Abstract
Objective
The use of drugs with intrinsic anticholinergic properties is widespread among old age persons. A growing body of evidences suggest that a high anticholinergic burden is associated with physical and cognitive impairment. However, the association between anticholinergic drug use and functional status is still poorly investigated, particularly among subjects with initial cognitive impairment.
Design
Cross-sectional study examining the association between drug-related anticholinergic burden and functional status in cognitively healthy (CH) (n=691), mild cognitive impairment (MCI) (n=541) or mild Alzheimer’s diseases (AD) (n=1127) subjects.
Setting
Data were gathered from the ReGAl project (Rete Geriatrica Alzheimer-Geriatric Network on Alzheimer’s disease), a large longitudinal Italian multicentric clinical-based study, promoted by the Italian Society of Gerontology and Geriatrics (SIGG).
Participants
2359 outpatients, older than 65 years, admitted to memory clinics. The total sample size, estimated according to a global effect size of 25% with type I error of 0.05 and a power of 95% is 2010 subjects.
Measurement
Functional status was evaluated by the Katz Index of Independence in Activities of Daily Living (ADL) and the Lawton-Brody Instrumental Activities of Daily Living (IADL) scales. The drug-related anticholinergic burden was estimated by the Anticholinergic Risk Scale (ARS).
Results
The 15.9 % (n=375) of total population used at least one drug with anticholinergic properties. Such a drug use was associated with partially dependence in ADL (OR:1.42, CI95%: 1.10-1.83; p=0.006), independently of gender, number of drugs, comorbidity index, presence of clinically relevant neuropsychiatric symptoms and adjusted MMSE. Anticholinergic drug use was associated with un-ability at each IADL task only in male MCI subjects, with significant impairment in shopping (p=0.011), and drug management (p=0.05).
Conclusions
The use of medications with anticholinergic properties is common among older persons cognitively health as well as with cognitive impairment. Our results suggest that the use of anticholinergic drugs is associated with functional impairment, especially in old age subjects with initial cognitive impairment. Minimizing anticholinergic burden should result in maintaining daily functioning, especially in a vulnerable population, such as MCI and mild AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional status is a proxy of the individual health status in terms of body structures, functional abilities and active participation in life (1). Decline of functional status, defined as functional impairment or disability in performing activities of daily living (ADL), is a risk factor for worsen quality of life, higher degree of dependence, healthcare service utilization and mortality (2-5). Among the many risk factors for functional decline, i.e. advanced age, low income, poor health status and comorbidities, prescription of drugs with intrinsic anticholinergic proprieties should be considered (6). In fact, many drugs with intrinsic anticholinergic effects are commonly used in geriatric clinical practice with a prevalence ranging from 8 to 37% (7), including tricyclic antidepressants, antipsychotics or first generation antihistamines.
While several studies have demonstrated the detrimental effect of anticholinergic drugs on cognition (8), fewer have been focused on the impact on physical performances and functional status. Han and colleagues (10) showed, in a cohort of community-living old men, that cumulative anticholinergic exposure across multiple medications over two years negatively affected executive functions. More recently, a prospective study on hospitalized elderly showed that drugs with anticholinergic properties are associated with worse performances in basic activities of daily living according to the global Barthel Index score (11). Indeed, Landi et al. (12) evaluated the association between the use of drugs with anticholinergic activity and measure of physical performance, muscle strength and functional status in frail subjects aged 80 years or older, showing a negative association between these drugs and impairment in physical performances. Such an association has been also confirmed more recently in nursing home residents (13).
To date, scanty data are available on the relationship between anticholinergic drug use and functional performance in ADL and in instrumental activities of daily living (IADL) among older persons with initial cognitive impairment, including MCI and mild AD. In light of such evidences, we aimed at investigating whether the use of drugs with anticholinergic properties is associated with impairment in functional status by a deep analysis among older persons with different cognitive status, from cognitively health to mild Alzheimer’s disease.
Subjects and methods
ReGAl project
Data were gathered from the ReGAl project (Rete Geriatrica Alzheimer-Geriatric Network on Alzheimer’s disease) as described elsewhere (14). Briefly, this is a large longitudinal Italian multicentric clinical-based study, promoted by the Italian Society of Gerontology and Geriatrics (SIGG), and focused on cognitive impairment and dementia in old age subjects. The project involves 36 Geriatric Memory Clinics (listed in the Acknowledgements), collecting data from all over Italy, coordinated by the Institute of Gerontology and Geriatrics, University of Perugia. At the beginning of the study, a training period was carried out and an instruction manual was delivered to each center. In each Memory Clinic collected data -including demographic characteristics, medical history, pharmacological treatments, clinical, neuropsychological and neurological examination, standard laboratory blood tests and neuroimagingwere recorded on a personal computer by means of a dedicated data entry program. Data were then sent to the coordinating center and processed for quality control and statistical analyses.
Subjects
The study sample consisted of 2359 subjects ≥65 years old, 691(29.3%) cognitively healthy (CH; CDR 0), 541 (23%) with mild cognitive impairment (MCI; CDR 0.5) and 1127 (47.7%) with mild Alzheimer’s disease (AD; CDR 1). Inclusion criteria for CH was an age and education-adjusted MMSE score ≥ 27, obtained by adding coefficients for classes of age and education (26). MCI and AD were diagnosed according to standard research criteria (27-29). Exclusion criteria were the presence of clinically severe psychiatric or systemic diseases, mental retardation, severe sensory impairment (blindness, deafness), and neurological conditions associated with cognitive impairment, a history of alcohol or substance abuse or dependence, and head injury with loss of consciousness.
Neuropsychological tests and behavioral assessment
The neuropsychological evaluation included the Mini Mental State Examination (MMSE), as test of general cognition (15) and a large battery of specific tests evaluating cognitive performances (14). The Clinical Dementia Rating scale (CDR) (16) was used to score dementia severity while current depressive symptoms were assessed by the 15-item version of the Geriatric Depression Scale (GDS) (17). Presence and severity of neuropsychiatric symptoms was evaluated with the Neuropsychiatric Inventory (NPI) (18). We considered neuropsychiatric symptoms with an FxG score ≥ 4 as clinically relevant.
Comorbidity
Comorbidity was assessed using the Cumulative Illness Rating Scale (CIRS) (19). This rating scale consists of 13 items covering several systemic diseases. Severity of diseases at each item is rated according to the following scale: 1 = no, 2 = mild, 3 = moderate, 4 = severe, 5 = life-threatening. No subjects obtained a score of 1 in our sample. After completion of the CIRS, two summary measures are calculated: the overall illness severity (SI) that represents the mean of the 13 CIRS items (CIRS-SI) and the comorbidity index (CIRS-CI) computed by counting the number of items with a score of moderate to severe degree (score ≥3). As a result, the CIRS-CI can also be considered as a surrogate of the number of clinically relevant concomitant diseases (19-21).
Functional status
Functional status was evaluated using the Katz Index of Independence in Activities of Daily Living (ADL) (22, 23) and Lawton-Brody Instrumental Activities of Daily Living (IADL) (24) scales. To avoid the underestimation of their own level of functional capacity, in subjects with cognitive impairment informant based rating of functional status were carried out (22). In most of the cases, informants were patients’ spouses or relatives, living in the same household.
ADL includes six activities: bathing, dressing, toileting, transferring, continence, and feeding. IADL includes eight activities: using telephone, shopping, meal preparation, housekeeping, laundry, use of transportation, selfadministration of drugs, and handling finances. Any dysfunction in the performances of these activities was recorded as dependence in the correspondent item. Because IADL items are often gender-specific, we used the version of the scale tested for male subjects included only five items, with housekeeping, cooking, and doing laundry excluded (25). ADL score ranges from 6 (total independence) to 0 (total dependence), and IADL from 8 (total independence) to 0 (total dependence) in women and from 5 (total independence) to 0 (total dependence) in men.
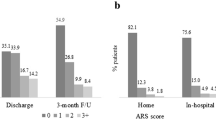
Anticholinergic Drug Burden
The ARS is a validated tool for estimating the extent to which an individual patient may be at risk of anticholinergic adverse effects that can lead to cognitive impairment (9). This is a ranked categorical list of commonly prescribed medications with anticholinergic potential that, compared with other scales, is more specific in capturing medication associated with a higher degree of functional impairment (9). The ARS scale ranks medications for anticholinergic potential on a 3-point scale (0: limited or none; 1: moderate; 2: strong; and 3 very strong). The ARS score for a patient is the sum of points of number of medications with anticholinergic effects. Subject using at least one drug with anticholinergic properties was indicated as “drug user”. Neither topical, ophthalmic, otologic, or inhalation medications nor the doses of drugs were considered in the development of the scale and therefore this information was not evaluated.
Calculations and statistical analyses
The observed data were normally distributed (Shapiro-Wilk W-Test) and presented as means ± Standard Deviation (SD). To assess differences among groups unpaired t test, ANOVA or Pearson’s Chi squared test were used, when appropriated. The association between anticholinergic drug use and functional impairment in ADL was examined by logistic regression analysis, where dependent variables were disability in ADL, defining the presence of functional independence as 0 and the presence of partial dependence as 1. The association between anticholinergic drug use and functional impairment in IADL was assessed by general linear model (GLM) procedures with an ordinal logistic regression analysis. The IADL disability were defined as functional totally independent as 0, partially dependent as 1 and totally dependent as 2. Indeed, binary logistic regression analyses were performed to evaluate the association between the anticholinergic drug use and un-ability to perform each single ADL or IADL task, independently of multiple covariates. The theory of directed acyclic graphs [30] was applied to select confounders for adjustment and analyzed with DAG program (version 0.21: http://epi.dife.de/dag). According to our graph the variable gender, number of drugs, CIRS (CI), presence of clinically relevant neuropsychiatric symptoms and MMSE adjusted belonged to the minimally sufficient adjustment set. We used these variables to adjust our effect estimation.
All p values presented are 2-tailed and a p < 0.05 was chosen for levels of significance. Statistical analyses were performed using SPSS 20 software package (SPSS, Inc., Chicago, IL).
Results
Clinical characteristics of all sample are displayed in Table 1. Subjects with cognitive impairment were older, with significantly lower scores on MMSE, GDS, and CIRS and used a lower number of drugs. The three groups significantly differ on ADL score and IADL score. The percentage of clinically relevant neuropsychiatric symptoms was higher in mild AD (78.0%; χ2= 193.972, p <0.0001) as compared with CH (46.9%) and MCI (57.5%), with the prevalence of anxiety and depression in CH and MCI, and irritability and agitation in mild AD.
About 16% (n=375) of participants used at least one drug with anticholinergic properties. Among drug users 93 (13.5%) were CH, 74 (13.7%) MCI and 208 (18.5%) mild AD (χ2=10.585; p=0.005). According with the ARS, the most used drugs with anticholinergic burden were paroxetine (3.7% and 4.6%, respectively) and trazodone (2.7% and 2.4%, respectively) in CH and MCI subjects and paroxetine (5.1%), trazodone (2.1%) and risperidone (2.3%) in mild AD.
The main characteristics of participants stratified according to anticholinergic drug use are shown in Table 2. Anticholinergic drug users were more likely to take a greater number of drugs, to be more functionally impaired in ADL and IADL, and to have lower cognitive performances and higher probability to suffer from neuropsychiatric symptoms.
Anticholinergic drug use and functional status
Functional status was assessed based on six activities of daily living (ADL). Grouping ADL according to the functional status in totally independent (ADL score =6), partially dependent (ADL score=1-5) and totally dependent (ADL score =0), none of subjects resulted totally dependent. Thus, we tested the association between anticholinergic drug use and disability in ADL using a binary logistic regression analysis with the dependent variable calculated as totally independent or partially dependent. The analysis conducted in all population revealed that participants taking drugs with anticholinergic properties had a higher probability to be partially dependent in ADL (OR:1.42, CI95%: 1.10-1.83; p=0.006), even after adjustment for gender, number of drugs, CIRS (CI), presence of clinically relevant neuropsychiatric symptoms, MMSE score. Distribution of ADL disability was examined item by item according to cognitive status (CH, MCI and mild AD) and in each subgroup by ARS exposure (Table 3). The prevalence of dependence on each ADL item was significantly higher among anticholinergic drug users independently of cognitive status (Table 3). Independent of gender, number of drugs, CIRS(CI), presence of clinically relevant neuropsychiatric disorders, MMSE score, participants affected by MCI using drugs with anticholinergic properties had higher probability to be dependent in dressing (OR: 2.81, CI95%: 1.13-6.95; p=0.025), while those with mild AD in toileting (OR: 2.01, CI95%: 1.21-3.35; p=0.007).
IADL were assessed separately for gender. In women grouping IADL according to the functional status in totally independent (IADL score = 8), partially dependent (IADL score =1-7) and totally dependent (IADL score= 0), 48 (3.2%) were totally dependent, 1049 (70.3%) were partially dependent and 395 (26.5%) were totally independent. The distribution of participants dependent in each IADL item by cognitive status are presented in Table 4 and 5, for women and men respectively. Compared with women without drug-related anticholinergic burden, those taking such drugs tended to be more dependent in each IADL item. Independent of several confounders -including number of drugs, CIRS (CI), presence of clinically relevant neuropsychiatric disorders MMSE score- only women affected by mild AD confirmed a higher probability to be dependent in preparing meals (OR: 1.66, CI95%: 1.13-2.49 p=0.013), washing (OR:1.57, CI95%: 1.03-2.38; p=0.033) and money management (OR: 1.61, CI95%: 1.10-2.37; p=0.015), while taking drugs with anticholinergic properties
In men grouping IADL according to the functional status in totally independent (IADL score = 5), partially dependent (IADL score =1-4) and totally dependent (IADL score= 0), 21 (2.4%) were totally dependent, 505 (58.2%) were partially dependent and 340 (39.2%) were totally independent. In men, the use of anticholinergic drug was associated with the presence of dependence in instrumental activity of daily living (OR: 2.00, IC95%: 1.23-3.27; p=0.005) after controlling for number of drugs, CIRS (CI), presence of almost one clinically relevant neuropsychiatric symptoms, MMSE score. The prevalence of men functionally dependent in each IADL was higher in the subgroup using anticholinergic drugs (Table 5). In particular, men with MCI taking anticholinergic drugs had a significantly higher likelihood of being impaired in shopping (OR: 3.41, CI95%: 1.33-8.73; p=0.011), and drug management (OR: 2.31, CI95%: 0.99-5.45; p=0.05).
Discussion
With this study, we explored the relationship between the use of drugs with anticholinergic properties and functional status in a large population of old age persons with intact cognitive performance, mild cognitive impairment and mild AD. The main findings are: i) 16 % of elderly subjects referring to a memory clinic take drugs with anticholinergic properties, particularly those with mild AD; ii) the use of such drugs is associated with a higher probability to be dependent on ADL, even after correction for multiple confounding factors including gender and cognitive status; iii) the use of such drugs is associated with a higher probability of IADL dependence in women affected by mild AD, and in men affected by MCI.
According to previous studies we found that a high percentage of old age persons are under treatment with drugs with anticholinergic properties. Moreover, the most users are subjects with initial cognitive impairment, such as MCI and mild AD. Among drugs with anticholinergic properties, antidepressants and antipsychotics have been linked more often with disorders due to anticholinergic activity (31). Accordingly, in our study, the most used drugs were antidepressants (mainly paroxetine and trazodone) and antipsychotics (mainly risperidone), supporting the observation that psychotropic drugs represent the major anticholinergic burden in old age population, especially among those with compromised cognitive function. Thus, the choice of a drug with higher anticholinergic effects may worsening functional impairment in old-age subjects. The preferential use of antidepressants with different mechanism of action, such as venlafaxine (a selective norepinephrine reuptake inhibitor), is likely to avoid anticholinergic side effects.
Recently Lowry and colleagues (32) demonstrated, in older hospitalized patients, that high ARS score is negatively associated with various components of Barthel Index, in particular bathing, dressing, transfers, mobility and climbing stairs. Here, analyzing in deep each ADL item, we found that the use of drugs with anticholinergic properties is associated with a statistically significant impairment in dressing in subjects with MCI and toileting in mild AD. Personal appearance is important for self-esteem and can significantly affect elderly’s desire to participate in social activities. Moreover, self-toileting is also important for maintaining self-esteem, continence and hygiene. Declines in functional abilities can lead to declines in mobility and self-care activities, leading to malnutrition (33) thus creating a vicious circle for a worse cognition and, in turn, functional status.
Since it is more likely to lose first the ability to perform complex and then the ability to perform simple activities of daily living, the IADL scale is more sensitive in detecting early functional decline. Considering that IADL scale can overemphasize tasks usually performed by women and so overestimate dependency in men, they were tested only in five items, with the exclusion of housekeeping, cooking, and doing laundry. In women, we found that the prevalence of IADL disabilities increased in users with mild AD, with meal preparation, washing and money management being the most affected items. In men, we found that the prevalence of IADL disabilities was significantly higher in subjects using anticholinergic drugs, with the higher likelihood of dependence in shopping and drug management in subjects with MCI. The reason why the use of drugs with anticholinergic properties on IADL resulted gender specific is unclear. Anticholinergic drugs act on the muscarinic receptors in central and peripheral nervous systems and inhibit acetylcholine-mediated responses by competitively binding to these receptors. Studies conducted in rats suggest that, from a diergic standpoint, the cholinergic nervous system appears to be more responsive in female than in male mammals; but, from a dimorphic standpoint, it appears to be less affected by aging in males than in females (34, 35). However, in old female rats, high-affinity binding sites were preserved in all brain regions, suggesting that the observed receptor decrease represents a loss of the low-affinity binding sites (36). In contrast, in old male rats, high-affinity binding sites were decreased and low affinity preserved. Thus, it is possible to hypothesize that drugs with anticholinergic properties are more selective for low-affinity binding sites which might explain the gender difference.
Our study has several strengths, including the relatively large number of subjects, the complete diagnostic approach and the adjustment for multiple potential confounders. Nevertheless, some limitations must be pointed out. The ReGAl project includes data from geriatric memory clinics and therefore our findings may not totally apply to the general population and to younger age groups. Moreover, due to the crosssectional design of our study, a causal relationship between anticholinergic drugs use and functional disability in subjects with MCI or mild AD can be only hypothesized. Population based longitudinal studies on BADL, IADL function and its correlates are needed to verify and extend our findings.
Implications of these findings for medical care are relevant. IADL independence is one of the defining features that distinguishes normal brain aging from MCI and dementia. Considering that impairment in IADL is a marker of increased risk of decline in cognitive performances, prescription of drugs with anticholinergic properties may significantly increase the risk of functional impairment due to deleterious effects on cognitive and physical individual domains. Thus, minimizing anticholinergic burden, choosing drugs with the same therapeutic properties but with no anticholinergic side effects, should result in improved daily functioning and quality of life, especially in a vulnerable population like MCI or mild AD. Moreover, a poorer functional performance in elderly subjects associated with the use of drugs with anticholinergic side effects might predict cognitive decline, frailty and disability, which are of major importance in geriatric assessment.
Acknowledgments: ReGAl study group: Coordinating center. Perugia, Istituto di Gerontologia e Geriatria, Dipartimento di Medicina, Universitàdi Perugia (P. Mecocci). Collecting centers: Arcugnano (VI) CRIC (C. Gabelli, A. Codemo, K. Marinelli)––Bari Cattedra di Geriatria e Gerontologia, Universitàdi Bari (A. Capurso)–– Bologna Reparto di Geriatria IV, Policlinico S. Orsola (D Cucinotta, A. Reggiani, L. Ellena)––Brescia Centro S. Giovanni di Dio-Fatebenefratelli (O. Zanetti)––Cagliari Centro Alzheimer Divisione di Geriatria, ASL 8 (P. Putzu)––Cassano delle Murge (BA) Fondazione S. Maugeri (M. Del Prete, S. Spaccamento)––Chieti Clinica Geriatrica, Università‘G. D’Annunzio’ (G. Abate, A. Di Iorio)––Dolo (VE) Centro per l’Invecchiamento Cerebrale, ULSS 13 (A. Cester, M. Formilan, F. Busonera)––Ferrara U.O. Geriatria, Azienda Ospedaliera (F. Anzivino)–– Firenze Istituto di Gerontologia e Geriatria, Universitàdi Firenze (G. Masotti, C. Cavallini, E. Mossello)–– Genova Istituto di Geriatria, Universitàdi Genova (P. Odetti, A.G. Cataldi)––Gualdo Tadino (PG) UVA ASL3 Umbria (M. Pippi)––Larino (CB) Fondazione S. Maugeri (A. Estraneo, G. Sica)––Lecce Ambulatorio Demenze (S. Renna)––Messina Cattedra di Gerontologia e Geriatria, Universitàdi Messina (V. Nicita-Mauro, G. Basile)––Modena Geriatria Universitàdi Modena e Reggio Emilia (G. Salvioli, C. Mussi, S. Ascari)––Montescano (PV) Fondazione S. Maugeri (R. Casale, G. Frazzitta)––Napoli ASL 1, Dipartimento Assistenza Anziani (M. Scognamiglio, A. Di Palma)––Napoli Cattedra di Geriatria, UniversitàFederico II (F. Rengo, V. Canonico, F. Fortunato)–– Padova Clinica Geriatrica Universitàdi Padova (G. Enzi)–– Palermo AUSL 6, Centro Regionale Demenze (M. Giordano, T. Vitrano Catania)––Pavia Istituto Gerontologia e Geriatria, Universitàdi Pavia (E. Ferrari, G. Cuzzoni)––Pescara Centro Alzheimer, U.O. Geriatria (M.L. Del Re, G. Guizzardi)–– Pistoia U.O. Geriatria, Azienda ULS 3 (C. Biagini)— Prato U.O. Geriatria, Azienda USL 4 (A. Bavazzano)–– Reggio Emilia Ambulatorio neurogeriatrico ASMN (A. Ferrari, A. Dallari)––Roma CEMI, UniversitàCattolica del Sacro Cuore (P. Carbonin, R. Bernabei, M.C. Silveri)––Roma U.O. Geriatria, Azienda USL RM/C, Ospedale S. Eugenio (L. Bartorelli, B. Gandolfi)––S. Felice a Cancello (CE) U.O. Geriatria e Lungodegenti (R. Cerqua)––San Giovanni Rotondo (FG) U.O. Geriatria, IRCSS ‘Casa Sollievo della Sofferenza’ (A. Pilotto, L. Cascavilla)–– Terni U.O. Geriatrica Le Grazie (A. Chiaranti, M. Marinelli)–– Trapani U.O. Alzheimer (G. Tripi)––Treviso U.O.S. Dipartimentale disturbi cognitivi e della memoria, Azienda ULSS 9 (M. Gallucci)––Veruno (NO) Fondazione S. Maugeri (C. Marchetti, V. Masiello, D. Sacco)––Villasanta (MI) RSA Villa San Clemente (G. Ricci).
Conflict of interest: The authors have no support or funding to report and declare no conflict of interest.
Ethical Standards: All experimental procedures were conducted in accordance with the guidelines in the Declaration of Helsinki and approved by the Ethics Committee of the University of Perugia.
References
World Health Organization. ICF: International Classification of Functioning, Disability and Health. Geneva, Switzerland: World Health Organization; 2001.
Fried LP, Guralnik JM. Disability in older adults: Evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997; 45: 92–100.
Peron EP, Gray SL, Hanlon JT. Medication Use and Functional Status Decline in Older Adults: A Narrative Review. Am J Geriatr Pharmacother. 2011; 9: 378–391.
Ferrucci L, Guralnik JM, Studenski S et al. for the Interventions on Frailty Working Group. Designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons: A consensus report. J Am Geriatr Soc. 2004; 52: 625–634.
Cutler DM. Declining diability among the elderly. Health Affairs. 2001; 20: 11–27.
Stuck AE, Walthert JM, Nikolaus T et al. Risk factors for functional status decline in community-living elderly people: A systematic literature review. Social Sci Med. 1999; 48: 445–469
Gray SL, Anderson ML, Dublin S et al. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Intern Med. 2015; 175: 401–407
Collamati A, Martone AM, Poscia A et al. Anticholinergic drugs and negative outcomes in the older population: from biological plausibility to clinical evidence. Aging Clin Exp Res. 2015. 2016; 28: 25–35
Rudolph JL, Salow MJ, Angelini MC et al. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008; 168: 508–513.
Han L, Agostini JV, Allore HG. Cumulative anticholinergic exposure is associated with poor memory and executive function in older men. J Am Geriatr Soc 2008; 56: 2203–2210.
Pasina L, Djade CD, Lucca U et al. Association of anticholinergic burden with cognitive and functional status in a cohort of hospitalized elderly: comparison of the anticholinergic cognitive burden scale and anticholinergic risk scale: results from the REPOSI study. Drugs Aging 2013; 30: 103–112.
Landi F, Russo A, Liperoti R et al. Anticholinergic drugs and physical function among frail elderly population. Clin Pharmacol Ther. 2007; 81: 235–241.
Landi F, Dell’Aquila G, Collamati A et al. Anticholinergic drug use and negative outcomes among the frail elderly population living in a nursing home. J Am Med Dir Assoc. 2014; 15: 825–829.
Mariani E, Monastero R, Ercolani S, et al for ReGAl Study Group. Influence of comorbidity and cognitive status on instrumental activities of daily living in amnestic mild cognitive impairment: results from the ReGAl project. Int J Geriatr Psychiatry. 2008; 23: 523–530.
Folstein M, Folstein S, McHugh PR. ‘Mini-mental state’: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–198.
Hughes CP, Berg L, Danziger WL, et al. A new clinical scale for the staging of dementia. Br J Psychiatry 1982; 140: 566–572.
Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. In: Brink TL, editor. Clinical Gerontology: A Guide to Assessment and Intervention. New York: The Haworth Press; 1986; 165–173.
Cummings JL. The Neuropsychiatric Inventory: assessing psychopathology in dementia patients. Neurology. 1997; 48:S10–6.
Parmelee PA, Thuras PD, Katz IR et al. Validation of the Cumulative Illness Rating Scale in a geriatric residential population. J Am Geriatr Soc 1995; 43: 130–137.
Conwell Y, Forbes NT, Cox C et al. Validation of a measure of physical illness burden at autopsy: the Cumulative Illness Rating Scale. J Am Geriatr Soc 1993; 41: 38–41
Nagaratnam N, Gayagay G. Scale (CIRS) in hospitalized nonagenarians. Arch Gerontol Geriatr 2007; 44: 29–36.
Tabert MH, Albert SM, Borukhova-Milov L, et al. Functional deficits in patients with mild cognitive impairment: prediction of AD. Neurology 2002; 58: 758–764.
Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963; 185: 914–919.
Lawton MP, Brody EM. Assessment of older people: self maintaining and instrumental activities of daily living. Gerontologist 1969; 9: 179–186
Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs 2008; 108: 52–62.
Magni E, Binetti G, Bianchetti A, Rozzini R, Trabucchi M. Mini-Mental State Examination: a normative study in Italian elderly population. Eur J Neurol. 1996; 3: 198–202.
Petersen RC, Doody R, Kurz A, et al. Current concepts in mild cognitive impairment. Arch Neurol 2001; 58: 1985–1992.
Petersen RC, O’Brien J. Mild Cognitive Impairment should be considered for DSMV. J Geriatr Psychiatry Neurol 2006; 19: 147–154.
McKhann G, Drachman D, Folstein M et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of the Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology, 1984; 39: 939–944
Knüppel S, Stang A. DAG program: identifying minimal sufficient adjustment sets. Epidemiology 2010; 21:159
Mintzer J, Burns A. Anticholinergic side-effects of drugs in elderly people. J R Soc Med. 2000; 93: 457–462
Lowry E, Woodman R, Soiza R et al. Drug Burden Index, physical function, and adverse outcomes in older hospitalized patients. J ClinPharmacol 2012; 52: 1584–1591
Chen LY, Liu LK, Hwang AC, Lin MH, Peng LN, Chen LK, Lan CF, Chang PL. Impact of Malnutrition on Physical, Cognitive Function and Mortality among Older Men Living in Veteran Homes by Minimum Data Set: A Prospective Cohort Study in Taiwan. J Nutr Health Aging. 2016; 20: 41–47.
Daulatzai MA. Early stages of pathogenesis in memory impairment during normal senescence and Alzheimer’s disease. J AlzheimersDis. 2010; 20: 355–367
Joseph A. Lieberman, Managing Anticholinergic Side Effects Prim Care Companion J Clin Psychiatry. 2004; 6(suppl 2): 20–23.
Gurwitz D, Egozi Y, Henis YI et al. Agonist and antagonist binding to rat brain muscarinic receptors: influence of aging Neurobiol. Aging 1987; 8: 115–122
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Boccardi, V., Baroni, M., Paolacci, L. et al. Anticholinergic burden and functional status in older people with cognitive impairment: Results from the ReGAl project. J Nutr Health Aging 21, 389–396 (2017). https://doi.org/10.1007/s12603-016-0787-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-016-0787-x