Abstract
Objective
To review the literature on epidemiology and postoperative outcomes particularly surgical, functional and quality of life of atypical femoral fractures (AFFs) in the older population (aged ≥65 years) using the first and second American Society of Bone Mineral Research (ASBMR) Task Force consensus definition.
Methods
Electronic search for articles on AFFs and bisphosphonates published in English was performed. Eligible studies were reviewed systematically in relation to (a) the epidemiology of AFFs in older people and (b) postoperative outcomes of AFFs.
Results
Twenty-three studies on AFFs were included: 14 on epidemiology and 11 on treatment outcomes (two articles reported on both aspects). The epidemiological studies showed that the incidence of AFFs is low (3.0-9.8 per 100,000 person-years) but relative risk increased with longer duration of bisphosphonates use, especially after more than three years. Most cases of AFFs occurred in older people aged 65 years and above. However, in six studies, the mean age of patients with bisphosphonate-related AFFs is younger than those with typical proximal femoral fractures (mean age range of 66–75 years versus 75-89 years respectively). Varying postoperative and functional outcomes have been reported but differences in study population, management approaches and endpoints may account for these variations. For incomplete AFFs, prophylactic surgical intervention is potentially beneficial.
Conclusion
The benefits of bisphosphonates in reducing osteoporotic fractures still outweigh the risk of AFFs in view of its low absolute risk, when the ASBMR Task Force criteria for this type of fracture were applied. The risk of AFFs in different age groups is not well defined but tends to affect the younger patients more (aged <65 years) as compared to the older population (aged ≥65 years). Evidence supporting different types of treatment in AFFs such as intramedullary or extramedullary surgical devices and the use of teriparatide, a parathyroid hormone analogue, is not yet well established.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major contributor of fragility fractures leading to a significant burden to both individuals and health service providers, with hip fractures accounting for an estimated $1.6 billion in total direct cost in Australia alone (1). Hip fractures contribute to increased morbidity, functional decline and premature death (2, 3). The prevalence of osteoporosis is expected to increase with population ageing. As a result, osteoporosis prevention and treatment is a priority as a means to reduce the detrimental societal and health care impact of fragility fractures.
Clinical trials provide evidence for the effectiveness of bisphosphonates in reducing the risk of vertebral, nonvertebral and hip fractures in postmenopausal women and older men with osteoporosis (4). Bisphosphonates use has grown due to the increased number of people diagnosed with osteoporosis (1). Bisphosphonates are generally well tolerated and the rate of adverse effects is usually low, ranging from milder but more frequent gastrointestinal symptoms to the more serious but rare osteonecrosis of the jaw, more commonly seen with higher doses of intravenous bisphosphonate and a history of malignancy (4).
In the past decade, attention has shifted towards the association between atypical femoral fractures (AFFs) and long-term bisphosphonates therapy (5-8). Concerns have been raised as to whether the frequency of AFFs may rise due to population ageing as increasing number of older adults will be prescribed bisphosphonates for osteoporosis management. In 2010, the American Society for Bone and Mineral Research (ASBMR) Task Force published a consensus to define AFFs allowing for a more standardized approach in reporting the epidemiology of AFFs (7). A revised definition was published in 2014 where it was determined that AFFs must be located distal to the lesser trochanter and proximal to the supracondylar region of the distal femur (8). The revised criteria also included the following: (a) no history or low-energy trauma (fall from standing height); (b) the fracture must originate at the lateral cortex, is transverse or short oblique in configuration; (c) there is minimal or no evidence of comminution; (d) fracture line extend through both cortices in complete fracture or, in incomplete fracture, involves only one side of the lateral cortex; and (e) presence of periosteal or endosteal thickening on the lateral cortex at the fracture site, also known as “beaking” (8).
Previous systematic and narrative reviews have included studies that did not used the ASBMR Task Force definition for AFFs as well as those without radiological adjudication, resulting in wide variation in findings (9, 10). Furthermore little has been reported in the literature on the outcomes of patients after sustaining an AFF. The aims of this systematic review are (a) to describe the epidemiology of AFFs in older adults (aged 65 years and above) using the ASBMR task force definition and (b) to examine the postoperative outcomes related to treatment of AFFs. This review will also provide relevant information required by clinicians to support discussions and decision making with osteoporotic patients.
Methods
Search Strategy
We searched MEDLINE, MEDLINE In Process and Non Indexed Citations, EMBASE, Cochrane and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases with the following key words: ‘atypical femoral fractures’, ‘subtrochanteric fractures’, ‘femoral shaft fractures’ AND ‘bisphosphonates’ (January 2003 – December 2014). Searches were limited to publications in the English language. Initial search was limited to 65 years of age and above but this yielded only three relevant articles, hence the age limit criterion was removed. Relevant references from articles identified through the search were also reviewed to allow for a more comprehensive identification.
Selection Criteria
Studies were selected for review if they met the following criteria: (a) adhered to the first or second ASBMR consensus definition for AFFs with radiological adjudication; and (b) reported on epidemiology and/or postoperative outcomes. Studies in the setting of high-impact traumatic femoral, neck of femur and intertrochanteric fractures; pathological fractures in the setting of malignancy; fractures associated with metabolic bone disease except for osteoporosis; and atypical non-femoral fractures were excluded. This review included prospective or retrospective cohort studies, case-control studies and randomized controlled trials. Case reports, case series, review articles, editorials and letters were excluded.
Data Synthesis
Data on the epidemiology of AFFs and postoperative outcomes were gathered and categorized separately. For the epidemiological studies, the association between AFFs and bisphosphonates use was examined. Data on baseline demographics (age, gender and ethnicity), type of bisphosphonates and duration of use were collected. For studies on postoperative outcomes of AFFs, outcomes related to surgery, functional outcomes and quality of life were analysed.
Quality Assessment
The studies included were rated using the Modified Joanna Briggs Institute Quality Assessment and Review Instrument Checklist which comprises of 10 questions with answers as yes, no or unclear, giving a score out of 10 (11). Only answers of yes were included in the overall quality score. Studies with scores of 7 or above were classified as credible, between 4 to 6 as equivocal and 3 or below as poor. Only studies with score of 7 and above were included.
Results
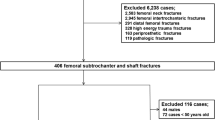
The initial electronic search identified 96 articles and 12 additional articles obtained from references cited in these studies. Figure 1 summarizes the search and selection process. After the removal of ten duplicates, 98 articles were identified. Seventy-five articles that did not meet inclusion criteria were excluded. A total of 23 articles were reviewed. Finally 14 studies were on epidemiology and 11 on treatment outcomes (two covered both aspects).
The epidemiology of AFFs
In total, 14 studies reported on epidemiology of AFFs. They were divided into two subgroups using either: (a) the first ASBMR definition (n = 10) (12-21) or (b) the second ASBMR definition (n = 4) (22-25) (Table 1). Seven were retrospective case-control studies, six were retrospective cohort studies and one used combined data from three prospective registries (Table 1). The number of AFFs in each study has ranged from 6 to 143 fractures, indicating a large variability in the size of cohorts with these fractures. In these studies, a total of 511 patients with AFFs were included. Studies using the second definition were generally smaller than those that used the first.
The overall incidence of AFFs in the general population is low with studies reporting an incidence between 3.0 and 9.8 per 100,000 person-years (Table 1) (14-16, 23). One study in Norway which included periprosthetic fractures showed a mean incidence of 9.8 per 100,000 person-years (95% CI 5.2-14.5) amongst women aged ≥65 years (23). Using the first ASBMR definition, the prevalence of AFFs accounted for only 0.2-0.8% of total hip fractures and 3.5-30.3% of subtrochanteric and femoral shaft fractures (13, 17-20). Similarly, three studies using the revised ASBMR definition reported a low prevalence of AFFs, estimated to be 0.63% of total hip fractures and 3.5-5.7% of subtrochanteric and femoral shaft fractures (22, 24, 25).
In all studies except for one, the mean age of patients with AFFs were reported to be above 65 years (Table 1) (12-25). Amongst these studies, six retrospective case-control studies showed that patients with bisphosphonate-related AFFs were younger than patients with typical proximal femoral fractures (TPFFs) (mean age range of 66–75 years versus 75-89 years respectively), at the time of fracture (12-15, 19, 22). However, these studies did not perform statistical comparison of the age differences between groups. The mean duration of bisphosphonate therapy in the AFFs group ranged between 3.75 and 6 years and the proportion of patients with typical fractures taking bisphosphonates was small, ranging from 3.8% to 9.9%. Similarly, one observational cohort study observed that the mean age of patients with bisphosphonate-related AFFs is also younger than bisphosphonate naïve typical proximal femoral fractures (67.5 ± 9.6 versus 78.4 ± 13.9 years; p <0.001) (21). However one study found no mean age difference, 80 years compared with 81 years in AFFs and TPFFs respectively (19). Although AFFs tend to occur in older adults of relatively younger age as compared to those with TPFFs, these fractures were diagnosed mostly among those aged 65 years and above.
Increased risk of AFFs have been associated with bisphosphonates use, predominantly alendronate, risedronate and zoledronic acid (12-18) and four studies reported that the risk increased with duration of bisphosphonates therapy (Table 1) (13, 15, 16, 24). Only two studies did not observe any association because the investigators were unable to determine the duration of bisphosphonates therapy (19, 20). Meier et al. reported odds ratio (OR) of 35.1 (95% CI 10–123.6) with <2 years of exposure, increasing to 117.1 (95% CI 34.2–401.7) for 5–9 years of exposure (15). Similarly, Dell et al. reported an age-adjusted incidence rate of 1.78 per 100,000 person-years with <2 years of exposure and 113.1 per 100,000 person-years for up to 9 years of exposure (16).
In majority of the studies, there was a predominance of female patients who sustained AFFs. In 12 studies (n = 440), 90% of AFFs occurred in females (Table 1) (13-19, 21, 22, 24, 25). Marcano et al. reported that Asians were found to be at a higher risk of bisphosphonate-related AFFs after conducting a multivariate analysis but this has only been observed so far in this single study (21).
Treatment outcomes
Table 2 and 3 summarize eleven studies that evaluated the postoperative outcomes of patients with complete and incomplete AFFs who were treated surgically (17, 23, 26-34). Two studies examined the role of teriparatide postoperatively (29, 31). Seven studies were retrospective cohort studies (23, 26, 28, 30-32, 34), three were retrospective case-control studies (17, 27, 33) and one was a prospective case-control study (29). All studies had small sample sizes with less than 35 patients.
For complete AFFs, six studies involved surgical intervention (Table 2) (17, 23, 26-28, 30); five looked at both intramedullary (IM) nailing and extramedullary (EM) devices such as plate and screws (17, 23, 26, 27, 30) and one study included only IM nailing (28). All were retrospective studies and results were mixed. IM nailing has a more favourable surgical outcome as compared to EM devices as showe in Teo et al. where in the IM nailing cohort, 11.1% had implant failure and 22.2% had revision surgery compared to 29% had implants failure and 38% had revision surgery with EM devices (30). Two studies reported a delayed healing time (mean of 10 months) (28, 30).
As for postoperative functional outcomes, four studies assessed post-operative mobility and ability to perform activities of daily living after fixation of complete AFFs over a mean follow-up period of 12 to 40.5 months (17, 23, 28, 30). The group that had IM nailing reported better functional outcomes, as seen by Egol et al. where 64% reported return to baseline function and 66% reported pain free at 12 months (28). Shkolnikova et al. followed 16 AFFs patients up to 46 months and 64% reported a functional decline, majority of them had EM devices (17). Meling et al. also reported nine patients (10 AFFs) were reviewed at a mean follow-up of 36.5 months (range: 10 to 104) and was associated with low mean Hip Harris Score with odds ratio (OR) 58.9 (95% CI 4.74-70.4) and mean Timed Up and Go test of 25.7 s (95% CI 12.7-38.8) (23).
Table 3 summarizes the studies that examined the role of prophylactic surgical nailing for incomplete AFFs. When compared to conservative management, prophylactic nailing has been found to be associated with shorter hospital length of stay (32), reduced progression to complete fractures (32), significant improvement in pain (33) and recovery to baseline function (34). Banffy et al. treated six patients with incomplete AFFs conservatively and five of these patients progressed to complete fractures requiring surgical intervention, as compared to six with prophylactic nailing, and none progressed to complete fracture and all had radiographic union (32).
The outcomes with the use of teriparatide in the postoperative management of AFFs are uncertain (Tables 3). One study reported that after 6 months of daily 20 μg teriparatide administered subcutaneously to 5 patients with incomplete AFFs, there was an increase bone remodeling markers and fracture healing when compared to those treated conservatively or prophylactic nailing (29). In another study, patients with AFFs treated surgically and received daily injection of teriparatide post-surgery also had a significantly shorter fracture healing time compared to those who did not receive the drug (5.4 ± 1.5 vs. 8.6 ± 4.7 months) and a significantly lower frequency of delayed healing or non-union (p = 0.014) (31).
Discussion
The key findings from this review are a low absolute risk of AFFs overall but the relative risk increases with bisphosphonates use, especially if prolonged (more than 3 years). Other findings include a trend towards younger age at the time of presentation with AFFs compared with those with typical proximal femoral fractures, a higher preponderance of females with AFFs and a lack of evidence on effectiveness of different treatment modalities.
The incidence of AFFs is very low as demonstrated by the studies reviewed, regardless of patients’ age or whether the first or second ASBMR Task Force definitions were used. Epidemiological studies indicated that the risk of AFFs increased with the use of bisphosphonates. In the absence of good quality prospective study, no causal relationship between AFFs and bisphosphonates therapy can be established. Furthermore AFFs have been reported in bisphosphonate-naïve patients with osteoporosis (35).
It is estimated that the average population risk of hip fracture is 1% per year in postmenopausal women and for every 10,000 patients at high risk, 300 hip fractures are expected and if these patients were treated with bisphosphonates, assuming an effectiveness of 36% (relative risk of 0.64), then 108 hip fractures are avoided (36). On the other hand, three to six subtrochanteric fractures (both typical and atypical) may be expected with bisphosphonates (36). Hence, the risk–benefit ratio for using bisphosphonates in managing osteoporosis remains favourable.
The association between AFFs and bisphosphonates, however, does appear to be related to the duration of use; hence patients on longer duration of bisphosphonates (more than 3 years) are at higher risk. It is clinically important to review the need for bisphosphonates over time and consideration be given to stopping after prolonged use which can reduce the risk of AFFs by 70% per year (12). This has led to the suggestion of bisphosphonates “drug holiday,” i.e. discontinuing therapy after five years though overall risk-benefit of this approach has not been clarified (4). Therefore, it is recommended that physicians remain vigilant in assessing patients treated with bisphosphonates for the treatment or prevention of osteoporosis and patients should be advised of the potential risks.
Although most AFFs were reported in patients over the age of 65 years, those with this type of fracture tended to be younger than those who present with TPFFs. Two explanations have been postulated for this observation. Firstly, it is possible that patients with AFFs have been treated for longer periods with bisphosphonate therapy compared to those who sustained TPFFs but available studies were limited in determining the exact duration of drug exposure. Secondly, some have suggested that younger people are more likely to be involved in physical activities, placing them at higher risk of developing stress fractures at the maximal tensile loading site that is the lateral cortex of the femur where AFFs tend to occur, particularly when bisphosphonate use is also present (17).
Our review also showed that AFFs affect predominantly females. The reason behind this predominance remains unclear. It is possible that this observation reflected the higher number of postmenopausal women compared to older men who are treated with bisphosphonates (37). Incidence rate of AFFs in women have been reported (23) but not in the male population.
Further research is needed to determine the most effective method to treat complete and incomplete AFFs. Available studies conducted in small samples have shown a trend towards a more favourable outcome with IM nailing (28, 30) but controlled studies are needed to confirm this finding. Although early results are in favour of prophylactic IM nailing of incomplete AFFs in preventing progression to complete fractures and improvement in pain, randomized controlled studies are required to confirm the benefit of this approach. Similarly with teriparatide, there is still no established evidence to prove its efficacy in bone healing because only a small number of patients with AFFs have been treated with this drug.
One of the strengths of this review is the inclusion of studies using the ASBMR criteria for AFFs, which meant that a more standardised, well-defined and reproducible definition was used. Prior to the criteria, the incidence and prevalence reported varied significantly between epidemiological studies due to differences in definition. In addition, this is the first review to systematically examine the postoperative outcomes of AFFs. A meta-analysis of the findings could not be performed due to the heterogeneity in study methods and outcome measures used. However, there are limitations to this review. Firstly, nearly all of the studies were retrospective in nature, preventing any causality to be drawn in the relationship between AFFs and bisphosphonates use. Moreover, study duration has been variable (range of mean reported were 3.75 to 8.70 years) limiting the interpretation of long-term exposure to bisphosphonates. Variation in the number of AFFs and size of study population also limits the compatibility between individual studies. Secondly, the finding of AFFs affecting a comparatively younger population should be interpreted with caution because of small sample size and possible selection bias in control groups. Thirdly, methodology and outcome measures after surgery have been inconsistent and non-standardized. Little is also known about the impact on treatment outcomes in increasing age for those with AFFs because no study has evaluated patients in different age groups, especially with age being an important predictor of outcomes in other types of fractures.
In summary, this systematic review of studies using the ASBMR Task Force criteria indicates that the incidence of AFFs is low but the relative risk increases with long-term bisphosphonate use. Current evidence suggests that the benefit of bisphosphonates in reducing osteoporotic fractures still outweighs the risk of AFFs. The risk of AFFs in the older age group is less well defined but there is a trend towards the elderly being affected at a younger age compared to those with typical proximal femoral fractures, which increases in frequency with age. Little is known about the postoperative outcomes of AFFs because of differences in treatments used. Large long-term prospective studies on older adults taking bisphosphonates are needed to better define specific risk factors of AFFs in this group and guide management of osteoporosis.
Conflict of interest: P.S. has received educational grants and honoraria from Novartis Pty Australia and Amgen Pty Ltd. R.V. is on the Malnutrition in the Elderly Advisory Board, Nestle Australia. She has been part of the PROT-AGE initiative and the MNA initiative that was supported by educational grants from Nestle, Inc. The other authors have no conflict of interests to declare.
Ethical Standards: All studies included in this systematic review complied with ethical standards of their respective institutions or countries.
References
Watts J, Abimanyi-Ochom J. Osteoporosis costing all Australians. A New Burden of Disease Analysis 2012-2022.
Marks R. Hip fracture epidemiological trends, outcomes, and risk factors, 1970-2009. Int J Gen Med 2010;3:1–17.
Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc 2002;50(10):1644–1650.
McClung M, Harris ST, Miller PD, Bauer DC, Davison KS, Dian L, et al. Bisphosphonate therapy for osteoporosis: benefits, risks, and drug holiday. Am J Med 2013;126(1):13–20.
Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab 2005;90(3):1294–1301.
Giusti A, Hamdy NA, Papapoulos SE. Atypical fractures of the femur and bisphosphonate therapy: A systematic review of case/case series studies. Bone 2010;47(2):169–180.
Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2010;25(11):2267–2294.
Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the american society for bone and mineral research. J Bone Miner Res 2014;29(1):1–23.
Girgis CM, Seibel MJ. Atypical femur fractures: a review of the evidence and its implication to clinical practice. Ther Adv Musculoskelet Dis 2011;3(6):301–314.
Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: a systematic review and meta-analysis. J Bone Miner Res 2013;28(8):1729–1737.
The Joanna Briggs Institute. Joanna Briggs Institute Reviewer’s Manual: 2014 edition. 2014 edition ed: The Joanna Briggs Institute.
Schilcher J, Michaelsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med 2011;364(18):1728–1737.
Giusti A, Hamdy NA, Dekkers OM, Ramautar SR, Dijkstra S, Papapoulos SE. Atypical fractures and bisphosphonate therapy: a cohort study of patients with femoral fracture with radiographic adjudication of fracture site and features. Bone 2011;48(5):966–971.
Feldstein AC, Black D, Perrin N, Rosales AG, Friess D, Boardman D, et al. Incidence and demography of femur fractures with and without atypical features. J Bone Miner Res 2012;27(5):977–986.
Meier RP, Perneger TV, Stern R, Rizzoli R, Peter RE. Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. Arch Intern Med 2012;172(12):930–936.
Dell RM, Adams AL, Greene DF, Funahashi TT, Silverman SL, Eisemon EO, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res 2012;27(12):2544–2550.
Shkolnikova J, Flynn J, Choong P. Burden of bisphosphonate-associated femoral fractures. ANZ J Surg 2013;83(3):175–181.
Thompson RN, Phillips JR, McCauley SH, Elliott JR, Moran CG. Atypical femoral fractures and bisphosphonate treatment: experience in two large United Kingdom teaching hospitals. J Bone Joint Surg Br 2012;94(3):385–390.
Warren C, Gilchrist N, Coates M, Frampton C, Helmore J, McKie J, et al. Atypical subtrochanteric fractures, bisphosphonates, blinded radiological review. ANZ J Surg 2012;82(12):908–912.
Beaudouin-Bazire C, Dalmas N, Bourgeois J, Babinet A, Anract P, Chantelot C, et al. Real frequency of ordinary and atypical sub-trochanteric and diaphyseal fractures in France based on X-rays and medical file analysis. Joint Bone Spine 2013;80(2):201–205.
Marcano A, Taormina D, Egol KA, Peck V, Tejwani NC. Are race and sex associated with the occurrence of atypical femoral fractures? Clin Orthop Relat Res 2014;472(3):1020–1027.
Saita Y, Ishijima M, Mogami A, Kubota M, Baba T, Kaketa T, et al. The incidence of and risk factors for developing atypical femoral fractures in Japan. J Bone Miner Metab 2015;33(3):311–318.
Meling T, Nawab A, Harboe K, Fosse L. Atypical femoral fractures in elderly women: a fracture registry-based cohort study. Bone Joint J 2014;96-B(8):1035–1040.
Luangkittikong S, Unnanuntana A. Prevalence of atypical femoral fractures in Thai patients at a single institution. J Med Assoc Thai 2014;97(6):635–643.
Juby AG, Crowther S, Cree M. Identifying atypical femoral fractures—a retrospective review. Calcif Tissue Int 2014;95(5):405–412.
Weil YA, Rivkin G, Safran O, Liebergall M, Foldes AJ. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma 2011;71(1):186–190.
Prasarn ML, Ahn J, Helfet DL, Lane JM, Lorich DG. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin Orthop Relat Res 2012;470(8):2295–2301.
Egol KA, Park JH, Rosenberg ZS, Peck V, Tejwani NC. Healing delayed but generally reliable after bisphosphonate-associated complete femur fractures treated with IM nails. Clin Orthop Relat Res 2013;472(9):2728–2734.
Chiang CY, Zebaze RM, Ghasem-Zadeh A, Iuliano-Burns S, Hardidge A, Seeman E. Teriparatide improves bone quality and healing of atypical femoral fractures associated with bisphosphonate therapy. Bone 2013;52(1):360–365.
Teo BJ, Koh JS, Goh SK, Png MA, Chua DT, Howe TS. Post-operative outcomes of atypical femoral subtrochanteric fracture in patients on bisphosphonate therapy. Bone Joint J 2014;96-B(5):658–664.
Miyakoshi N, Aizawa T, Sasaki S, Ando S, Maekawa S, Aonuma H, et al. Healing of bisphosphonate-associated atypical femoral fractures in patients with osteoporosis: a comparison between treatment with and without teriparatide. J Bone Miner Metab 2015;33(5):553–559.
Banffy MB, Vrahas MS, Ready JE, Abraham JA. Nonoperative versus prophylactic treatment of bisphosphonate-associated femoral stress fractures. Clin Orthop Relat Res 2011;469(7):2028–2034.
Egol KA, Park JH, Prensky C, Rosenberg ZS, Peck V, Tejwani NC. Surgical treatment improves clinical and functional outcomes for patients who sustain incomplete bisphosphonate-related femur fractures. J Orthop Trauma. 2013;27(6):331–335.
Oh CW, Oh JK, Park KC, Kim JW, Yoon YC. Prophylactic nailing of incomplete atypical femoral fractures. Scientific World Journal 2013;450148.
Adachi JD, Lyles K, Boonen S, Colon-Emeric C, Hyldstrup L, Nordsletten L, et al. Subtrochanteric fractures in bisphosphonate-naive patients: results from the HORIZON-recurrent fracture trial. Calcif Tissue Int 2011;89(6):427–433.
Rizzoli R, Akesson K, Bouxsein M, Kanis JA, Napoli N, Papapoulos S, et al. Subtrochanteric fractures after long-term treatment with bisphosphonates: a European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis, and International Osteoporosis Foundation Working Group Report. Osteoporos Int 2011;22(2):373–390.
Bor A, Matuz M, Gyimesi N, Biczok Z, Soos G, Doro P. Gender inequalities in the treatment of osteoporosis. Maturitas 2015;80(2):162–169.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khow, K.S.F., Shibu, P., Yu, S.C.Y. et al. Epidemiology and postoperative outcomes of atypical femoral fractures in older adults: A systematic review. J Nutr Health Aging 21, 83–91 (2017). https://doi.org/10.1007/s12603-015-0652-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-015-0652-3