Abstract
Adequate protein intake and resistance training are effective strategies to maintain muscle mass, but the effect of their combination on metabolic profile during weight loss remains to be determined in older adults. The main objective of this study was to determine the effect of a 16-week high-protein caloric restriction combined with resistance training on chronic disease risk factors in obese older individuals with metabolic impairments. A total of 26 overweight adults aged between 60 and 75 years (BMI 32.4 ± 3.9 kg/m2) with at least 2 factors of the metabolic syndrome participated in this study and were randomized into two groups: 1) high-protein caloric restriction (HP; n= 12) and 2) high-protein caloric restriction combined with dynamic-resistance training (HP+RT; n=14). Caloric intake was reduced by 500 kcal/d in all participants and protein intake equated 25-30% of total calories (~1.4 g/kg/d). Exercise training consisted of 3 session/week of resistance training on pulley machines. Outcome measures included total and trunk fat mass (FM), total and appendicular lean body mass (LBM), fasting glucose level, lipid profile and blood pressure. Our results showed that total and trunk FM (all p<0.0001) as well as fasting glucose (p<0.0001), triglycerides (p=0.002) and total cholesterol (p=0.03) levels decreased similarly in both groups. However, total (p=0.04) and appendicular (p=0.02) LBM decreased in the HP group only. Our data show that high-protein energy restriction improves health profile of obese elderly at high risk of chronic disease but needs to be combined with resistance training to maintain LBM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is an important public health problem associated with high blood pressure, and several metabolic impairments such as hyperlipidemia, hyperinsulinemia and glucose intolerance which increase the risk of chronic diseases such as cardiovascular diseases, type 2 diabetes and cancer (1, 2).
Furthermore, aging is associated with a reduction in lean body mass and an increase in fat mass (3), particularly at the abdominal level (4), which is strongly associated with metabolic syndrome (MS), a cluster of risk factors for chronic diseases (5). Knowing that MS is also strongly associated with mortality in elderly (6), weight loss is commonly suggested to decrease fat mass and improve health profile. In fact, recommendations for the treatment of obesity in overweight or obese adults usually focus on modifications of lifestyle with reduced daily energy intake and increased energy expenditure with exercise (7).
It is now well recognized that losing 5 to 10% of the initial body weight is sufficient to improve health profile and thus reduce MS risk (8-10). However, energy restriction diets are usually associated with an important loss of lean body mass which could be detrimental in older adults who are at high risk of sarcopenia (11) and dynapenia (12). Knowing that, weight loss interventions often combined resistance training and caloric restriction in order to preserve lean body mass, especially in older individuals (13). However, Brochu et al. (14) have reported that lean body mass was not preserved by resistance training after a 6-month weight loss intervention in obese aging women, suggesting that resistance training per se is not sufficient to prevent the decline in lean body mass in energy-restricted aging women.
On the other hand, it was previously demonstrated that combining resistance training and appropriate protein supplementation could improve muscle mass and strength in elderly (15, 16). Furthermore, it was also established that moderately high-protein caloric restriction (between 20 and 30% of energy intake) induce greater reductions in fat mass (17, 18) while the loss of lean body mass is attenuated in middle-aged healthy obese individuals (19, 20). Moreover, Demling et al. (21) found that hypocaloric diet with an increased protein intake combined with resistance training resulted in a significant loss of fat mass and gain of lean mass compared to a hypocaloric diet alone in middle-aged active men. Hence, the scientific literature suggests a greater effectiveness of a high-protein caloric restriction combined with resistance training for the maintenance of lean mass in healthy overweight men (21, 22) and women (20). However, the impact of such an intervention on chronic disease risk and MS factors in older obese individuals remains to be clarified. Therefore, the main objective of this study was to examine the effect of resistance training combined with high-protein caloric restriction diet on chronic disease risk factors in aging individuals with metabolic alterations.
Participants and Methods
Study design
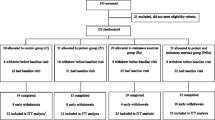
A total of 60 participants were recruited through newspaper advertisements. Among them, only 31 participants met the inclusion criteria and were randomly assigned to one of the two experimental groups: 1) high-protein caloric restriction (HP); 2) high-protein caloric restriction combined with dynamic-resistance training (HP+RT). All measurements were performed when weight was stabilized (i.e. after a 4-week weight stabilisation period) before and after the 16-week weight loss intervention. Resting metabolic rate, body composition and fasting blood samples were obtained in all participants after a 12h-overnight fast. Participants were asked to follow the caloric restriction plan that was prescribed and to not modify their physical activity habits (except for the exercise program when randomized in the HP+RT group) throughout the study. To be included in the final analyses, HP+RT group participants had to complete 85% of the exercise sessions during the 16-week intervention (i.e. 41 exercise sessions minimum). The study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures were approved by the Ethics Committee of the Geriatric Institute of the University of Sherbrooke (CSSS-IUGS). Written informed consent was obtained from all subjects before the entry in the study.
Participants
A total of 17 overweight men and 14 overweight women aged between 60 and 75 years (65.8 ± 3.1 years; BMI: 32.4 ± 3.9 kg/m2) participated in this study and had to meet the following criteria: 1) Sedentary (< 2 sessions of supervised exercise training per week), 2) non-smoker, 3) low to moderate alcohol consumption (< 15 g ethanol/d), 4) waist circumference > 102 cm for men and > 88 cm for women, 5) stable medication (no change since 6 weeks) for metabolic alterations (hyperlipidemia or hyperglycemia). Twenty-six participants completed the study (12 men and 14 women), with a dropout rate of 10.3%. Reasons for dropout included medical problems unrelated to the training program (n=2), no interest in nutrition meetings (n=2) and no reason (n=1).
Caloric restriction diet
To induce a progressive body weight loss, 500 kcal were subtracted from baseline resting metabolic rate (determined by indirect calorimetry, CCM Express system, Medgraphics Cardiorespiratory Diagnostic, Saint-Paul, MN) multiplied by a physical activity factor of 1.4 which corresponds to a sedentary state for the two groups. As resistance training performed during the study represented a modest energy cost, we did not adjust energy restriction in the HP+RT group. In average, total daily caloric intake was decreased by 433.1 ± 96.4 kcal/d in the HP group and 472.74 ± 52.5 kcal/d in the HP+RT group (p=NS). The diet macronutrient composition was 45-50 % from carbohydrates (HP: 44.7 ± 3.2 %; HP+RT: 45.1 ± 2.8 %), 25-30 % from proteins (HP: 29.2 ± 2.8 %; HP+RT: 28.5 ± 3.5 %), and 25-30 % from lipid (HP: 26.3 ± 1.8 %; HP+RT: 26.4 ± 1.9 %). A monthly dietary journal, explained by the study nutritionist, was provided to help participants follow their calorie-restricted diet. Moreover, each participant was invited to a total of 8 nutrition meetings (2/month), given by the study nutritionist, to inform them on the benefits of a healthy diet as a component of their lifestyle habits (excluding exercise training to avoid bias). Finally, each participant was invited to follow a log book that explain and represent many examples of food intake in the 6 food-times of day (breakfast, A.M snack, dinner, P.M snack, supper, and evening snack) during the diet.
Weight stabilization period
As previously performed by the MONET group (14), all participants were submitted to a 4-week weight stabilization period (body weight fluctuation < 2 kg) before and after the weight loss intervention. At baseline, participants were asked to maintain normal activity level and eating habits for 4 weeks. After the intervention, 350-400 kcal from lipids and carbohydrates were added to the caloric restriction plan by the nutritionist in order to stabilize the weight. Before and after the intervention, weekly weighing was performed during the 4-week weight stabilization period at the research unit to verify the weight maintenance. The purpose of this strategy is to stabilize the metabolic variables of interest that could be altered by important body weight fluctuations (± 2 kg).
High animal protein intake
To increase protein intake, 25-30 g of animal protein was added to each caloric restriction plan by the study nutritionist. To ensure compliance, half of the protein intake had to come from meat and alternatives. Therefore, a food guide with several examples of easy 12g-protein snacks (e.g. milkshake and chocolate milk recipes), specially created by the nutritionist for this study, was provided and explained to each participant. The HP+RT group was asked to consume a 12g-protein snack within the 2 hours following the training session.
Exercise intervention
During the 16-week intervention, participants in the HP+RT group attended the exercise laboratory on 3 non-consecutive days per week. Resistance training consisted of a 5-min warm-up and 5-min cool-down period of low-intensity stationary cycling or treadmill walking and ~45 min of moderate-intensity resistance training using dynamic exercises performed on weighted pulley machines (Life fitness, Canada). Resistance was set at 70-80% of each individual’s one repetition maximum (1-RM) for upper body exercises and at 65-70% of 1-RM for lower body exercises. The 1-RM was defined as the maximum amount of resistance that could be moved through the full range of motion of an exercise for no more than one repetition. All subjects followed an individually monitored and supervised progressive resistance training program. For the two first months, 8 different exercises were used and another 8 different exercises for the last two months. Two sets of 8–12 repetitions for upper body exercises and two sets of 12-15 repetitions for lower body exercises with a 1-2 minutes rest between sets were performed at each training session. The weight loading was progressively increased for each exercise after subjects had successfully achieved two sets of 12 repetitions with appropriate technique. To individualize each resistance training program, a 1-RM was determined before and after 8 weeks of training for the HP+RT group. Resistance training was conducted at the laboratory under the exercise specialists (kinesiologists) supervision.
Anthropometry, body composition and resting blood pressure
As previously described (23), body weight was measured to the nearest 0.1 kg using an electronic scale (model 707, SECA, Hamburg, Germany). Height was determined using a wall-mounted stadiometer while standing straight. Waist circumference was measured at the midpoint between the costal inferior border and the iliac crest using an adequate length measuring tape. BMI was calculated using the following equation: body weight (kg)/height (m)2. Total, trunk and appendicular fat mass (FM) as well as total and appendicular lean body mass (LBM) were measured using dual-energy x-ray absorptiometry (DXA, Lunar Prodigy; GE Medicals, Madison, WI). Visceral FM was estimated using the equation of Bertin (24). DXA calibration was performed every two day with a standard phantom. Coefficients of variation in our laboratory, for repeated measures (1 week apart) of FM and LBM in 10 adults, are 0.9% and 0.5%, respectively.
Resting blood pressure
Resting systolic and diastolic blood pressures were taken when participants were lying, with both arms relaxed and supported, after a rest period of at least 10 minutes, with an automatic standardized blood pressure monitor (Welch Allyn Canada Ltd., Mississauga, Ontario, Canada).
Resting metabolic rate
Resting metabolic rate (RMR) was measured using a breathing mask by indirect calorimetry (CCM Express system, Medgraphics Corporation, St Paul, MN, USA) and assessed after a 12h fast, in the early morning. Measurement lasted 30 min, with the participant lying comfortably on their back. The first 10 min were used to allow the subject to familiarise with the equipment and environment and were thus discarded from analyses as well as the last 5 minutes that were considered invalid because of the anticipation of the end of the test. Resting metabolic rate (kcal/d), used for the caloric restriction plan, was then calculated using the remaining 15 min. Test–retest measures of RMR in ten adults, with a 1-week interval, yielded a mean absolute CV of 2.1 % in our laboratory.
Lipid profile and glucose metabolism
Blood samples were drawn after a 12-hour overnight fast from an antecubital vein by an experimented research nurse. Fasting lipid profile (triglycerides, total cholesterol, HDL- and LDL-cholesterol) as well as glucose levels were analyzed at the Sherbrooke University Hospital Center (CHUS) by enzymatic and immunologic method.
Dietary intake
As previously described, subjects were asked to complete a 3-day dietary record before and after the study (23). Daily energy and macronutrient intakes were analyzed using Nutrifiq software (Laval University, Québec).
Statistical analysis
Normality of each variable of interest was assessed using the Kolmogorov-Smirnov test. Results are given as means ± standard deviation (SD) in tables and means ± standard error of the mean (SEM) in figures. Between-group comparisons and sex differences at baseline were verified with one-way analysis of variance. A two factors (group and time) repeated measures ANOVA were performed to verify the effect of 16 weeks of high-protein caloric restriction diet alone (HP) or combined with resistance training (HP+RT) in all participants. When a Time X Group interaction was significant, a dependent T test was performed in each group. Secondary analyses were made to verify if there was an influence of sex by using a three factors (group, sex and time) repeated measures ANOVA. When a Time X Sex interaction was significant, a dependent T test was performed in each sex whereas false discovery rate-corrected pairwise comparisons were performed if a Time X Group X Sex interaction was significant. All analyzes were performed using SPSS 21.0 program for windows (SPSS, Chicago, IL). Statistical significance was set at p ≤ 0.05.
Results
Baseline characteristics of both intervention groups and sex differences
As shown in Table 1, there was no significant difference between groups (HP and HP+RT) at baseline. As expected, our analyses revealed sex differences for total body weight (men: 96.3 ± 7.7 kg; women: 77.6 ± 8.2 kg; p<0.0001), waist circumference (men: 113.9 ± 8.9 cm; women: 102.7 ± 6.9 cm; p<0.001), appendicular FM (men: 11.5 ± 2.7 kg; women: 15.8 ± 4.0 kg; p=0.003), total LBM (men: 59.1 ± 3.8 kg; women: 39.7 ± 3.9 kg; p<0.0001) and appendicular LBM (men: 27.3 ± 2.1 kg; women: 18.0 ± 1.9 kg; p<0.0001). Moreover, while fasting glucose levels were higher in men (men: 5.9 ± 1.0 mmol/L; women: 5.1 ± 0.6 mmol/L; p=0.02), total cholesterol (men: 3.8 ± 0.7 mmol/L; women: 5.2 ± 1.0 mmol/L; p<0.0001), LDL-C (men: 2.0 ± 0.6 mmol/L; women: 3.1 ± 0.2 mmol/L; p<0.0001) and HDL-C (men: 1.1 ± 0.2 mmol/L; women: 1.4 ± 0.2 mmol/L; p=0.001) levels were higher in women. Also, as usually observed, total energy intake was higher in men (men: 2433.5 ± 479.6 kcal/d; women: 1924.5 ± 390.5 kcal/d; p=0.004), with greater lipid (men: 90.7 ± 20.9 g; women: 72.7 ± 21.1 g; p=0.02) and carbohydrate (men: 292.3 ± 73.7 g; women: 224.0 ± 52.4 g; p=0.01) intake. RMR and estimated total energy expenditure was similar between group (p=0.21) but higher in men (p<0.0001). Finally, we observed a sex by group interaction for lipid intake at baseline which indicated that men in the HP group consumed more lipids than women in the HP group (p=0.01).
Effect of high-protein caloric restriction diet alone or combined with dynamic resistance training on anthropometry and body composition
Table 2 shows that total body weight, BMI, total, trunk and appendicular FM (all p<0.0001) decreased in all participants, irrespective of the group intervention (HP or HP+RT). Analyses for sex differences revealed that waist circumference decreased in men (-8.15 ± 8.88 cm; p=0.009) but remained unchanged in women (-1.96 ± 8.57 cm; p=0.41), irrespective of the group (HP or HP+RT). However, visceral FM remained unchanged after the intervention (p=0.18) in all participants. Finally, as shown in Figure 1, while appendicular LBM slightly decreased in HP group (p=0.02, it remained stable in HP+RT group (p=0.15).
Effect of high-protein caloric restriction diet alone or combined with dynamic resistance training on metabolic profile
As shown in Figure 2, fasting glucose (p<0.0001), triglycerides (p=0.002) and total cholesterol (p=0.035) levels were reduced in all participants, irrespective of the group intervention or sex (p≥0.14). RMR and estimated energy expenditure remained unchanged irrespective of the groups (all p>0.40). Moreover, systolic and diastolic blood pressure also decreased similarly in both groups (p=0.04 and p=0.007, respectively). While LDL-C remained unchanged (p>0.14), a time by sex interaction indicated that change in HDL-C was different between men and women. In fact, our analyses showed that HDL-C has increased in men only (p=0.04).
Discussion
The main objective of the present study was to examine the effect of high-protein caloric restriction diet alone or combined with dynamic resistance training on chronic disease risk factors in obese older individuals with metabolic impairments. After the 16-week weight loss program, FM and metabolic profile were improved in both groups similarly, although appendicular LBM was maintained in the HP+RT group only. Interestingly, apart from a few differences between men and women, the response to the intervention appears to be broadly similar.
Although we did not observe any baseline differences between groups because of the randomization, we reported several differences between men and women. As expected, despite a similar BMI, waist circumference, appendicular FM as well as total and appendicular LBM were greater in men compared to women. Interestingly, overweight men were characterized by a better lipid profile at baseline, which could be attributed to different factors. In fact, although older men and women had the same absolute FM at baseline, relative total and trunk FM were higher in women compared to men (data not shown), suggesting that older obese women with metabolic alterations exhibit a worst health profile and thus a higher risk of chronic diseases than BMI- and age-matched men. Our results are consistent with the literature demonstrating that women after menopause have an increased abdominal FM leading to a higher risk of chronic diseases (25, 26).
It should be noted that since all participants had metabolic impairments at baseline, some of them were taking drugs such as statins. More specifically, we noticed that only 4 women were using statins whereas all men who completed the study were taking this lipid-lowering drug. Statins are the most efficient class of lipid-lowering drug (27, 28) and the most widely prescribed in elderly (29). Hence, greater statin use, in addition to lower trunk FM, may explain the better lipid profile observed in men.
On the other hand, we also observed higher fasting glucose levels in men compared to women before the intervention. Recently, we demonstrated that a high muscle mass could be detrimental for insulin sensitivity in sedentary older adults (30, 31). In this context, the higher LBM observed in men could be associated with a reduced insulin sensitivity, which could, in turn, lead to greater fasting glucose levels. The positive correlation between LBM and glucose levels at baseline (r=0.45, p=0.01, data not shown) supports this hypothesis.
Finally, although similar between experimental groups (HP and HP+RT), it is interesting to note that all participants had a protein intake close to 1.1 g/kg/day before the high-protein caloric restriction, which is higher than the current Recommended Dietary Allowances (RDAs; 0.8 g/kg/day) for this population. In this context, the addition of 25 g of dietary protein per day has led to an increase of close to 1.4 g/kg/day of protein, which was previously recommended to prevent progressive muscle mass loss in elderly (32-35).
Albeit the weight loss intervention diminished waist circumference in men only, total body weight and BMI, as well as trunk, appendicular and total body FM decreased in all participants. These results demonstrate that high-protein caloric restriction alone or combined with resistance training is an efficient strategy to reduce body weight (≈ 6.1 %) and FM in both men and women (≈ 13.8 %). Therefore, whereas 20 individuals had a BMI greater than 30 kg/m2 at baseline, only 12 remained obese after the intervention, which could reduce the risk of MS. Also, the body weight and FM losses achieved with this intervention are close to what is usually observed with standard caloric restriction in aging adults (14, 36). Hence, these results suggest that obese older adults with metabolic alterations could similarly benefit from such an intervention and thus reduce their chronic disease risk. Furthermore, our results demonstrate that appendicular LBM is maintained only when dynamic resistance training is added. This suggests that dynamic resistance training performed with pulleys modulates the effect of high-protein caloric restriction on LBM. Hence, it seems that a protein intake, consumed after the resistance training (according to the study protocol and log book), may be essential to induce additive effect. Although previous studies have demonstrated that a 20g-protein supplement is required to induce a muscle gain in the aging adults (16, 37, 38), our results show that a 12g-animal protein intake following resistance training seems sufficient to maintain appendicular LBM in a context of caloric restriction in obese elderly. Nevertheless, while our results suggest an impact of protein intake and resistance training on LBM in a context of weight loss program, it has to be mentioned that Weisgarber et al. (2015) (39) did not reported additive effect of protein supplementation and resistance training on LBM in healthy postmenopausal women. The fact that protein intake was consumed during, and not after, the resistance training as well as the absence of caloric restriction may explain this inconsistency. This difference may also reinforce the importance of consuming protein intake in the hours following resistance training to maximize protein synthesis (40), particularly in older individuals.
On the other hand, regardless of LBM changes, our results demonstrate that 6% of weight loss in response to a high-protein energy restricted diet (alone or combined with resistance training) is sufficient to reduce fasting glucose levels by 6.4 % (≈ 0.4 mmol/L), fasting triglycerides levels by 16.3 % (≈ 0.3 mmol/L), and fasting total cholesterol by 6.1 % (≈ 0.3 mmol/L), which could considerably reduce chronic disease risk especially in older individuals with metabolic impairments. Finally, systolic and diastolic blood pressures were also decreased in response to the weight loss program. These metabolic improvements were not different when resistance training was added suggesting that dynamic resistance training, and thus the maintenance of LBM, did not contribute to reduce the risk of chronic diseases in a context of weight loss. This is in agreement with a previous study from the MONET group (14) showing that resistance training does not contribute to improve metabolic profile after weight loss. Although it was previously demonstrated that aerobic training has beneficial additive effect to caloric restriction on metabolic profile (41, 42), there is less concordance between studies regarding the addition of resistance training. In fact, while we and others (14, 43) did not report any additive effect of resistance training on the metabolic profile in older individuals, Potteiger et al. (44) have shown that resistance training has additive effect on clinical risk factor profile in middle-aged men (age 27-48 years) with at least one risk factor for MS. In this study (44), participants were trained 4 times per week and had high intensity days with 4 sets of 100% of 5-7 RM alternated with a moderate intensity day (8-10 repetitions at 80% of 1 RM). Hence, it may be possible that using a dynamic resistance training performed on pulleys did not allow achieving sufficient intensity to induce an additive effect of resistance training. Therefore, the impact of progressive high-intensity resistance training requires further investigation, especially in addition to a high protein intake in older adults.
Some limitations of this study should be discussed. The post-training 12g-protein snack was not provided by the research team following the exercise session. Nevertheless, as mentioned in the methods section, a guide, explained by the nutritionist, with different examples of protein snacks was given to all participants at the beginning of the study. Another limit to this study is the prevalence of statin use difference between our male and female participants which may have biased some results. Nevertheless, this could be representative of the reality as it was recently reported that the proportion of women that used lipid-lowering drugs is lower than men (45, 46). Finally, we did not measure a biomarker for protein intake such as urinary nitrogen. In fact, this limitation is mainly due to its complexity and cost. Nevertheless, all participants were asked to record their energy intake into a log book during the intervention. Hence, this strategy allowed us to ensure compliance to the prescribed diet.
Regardless of the latter limitations, the results of the present study are strengthened by several key methodological elements. First, we used a randomized study design, which is recognized as the gold standard in clinical studies. Second, to ensure highprotein intake, we provided a guide with several examples of protein snacks as well as a monthly dietary journal (log book) to each participant. Furthermore, we used a 4-week weight stabilization period before and after the intervention to minimize the impact of body weight fluctuations on metabolic profile (47). Finally, the dynamic resistance training, performed under the supervision of kinesiologists, was executed on pulleys, which induced a greater core workload compared to standard resistance training.
Conclusion
In conclusion, this is the first study showing that moderately high-protein dietary intake (~ 1.4 g/kg/d) during energy restriction improves metabolic profile in obese older adults with metabolic impairments. However, our results show that it needs to be combined with dynamic resistance training if we want to maintain muscle mass. Knowing the increased prevalence of obesity and sarcopenia in aging individuals, this study provides significant information regarding the clinical management of obesity-induced metabolic alterations in older adults.
Conflict of Interest: None.
Acknowledgments: We sincerely thank all participants to this study as well as Martine Fisch, the research nurse, and all kinesiologists, who supervised the training sessions, for their professional support. We also thank Dre Stéphanie Chevalier for her editorial work. This study was supported by the Faculty of physical activity sciences and the Quebec Network for Research on Aging. Dre. Eléonor Riesco is the guarantor of this work, had full access to all the data, and takes full responsibility for the integrity of data and the accuracy of data analysis.
Ethical Standards: The study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures were approved by the Ethics Committee of the Geriatric Institute of the University of Sherbrooke (CSSS-IUGS). Written informed consent was obtained from all subjects before the entry in the study.
References
Pischon T, Nothlings U, Boeing H. Obesity and cancer. Proc Nutr Soc 2008;67(2):128–145.
Wahba IM, Mak RH. Obesity and obesity-initiated metabolic syndrome: mechanistic links to chronic kidney disease. Clin J Am Soc Nephrol 2007;2(3):550–562.
Ribeiro SM, Kehayias JJ. Sarcopenia and the analysis of body composition. Adv Nutr 2014;5(3):260–267.
Zamboni M, et al. Adipose tissue, diet and aging. Mech Ageing Dev 2014;136–137:129–137.
Tang M, Leidy HJ, Campbell WW. Regional, but not total, body composition changes in overweight and obese adults consuming a higher protein, energy-restricted diet are sex specific. Nutr Res 2013;33(8):629–635.
Isomaa B, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001;24(4):683–689.
Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults—The Evidence Report. National Institutes of Health. Obes Res 1998;6 Suppl 2:51S–209S.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series 2000;894:i-xii, 1-253.
Brochu M, Tchernof A, Turner AN, Ades PA, Poehlman ET. Is there a threshold of visceral fat loss that improves the metabolic profile in obese postmenopausal women? Metabolism 2003;52(5):599–604.
You T, Berman DM, Ryan AS, Nicklas BJ. Effects of hypocaloric diet and exercise training on inflammation and adipocyte lipolysis in obese postmenopausal women. The Journal of clinical endocrinology and metabolism 2004;89(4):1739–1746.
Fielding RA, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 2011;12(4):249–256.
Manini TM, Clark BC. Dynapenia and aging: an update. J Gerontol A Biol Sci Med Sci 2012;67(1):28–40.
Anton SD, et al. Effects of a weight loss plus exercise program on physical function in overweight, older women: a randomized controlled trial. Clin Interv Aging 2011;6:141–149.
Brochu M, et al. Resistance training does not contribute to improving the metabolic profile after a 6-month weight loss program in overweight and obese postmenopausal women. J Clin Endocrinol Metab 2009;94(9):3226–3233.
Cermak NM, Res PT, de Groot LC, Saris WH, van Loon LJ. Protein supplementation augments the adaptive response of skeletal muscle to resistancetype exercise training: a meta-analysis. The American journal of clinical nutrition 2012;96(6):1454–1464.
Karelis AD, Messier V, Suppere C, Briand P, Rabasa-Lhoret R. Effect of cysteinerich whey protein (immunocal(R)) supplementation in combination with resistance training on muscle strength and lean body mass in non-frail elderly subjects: a randomized, double-blind controlled study. The journal of nutrition, health & aging 2015;19(5):531–536.
Due A, Toubro S, Skov AR, Astrup A. Effect of normal-fat diets, either medium or high in protein, on body weight in overweight subjects: a randomised 1-year trial. Int J Obes Relat Metab Disord 2004;28(10):1283–1290.
Skov AR, Toubro S, Ronn B, Holm L, Astrup A. Randomized trial on protein vs carbohydrate in ad libitum fat reduced diet for the treatment of obesity. Int J Obes Relat Metab Disord 1999;23(5):528–536.
Farnsworth E, et al. Effect of a high-protein, energy-restricted diet on body composition, glycemic control, and lipid concentrations in overweight and obese hyperinsulinemic men and women. Am J Clin Nutr 2003;78(1):31–39.
Layman DK, et al. A reduced ratio of dietary carbohydrate to protein improves body composition and blood lipid profiles during weight loss in adult women. J Nutr 2003;133(2):411–417.
Demling RH, DeSanti L. Effect of a hypocaloric diet, increased protein intake and resistance training on lean mass gains and fat mass loss in overweight police officers. Ann Nutr Metab 2000;44(1):21–29.
Villareal DT, Banks M, Sinacore DR, Siener C, Klein S. Effect of weight loss and exercise on frailty in obese older adults. Arch Intern Med 2006;166(8):860–866.
Riesco E, et al. Effect of exercise training combined with phytoestrogens on adipokines and C-reactive protein in postmenopausal women: a randomized trial. Metabolism 2012;61(2):273–280.
Bertin E, Marcus C, Ruiz JC, Eschard JP, Leutenegger M. Measurement of visceral adipose tissue by DXA combined with anthropometry in obese humans. Int J Obes Relat Metab Disord 2000;24(3):263–270.
Abad-Diez JM, et al. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr 2014;14:75.
Kim IH, Chun H, Kwon JW. Gender differences in the effect of obesity on chronic diseases among the elderly Koreans. J Korean Med Sci 2011;26(2):250–257.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285(19):2486–2497.
Furberg CD. Natural statins and stroke risk. Circulation 1999;99(2):185–188.
Grundy SM. Can statins cause chronic low-grade myopathy? Ann Intern Med 2002;137(7):617–618.
Barsalani R, Brochu M, Dionne IJ. Is there a skeletal muscle mass threshold associated with the deterioration of insulin sensitivity in sedentary lean to obese postmenopausal women? Diabetes Res Clin Pract 2013;102(2):123–128.
Lebon J, et al. Is a small muscle mass index really detrimental for insulin sensitivity in postmenopausal women of various body composition status? J Musculoskelet Neuronal Interact 2012;12(3):116–126.
Elango R, Humayun MA, Ball RO, Pencharz PB. Evidence that protein requirements have been significantly underestimated. Curr Opin Clin Nutr Metab Care 2010;13(1):52–57.
Gaffney-Stomberg E, Insogna KL, Rodriguez NR, Kerstetter JE. Increasing dietary protein requirements in elderly people for optimal muscle and bone health. J Am Geriatr Soc 2009;57(6):1073–1079.
Paddon-Jones D, Short KR, Campbell WW, Volpi E, Wolfe RR. Role of dietary protein in the sarcopenia of aging. Am J Clin Nutr 2008;87(5):1562S–1566S.
Wolfe RR, Miller SL, Miller KB. Optimal protein intake in the elderly. Clin Nutr 2008;27(5):675–684.
Lau DC, et al. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ 2007;176(8):S1–13.
Pennings B, et al. Amino acid absorption and subsequent muscle protein accretion following graded intakes of whey protein in elderly men. Am J Physiol Endocrinol Metab 2012;302(8):E992–999.
Yang Y, et al. Resistance exercise enhances myofibrillar protein synthesis with graded intakes of whey protein in older men. Br J Nutr 2012;108(10):1780–1788.
Weisgarber KD, Candow DG, Farthing JP. Whey protein and high-volume resistance training in postmenopausal women. The journal of nutrition, health & aging 2015;19(5):511–517.
Tang JE, Phillips SM. Maximizing muscle protein anabolism: the role of protein quality. Current opinion in clinical nutrition and metabolic care 2009;12(1):66–71.
Ryan AS, et al. Aerobic exercise and weight loss reduce vascular markers of inflammation and improve insulin sensitivity in obese women. J Am Geriatr Soc 2014;62(4):607–614.
Ryan AS, et al. Aerobic exercise plus weight loss improves insulin sensitivity and increases skeletal muscle glycogen synthase activity in older men. J Gerontol A Biol Sci Med Sci 2014;69(7):790–798.
Morencos E, et al. Effects of dietary restriction combined with different exercise programs or physical activity recommendations on blood lipids in overweight adults. Nutr Hosp 2012;27(6):1916–1927.
Potteiger JA, et al. Resistance exercise and aerobic exercise when paired with dietary energy restriction both reduce the clinical components of metabolic syndrome in previously physically inactive males. Eur J Appl Physiol 2012;112(6):2035–2044.
Koopman C, et al. Persisting gender differences and attenuating age differences in cardiovascular drug use for prevention and treatment of coronary heart disease, 1998-2010. Eur Heart J 2013;34(41):3198–3205.
Robinson JG, Booth B. Statin use and lipid levels in older adults: National Health and Nutrition Examination Survey, 2001 to 2006. J Clin Lipidol 2010;4(6):483–490.
Weinsier RL, et al. Do adaptive changes in metabolic rate favor weight regain in weight-reduced individuals? An examination of the set-point theory. Am J Clin Nutr 2000;72(5):1088–1094.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amamou, T., Normandin, E., Pouliot, J. et al. Effect of a high-protein energy-restricted diet combined with resistance training on metabolic profile in older individuals with metabolic impairments. J Nutr Health Aging 21, 67–74 (2017). https://doi.org/10.1007/s12603-016-0760-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-016-0760-8