Abstract
Background: Aim
The aim of this study was to explore whether multidomain intervention (MI) and Omega-3 Polyunsaturated Fatty Acids supplementation can modify the cognitive function on elderly according to frail status.
Method
Data are from a secondary exploratory analysis of the Multidomain Alzheimer Preventive Trial (MAPT), a French community-dwellers aged 70 or over reporting subjective memory complaints, but free from clinical dementia. The multidomain intervention consisted of 2 hours group sessions focusing on three domains (cognitive stimulation, physical activity, and nutrition) and a preventive consultation (at baseline, 12 months, and 24 months). For Omega-3 Polyunsaturated Fatty Acids supplementation, participants took two capsules of either placebo or polyunsaturated fatty acids daily. Linear mixed-model repeated-measures analyses were used including baseline, 6, 12, 24 and 36-month follow-up data to assess between-group differences in the change in cognitive tests over 36 months.
Results
The overall mean age of the MAPT study population was 75.25(±4.38). A tend toward significant differences in TMT-A were found for the effect of the multidomain intervention on the prefrail group compared to non-frail group. The MI and n3 PUFA program could not significantly have reduced cognitive function in a sample of pre-frailty elders.
Conclusion
This populationbased study in community-dwellers aged 70 years or over suggested that multidomain intervention and n3 PUFA supplementation have not significant effects on cognitive function change in frail older adults with memory complaints. The beneficial effect of multidomain intervention and n3 PUFA supplementation on cognitive function did not differ between frail and nonfrail participants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preventive intervention able to modify the natural history of age-related conditions such as reduce the risk of cognitive impairment are needed in the field of Alzheimer Disease (1–3).
Because of the multifactorial nature of AD, of the most promising preventive interventions for AD, multidomain intervention (MI) is surely one of the most studied and promising (4–6).
The intervention in frail elders for preventing negative health-related outcomes has recently been provided by the Lifestyle Interventions and Independence for Elderly (LIFE) trial. The authors shows that the beneficial effect of physical activity on the incidence of major mobility disability did not differ between frail and nonfrail participants (7). Another research on nonpharmacological interventions such as physical exercise and nutritional interventions showed promising effects on frailty status, functional outcomes, and cognitive outcomes. These interventions can be combined with each other or with other (eg, pharmacological, hormonal, or cognitive) therapies to prevent or treat frailty (8). There is a current consensus that physical frailty is potentially reversible or modifiable by interventions suggesting the evidence based interventions for targeting frail older people (9). Frailty is a geriatric syndrome caused by the loss of reserve capacity in multiple physiological systems making older adults more vulnerable to adverse environment (10). Frailty has been associated with risk of negative health-related outcomes including falls, hospitalizations, disability, institutionalization, and mortality (11–13). The clinical identification of frailty could be playing an important role in the development of preventive strategies against age-related conditions (14). To our knowledge, no study has yet explored whether MI and Omega-3 Polyunsaturated Fatty Acids supplementation can modify the cognitive function on elderly according to frail status. In this work, we hypothesize that the effects of MI and Omega-3 Polyunsaturated Fatty Acids supplementation may be influenced by the frailty status. This hypothesis is based on data from the Multidomain Alzheimer Preventive Trial (MAPT) [Therefore the results were recently published (6) and the findings for the primary outcome (the change from baseline to 36 months in a composite Z score combining four cognitive tests) were negative], in which participants on MI showed a trend towards less cognitive decline over 36 months in comparison to subjects on placebo. Here we sought to extend our findings by exploring the effects of MI on a number of cognitive tests in subjects in order to obtain preliminary information on which cognitive domains might be affected by MI in elderly according frail status.
Methods
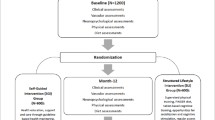
The data used in this study was collected from the MAPT study, a 4-arm randomized controlled trial aimed at assessing the effects of isolated supplementation with omega-3 fatty acid, an isolated multidomain intervention (consisting of nutritional counseling, physical exercise, cognitive stimulation), or a combination of the 2 interventions, versus placebo, on cognitive functions modifications in older persons aged 70 years and older. A detailed description of the methodology used for the MAPT study was already published (15). A total of 1,680 individuals aged 70 and older, initially non-institutionalized, were included in 13 French memory clinics follow up for 3 years. The protocol is registered on a public-access clinical trial database (www.clinicaltrials.gov, Number: NCT01513252). Written informed consent was obtained from all participants.
Frailty Status: frailty was defined according to the five components proposed by Fried and colleagues: (i) unintentional weight loss (self-reported unintentional loss of 4.5 kg or more recently); (ii) exhaustion (using two items of the Center for Epidemiologic Studies Depression Scale (16) (CES-D) : during the past week, “I felt that everything I did was an effort” and “I could not get going); (iii) weakness (using the handgrip strength ascertained by dynamometer); (iv) slowness (the time needed to cover the four-meter walk) and (v) low energy expenditure ( no engagement in physical activities). Participants meeting three or more criteria were classified as frail, those meeting one or two were considered prefrail, and those meeting none as non-frail (11).
MAPT intervention
MAPT was a multicenter, randomized, placebo-controlled superiority trial with four parallel groups, including three intervention groups (i.e, one group with a multidomain intervention plus placebo, one group with polyunsaturated fatty acids and one group with a multidomain intervention plus polyunsaturated fatty acids and one placebo group). The multidomain intervention consisted of 2 hours group sessions focusing on three domains (cognitive stimulation, physical activity, and nutrition) and a preventive consultation (at baseline, 12 months, and 24 months) and for Omega-3 Polyunsaturated Fatty Acids supplementation, participants took two capsules of either placebo or polyunsaturated fatty acids daily. The n-3 PUFA supplementation group consumed a daily dose of DHA (800 mg) and EPA (a maximum amount of 225 mg) for 3 years. The placebo group received identical capsules comprising liquid paraffin oil (6).
Cognitive assessment
Cognitive tests
The battery of neuropsychological tests included the Controlled Oral Word Association Test and Category Naming Test (17) (COWAT and CNT, for verbal fluency), the Digit Symbol Substitution Subtest of the Wechsler Adult Intelligence Scale-Revised (for attention and executive function) (18), the Trail-Making Test (19) (TMT), the Mini Mental State Examination (20) (MMSE) were used to evaluate cognitive changes over 36 months. Data from cognitive tests conducted at study baseline, then at 6, 12, 24 and 36 months were used in this study.
Others Variables
Socio-demographic information included age and sex. Educational level was defined as a four-level variable: no diploma or primary school certificate, secondary education, high school diploma and university level. The body mass index (BMI) was defined as weight (in kilograms) divided by squared height (in meters).
Statistical analysis
Chi-square and t test were used to compare the participants’ characteristics from the two groups according to the frailty status at baseline. To assess and to compare the effect of each intervention group on the change of cognitive functions at 36 months according to the level of frailty at baseline we used linear mixed models including baseline, 6, 12, 24 and 36-month follow-up data. These linear mixed models included a centre specific random intercept (when this parameter was significant) to take into account the correlation intra centre and a subjectspecific random intercept and slopes to take into account the correlation intra subject. For each model, we included the following fixed effects: intervention group, time, interaction between intervention group and time. Time was treated as a continuous variable and we included in the model time² and time3 terms when the trajectory forms were not linear. For each model, we presented means estimate and standard errors (SE). P values were based on two-sided tests. To account for the multiplicity of tests with an overall risk of 5%, each comparison compared to the reference group is considered significant if the «p» is <0.05/number of comparison, either 0.017 for 3 comparisons (first analysis), and 0.025 for 2 comparisons (second analysis). All analyses were performed using SAS software version 9.4 (SAS Institute Inc, Cary, NC).
Results
Baseline descriptive characteristics of the participants included in this study (n =1464) are presented Table 1. The overall mean age of the MAPT study population was 75.25(±4.38). Compared to non-frail, pre-frail participants (n=665 persons) have low performance of cognitive test : TMTA [49.16(19.14) vs 44.48(14.62)], TMTB [132.65 (71.37) vs 113.78(51.94)], FCSRT [71.68 (10.28) vs 73.89(9.06)], MMSE [27.95(1.60) vs 28.24(1.55)], COWAT [19.06(6.73) vs 20.31(6.29)], CNT [25.02(7.69) vs 26.76(7.12)] , DSST [36.25(10.24) vs 39.12(9.52)], and high BMI [26.74(4.36) vs 25.63(7.71)]. No significant differences in gender and educational level between groups were found. Table 2 shows the result of the changes in cognitive test scores over 36 months. Linear mixed-model repeated-measures analyses showed no differences in the change in cognitive tests over 36 months according to frail criteria status.
Table 3 shows the result of the difference of change between baseline and 36 months. A trend toward significance difference in TMT-A were found for the effect of the MI between the two groups (pre-frail or not).
Discussion
Our results from a large sample of French communitydwellers show that the MI and n3 PUFA program could not significantly have reduced cognitive function in a sample of pre-frailty elders. Our findings are consistent with the previous finding of MAPT trail in general population (6). Such finding suggests that frailty status is not the mechanism explaining cognitive change after MI and n3 PUFA. However, we show an improvement in Trail Making Test-A (TMTA) performance with a trend toward significance difference for the effect of the MAPT interventions between the two groups (pre-frail or not). Low TMT-A possibly reflects an age-related reduction in physiologic reserve, which may render the brain more vulnerable to the accumulation of cognitive decline and subsequent damage.
No evident hypothesis can explain the lack of association between MI and n3 PUFA program and cognitive performance in our study. However, several hypotheses could explain this negative finding: 1/ Low analytic sample size may have resulted in limited, making difficult the detection of an association. 2/ People who reach the age 70 are somewhat survivors. Thus a survival effect may be a second explanation. Another explanation would be related to the definition of the phenotype of frailty in the current study (6, 21) (participants were classified as frail if they met one or more criteria among the following: unintentional weight loss, exhaustion, weakness, slowness and low energy expenditure). It is possible that the characteristic on Fried’s model (11) was not maintained in the proposed instrument and we could not capture frailty status of participants (in our study only 5 % of participants as consider as frail according to phenotype of frailty).
To our knowledge, this is the first randomized clinical trial that has evaluated the effects of MI and n3 PUFA supplementation on cognitive function according to frailty status in older persons. Physical activity (frailty criterion) is a potential intervention to modulate the neuromusclar response and it is possible that the physical activity may modify the neuromuscular signals generated in muscle activation. Taken together, these findings suggest that the understanding of physiopathology of frailty syndrome beyond the conceptual may help to improve diagnostic acuity and present meaningful targets for interventions among cognitively frail individuals to prevent dementia (1, 3).
The strengths of the present study are the large number of participants selected from multiple community-dwelling, the longitudinal design with substantial follow-up in a wellcharacterized set of non-demented older adults with memory complaint and the very low percentage of missing data. Our data are collected as part of standard care, thus highly mirroring the current clinical practice. p ]The main limitation of this study is related to the fact that it is a post-hoc analysis, the study was not specifically design to detect a significant difference taking to account the frailty status and the definition of frailty (different to the operational definition proposed by Fried et al.). The individual frailty criterion could not be able to define frailty status. The study participants were recruited among community-dwelling older persons with a subjective memory complaint as main inclusion criteria. This may introduce a representativeness bias. Our findings may therefore not be applicable to communitydwelling older adults without any memory complaint.
Conclusions
This population-based study in community-dwellers aged 70 years or over suggested that multidomain intervention and n3 PUFA supplementation have not significant effects on cognitive function change in frail older adults with memory complaints. These findings need to be confirmed by further studies with larger sample size and better define frail status of participants.
Acknowledgement section: MAPT/DSA funding must be acknowledged using language similar to the following: “The MAPT study was supported by grants from the Gérontopôle of Toulouse, the French Ministry of Health (PHRC 2008, 2009), Pierre Fabre Research Institute (manufacturer of the omega-3 supplement), Exhonit Therapeutics SA, and Avid Radiopharmaceuticals Inc. The promotion of this study was supported by the University Hospital Center of Toulouse. The data sharing activity was supported by the Association Monegasque pour la Recherche sur la maladie d’Alzheimer (AMPA) and the UMR 1027 Unit INSERM-University of Toulouse III”.
Author Contributions: Maturin Tabue-Teguo: Conceptualization and design, interpretation of data. He wrote the manuscript, had full access to all of the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis. Cantet Christelle: statistical analyses, interpretation of data, drafting the manuscript. Sandine Andrieu, Barreto de Souza philippe, Simo Nadine, Fougère Bertrand: Interpretation of data, revision of the article. Jean-François Dartigues and Bruno Vellas: Conceptualization and design, interpretation of data, drafting the manuscript.
Financial Disclosure: None.
Conflict of interest: None.
References
Sink KM, Espeland MA, Castro CM, et al. Effect of a 24-Month Physical Activity Intervention vs Health Education on Cognitive Outcomes in Sedentary Older Adults: The LIFE Randomized Trial. JAMA 2015;314:781–90. doi:10.1001/jama.2015.9617
Albanese E, Shah H, Rudan I, et al. Dementia research priorities-1. Lancet Neurol 2017;16:180–1. doi:10.1016/S1474-4422(17)30006-6
Andrieu S, Coley N, Lovestone S, et al. Prevention of sporadic Alzheimer’s disease: lessons learned from clinical trials and future directions. Lancet Neurol 2015;14:926–44. doi:10.1016/S1474-4422(15)00153-2
Ngandu T, Lehtisalo J, Solomon A, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet Lond Engl 2015;385:2255–63. doi:10.1016/S0140-6736(15)60461-5
Moll van Charante EP, Richard E, Eurelings LS, et al. Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): a clusterrandomised controlled trial. Lancet Lond Engl 2016;388:797–805. doi:10.1016/S0140-6736(16)30950-3
Andrieu S, Guyonnet S, Coley N, et al. Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (MAPT): a randomised, placebocontrolled trial. Lancet Neurol 2017;16:377–89. doi:10.1016/S1474-4422(17)30040-6
Trombetti A, Hars M, Hsu F, et al. Effet of physical activity on frailty: secondary analysis of a randomized controlled trail. Ann Intern Med. 2018 Jan 9. doi: 10.7326/M16-2011.
Fairhall N, Langron C, Sherrington C, et al. Treating frailty–a practical guide. BMC Med. 2011;9:83
Morley JE. Frailty: diagnosis and management. J Nutr Health Aging 2011;15:667–70.
Theou O, Brothers TD, Mitnitski A, et al. Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc 2013;61:1537–51. doi:10.1111/jgs.12420
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–156.
Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ Can Med Assoc J J Assoc Medicale Can 2005;173:489–95. doi:10.1503/cmaj.050051
Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. Lancet Lond Engl 2013;381:752–62. doi:10.1016/S0140-6736(12)62167-9
Subra J, Gillette-Guyonnet S, Cesari M, et al. The integration of frailty into clinical practice: preliminary results from the Gérontopôle. J Nutr Health Aging 2012;16:714–20. doi:10.1007/s12603-012-0391-7
Vellas B, Carrie I, Gillette-Guyonnet S, et al. MAPT Study: A multidomain approach for preventing Alzheimer’s disease: design and baseline data. J Prev Alzheimers Dis 2014;1:13–22.
Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1982;17:37–49.
Cardebat D, Doyon B, Puel M, et al. [Formal and semantic lexical evocation in normal subjects. Performance and dynamics of production as a function of sex, age and educational level]. Acta Neurol Belg 1990;90:207–17.
Kaufman AS. Test Review: Wechsler, D. Manual for the Wechsler Adult Intelligence Scale, Revised. New York: Psychological Corporation, 1981. J Psychoeduc Assess 1983;1:309–13. doi:10.1177/073428298300100310
Reitan R. Validity of the Trail Making Test as an indicator of brain damage. Percept Mot Skills. 1958:271–6.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98.
Delrieu J, Andrieu S, Pahor M, et al. Neuropsychological Profile of “Cognitive Frailty” Subjects in MAPT Study. J Prev Alzheimers Dis 2016;3:151–9. doi:10.14283/ jpad.2016.94
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tabue-Teguo, M., Barreto de Souza, P., Cantet, C. et al. Effect of Multidomain Intervention, Omega-3 Polyunsaturated Fatty Acids Supplementation or their Combinaison on Cognitive Function in Non-Demented Older Adults According to Frail Status: Results from the MAPT Study. J Nutr Health Aging 22, 923–927 (2018). https://doi.org/10.1007/s12603-018-1024-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-018-1024-6