Abstract
Objectives
The aim of the study was to investigate whether nutritional status as measured by the Mini Nutritional Assessment Short-Form (MNA-SF) predicts level of care of the discharge destination after post-acute care in a nursing home.
Design
Cohort study.
Setting
Post-acute intermediate care nursing home, 19-bed unit with increased multidisciplinary staff.
Participants
Patients ≥70 years in post-acute care (N=900) following an acute admission to the hospital.
Measurements
The predictive value of nutritional status, as measured by the MNA-SF, on discharge destination was analysed by means of a multinomial logistic regression model with the MNA-SF as the independent variable, discharge destination as the dependent variable and age and living situation as co-variates. The participants were grouped into three categories according to their discharge destination: home, other institution or readmitted to the hospital.
Results
A higher score on the MNA-SF significantly predicted a reduced risk of discharge to institution (adjusted OR=0.90 (95% CI=0.84;0.97), p=0.003).
Conclusion
Nutritional status, as measured by the MNA-SF, predicted discharge destination from an intermediate care nursing home following acute hospitalisation. The findings underscore the value of nutritional assessment as part of overall clinical assessment and care planning prior to discharge. The findings may also imply that interventions to improve nutritional status could increase patients’ ability to return home, as opposed to further institutionalisation, after hospitalisation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Poor nutritional status is common in elderly patients. In a pooled analysis with combined data on nutritional status in elderly women and men, the overall prevalence of malnutrition was 23%. Forty-six percent of the patients were categorised as being at risk of malnutrition (1). However, despite the high prevalence, malnutrition in geriatric patients is rarely recognised (2). Malnutrition is characterised by weight loss, loss of muscle mass and lack of energy. The deterioration of nutritional status has been associated with decreased independence in activities of daily living (ADL) and mobility in geriatric patients (3) and increased mortality after hip fracture surgery (4). Further, earlier studies have shown that nutritional status declines during hospital stay (5) and that malnutrition in elderly hospital patients increases the risk of death, prolonged hospital stay and results in discharge to a higher level of care (6).
Intermediate care in post-acute settings aims at increasing the independence of patients with the potential for rehabilitation. Currently, there is need for knowledge about the predictive value of various clinical characteristics for the level of health care needed by elderly patients after discharge. From the perspective of the clinician responsible for this patient group, knowledge about predictors for discharge destination is useful, as it helps in individualising treatment and level of care after discharge to meet the patients’ individual needs. From a health care service perspective, knowledge about the predictors for health care service use forms the basis for improved planning and monitoring of health services. Further, knowledge about the predictors of discharge destination is important as health care costs vary as a function of the level of care after discharge. Nutritional status may be one such factor that predicts the need for health care. However, studies exploring the question of whether, or to what extent, nutritional status predicts discharge destination are difficult to find.
A few previous studies have examined whether nutritional status predicts discharge destination. These studies found that poor nutritional status predicts discharge to a higher level of care (6) and long-term care (7). Furthermore, good nutritional status predicts patients returning home (8). Van Nes and colleagues found that patients with poor nutritional status, as identified by the Mini Nutritional Assessment (MNA), had a higher rate of discharge to nursing homes compared to well-nourished patients (9). Although these studies all support the predictive value of nutritional status for discharge destination, they may be criticised for having low sample sizes, low participation rates or for being performed on convenience samples. A systematic literature review of factors affecting outcomes in older medical patients identified only two reports investigating the predictive value of nutritional status, neither of which utilised discharge destination as an outcome measure (10).
As poor nutritional status is common in the elderly and affects health outcomes negatively, there are arguments supporting the relevance of nutritional screening in this group. However, screening has to be practical and resource efficient to be performed in a clinical setting. Hence, gaining more knowledge about the predictive value of shorter, available screening tools that are practical to use in clinical settings is important. Studies investigating the predictive value of nutritional screening tools for discharge destination have reported conflicting results. A systematic review including seven studies with move to higher level care as an outcome measure found that only four showed associations with nutritional screening scores (11). One investigation utilised the six-item MNA-SF in a study of predictive factors for patients discharged after a post-acute care programme. This study suggested that patients with higher baseline MNA-SF scores, i.e. patients with better nutritional status, were more likely to return home than move to long-term care (8). In contrast, a study of several nutritional screening tools found no significant association between MNA-SF scores and discharge to a higher level of care (12). The contrasting findings underline the need to investigate the question of whether the MNA-SF has the ability to predict the risk of institutionalisation in a cohort that has a large sample size and low attrition rate.
The objective of the current study was to investigate whether nutritional status, as measured by the MNA-SF, predicts the level of care of the discharge destination after post-acute care in a nursing home. We hypothesised that lower MNA-SF scores predict a higher level of care of the discharge destination after post-acute care in an intermediate nursing home. To the authors’ knowledge, this is the first study to investigate the predictive value of the MNA-SF for discharge destination in a large group of patients after stay in a post-acute nursing home.
Materials and methods
Study design
The study was a cohort study of elderly patients transferred to an intermediate care nursing home after acute hospital admission. The patients were followed for a mean of 14 days after transfer from the general hospital to the intermediate care nursing home.
Setting and subjects
Data were collected from patients ≥ 70 years of age at the Storetveit nursing home unit for intermediate care in Bergen, Norway, from 2011 to 2014. The nursing home is owned by the municipality of Bergen and has a catchment area of approximately 250,000 citizens. The intermediate care unit (IC unit) is a 19-bed unit with multidisciplinary staff that provides post-acute care to elderly patients discharged from the two public hospitals in Bergen. The two public hospitals deliver specialised health services to 22 municipalities in Western Norway, covering approximately 435,000 citizens. The hospital doctors responsible for the patient prior to admission to the IC unit expect that the patient will be able to return home within two weeks of treatment in the IC unit.
Out of the 1,085 community living patients admitted to the IC unit for intermediate care after acute hospitalisation, 959 were included in the present study. Of these, 900 (mean age 84 years) who had valid MNA-SF scores and information about their discharge destination were included in the valid analysis file (Figure 1).
All patients admitted to Storetveit intermediate care unit were defined as eligible for inclusion. The inclusion criteria were as follows: Patient ≥ 70 years of age that was homedwelling in the municipality of Bergen. The patients were respiratorily and circulatorily stable and with no major cognitive impairment or delirium, as judged by a clinical assessment by the hospital doctor before admission to Storetveit.
Data collection
The patients were asked to participate in the study by the doctor who admitted them to the IC unit. Demographic and baseline clinical characteristics of the patients were obtained from hospital records. During the stay in the IC unit, the Comprehensive Geriatric Assessment (CGA) was performed on all the patients during the first week, including an assessment of their activities of daily living (ADL-functioning) and functional status using the Barthel Index (13). Cognitive impairment was assessed with the Mini Mental State Examination (MMSE) (14), and depressive symptoms were assessed with the Geriatric Depression Scale (GDS) (15). Nutritional assessment was done using the Norwegian version of the six-item validated MNA-SF (16, 17). Discharge destination was defined by three categories: whether the patient was discharged to home, an institution or readmitted to the hospital.
Sampling process
An overview of patient inclusion in the study is shown in Figure 1. A total of 964 patients met the criteria for inclusion. Of the 959 patients who agreed to participate, 49 with missing MNA-SF-scores and 2 who died were excluded from the analysis sample. Furthermore, 8 patients were discharged for further rehabilitation, and these patients were excluded since the group size (n=8) was too small for statistical analyses. Thus, analyses were performed on a valid sample of 900 patients, which represented 83% of the patients admitted to the IC unit and 93% of the patients invited to participate. For further details on the setting and subjects, see Abrahamsen (2015) (18).
Ethical considerations
Ethical approval was obtained from the Western Norway Regional Committee for Medical and Health Research Ethics (ref. no 2011/1893). The patients provided written informed consent before entering the study.
Statistics
A multinomial logistic regression model with MNA-SF as the independent variable and discharge destination as the dependent variable was employed. Age and living situation were entered as co-variates into the model, as these could confound the relationship between nutritional status and discharge destination. Odds ratios with 95% confidence intervals (CI) were estimated in the model, and discharge to home was entered as the reference category. Tests were twotailed with a p-value of 0.05. Statistical analysis was conducted using IBM SPSS Statistics 22 (Armonk, NY: IBM Corp.).
Results
Patient characteristics
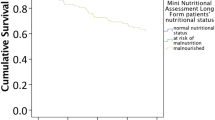
The patient characteristics can be seen in Table 1. The mean age was 84 years (standard deviation (SD) 6.2, range 70–102), and the mean MNA-SF score was 9.5 (SD 2.7, range 2–14). Fracture/orthopaedic injury/fall were the most common causes of hospital stay (36% of patients). Eighty-three per cent of patients were discharged to their homes, while fourteen per cent were transferred to another institution and three per cent were readmitted to the hospital.
The predictive value of the MNA-SF for discharge destination
In the crude multinomial logistic regression model with the MNA-SF as the predictor variable and discharge destination (home/institution/readmission) as the outcome variable, higher MNA-SF scores were significantly associated with a decreased risk of being discharged to an institution compared to home (odds ratio (OR)=0.90 (95% CI=0.84;0.97), p=0.004) (see Table 2). In the fully adjusted model, higher MNA-SF scores significantly predicted a reduced risk of discharge to an institution (OR=0.90 (95% CI=0.84;0.97), p=0.003). The OR of being readmitted to the hospital versus home was 0.96 (95% CI=0.83;1.12) in the fully adjusted model. However, the OR for readmission was not significant in either the crude or fully adjusted model (all p>0.05).
Discussion
The present study aimed to investigate the predictive value of nutritional status, as measured by the MNA-SF, on discharge destination for a cohort of elderly patients who stayed in an intermediate post-acute care nursing home after treatment at a general hospital. The patients with better nutritional status, i.e. higher scores on the MNA-SF, had a lower risk of being discharged to an institution compared to home. This finding supports the findings of Van Nes et al. (9) and Rasheed et al. (7), who found a higher rate of discharge to nursing homes and long term care, respectively, in elderly hospitalised patients with poor nutritional status compared to patients with normal nutritional status. The findings are also in accordance with those of Charlton et al. (6), who showed that malnutrition in subacute patients was associated with discharge to a higher level of care. In contrast, one investigation of factors predicting outcomes failed to identify nutritional status as a predictor for institutionalisation (19). Although Alarcon et al. indicated that they used the CGA, they did not report details regarding their negative findings, thus precluding any discussion of these contrasting finding. Dent et al. investigated the association of different nutritional screening tools (NSTs) with hospital discharge outcomes. In their study MNA-SF scores did not predict patients’ moving to a higher level of care after hospital discharge, nor did other NSTs (12). The discrepancy between our findings and those of Dent et al. (12) may be explained by different settings and patient groups. The participants in the current study were receiving intermediate care after hospital discharge, i.e. they were considered to have rehabilitation potential and did not have major cognitive impairments, whereas Dent et al. studied in-patients in a higher specialised geriatric unit in a hospital setting including patients with dementia. Slattery and colleagues (20) also failed to find a significant relationship between nutritional status and level of care after discharge from a rehabilitation unit, but the results in their study were inconclusive due to the small sizes of the subgroups.
The existing literature has shown that assessment tools that are far more comprehensive than the short MNA-SF version used in the present study predict level of care after discharge (6, 7, 9). The finding that the six-item version of the MNA-SF instrument predicted discharge destination in our study supports the validity and predictive power of this short instrument version. As the acceptability of the six-item MNA-SF version is far higher in clinical settings than that of more extensive instruments assessing nutritional status, we argue that the sixitem MNA-SF should be used in such settings. Challenges related to the acceptability and feasibility of longer instruments may be the reason why only 24% of the participants completed the full 18-item version of the MNA in the study by Van Nes et al. (9). The present study thus indicates that the MNA-SF could be used as a screening tool in elderly patients admitted to post-acute care to identify those in need of nutritional support and in the planning of care for older patients. Furthermore, the increased accuracy of nutritional support could lower the number of patients discharged to further stays in nursing homes. The identification of nutritional risk and malnutrition is crucial for early nutritional interventions, which in turn may improve both functional and nutritional status (21) and decrease mortality (22).
Contrary to expectations, patients living alone did not have a significantly higher risk of institutionalization compared to patients living with someone. This might be due to differences prior to hospitalization, as elderly persons living alone may have a generally better functional level.
The strengths of the current study include the large sample size and the high participation rate, which increases the generalisability of findings. We argue that the findings are transferable to patients treated in intermediate care units, and possibly also to elderly patients in specialised hospital settings. Further, the thorough assessment of nutritional status, clinical status and relevant domains of functioning represent strengths of the study.
In our study, only 5% of the participants had missing data on the MNA-SF. Participants with missing MNA-SF scores may have had poorer functioning or more severe pathology than the participants with completed MNA-SF scores. We argue, however, that the level of missing values (5% of the 959 patients that met the inclusion criteria) in such a large sample will have a low impact on the results produced.
A possible limitation of this study is the lack of information on the participants’ educational level. However, very few members of the generation studied completed more than the seven years of schooling that were compulsory at the time they grew up.
The effect of nutritional status on discharge destination demonstrated in the present study may be mediated by the patients’ level of functioning. However, a recent study found that MNA-SF was less associated with functional level than the full MNA, as the short form has fewer items regarding functional level and independence (23). Still, while being aware of the fact that the effect of malnutrition on discharge destination may be shared with the effect of the patients’ functional level, we argue that the present study supports the MNA-SF as a useful predictor for discharge.
A low sample size in one of the outcome category groups, readmission to hospital (n=24), imposed a risk of type II error (i.e. false negative finding due to small group size) in this analysis. Therefore, the finding of no statistically significant association of nutritional status with readmissions should be interpreted with caution. Consequently, the association between nutritional status and readmission rates needs to be further investigated in future studies with larger group sizes. There are some previous reports showing that the rates of hospital readmission were not associated with MNA/MNA-SF scores (6, 19, 20).
Conclusion
The early identification of predictive factors for institutionalisation may help health care providers, patients and families to plan care and facilitate the appropriate use of health care services. The current study supports previous findings regarding the predictive value of nutritional status for discharge destination, as it shows that the clinically applicable six-item MNA-SF predicts the risk of subsequent institutionalisation after post-acute care. The findings underscore the importance of nutritional assessment in intermediate care nursing home residents. They may also imply that interventions to improve nutritional status could increase patients’ ability to return home, as opposed to further institutionalisation, after hospitalisation. Future research should aim at identifying nutritional interventions targeting the ability to return home following post-acute care.
Ethical standards: Ethical approval was obtained from the Western Norway Regional Committee for Medical and Health Research Ethics (ref. no 2011/1893). The patients provided written informed consent before entering the study.
Conflict of interest: The authors KIF, EB and JFA declare no conflicts of interest.
Acknowledgements: The authors thank Cathrine Haugland, research physiotherapist at Storetveit Nursing Home, Bergen, for assistance with the database.
References
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, Thomas DR, Anthony PS, Charlton KE, Maggio M, Tsai AC, Vellas B, Sieber CC. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc 2010;58:1734–8. doi: 10.1111/j.1532- 5415.2010.03016.x
Volkert D, Saeglitz C, Gueldenzoph H, Sieber CC, Stehle P. Undiagnosed malnutrition and nutrition-related problems in geriatric patients. J Nutr Health Aging 2010;14:387–92. doi: 10.1007/s12603-010-0085-y
Schrader E, Baumgartel C, Gueldenzoph H, Stehle P, Uter W, Sieber CC, Volkert D. Nutritional status according to Mini Nutritional Assessment is related to functional status in geriatric patients—independent of health status. J Nutr Health Aging 2014;18:257–63. doi: 10.1007/s12603-013-0394-z
van Wissen J, van Stijn MF, Doodeman HJ, Houdijk AP. Mini Nutritional Assessment and Mortality after Hip Fracture Surgery in the Elderly. J Nutr Health Aging 2016;20:964–8. doi: 10.1007/s12603-015-0630-9
McWhirter JP, Pennington CR. Incidence and recognition of malnutrition in hospital. BMJ 1994;308:945–8. doi: http://dx.doi.org/10.1136/bmj.308.6934.945
Charlton K, Nichols C, Bowden S, Milosavljevic M, Lambert K, Barone L, Mason M, Batterham M. Poor nutritional status of older subacute patients predicts clinical outcomes and mortality at 18 months of follow-up. Eur J Clin Nutr 2012;66:1224–8. doi: 10.1038/ejcn.2012.130
Rasheed S, Woods RT. Malnutrition and associated clinical outcomes in hospitalized patients aged 60 and older: an observational study in rural Wales. J Nutr Gerontol Geriatr 2013;32:71–80. doi: 10.1080/21551197.2012.753772
Lee Y-S, Lin C-S, Jseng Y-H, Luo T-W, Hung P-J, Wu M-C, Tang Y-J. Predictive factors for patients discharged after participating in a post-acute care program. J Clin Gerontol Geriatr 2012;3:25–8. doi: http://dx.doi.org/10.1016/j.jcgg.2011.11.008
Van Nes MC, Herrmann FR, Gold G, Michel JP, Rizzoli R. Does the mini nutritional assessment predict hospitalization outcomes in older people? Age Ageing 2001;30:221–6. doi: 10.1093/ageing/30.3.221
Campbell SE, Seymour DG, Primrose WR. A systematic literature review of factors affecting outcome in older medical patients admitted to hospital. Age Ageing 2004;33:110–5. doi: 10.1093/ageing/afh036
Dent E, Visvanathan R, Piantadosi C, Chapman I. Nutritional screening tools as predictors of mortality, functional decline, and move to higher level care in older people: a systematic review. J Nutr Gerontol Geriatr 2012;31:97–145. doi: 10.1080/21551197.2012.678214
Dent E, Chapman I, Piantadosi C, Visvanathan R. Nutritional screening tools and anthropometric measures associate with hospital discharge outcomes in older people. Australas J Ageing 2015;34:E1–6. doi: 10.1111/ajag.12130
Mahoney FI, Barthel DW. Functional Evaluation: The Barthel Index. Md State Med J 1965;14:61–5.
Strobel C, Engedal K. MMSE-NR. Norwegian revised mini mental status evaluation. Revised and expanded manual. National Center for Aging and Health, Oslo, 2008
Yesavage JA. Geriatric Depression Scale. Psychopharmacol Bull 1988;24:709–11. doi
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 2001;56:M366–72. doi: 10.1093/gerona/56.6.M366
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, Thomas DR, Anthony P, Charlton KE, Maggio M, Tsai AC, Grathwohl D, Vellas B, Sieber CC. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging 2009;13:782–8. doi: 10.1007/s12603-009-0214-7
Abrahamsen JF, Haugland C, Nilsen RM, Ranhoff AH. Three different outcomes in older community-dwelling patients receiving intermediate care in nursing home after acute hospitalization. J Nutr Health Aging 2016;20:446–52. doi: 10.1007/s12603-015-0592-y
Alarcon T, Barcena A, Gonzalez-Montalvo JI, Penalosa C, Salgado A. Factors predictive of outcome on admission to an acute geriatric ward. Age Ageing 1999;28:429–32. doi: 10.1093/ageing/28.5.429
Slattery A, Wegener L, James S, Satanek ME, Miller MD. Does the Mini Nutrition Assessment—Short Form predict clinical outcomes at six months in older rehabilitation patients? Nutr Diet 2015;72:63–8. doi: 10.1111/1747-0080.12094
Beck AM, Kjaer S, Hansen BS, Storm RL, Thal-Jantzen K, Bitz C. Follow-up home visits with registered dietitians have a positive effect on the functional and nutritional status of geriatric medical patients after discharge: a randomized controlled trial. Clin Rehabil 2013;27:483–93. doi: 10.1177/0269215512469384
Feldblum I, German L, Castel H, Harman-Boehm I, Shahar DR. Individualized nutritional intervention during and after hospitalization: the nutrition intervention study clinical trial. J Am Geriatr Soc 2011;59:10–7. doi: 10.1111/j.1532- 5415.2010.03174.x
Schrader E, Grosch E, Bertsch T, Sieber CC, Volkert D. Nutritional and Functional Status in Geriatric Day Hospital Patients-MNA Short Form Versus Full MNA. J Nutr Health Aging 2016;20:918–26. doi: 10.1007/s12603-016-0691-4
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Folven, K.I., Biringer, E. & Abrahamsen, J.F. Mini nutritional assessment short-form (MNA-SF) predicts institutionalisation in an intermediate post-acute care setting. J Nutr Health Aging 22, 199–204 (2018). https://doi.org/10.1007/s12603-017-0879-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-017-0879-2