at the midpoint between the lower edge of the rib cage and the iliac crest. Abdominal obesity was considered when waist circumference was ≥ 88cm for women or ≥ 102 cm for men (33, 34).
Covariates
Physical performance
For gait speed assessment the participant was requested to walk at their usual-pace in a distance of four meters, or three meters if four meters of space was unavailable in the home (31). The gait speed was defined by the distance (in meters) divided by time (in seconds). Two measurements were performed and the fastest value was used for analysis. Handgrip strength was measured using a handheld dynamometer (Jamar Hydraulic Hand Dynamometer®). Participants were instructed by the interviewer and verbally encouraged to grip the handle as hard as possible using their dominant hand. The measurement protocol for handgrip strength followed the recommendations of The American Society of Hand Therapists (35). Three measurements were performed, and the highest value was used in the analyses.
Depressive symptoms
Depressive symptoms were reported as the score on the Center for Epidemiologic Studies Depression Scale (CESD), which is a widely used 20-item test with scores from 0 to 60 (highest possible burden of depressive symptomatology). Scores ≥ 16 were used as indicative of clinically relevant depression (36).
Sociodemographic information obtained at baseline during the structured interview included age, sex, education (years) and income sufficiency. Income sufficiency was recorded by the answer to the question: To what extent is your income sufficient to make ends meet? Possible responses were: very sufficient, suitable, and insufficient (37). Chronic conditions were assessed as self-report of having been diagnosed by a medical doctor with any of the following conditions: hypertension, heart diseases, diabetes, cancer, chronic respiratory disease, arthritis or osteoporosis. As an indicator of comorbidity, we used the sum of all chronic conditions and then we categorized in 0–1, 2–3 and 4 or more chronic conditions (38, 39). Height (cm) was measured to the nearest 0.1 cm with a stadiometer. Body weight (kg) was assessed using a digital scale with participants wearing light indoor clothes and no shoes. Body mass index was calculated using weight and height2 (kg/m2). Finally, physical activity was self-reported using total walking time per week obtained from the Mobility Assessment tool for Walking (MAT-W) (40). Smoking was classified into three categories: never smoked, ex-smoker and smoker.
Statistical analysis
Descriptive statistics were used to summarize the data. Continuous variables were presented by mean values and standard deviations, while categorical variables were presented by proportions. Sex-specific results are shown according to disability status only for descriptive purposes. Differences between mobility disability, ADL disability, and complete function groups were compared using ANOVA and Chi-square test. The incidence of mobility and ADL disability in 2014 were calculated considering the participants who were free of disability at baseline. 2016 disability incidence was only considered for those participants without disability (mobility and ADL) in 2014.
We used Generalized Estimating Equations (GEE) to model the longitudinal associations between mobility disability and ADL disability with abdominal obesity, adjusting for depressive symptoms and physical performance measures and remaining covariates. GEE is an extension of the generalized linear model that accounts for the within-subject correlation across repeated measurements, allows for within-subject missing data, and is appropriate to estimate population-averaged effects over time. We used an unstructured correlation structure for GEE analysis for which we built two models; one model with mobility disability as the dependent variable, and the other model with mobility-related ADL disability as the dependent variable. Both models were adjusted by the following baseline variables: age, sex, years of education, income sufficiency, research site, number of chronic conditions, and height; and by the following time-varying variables: abdominal obesity, depression, handgrip strength, gait speed and time of follow up (representing the 3 waves of data collection). Sex interactions for abdominal obesity, depressive symptomatology and physical performance measures were tested in both models. Since these interactions were not significant, sex was included as a covariate.
Finally, we performed a multinomial regression to assess the predictive value of baseline abdominal obesity, depressive symptomatology, handgrip strength, and gait speed for 2016 mobility disability. Participants were classified into four categories according to disability in 2016: complete function, mobility disability, mobility-related ADL disability, and death (the distribution of this outcome is shown in Table 1). All analyses were controlled by disability status in 2012, age, sex, education, income sufficiency, research site, number of chronic conditions and height. Sex interactions were also tested using product terms for abdominal obesity, depressive symtptomatology and physical performance measures, however they were non-significant. Comparative analyses between the subjects who remained in the study and those who dropped out of follow-up assessment in 2016 were performed considering socio-demographic factors and variables of interest. No differences in sex, age, abdominal obesity or depression were observed; however, those lost to follow up had lower education.
Results
Sex-specific characteristics according to disability status are shown in Table 2. Disability was more frequent among those with insufficient income, higher comorbidity, those with depression and those with abdominal obesity. Both men and women with mobility disability in 2012 had fewer years of schooling, handgrip strength, and gait speed values. Moreover, both men and women who had ADL disability showed significant lower baseline values in gait speed and handgrip strength compared to those participants without disabilities.
Sex-specific baseline prevalence, two years and four years incidence of mobility and ADL disability in both sexes and across research sites are shown in Table 3. Generally, participants from Latin American cities and Tirana presented more disability rates than Canadian participants. Among men, the baseline prevalence of mobility disability varied from 12.1% to 38.3%, and from 10.9% to 27.8% for ADL disability among research sites. At baseline, prevalence rates were higher in women than men for both mobility, ranging from 21.7% to 66.0% and 20.4% to 43.9% for ADL disability. Similar patterns of women presenting higher values of disability incidence were observed in 2014 and 2016 (Table 3).
The longitudinal association between mobility disability and obesity is shown in Table 4. The generalized estimation equation model showed that the association between mobility disability and abdominal obesity remained statistically significant even after adjustment by depressive symptoms, handgrip strength and gait speed. Those participants with abdominal obesity had an odds ratio of 1.68 (95% CI 1. 23–1.76) for developing mobility disability in 4 years compared to the reference group without abdominal obesity. Stronger associations were also found with depressive symptomatology (OR: 1.93, 95% CI 1.82–2.63), while higher values in the physical performance measures were protective factors for mobility disability (Table 4).
In the fully adjusted model, we found higher odds of ADL disability among those with abdominal obesitye (OR: 1.47, CI 95% 1.23–1.76). Again, we observed a strong longitudinal association between depressive symptoms and ADL disability (OR: 2.19, CI 95% 1.89–2.63). Higher values of handgrip strength and gait speed were associated with lower risk of ADL disability (Table 4).
In our analyses of baseline predictors for 2016 disability controlling for mortality, abdominal obesity (OR: 1.93; CI 95% 1.17–3.17) was a predictor of mobility disability in 2016, also gait speed (OR: 0.34; CI 95% 0.10–1.07) and handgrip strength (OR: 0.95; CI 95% 0.92–0.99) were protective factors for mobility disability (Table 5). Nevertheless, abdominal obesity was not a predictor of ADL disability (OR: 1.59; CI 95% 0.93–2.71) or death (OR: 1.64; CI 95% 0.68-3.92). Also, in relation to death gait speed was protective (OR: 0.11; CI 95% 0.01–0.89).
Discussion
In this study we aimed to describe the prevalence and incidence of mobility and mobility-related ADL disability in an international, multisite study of community-dwelling older adults. Moreover, we also examined the longitudinal relationship between mobility and mobility-related ADL disability with abdominal obesity, controlling for depression and physical performance measures in older adults from different epidemiologic contexts. We observed that the prevalence and incidence of mobility and mobility-related ADL disability varied across research sites and between sexes. In general, higher prevalence and incidence of disability were found in those participants from Latin America and Tirana and among women compared to men. Previous crosssectional analyses based on data from the first wave of the IMIAS showed that women were more likely to report having difficulties in mobility and in performing ADLs (26). Also, the high load of prevalence and incidence of disability in older adults from Latin America has support in previous studies conducted in Latin America (1, 41).
The longitudinal relationship between abdominal obesity and mobility disability remained statistically significant even after controlling for depressive symptomatology, physical performance measures, health behaviors, comorbidity, socioeconomic variables and research site. Those participants with waist circumference higher than 102 cm (men) or 88 cm (women), respectively had a higher risk of mobility disability in 4 years of follow-up (OR 1.47). Similar results were found by Koster et al. (2008) using data from the Health ABC study, in which older adults who had higher values of waist circumference had a higher risk for developing mobility disability after 6.5 years of follow-up (42). Guallar-Castillón et al. (2007) also found that waist circumference was associated with mobility disability after two years of follow-up in older Spanish adults (43). Same pattern was seen abdominal obesity and mobility-related ADL did not reach statistical significance. Corona et al. (2016) found that abdominal obesity was a strong predictor of ADL disability over five years of followup in Brazilian older adults (participants in the SABE study) controlling for handgrip strength, age, sex, education, physical activity level, cognitive function and chronic conditions (14). A prospective study of preretirement age adults from England also found that waist circumference was the best predictor for the risk of developing disability among the five anthropometric measures of obesity after five years, even adjusting for age, height, smoking, social class and education corroborant with our findings (12).
Consistent with results from the GEE models, we found that baseline abdominal obesity was an important predictor of mobility disability development after four years in the multinomial regression model. However, it did not predict more severe disability (ADL disability) and mortality. Perhaps the lack of association was influenced by the relatively small number of incident cases of ADL disability, since our sample is composed of younger older subjects, where this type of disability is uncommon. Furthermore, a previous study showed that obese older adults can use compensatory strategies in order to facilitate the successful completion of physical tasks as older adults who report no signs of difficulty (44). Additionally, this discrepancy may reflect that abdominal obesity could bring greater difficulties experienced in walking intermediate distances compared to the difficulties posed by shorter walking in everyday activities (12). Despite this, Guallar-Castillon et al. (2007) also did not find an association between high quintile of waist circumference and ADL disability in Spanish older adults, which corroborates with our findings (13). Nevertheless, the relationship between central obesity and mortality is still contradicted in older populations (45).
Despite this, the literature does provide explanations for the association between central obesity and disability. The presence of abdominal obesity can be linked to physical inactivity, which in turn could lead to disability (43). Another possibility is that the presence of abdominal obesity could represent a burden for the osteomuscular system, thus limiting mobility (43). Finally, other authors have suggested that the increase in the amount of adipose tissue can be related to an up-regulation of systemic inflammation, thus leading to a disability process (46, 47).
Our analyses found that the presence of depressive symptoms was strongly associated to mobility and mobilityrelated ADL in both sexes and these findings are in line with results from previous studies (3–6). However, the presence of depressive symptoms at baseline did not predict the disability status after 4 years. Absence of predictive power of depression for disability was also seen in other studies (48, 49). Perhaps this lack of prediction could be a side effect of the exclusion of those who were already disabled at baseline; thus, we may have excluded some participants with both disability and depression, and this might have reduced the number of depressed participants, influencing the prediction power 4 years later. We also found that physical performance measures (handgrip strength and gait speed) were longitudinally associated to mobility and mobility-related ADL. Also, these measures showed association with the mobility disability status in 2016. These findings are in line with previous studies (8, 24, 50, 51). Moreover, gait speed was an important protective factor for mortality, which is line with previous studies (52).
Limitations and strengths
This study has some strengths. First, we used waist circumference to measure obesity, which is a better predictor of body fat amount in older adults compared to body mass index (12). In a recent study, Batis et al. (2016) found that diagnostic accuracy of BMI was poor in both sexes with advanced age, and for this population the use of centrally adiposity measures were recommended (53). Furthermore, we used the same standardized assessment protocols over the four years in four international research sites. Additionally, this is the first study to date which examined the relationship between obesity and disability status controlling for important confounders such as physical performance and depression in diverse populations of older adults with distinct ways of living.
Despite this, some limitations should be considered. The study sample was relatively small to do site-specific analyses, with inclusion of quartiles or quintiles distribution for abdominal obesity. However, in bivariate analyses for increased disability risk in the lowest and the highest quintiles of BMI and we did not find significant differences in these extreme categories. Due to our limited sample size, other important confounders could not be included such as life space mobility, social participation or individual’s medical conditions. Also, our outcomes were self-reported, which may be influenced by culture or education (54). However, self-reported measures are considered valid and cost-effective measures of disability assessment in older adult populations (55). Another possible limitation is that our sample is composed of the young-old (aged 65–74 years) added to the short time of follow up, could be related to the small number of incident cases of ADL disability and may result in lack of statistical power to detect the association between abdominal obesity and ADL disability. However, we have verified that in bivariate analyses the associations between abdominal obesity and mobility and ADL disability yielded high statistical power (97% and 93%, respectively).
In this study abdominal obesity was defined according to NIH recommendations (> 88 cm for women and >102 cm for men) (34), despite of previous discussion about ethnic-based cut offs for abdominal obesity to increase the accuracy for screening metabolic and cardiovascular diseases (56, 57), recent finding have been showing that obesity can be also related to socioeconomic disparities than only genetic influence (58). Moreover the cut off adopted in this study was associated to disability in prior studies from diverse countries (14, 23, 59, 60). Finally, in order to avoid overload in statistical analysis comorbidity was used as the sum of eight chronic conditions. Despite of some previous work argued that this approach does not consider the disease severity, using comorbidity in this way we could provide a global measure of the overall impact of disease burden on disability process (38, 39).
Relevant clinical implications
We observed that abdominal obesity has an important role in the development of mobility disability in a short period of time (4 years) in community-dwelling older adults from different epidemiological contexts. The presence of abdominal obesity remained an important risk factor for disability independent of sex, country, or other significant factors, demonstrating that it is urgent to implement health promotion policies to reduce obesity in adult populations in order to prevent mobility disability in later life.
Conclusion
In summary, our results showed that the presence of abdominal obesity has a central role in the mobility disability process. Future intervention studies and health policies are needed to reduce obesity in order to interrupt the progression from functional limitation to disability sooner in older populations.
Conflicts of interest: The authors declare no conflict of interest.
Acknowledgements: This project was funded by the Canadian Institutes of Health Research, Institute of Aging, New Emerging Team; gender differences in immobility; reference number: AAM 108751.
Author Contributions: JFSB, MVZ and ROG contributed through conception and design/analysis and interpretation of data. JVC contributed to the statistical analysis and interpretation of data. TA, CSG, CLC, JFG contributed to interpretation of results and revised the paper. All the authors revised the manuscript critically for the intellectual content and read/approved the final version.
Ethical standard: The Research Ethics Committees at the Universidad de Caldas, Universidade Federal do Rio Grande do Norte, Albanian Institute of Public Health, Queens University and Centre de Recherche du Centre Hospitaliere de l’Université de Montréal approved the study, and written informed consent was obtained from all subjects prior to study participation.
References
World Health Organization., World Bank. World Report on Disability 2011. World Health Organization
Manini T. Development of physical disability in older adults. Curr Aging Sci 2011;4:184–91. doi: 10.2174/1874609811104030184
Chen CMC-M, Mullan J, Su YYY-Y, et al. The Longitudinal Relationship Between Depressive Symptoms and Disability for Older Adults: A Population-Based Study. Journals Gerontol-Ser A Biol Sci Med Sci 2012;67:1059–1067. doi: 10.1093/gerona/gls074
Cronin-Stubbs D, de Leon CF, Beckett L a, et al. Six-year effect of depressive symptoms on the course of physical disability in community-living older adults. Arch Intern Med 2000;160:3074–80. doi: 10.1001/archinte.160.20.3074
Lenze EJ, Schulz R, Martire LM, et al. The Course of Functional Decline in Older People with Persistently Elevated Depressive Symptoms: Longitudinal Findings from the Cardiovascular Health Study. J Am Geriatr Soc 2005;53:569–575. doi: 10.1111/j.1532-5415.2005.53202.x
Van Gool CH, Kempen GIJM, Penninx BWJH, et al. Impact of depression on disablement in late middle aged and older persons: Results from the Longitudinal Aging Study Amsterdam. Soc Sci Med 2005;60:25–36. doi: 10.1016/j.socscimed.2004.04.021
Legrand D, Vaes B, Matheï C, et al. Muscle strength and physical performance as predictors of mortality, hospitalization, and disability in the oldest old. J Am Geriatr Soc 2014;62:1030–8. doi: 10.1111/jgs.12840
Cesari M, Rolland Y, Abellan Van Kan G, et al. Sarcopenia-related parameters and incident disability in older persons: results from the “invecchiare in Chianti” study. J Gerontol A Biol Sci Med Sci 2014;70:457–63. doi: 10.1093/gerona/glu181
Samper-Ternent R, Al Snih S. Obesity in Older Adults: Epidemiology and Implications for Disability and Disease. Rev Clin Gerontol 2012;22:10–34. doi: 10.1017/S0959259811000190
Vincent HK, Vincent KR, Lamb KM. Obesity and mobility disability in the older adult. Obes Rev 2010;11:568–579. doi: 10.1111/j.1467-789X.2009.00703.x
Harris TB, Visser M, Everhart J, et al. Waist circumference and sagittal diameter reflect total body fat better than visceral fat in older men and women. The Health, Aging and Body Composition Study. Ann N Y Acad Sci 2000;904:462–73. doi: 10.1111/j.1749-6632.2000.tb06501.x
Angleman SB, Harris TB, Melzer D. The role of waist circumference in predicting disability in periretirement age adults. Int J Obes 2006;30:364–373. doi: 10.1038/ sj.ijo.0803130
Guallar-Castillon P, Sagardui-Villamor J, JR B, et al. Waist circumference as a predictor of disability among older adults. Obesity 2007;15:233–244
Pires Corona L, Da T, Alexandre S, et al. Abdominal obesity as a risk factor for disability in Brazilian older adults. Public Health Nutr 2017;20:1046–1053. doi: 10.1017/S1368980016003505
Hamer M, Batty GD, Kivimaki M. Sarcopenic obesity and risk of new onset depressive symptoms in older adults: English Longitudinal Study of Ageing. Int J Obes (Lond) 2015;39:1717–20. doi: 10.1038/ijo.2015.124
Marijnissen RM, Vogelzangs N, Mulder ME, et al. Metabolic dysregulation and latelife depression: a prospective study. Psychol Med 2017;47:1041–1052. doi: 10.1017/ S0033291716003196
Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, Obesity, and Depression. Arch Gen Psychiatry 2010;67:220. doi: 10.1001/archgenpsychiatry.2010.2
Xiang X, An R. Obesity and onset of depression among U.S. middle-aged and older adults. J Psychosom Res 2015;78:242–248. doi: 10.1016/j.jpsychores.2014.12.008
Murphy RA, Reinders I, Register TC, et al. Associations of BMI and adipose tissue area and density with incident mobility limitation and poor performance in older adults. Am J Clin Nutr 2014;99:1059–65. doi: 10.3945/ajcn.113.080796
Keevil VL, Luben R, Dalzell N, et al (2015) Cross-Sectional Associations between Different Measures of Obesity and Muscle Strength in Men and Women in a British Cohort Study. J Nutr Health Aging 2015;19:3–11. doi: 10.1007/s12603-014-0492-6
Vermeulen J, Neyens JCLJ, van Rossum E, et al (2011) Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr 2011;11:33. doi: 10.1186/1471-2318-11-33
Bianchi L, Ferrucci L, Cherubini A, et al (2015) The Predictive Value of the EWGSOP Definition of Sarcopenia: Results From the InCHIANTI Study. J Gerontol A Biol Sci Med Sci 2015;71:glv129-. doi: 10.1093/gerona/glv129
Alexandre T da S, Scholes S, Ferreira Santos JL, et al. The combination of dynapenia and abdominal obesity as a risk factor for worse trajectories of IADL disability among older adults. Clin Nutr 2017;:. doi: 10.1016/j.clnu.2017.09.018
Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging 2009;13:881–9. doi: 10.1007/s12603-009-0246-z
Gomez F, Zunzunegui MV, Alvarado B, et al. Cohort Profile: The International Mobility In Aging Study (IMIAS). Int J Epidemiol, 2018. doi: 10.1093/ije/dyy074
Zunzunegui MV V, Alvarado BEE, Guerra R, et al. The mobility gap between older men and women: The embodiment of gender. Arch Gerontol Geriatr 2015;61:140–148. doi: 10.1016/j.archger.2015.06.005
Caldas VV de A, Zunzunegui MV, Freire A do NF, Guerra RO. Translation, cultural adaptation and psychometric evaluation of the Leganés cognitive test in a low educated elderly Brazilian population. Arq Neuropsiquiatr 2012;70:22–7
Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-Extremity Function in Persons over the Age of 70 Years as a Predictor of Subsequent Disability. N Engl J Med 1995;332:556–562. doi: 10.1056/NEJM199503023320902
Nagi SZ. An Epidemiology of Disability among Adults in the United States. 1976;54:439–467
Freire a. N, Guerra RO, Alvarado B, et al. Validity and Reliability of the Short Physical Performance Battery in Two Diverse Older Adult Populations in Quebec and Brazil. J Aging Health 2012;24:863–878. doi: 10.1177/0898264312438551
Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 2000;55:M221–31
Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med 1995;332:556–61. doi: 10.1056/NEJM199503023320902
World Health Organization (2000) WHO | Obesity: preventing and managing the global epidemic. World Health Organization
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and T of HBC in A (Adult TPI. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–421
Fess E. Grip Strength, 2nd ed. American Society of Hand Therapists, Chicago 1992
Ylli A, Miszkurka M, Phillips SP, et al. Clinically relevant depression in old age: An international study with populations from Canada, Latin America and Eastern Europe. Psychiatry Res 2016;241:236–241. doi: 10.1016/j.psychres.2016.04.096
Bento JA, Lebrão ML. Suficiência de renda percebida por pessoas idosas no Município de São Paulo/Brasil. Cien Saude Colet 2013;18:2229–2238. doi: 10.1590/ S1413-81232013000800007
Guralnik JM. Assessing the impact of comorbidity in the older population. Ann Epidemiol 1996;6:376–80
Fried LP, Bandeen-Roche K, Kasper JD, Guralnik JM. Association of comorbidity with disability in older women: the Women’s Health and Aging Study. J Clin Epidemiol 1999;52:27–37
Marsh AP, Janssen JA, Ip EH, et al. Assessing Walking Activity in Older Adults: Development and Validation of a Novel Computer-Animated Assessment Tool. Journals Gerontol Ser A Biol Sci Med Sci 2015;70:1555–1561. doi: 10.1093/gerona/ glv101
Drumond Andrade FC, Guevara PE, Lebrão ML, et al. Gender Differences in Life Expectancy and Disability-Free Life Expectancy Among Older Adults in S??o Paulo, Brazil. Women’s Heal Issues 2011;21:64–70. doi: 10.1016/j.whi.2010.08.007
Koster A, Patel K V., Visser M, et al. Joint Effects of Adiposity and Physical Activity on Incident Mobility Limitation in Older Adults. J Am Geriatr Soc 2008;56:636–643. doi: 10.1111/j.1532-5415.2007.01632.x
Guallar-Castillón P, Sagardui-Villamor J, Banegas JRJR, et al. Waist circumference as a predictor of disability among older adults. Obesity 2007;15:233–244. doi: 10.1038/ oby.2007.532
Naugle KM, Higgins TJ, Manini TM. Obesity and use of compensatory strategies to perform common daily activities in pre-clinically disabled older adults. Arch Gerontol Geriatr 2012;54:e134–e138. doi: 10.1016/j.archger.2011.10.017
Yerrakalva D, Mullis R, Mant J. The associations of fatness, fitness, and physical activity with all-cause mortality in older adults: A systematic review. Obesity 2015;23:1944–1956
Na YM, Park HA, Kang JH, et al. Obesity, obesity related disease, and disability. Korean J Fam Med 2011;32:412–22. doi: 10.4082/kjfm.2011.32.7.412
Schrager MA, Metter EJ, Simonsick E, et al. Sarcopenic obesity and inflammation in the InCHIANTI study. J Appl Physiol 2007;102:919–25. doi: 10.1152/ japplphysiol.00627.2006
Angel RJ, Angel JL, Hill TD. Longer lives, sicker lives? Increased longevity and extended disability among Mexican-origin elders. Journals Gerontol -Ser B Psychol Sci Soc Sci 2015;70:639–649. doi: 10.1093/geronb/gbu158
Hill TD, Burdette AM, Taylor J, Angel JL. Religious Attendance and the Mobility Trajectories of Older Mexican Americans. J Health Soc Behav 2016;57:118–134. doi: 10.1177/0022146515627850
Schaap LA, Koster A, Visser M. Adiposity, Muscle Mass, and Muscle Strength in Relation to Functional Decline in Older Persons. Epidemiol Rev 2013;35:51–65. doi: 10.1093/epirev/mxs006
Perera S, Patel K V, Rosano C, et al. Gait Speed Predicts Incident Disability: A Pooled Analysis. J Gerontol A Biol Sci Med Sci 2016;71:63–71. doi: 10.1093/gerona/glv126
Abellan Van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging 2009;13:881–889. doi: 10.1007/s12603-009-0246-z
Batsis JA, Mackenzie TA, Bartels SJ, et al. Diagnostic accuracy of body mass index to identify obesity in older adults: NHANES 1999–2004. Int J Obes (Lond) 2016;40:761–7. doi: 10.1038/ijo.2015.243
Spencer SM, Albert SM, Bear-Lehman J, Burkhardt A. Relevance of race and ethnicity for self-reported functional limitation. J Am Geriatr Soc 2008;56:553–7. doi: 10.1111/j.1532-5415.2007.01595.x
Crawford SL, Jette AM, Tennstedt SL. Test-retest reliability of self-reported disability measures in older adults. J Am Geriatr Soc 1997;45:338–41
Misra A, Wasir JS, Vikram NK. Waist circumference criteria for the diagnosis of abdominal obesity are not applicable uniformly to all populations and ethnic groups. Nutrition 2005;21:969–976. doi: 10.1016/j.nut.2005.01.007
Chateau-Degat ML, Dewailly E, Poirier P, et al. Comparison of diagnostic criteria of the metabolic syndrome in 3 ethnic groups of Canada. Metabolism 2008;57:1526–1532. doi: 10.1016/j.metabol.2008.06.006
Ujcic-Voortman JK, Bos G, Baan CA, et al. Obesity and body fat distribution: Ethnic differences and the role of socio-economic status. Obes Facts 2011;4:53–60. doi: 10.1159/000324555
Bannerman E, Miller MD, Daniels LA, et al. Anthropometric indices predict physical function and mobility in older Australians: the Australian Longitudinal Study of Ageing. 2017;doi: 10.1079/PHN2002336
Nam S, Kuo Y-F, Markides KS, et al. Waist circumference (WC), body mass index (BMI), and disability among older adults in Latin American and the Caribbean (LAC). Arch Gerontol Geriatr 2012;55:e40–e47. doi: 10.1016/j.archger.2012.04.006
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fernandes de Souza Barbosa, J., dos Santos Gomes, C., Vilton Costa, J. et al. Abdominal Obesity and Mobility Disability in Older Adults: A 4-Year Follow-Up of the International Mobility in Aging Study. J Nutr Health Aging 22, 1228–1237 (2018). https://doi.org/10.1007/s12603-018-1100-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-018-1100-y