Abstract
With the emphasis on intestinal health, probiotics have exploded into a vast market potential. However, new scientific evidence points out that the beneficial health benefits of probiotics are not necessarily directly related to viable bacteria. However, the metabolites or bacterial components of the live bacteria are the driving force behind health promotion. Therefore, scientists gradually noticed that the beneficial effects of probiotics are based on bacteria itself, metabolites, or cell lysates, and these factors are officially named “postbiotics” by the ISAPP. Postbiotic components are diverse and outperform live probiotics in terms of technology, safety, and cost due to their good absorption, metabolism, and organismal distribution. Postbiotics have been shown to have bioactivities such as antimicrobial, antioxidant, anti-inflammatory, anti-proliferative, and immunomodulation. Moreover, numerous studies have revealed the significant potential of postbiotics for disease treatment. This paper first presents the production and classification of postbiotics with examples from lactic acid bacteria (LAB), followed by the mechanisms of action with the most recent pre-clinical and clinical studies and the wide range of non-clinical and clinical applications of postbiotics. Furthermore, the current and future prospects of the postbiotic market with commercial available products are discussed. Finally, we comment on the knowledge gaps and future clinical applications with several examples.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past few decades, researchers have clarified that the human microbiome is critical to both short- and long-term human health. The microbiome is intimately linked to immune system development and determines immune function, microbiome, and overall health in adulthood. The concept of probiotics has been evolving over the past few decades, with the currently accepted definition describing probiotics as “live microorganisms that can benefit the host when consumed in sufficient quantities [1]. Although the definition of probiotics suggests that microorganisms should be viable to provide beneficial effects, recent studies have shown that microbial viability is not necessary to produce benefits [2, 3]. Some studies have found that extracts of Bifidobacterium spp. and Lactobacillus spp. have in vitro tumor suppressive activity [4, 5]. The idea that nonviable or inactive probiotics and their metabolic by-products can provide health benefits to the host has been proposed [6]. Postbiotics, also known as metabolites, biogenic or cell-free supernatant (CFS), refer to “soluble factors secreted by living bacteria or released by bacterial lysis” [5, 7]. These soluble factors can be short-chain fatty acids (SCFAs), microbial fractions, functional proteins/enzymes, extracellular polysaccharides, cell lysates, cell wall peptides (teichoic acid, lipoteichoic acid, peptidoglycans, etc.) [7,8,9,10]. The exact mechanism of action by which postbiotics exert specific effects has not been fully elucidated [7, 11]. However, available scientific data suggest that postbiotics have different functional properties, including but not limited to antibacterial, antioxidant, and immunomodulatory, which provide an immediate defense to the host [12,13,14,15,16,17,18,19,20,21,22]. These properties can positively affect microflora homeostasis, host metabolism, and signaling pathways, thus influencing specific physiological, immune, neurohormonal biological regulation, and metabolic responses [7, 23]. Recent studies have shown that the functional properties of postbiotics may be related to the enhancement of intestinal barrier function and mucosal immunity, which in turn can prevent immune diseases and regulate microflora composition and activity [24,25,26,27,28,29]. It has also been suggested that postbiotics have functional properties such as pathogen inhibition, obesity control, and maintenance of glucose homeostasis [30]. Although the importance of postbiotics has not been universally appreciated, and studies have been mainly derived from common Lactobacillus, research on their functional properties is gradually increasing [31]. Given the diversity of postbiotic components and significant bioactivities, this review presents and discusses the production and characterization of postbiotics, mechanisms of action with the most recent pre-clinical and clinical studies, and the wide range of non-clinical and clinical applications. The current and future market trends, knowledge gaps, and future clinical applications of postbiotics are also analyzed and discussed.
Production and Classification of Postbiotic Components
Postbiotics are secreted by food-grade microorganisms or released after cell lysis in complex microbial cultures (cell-free supernatant), food, or intestine [5, 32,33,34] (Fig. 1). After extracting the supernatant, the effects of the supernatant itself can be studied, or specific substances can be isolated from the supernatant for further study [25, 35,36,37]. The amount and type of postbiotic products are mainly related to the type of bacterial strain, the culturing medium, and the treatment of the bacteria after propagation. Postbiotics in the food undergo no post-propagation treatment and contain only soluble factors, such as products or metabolic by-products secreted into the medium during bacterial growth [34]. However, in some work, bacterial cells are subjected to lysis after propagation by cell fragmentation techniques, including thermal, enzymatic, chemical, sonication, hyperbaric, solvent extraction, or a combination [36, 38, 39]. These treatments introduce many additional intracellular metabolites and cell wall-derived materials into the postbiotic mixture and impart new functions to the obtained postbiotics. The obtained solutions were subjected to additional extraction and purification steps such as centrifugation, dialysis, lyophilization, and column purification in both treated and untreated postbiotic mixtures to separate the bacterial cells from the postbiotic metabolites [32, 40]. In general, postbiotics are characterized by the microorganisms used as starting points and inactivation procedures or techniques used for their production, as each process affects the quality and quantity of the final postbiotics produced and results in different postbiotics with different effects [41]. Given the complexity of biological compounds with varying degrees of polymerization and glycosidic bonds, qualitative and quantitative analysis of postbiotics typically necessitates complex equipment and multiple concentration/purification steps using common methods such as chromatography (gas-phase, liquid-phase, thin-layer chromatography, etc.), spectroscopy (NMR, Fourier transform infrared absorption spectroscopy), and spectrophotometry [11, 37]. The appropriate method is usually chosen according to the analytical objectives and the type of characterization sought—the main postbiotic components and production process as shown in Fig. 1.
The use of high-tech equipment, simulating the human intestinal environment, directly produces soluble factors of health effects on the human body. Postbiotics can withstand the destructive effects of gastric juice, digestive enzymes, and bile and can be absorbed directly after administration without going through the traditional trilogy of live probiotics. Compared to probiotics, postbiotics have several advantages: first, postbiotics are more stable, with a longer shelf life and better environmental tolerance; second, postbiotics are safer. Postbiotics are equally adaptable to some special populations, such as newborns and sensitive people. Postbiotics are also not inhibited by the interference of antibiotics, and there is no risk of passing on drug-resistant genes; third, postbiotics have a wider range of action targets. The poor stability and potential safety risks associated with the presence of live bacteria are well addressed by postbiotics, so the safer and more effective intestinal native bacteria, Lactobacillus, will be the mainstay of postbiotic development. Lactobacillus and Bifidobacterium are the only strains approved for use in infant foods, indicating their safety and effectiveness in actual use. Similarly, inactivated Bifidobacterium or Lactobacillus are undoubtedly superior to other classes of inactivated probiotics in terms of safety and effectiveness of use. Because the production of inactivated Lactobacillus postbiotics necessitates the activation and expansion, inactivated Lactobacillus, with its relatively simple cultivation conditions, controllable cost, and low management difficulty, naturally becomes the dominant force in postbiotics. The preparation and application of postbiotics from various LAB strains are shown in Table 1.
Overview of Possible Mechanisms of Action
Current studies on the physiological functions of postbiotics have mainly focused on macro-level analysis and evaluation, and the mechanisms of action of postbiotics have not been precisely and completely elucidated. Since postbiotics can be a mixture of multiple active substances, they may be driven and mediated by many different mechanisms for the health effects of the target host. We will only briefly outline the mechanisms of action, as they are described in detail in other publications [7] (Fig. 1).
The Lactobacillus genus of probiotics includes some of the most widely studied microorganisms in the world. Given the important role of Lactobacillus in many biological processes, it is not surprising that they receive great scientific attention. The specific postbiotics secreted by Lactobacillus can vary by species. For example, one of the first postbiotic compounds described with potent anti-pathogenic activity was reuterin, produced by L. reuteri [42], which inhibits the growth of many gut pathogens, including Salmonella, Shigella, Proteus, Pseudomonas, Staphylococcus, fungi, and protozoa. As such, reuterin plays an important role in maintaining a healthy gut microbiome, thereby supporting optimal intestinal permeability [43]. Similarly, Lactobacillus-secreted supernatants, in general, appear to be a rich source of antibacterial postbiotics known as bacteriocins, which also restrict the growth and activities of specific pathogens to promote a healthy gut [19, 44]. Research has shown that Lactobacillus-derived postbiotics strengthen intestinal permeability via several additional mechanisms. For example, the supernatant extracted from a L. rhamnosus GG culture reverses alcohol-induced intestinal permeability by restoring optimal levels of tight junction proteins and the factors involved in mucin production [45]. The L. rhamnosus GG supernatant includes two specific postbiotic compounds, HM0539 and p40, known to stimulate the intestinal epithelial cells to secrete mucins, which improve intestinal permeability [24]. Other postbiotics in Lactobacillus-derived supernatants inhibit the death of the epithelial cells in the gut and promote their growth. Exopolysaccharides produced by L. plantarum, for example, positively influence intestinal integrity by promoting goblet cell differentiation, and the goblet cells produce the mucus that protects the intestinal epithelial cells [46]. Lactobacillus also appears to support tissue repair through the secretion of postbiotics. Research has shown that Lactobacillus-derived postbiotics known as indoles assist during epithelial damage to promote the healing of the gut lining [47]. Lactate, another postbiotic produced by Lactobacillus, supports the healing of the intestinal mucosa in several ways. According to animal studies, lactate promotes the healthy migration rate of intestinal epithelial cells by enhancing mitochondrial ATP production and ameliorates colitis in animal studies by inducing the expression of Cdc42 and Pak1, two factors associated with healthy intestinal epithelial cell migration [48]. SCFAs also positively affect wound healing since they enhance epithelial proliferation and differentiation to repair damage to the intestinal wall [49, 50]. Postbiotics can also indirectly contribute to wound healing in the gut. A specific postbiotic from L. brevis enhances the integrity of the epithelial barrier by improving platelet accumulation at the site of the wound [51]. Furthermore, when purified from the supernatant of L. casei ss rhamnosus, the soluble postbiotic known as LCrS5-30 reduces inflammation in the gut by stimulating the apoptosis, or cell death, of human immune cells without harming the intestinal epithelial cells [52]. So, postbiotics also offer anti-inflammatory benefits, and immunomodulation at local and systemic levels is usually transduced by postnatal molecules interacting with specific receptors, including Toll-like receptors (TLRs), nucleotide-binding oligomeric structural domain receptors (NODs), such as lipoteichoic acid regulating TLR2 or TLR6 signaling, and peptidoglycan or its derived peptides regulating NOD2 signaling [12, 53, 54]. Additionally, several studies have shown that postbiotics have positive effects on host metabolism and signaling pathways, with microbial-derived vitamins and SCFAs being known host metabolic modulators, such as propionate, which alters lipid metabolism and improves insulin sensitivity and glucose tolerance [55], and butyrate, which upregulates antioxidant glutathione and has beneficial effects on oxidative stress [56]. Concrete evidence of the impressive effects of postbiotic compounds secreted by different probiotic strains is progressively increasing. In recent years there has been a significant upsurge in the research volume, initiating a better understanding of the underlying postbiotic mechanisms (Table 2). The positive impacts of postbiotics on gastrointestinal health and immune system function are just beginning to be explored in clinical studies (Table 3). Even so, the research completed thus far confirms that postbiotics play a significant role in modulating intestinal homeostasis, supporting the integrity of the intestinal mucosal, balancing the gut microbiome, and modulating immune responses, thereby conferring intriguing benefits to our health [57]. Future research will continue to shed light on how postbiotics play a role in our overall health to prevent and treat many chronic diseases.
Recent Pre-clinical and Clinical Postbiotic Studies
Inactivated Probiotics (Nonviable Probiotics)
Inactivation is a key step in the production of postbiotics. The most classic is thermal inactivation which has been used for centuries to inactivate microorganisms. Well-known pasteurization and sterilization are used almost every day for food preservation.
The abundance of Akkermansia muciniphila (Akk) is negatively associated with obesity, type 2 diabetes, and hypertension. A randomized, double-blind, placebo-controlled trial (NCT02637115) published in 2019 divided 40 overweight/obese people with insulin resistance into 3 groups, with 2 intervention groups receiving 10^10 of live or pasteurized Akk orally daily for 3 months [58]. Compared to the placebo group, pasteurized Akk supplementation significantly reduced insulin levels, insulin resistance, and total plasma cholesterol, decreased white blood cell counts and blood lipopolysaccharides, and slightly reduced body weight, fat mass, and hip circumference. Moreover, supplementation with pasteurized Akk significantly reduced blood markers of liver disease and tissue and muscle damage levels compared to pre-intervention. However, the overall benefit of live Akk supplementation was not significant. Overall, pasteurized Akk was safe and well tolerated and did not affect the overall structure of the microflora. How does pasteurized Akk help with weight loss? A subsequent study by Depommier et al. answered this question [59]. Oral administration of pasteurized Akk to diet-induced obese mice alleviated their obesity and reduced food energy efficiency. This effect was associated with increased energy expenditure, oxygen consumption, and spontaneous physical activity in mice and was not associated with the browning of white adipose tissue, as pasteurized Akk did not modulate white fat browning in subcutaneous tissue. Lipid droplet regulator perilipin2-associated protein expression was downregulated in brown and white adipose of mice orally treated with pasteurized Akk. Pasteurized Akk treatment increased energy excretion in the feces of mice, where the mechanism of action may involve a reduction in carbohydrate absorption and an increase in intestinal epithelial cell renewal. Recently, pasteurized Akk has been shown to alleviate Porphyromonas gingivalis-induced periodontitis. In a study by Mulhall et al. in lean and obese mice, P. gingivalis-associated periodontitis was induced by oral or gavage administration of live Akk (10^9), pasteurized Akk (10^9), and the Akk outer membrane protein Amuc_1100 (6 ug/mouse) for 3 weeks [60]. The results showed that live Akk bacteria, pasteurized Akk, and Amuc_1100 significantly reduced P. gingivalis-induced periodontal injury and inflammatory infiltration, decreased plasma TNF-α levels, and increased IL10 levels. Mechanically, Akk was able to decrease the growth and virulence of P. gingivalis (gingival protease and type IX secretion system) combined with an increased expression of antibacterial factors by Akk in co-culture. In another multicenter, randomized, double-blind, controlled clinical trial (ISRCTN14066467) enrolling 443 patients with irritable bowel syndrome (IBS), heat-inactivated B. bifidum MIMBb75 (10^9 cells) was administered orally once daily to the trial group (221), and placebo was administered to the control group for 8 weeks [61]. The primary composite treatment endpoint (at least 30% improvement in abdominal pain and adequate relief of IBS symptoms for at least 4 weeks during the trial) was met in 34% and 19% of patients, respectively, with significant differences between the two groups, indicating that inactivated B. bifidum MIMBb75 improved IBS and was similarly safe and well tolerated in both groups, with no serious adverse events. Until now, despite the ability of anti-inflammatory drugs to treat wheezing attacks (WA), the lack of a vaccine remains a major problem in preventing this disease. Last year, a Phase 3 randomized, double-blind, placebo-controlled, parallel-group trial (NCT01734811) including a cohort of 120 children < 3 years old with ≥ 3 WA was conducted, aiming to evaluate the efficacy and safety of mucosal immunotherapy based on whole inactivated bacteria (MV130) in preventing WA in children [62]. Results showed a significant reduction in the number of WA and a significant reduction in the median total number of days and median duration of WA in patients in the MV130 group compared to the placebo. MV130 significantly prolonged the median time from the start of treatment to the first WA in patients compared to the placebo. During this period, there were 166 adverse events, 81 in the MV130 group and 85 in the placebo group, none related to the composition of the treatment product. Thus, mucosal bacterial immunotherapy with MV130 was confirmed to prevent WA in children effectively.
Bacterial Lysates
A recent study revealed the potential to improve immunometabolic homeostasis through lysates of Methylococcus capsulatus Bath (McB) (ATCC 33009) [63]. McB restored altered microflora in mice on a high-fat, high-sugar Western diet (WD), shifting them to a low-fat fed “lean” flora composition. McB treatment of WD mice increased levels of SCFAs and alleviated diet-induced obesity. The McB diet improved glucose metabolism, reduced body and liver lipids, decreased hepatic immune cell infiltration, and alleviated non-alcoholic fatty liver disease (NAFLD). The McB diet significantly enriched Parabacteroides abundance and increased FoxP3 + RORγt + IL-17 + regulatory T cells. Moreover, the study by Pivniouk et al. demonstrated that the bacterial lysate OM-85 (Broncho-Vaxom), a standardized lysate of 21 bacterial strains, might inhibit infection of epithelial cells by SARS-CoV-2 [64]. Researchers discovered that OM-85 downregulated transcription of angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2 (TMPRSS2) (SARS-CoV-2 receptor) and decreased ACE2 protein expression in a renal epithelial cell line (Vero E6), a lung epithelial cell line (Calu-3), an intestinal epithelial cell line (Caco-2) and primary human bronchial epithelial cells. Meanwhile, OM-85 significantly inhibited the binding of SARS-CoV-2 spike (S) protein to epithelial cells and reduced the entry of S protein-pseudotyped lentiviral particles into epithelial cells, as well as reduced SARS-CoV-2 infection of epithelial cells. The above effects of OM-85 depended on its resulting down-regulation of neo-coronavirus receptors. A recent clinical study investigated the effectiveness of treating IBS with the nonviable bacterial lysate of cells and cell fractions of Escherichia coli (DSM 17252) and Enterococcus faecalis (DSM 16440) [65]. This is a phase IV, randomized, double-blind, placebo-controlled, multicenter, parallel-group study (EudraCT-No.: 2012–002741-38) that included 389 patients with IBS randomized into 2 groups, 191 receiving daily oral nonviable bacterial lysate and 198 with placebo, with the intervention lasting 26 weeks. There were no significant differences between the nonviable bacterial lysate and placebo groups in IBS-GAI score response (17.4% vs. 14.4%) and abdominal pain response (42.0% vs. 35.4%). The subgroup analysis showed better abdominal pain and improved stool firmness in the nonviable bacterial lysate group for patients with diarrhea-type IBS (IBS-D). Patients tolerated nonviable bacterial lysate well.
Bacterial Vesicles
Chen et al. recently demonstrated the osteoprotective effects of specific enterobacteria and their extracellular vesicles in a study (EVs) [66]. Glucocorticoid (GC)-induced osteonecrosis of the femoral head (ONFH) mice caged with healthy mice alleviated ONFH symptoms and restored the GC-induced reduction of intestinal bacteria L. animalis and extracellular vesicles from L. animalis (L. animalis-EVs). Furthermore, transplantation of microflora from healthy mice alleviated ONFH mice symptoms. Oral administration of L. animalis had osteoprotective effects in both ONFH mice and healthy mice. The enriched functional proteins in L. animalis-EVs were mainly involved in nucleotide-binding oligomerization domain (NOD)-like receptor signaling pathway, phosphotransferase system, β-lactam resistance, and adenosine triphosphate–binding cassette (ABC) transport. L. animalis-EVs could enter the femoral head, increase angiogenesis and osteogenesis, reduce apoptosis and thus alleviate the symptoms of ONFH. The results of another study showed that the outer membrane vesicles (OMVs) of Bacteroides thetaiotaomicron (Bt) play an immunomodulatory role by regulating the dendritic cell (DC) response [67]. In this study, DCs were first isolated from healthy individuals’ blood or colonic mucosa, patients with ulcerative colitis (UC), and patients with Crohn’s disease (CD). Colonic CD103 + DCs were significantly fewer in IBD patients than in healthy individuals, suggesting a regulatory DC deficiency in IBD patients. They found that Bt OMVs increased IL-10 expression in colonic DCs from healthy subjects but failed to upregulate IL-10 expression in UC patients. Bt OMVs significantly upregulated IL6 and CD80 expression in the blood of healthy individuals; compared with healthy individuals, the percentage of IL-10 expression in the blood of DCs from IBD patients was significantly reduced by Bt OMVs induction. Furthermore, in another study, extracellular vesicles (Q7-EVs) with a bilayer membrane structure in L. plantarum Q7 culture supernatant were obtained by ultrafiltration and ultracentrifugation with a mean size of 185.5 ± 65.4 nm [68]. The findings demonstrated that Q7-EVs ameliorated the symptoms of DSS-induced colitis model mice, including colonic shortening, bleeding, weight loss, and reduced splenic index, and Q7-EVs significantly Q7-EVs improved DSS-induced intestinal dysbiosis by increasing the number of anti-inflammatory bacteria such as Lactobacillus, Akkermansia, Bifidobacteria, and Muribaculaceae and decreasing the number of pro-inflammatory bacteria such as Proteobacteria, revealing the potential of L. plantarum EVs to support the probiotic effect.
Bacterial Metabolites
Current traditional therapies based on active probiotics or prebiotics may have limited efficacy due to the inability of exogenous bacteria to colonize hosts with inconsistent microbiome structure or the lack of probiotic targets. Microbiome-modulating metabolites can overcome these constraints by exerting beneficial host effects downstream of the microbiome or by transferring microbial configurations in a stable manner [69]. For example, during recurrent Clostridium difficile infections, the pathogen has a colonization advantage over the intestinal commensal microbiome. FMT can restore colonization resistance, effectively clearing this opportunistic infection. Buffie et al. recently demonstrated that a fraction of C. scindens with an intact secondary bile acid biosynthetic pathway could be administered to inhibit C. difficile growth, implying that supplementation with secondary bile acids could be considered as a metabolite-based alternative or supplement to FMT for the treatment of C. difficile infections. Thus, metabolite therapy may improve efficacy when combined with other microbiome-based therapies such as probiotics and nutritional interventions. These approaches will be optimized when personalized to the individual’s physiological and microbiome configuration. Many host microflora interactions relevant to human health are regulated by metabolites, which include SCFAs, amino acids, bile acids, vitamins, and polysaccharides. In recent years, there has been a proliferation of research on the role of flora metabolites in disease and health. Finn Hinrichsen et al. recently explored the alleviating effect of the flora metabolite butyrate on colitis [70]. They found that intestinal epithelial hexokinase 2 (HK2) expression was elevated during colitis in mice and patients with IBD. Specific knockdown of HK2 in intestinal epithelial cells reduced susceptibility to acute colitis in mice. In intestinal organoid and Caco-2 cells, deletion of HK2 reduced cell death and affected mitochondrial function (e.g., decreased mitochondrial respiration). Specific intestinal bacteria upregulate intestinal epithelial HK2 expression, whereas the microbially derived butyrate inhibits HK2 expression via histone deacetylase 8 (HDAC8); butyrate supplementation reduces mitochondrial respiration in Caco-2 cells and alleviates colitis in mice by inhibiting HK2. In addition, Rosser et al. found that the bacterial metabolite butyrate “relays” on regulatory B cell (Breg) activation and suppresses rheumatoid arthritis (RA) [71]. It was found that reduced fecal butyrate levels in patients with RA were associated with a reduction in CD19 + CD24hi CD38hi B cells and IL-10 + Breg. Similarly, fecal butyrate and acetate levels were reduced in a mouse model of arthritis, and butyrate supplementation relieved arthritis in a Breg-dependent manner. Moreover, butyrate supplementation enhanced the immunosuppressive function of Breg and inhibited the differentiation of germinal center B cells and plasma cells. Mechanistically, butyrate supplementation promoted the metabolism of 5-hydroxytryptamine (5-HP, serotonin) to 5-hydroxyindole-3-acetic acid (5-HIAA) by the microflora, which activated aromatic hydrocarbon receptors to activate the aryl-hydrocarbon receptor (AhR)-dependent gene transcription in the Breg. Furthermore, Yao He’s team recently revealed the mechanism by which butyrate enhances the anticancer efficacy of chemotherapy [72]. They found that butyrate could promote the efficacy of oxaliplatin by regulating CD8 + T cell function in the tumor microenvironment (TEM). Butyrate directly enhanced the antitumor cytotoxic effects of mouse CD8 + T cells in an ID2-dependent manner in vivo and in vitro by promoting the IL-12 signaling pathway. Moreover, butyrate induced ID2 expression through its histone deacetylase inhibitory activity. Butyrate levels were significantly higher in the sera of tumor patients responding to oxaliplatin than in tumor patients without response. Butyrate also increased ID2 and IFN-γ expression in CD8 + T cells isolated from healthy human in vitro cultures.
A recent study demonstrated that the intestinal flora metabolite propionate might assist in the fight against cancer [73]. Propionate inhibits colorectal cancer (CRC) growth by upregulating the HECT structural domain E3 ubiquitin-protein ligase 2 (HECTD2) and promoting the proteasomal degradation of the euchromatic histone-lysine N-methyltransferase 2 (EHMT2). Downregulation of EHMT2 leads to decreased levels of H3K9me2 in the tumor necrosis factor alpha-inducible protein 1 (TNFAIP1) promoter region, increased TNFAIP1 transcription, and induction of apoptosis. Moreover, Bacteroides thetaiotaomicron culture supernatant (rich in propionate) inhibited CRC cell growth. Both in vitro and in vivo experiments showed that EHMT2 is a therapeutic target for CRC and that propionate and EHMT2 inhibitor (BIX01294) have synergistic oncogenic effects. Although intestinal flora can produce histone deacetylase (HDAC) inhibitors such as butyrate, intestinal epithelial cells of germ-bearing mice have higher HDAC3 activity than germ-free mice. Besides that, another study also confirmed that supplementation with propionic acid alleviates multiple sclerosis (MS) [74]. Patients with MS had significantly reduced levels of propionic acid in blood and stool, accompanied by changes in the composition of the intestinal flora. Long-term propionic acid supplementation significantly reduced the annual relapse rate and improved disease progression and brain atrophy in patients with new-onset and stable patients receiving immunotherapy. After propionic acid supplementation, responders’ intestinal flora promoted Treg-inducible gene expression in the gut, and patients’ Treg mitochondrial function and morphology were restored. Furthermore, dietary isoflavones have recently been shown to ameliorate MS through microflora and its metabolite equol [75]. Bacteria metabolizing isoflavones are reduced in patients with MS, suggesting that they may have a protective effect against MS. In MS mouse models in this study, isoflavone-containing diets significantly suppressed experimental autoimmune encephalomyelitis (EAE), pro-inflammatory immune cell infiltration in the brain, and activation and proliferation of self-attacking myelin oligodendrocyte glycoprotein (MOG)-specific CD4 T cells. Mice on the isoflavone diet and the isoflavone-free diet had different intestinal flora compositions, and some differentially enriched bacteria were also present between healthy individuals and MS patients. The protective effect of the isoflavone diet against MS is dependent on the bacteria that metabolize isoflavones (e.g., Adlercreutzia and Parabacteroides distasonis) and their metabolite equol.
A recent study by Vuong et al. demonstrated that normal fetal brain nerve development depends on the maternal microbiome [76]. Abnormal expression of axonogenesis-related genes and impaired axonal growth in thalamocortical axons in embryos from antibiotic-treated (ABX) and germ-free pregnant rats affected tactile sensitivity in offspring as adults. Pre-pregnancy colonization of ABX dams with multi-strain colonies prevented these neurodevelopmental and behavioral defects in offspring. Maternal microflora regulates the metabolome of maternal blood and the embryonic brain. Microflora-associated metabolites such as metabolite trimethylamine-N-oxide (TMAO) and imidazole propionate (IP) promote embryonic thalamic axon growth. Supplementation of ABX pregnant rats with these metabolites (but not SCFAs) also prevented axon growth defects and subsequent abnormalities in tactile behavior in embryos. A multi-omics analysis of a triple-negative breast cancer (TNBC) cohort (n = 360) this year found that TMAO enhances the immunotherapeutic effect of TNBC [77] (NCT03805399). Tumor tissues from patients with the immunomodulatory subtype (immune activation of the TME) showed an elevated abundance of multiple genera under Clostridiales and TMAO, and higher plasma TMAO levels were associated with a better immunotherapeutic response. Cellular and TNBC mouse experiments demonstrated that TMAO induced GSDME-mediated pyroptosis by activating endoplasmic reticulum stress kinase PERK, thereby enhancing CD8 + T cell-mediated antitumor immunity. Supplementing dietary choline (TMAO precursor) to TNBC mice increased tumor TMAO levels and enhanced immunotherapeutic response.
A study exploring radiation protective effects of intestinal bacteria and metabolites found that surviving mice that lived to a normal lifespan after high doses of radiation had unique intestinal flora and that their microflora protected the recipient mice against radiation [78]. This radioprotection was associated with increased members of the Lachnospiraceae and Enterococcaceae in the microflora, and similar findings were found in leukemia patients treated with radiation. Colonization with both types of bacteria protected mice against radiation, promoted hematopoiesis, and alleviated gastrointestinal damage. SCFA (especially propionic acid) produced by the colonies helped mice resist radiation by attenuating DNA damage and reactive oxygen species (ROS) release in hematopoietic and gastrointestinal tissues, and the tryptophan metabolites I3A and kynurenine also had long-lasting protective effects.
Another well-known metabolite of the microflora, the bile acid metabolite isoallolithocholic acid (isoalloLCA), enhances the differentiation of anti-inflammatory Treg by promoting the formation of open chromatin structures in the Foxp3 promoter region [79,80,81]. A recent study found that Bacteroidetes can produce isoalloLCA using the 3-oxolithocholic acid and contain a cluster of isoalloLCA-producing genes [82]. The nuclear hormone receptor NR4A1 is required for isoalloLCA to enhance Treg differentiation. In patients with IBD, the levels of isoalloLCA and its related biosynthetic genes are significantly reduced, suggesting that isoalloLCA and isoalloLCA-producing bacteria may have an important role in maintaining human immune homeostasis. Another study focused on the intestinal flora of centenarians and found that a specific group of bile acids may contribute to longevity [83]. Centenarians have a unique intestinal flora profile accompanied by changes in the fecal bile acid profile, such as a decrease in primary bile acid and an enrichment of a group of lithocholic acid (LCA) derivatives. In this study, fecal bacteria from a centenarian were isolated and cultured, and Odoribacteraceae, capable of producing these LCA derivatives, were identified. Among them, several strains of Odoribacteraceae were able to produce isoalloLCA in vitro and in vivo and were dependent on 5α-reductase (5AR) and 3β-hydroxysteroid dehydrogenase (3β-HSDH). isoalloLCA potently inhibited Gram-positive pathogenic bacteria such as Clostridium difficile, suggesting that it may contribute to the reduction of pathogenic commensal infections and, thus, to the maintenance of intestinal homeostasis.
Wypych et al. used an animal model with a restricted antibody repertoire, the MD4 mouse, and found that they are resistant to allergic airway disease, which is related to the protective effect of its microflora [84]. MD4 mice have altered intestinal flora composition and function and a strong ability to metabolize l-tyrosine, resulting in increased production of p-cresol sulfate (PCS). Supplementation with l-tyrosine or PCS attenuates the airway inflammatory response in mice with asthma models. Mechanistically, PCS can selectively inhibit the production of chemokine CCL20 by lung epithelial cells by uncoupling EGFR and TLR4 signaling, thereby reducing DC activation and exerting an anti-airway inflammatory effect. Another study revealed that symbiotic bacterial fermentation products alter intestinal cell lipid metabolism [85]. The involvement of commensal strains of L. paracasei and E. coli in regulating intestinal lipid metabolism was demonstrated using m-ICcl2 enterocytes and murine models, respectively. L. paracasei produced l-lactate to inhibit the secretion of chylomicron by intestinal epithelial cells, and intestinal cells absorbed l-lactate to produce malonyl-CoA, which inhibited lipid β-oxidation and promoted lipid storage. E. coli RB01 produced acetate to inhibit chylomicron secretion by intestinal epithelial cells. The acetate was absorbed and metabolized by enterocytes to acetyl CoA and AMP, which upregulated the AMPK/PGC-1α/PPARα signaling pathway and promoted lipid β-oxidation. This study provides a basis for developing specific probiotics and metabolites as therapeutic products.
Moreover, Suez and Elinav study discovered that intestinal bacteria expressing phytase, such as Escherichia coli, metabolize dietary phytate to produce inositol-1,4,5-trisphosphate (InsP3), which directly activates HDAC3 [69]. Supplementation with either phytate or InsP3 promoted intestinal epithelial proliferation and injury recovery, improving the condition and survival of mice with colitis. InsP3 partially counteracted the inhibitory effect of butyric acid by activating HDAC3 and inducing colonic-like organ growth in mice. Bacterial phytase abundance was significantly reduced in the intestine of patients with IBD, and InsP3 induced intestinal organoid growth in patients.
Mager et al. recently focused on a microbiome-derived metabolite, inosine, that enhances the efficacy of cancer immunotherapy [86]. They identified three bacterial species, B. pseudolongum, L. johnsonii, and Olsenella, from immune checkpoint blockade (ICB)-treated CRC mouse tumor isolates that effectively enhanced the efficacy of ICB. ICB weakened intestinal barrier function, allowing inosine, a key metabolite produced by B. pseudolongum, to enter the bloodstream and promote antitumor T cell immunity. Inosine acts on the adenosine A2A receptor expressed by T cells, which promotes the differentiation and activation of Th1 cells under the co-stimulation of DCS, thus enhancing the therapeutic effect of ICB. In mouse models of CRC, bladder cancer, and melanoma, supplementation with inosine enhanced ICB efficacy.
Another microbiome product, indole, was found to help fight non-alcoholic fatty liver disease (NAFLD) [87]. The findings showed that serum indole levels of 137 subjects analyzed were negatively correlated with BMI and that obese individuals had significantly lower indole levels than lean individuals, accompanied by increased liver fat content. Indole supplementation to high-fat diet (HFD)-fed mice significantly reduced the severity of hepatic steatosis and inflammation. Indole treatment stimulated the expression of PFKFB3, a master regulator of glycolysis, in cells and inhibited macrophage pro-inflammatory activation in a PFKFB3-dependent manner. Knockdown of PFKFB3 in mouse bone marrow cells exacerbated HFD-induced hepatic steatosis and inflammation and diminished the ameliorative effect of indole on NAFLD.
Recently, a study by Bell et al. demonstrated that the microbiome metabolite reuterin could inhibit CRC growth [88]. The study found that fecal metabolites from healthy mice and human sources inhibited CRC cell growth. L. reuteri and its metabolite reuterin were significantly reduced in CRC-bearing mice and patients, and fecal metabolites significantly reduced growth inhibition of CRC. Reuterin alters redox homeostasis by depleting glutathione and reduces CRC cell proliferation and survival. Reuterin induced protein oxidation and selectively inhibited ribosome biosynthesis and protein translation. Exogenous L. reuteri increased tumor ROS, reduced protein translation in vivo, limited colon tumor growth, and prolonged survival in mice.
Other Components
Lai et al. recently identified probiotic and postbiotic lipopolysaccharide (LPS) that may improve chronic obstructive pulmonary disease (COPD) [89]. LPS are bioactive substances present in the outer membrane of Gram-negative bacteria and are considered to be very typical endotoxins [90]. They cause a range of biological effects that may be harmful or beneficial to the host [90]. The study first established a mouse model of smoking-induced COPD and confirmed that intestinal flora could influence COPD progression through cohabitation, antibiotic treatment, and fecal transplantation experiments. Parabacteroides goldsteinii was negatively associated with COPD, and oral administration of an isolated strain of P. goldsteinii (MTS01) to mice alleviated COPD by reducing intestinal inflammation, enhancing mitochondrial and ribosomal activity in colonocytes, restoring abnormal amino acid metabolism, and suppressing lung inflammation. LPS of P. goldsteinii had anti-inflammatory effects and inhibited COPD by antagonizing the TLR4 signaling pathway to alleviate COPD. Furthermore, Kawanabe-Matsuda et al. found that dietary Lactobacillus-derived exopolysaccharide may enhance tumor immunotherapy [91]. Oral administration of microbial exopolysaccharide (EPS-R1) produced by L. delbrueckii subsp. bulgaricus OLL1073R-1 in mice induced CCR6 + CD8 + T cells in Peyer’s patches. In CCL20-expressing cancers, CCR6 gene expression was associated with better patient prognosis. In mice, EPS-R1 enhanced the efficacy of CTLA-4 monoclonal antibody and PD-1 monoclonal antibody against CCL20-expressing tumors by increasing CCR6 + CD8 + T cell infiltration and inducing IFN-γ production to maintain T cell function and the effect was microbiome-independent. Mechanistically, the phosphorylated structure of EPSR1 induces CCR6 + CD8 + T cells by acting on the lysophosphatidic acid receptor on CD8 + T cells.
Current and Future Perspectives of the Postbiotic Market
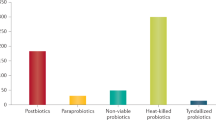
The biotics market is still being shaped today. If the definition of probiotics is clear to consumers, prebiotics and postbiotics still have a long way to go. For professionals in the industry, postbiotics become even clearer after being defined by ISAPP in 2021 [7]. However, consumers are still far from knowing the definition and concept of postbiotic, even if we see the term catching on in some media. Since 2013, the number of global research projects involving postbiotics has been growing. However, due to the late start, the number of postbiotic research projects is still far behind compared to probiotics and prebiotics. The postbiotic market has a broad scope for development, attracting many food companies to layout, including Good Service Foods, Kameda Fruit, Asahi, Cargill, ADM, etc. With the help of related companies, the commercialization process of postbiotics will be accelerated. Globally, the postbiotic market is mainly concentrated in the United States, Japan, and Europe.
From the perspective of intestinal health, probiotics, prebiotics, and postbiotics all play an important role in the human body, but compared to probiotics and prebiotics, postbiotics have unique advantages; for example, postbiotics have a targeted regulation effect, and the target points are not limited to the intestinal tract, but also include the oral cavity, skin, genitourinary tract, nasopharynx and other parts. Moreover, Due to the good processing performance of the product, postbiotics can be applied to the production of various products. Therefore, the application of postbiotics is very wide and can be used in many industries, such as food, beverages, healthcare products, cosmetics, nutraceuticals, etc. (Fig. 2). Driven by the improvement of residents’ health care awareness and increased health food demand, major enterprises have devoted themselves to researching and developing postbiotics-related products. In this context, the application of postbiotic products has gradually expanded from candy, juice, shakes, meal replacement powder, and other healthy foods to bread, snacks, and other daily foods. We currently see a few products on the market (Table 4). As the research on postbiotics continues to intensify, postbiotics are now also being introduced to prevent or treat diseases. A recently published work systematically reviewed the use of postbiotics in clinical treatment [92]. Current evidence suggests that postbiotics have a more pronounced effect in improving acute/chronic diarrhea, immune function, allergic reactions, and neurodegenerative diseases, with good stability and safety [92]. However, the health effects of postbiotics are also subject to extensive scientific evidence. In the future, we can draw on the research methods of the health effects of probiotics to construct a more scientific, reasonable, and better evaluation method of the quantitative-effect relationship to provide stronger support for the healthy and sustainable development of postbiotic preparations. Although there is limited clinical evidence on the use of postbiotics for disease prevention and treatment, it is believed that as research continues, there will be more large-scale, higher quality, and more rigorous trial data to support the efficacy of postbiotics. Moreover, although there are no clear international regulatory standards for postbiotics, in some countries, postbiotics have been incorporated into their national regulations, and their products have entered the public domain. In conclusion, research on the definition, mechanism, efficacy, and safety of postbiotics will provide producers and regulatory agencies with practical criteria for evaluation.
Knowledge Gaps and Future Clinical Applications
Based on the studies discussed in this review, it is clear that researchers have begun to identify specific components of postbiotic preparations that play a critical role in producing health-modifying effects. However, more research is required to fill knowledge gaps and broaden our understanding of how these health-modifying effects occur. Postbiotics, unlike probiotics, do not proliferate or grow in the gut and thus do not provide a sustained effect once supplementation is discontinued. More research is needed to identify various crucial postbiotic biomarkers at the concentrations required to induce positive health effects. Quantifying postbiotic biomarkers would also aid in determining whether the levels detected in a specific host microbiome environment are insufficient and/or indicative of disease status and whether the host would benefit from postbiotic supplementation. Furthermore, many components of the bacterial cell wall are immunogenic, such as LPS and lipoteichoic acid, found in the cell walls of Gram-negative and Gram-positive bacteria, respectively, and can be released into the environment spontaneously. Although LPS and lipoteichoic acid have been shown to stimulate the immune system, data on their activity is lacking. For instance, some reports suggest that lipoteichoic acid reduces the production of IL-12 and induces the production of cytokines with immunomodulatory activity (e.g., IL-10) [93]. In contrast, some studies suggest that lipoteichoic acid does not reduce the inflammatory process and causes damage to intestinal tissues [94]. Despite the reported beneficial activity, LPS and lipoteichoic acid may have side effects on the organism and cause excessive inflammatory responses. Therefore, further safety assessment, including mode of administration and dosage, is necessary. Further to that, if postbiotic supplementation is thought to be beneficial, more research will be needed to determine the extent to which supplemental postbiotics delivered via different modes of administration reach the target microbiome and have the desired impact. For example, when certain postbiotics are taken orally, there is a chance that they will be metabolized by microflora before reaching the large intestine, causing the health benefits to be diluted. In this case, studies using in vitro gut models could be crucial in this work.
Postbiotics play a crucial role in immune system maturation by influencing the tightness of the barrier and the intestinal ecosystem and indirectly shaping the structure of intestinal flora. Thus, postbiotics can treat or prevent many diseases, including those for which no effective etiological treatments exist. Prebiotics may be especially beneficial for infants because the first few months of life are critical for developing an appropriate microflora structure. As the microflora “matures” to around 3 years of age, any abnormalities may have short and long-term consequences (e.g., necrotizing small bowel colitis and asthma). Creating the right environment for the formation of the correct microflora is essential for the future development and maintenance of a healthy child, and postbiotics can provide this. Postbiotic may also be used to prevent and treat SARS-CoV-2 infections, as the structural and metabolic activity of the gut microbiome may be associated with biomarkers of the course of severe COVID-19. The potential value of postbiotics is not limited to therapeutic applications. Indeed, the emergence of biostimulants is an area of interest. A recent study in mice found that bacteria from the genus Veillonella in the intestine converted lactic acid to propionate, significantly improving the animals’ physical performance [95]. Similar results were obtained with enteral propionate administration, implying that the use of postbiotics may improve physical health, with the observed effects being independent of the presence of the bacteria.
Concluding Remarks
Using metabolites or fragments of microbial origin (i.e., ‘postbiotics’) is an attractive therapeutic and preventive strategy in modern medicine. According to current data, such postbiotics have pleiotropic effects, including immunomodulatory, antimicrobial, anti-inflammatory, antioxidant, and anti-proliferative properties. Some of these properties are even used clinically. In some trials, the line between probiotics and postbiotics is blurred, as their effects on outcomes are often not assessed separately. We anticipate that further research into the biological activity of these metabolites will reveal new uses for postbiotics in medicine and beyond.
References
Sanders ME, Merenstein DJ, Reid G, Gibson GR, Rastall RA (2019) Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nat Rev Gastroenterol Hepatol 16(10):605–616
de Almada CN, de Almada CN, de Souza Sant’Ana A (2018) Paraprobiotics as potential agents for improving animal health. In: Di Gioia D, Biavati B, editors. Probiotics and prebiotics in animal health and food safety. Cham: Springer International Publishing 247–68
Vallejo-Cordoba B, Castro-López C, García HS, González-Córdova AF, Hernández-Mendoza A (2020) Postbiotics and paraprobiotics: a review of current evidence and emerging trends. Adv Food Nutr Res 94:1–34
Raman M, Ambalam P, Doble M (2016) Bioactive carbohydrate: dietary fibers and colorectal cancer. In: Raman M, Ambalam P, Doble M (eds) Probiotics and bioactive carbohydrates in colon cancer management. Springer India, New Delhi, pp 35–55
Aguilar-Toalá JE, Garcia-Varela R, Garcia HS, Mata-Haro V, González-Córdova AF, Vallejo-Cordoba B et al (2018) Postbiotics: an evolving term within the functional foods field. Trends Food Sci Technol 75:105–114
Martín R, Langella P (2019) Emerging health concepts in the probiotics field: streamlining the definitions. Front Microbiol 10
Salminen S, Collado MC, Endo A, Hill C, Lebeer S, Quigley EMM et al (2021) The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat Rev Gastroenterol Hepatol 18(9):649–667
Anandharaj M, Sivasankari B, Parveen RR (2014) Effects of probiotics, prebiotics, and synbiotics on hypercholesterolemia: a review. Chin J Biol 2014:572754
Sánchez B, Delgado S, Blanco-Míguez A, Lourenço A, Gueimonde M, Margolles A (2017) Probiotics, gut microbiota, and their influence on host health and disease. Mol Nutr Food Res 61(1)
Wegh CAM, Schoterman MHC, Vaughan EE, Belzer C, Benninga MA (2017) The effect of fiber and prebiotics on children’s gastrointestinal disorders and microbiome. Expert Rev Gastroenterol Hepatol 11(11):1031–1045
Barros CP, Guimarães JT, Esmerino EA, Duarte MCKH, Silva MC, Silva R et al (2020) Paraprobiotics and postbiotics: concepts and potential applications in dairy products. Curr Opin Food Sci 32:1–8
Lebeer S, Vanderleyden J, De Keersmaecker SC (2010) Host interactions of probiotic bacterial surface molecules: comparison with commensals and pathogens. Nat Rev Microbiol 8(3):171–184
Luan H, Zhang Q, Wang L, Wang C, Zhang M, Xu X et al (2014) OM85-BV induced the productions of IL-1β, IL-6, and TNF-α via TLR4- and TLR2-mediated ERK1/2/NF-κB pathway in RAW264.7 cells. J Interferon Cytokine Res 34(7):526–536
Morita N, Umemoto E, Fujita S, Hayashi A, Kikuta J, Kimura I et al (2019) GPR31-dependent dendrite protrusion of intestinal CX3CR1(+) cells by bacterial metabolites. Nature 566(7742):110–114
Cervantes-Barragan L, Chai JN, Tianero MD, Di Luccia B, Ahern PP, Merriman J et al (2017) Lactobacillus reuteri induces gut intraepithelial CD4(+)CD8αα(+) T cells. Science 357(6353):806–810
Thomas CM, Hong T, van Pijkeren JP, Hemarajata P, Trinh DV, Hu W et al (2012) Histamine derived from probiotic Lactobacillus reuteri suppresses TNF via modulation of PKA and ERK signaling. PLoS ONE 7(2):e31951
Thangaraju M, Cresci GA, Liu K, Ananth S, Gnanaprakasam JP, Browning DD et al (2009) GPR109A is a G-protein-coupled receptor for the bacterial fermentation product butyrate and functions as a tumor suppressor in colon. Cancer Res 69(7):2826–2832
Sun Z, Harris HM, McCann A, Guo C, Argimón S, Zhang W et al (2015) Expanding the biotechnology potential of lactobacilli through comparative genomics of 213 strains and associated genera. Nat Commun 6:8322
Corr SC, Li Y, Riedel CU, O’Toole PW, Hill C, Gahan CG (2007) Bacteriocin production as a mechanism for the antiinfective activity of Lactobacillus salivarius UCC118. Proc Natl Acad Sci U S A 104(18):7617–7621
Nakamura F, Ishida Y, Sawada D, Ashida N, Sugawara T, Sakai M et al (2016) Fragmented lactic acid bacterial cells activate peroxisome proliferator-activated receptors and ameliorate dyslipidemia in obese mice. J Agric Food Chem 64(12):2549–2559
Tiptiri-Kourpeti A, Spyridopoulou K, Santarmaki V, Aindelis G, Tompoulidou E, Lamprianidou EE et al (2016) Lactobacillus casei exerts anti-proliferative effects accompanied by apoptotic cell death and up-regulation of TRAIL in colon carcinoma cells. PLoS ONE 11(2):e0147960
Compare D, Rocco A, Coccoli P, Angrisani D, Sgamato C, Iovine B et al (2017) Lactobacillus casei DG and its postbiotic reduce the inflammatory mucosal response: an ex-vivo organ culture model of post-infectious irritable bowel syndrome. BMC Gastroenterol 17(1):53
Sharma M, Shukla G (2016) Metabiotics: one step ahead of probiotics; an insight into mechanisms involved in anticancerous effect in colorectal cancer. Front Microbiol 7:1940
Yan F, Liu L, Dempsey PJ, Tsai YH, Raines EW, Wilson CL et al (2013) A Lactobacillus rhamnosus GG-derived soluble protein, p40, stimulates ligand release from intestinal epithelial cells to transactivate epidermal growth factor receptor. J Biol Chem 288(42):30742–30751
Gao J, Li Y, Wan Y, Hu T, Liu L, Yang S et al (2019) A novel postbiotic from Lactobacillus rhamnosus GG with a beneficial effect on intestinal barrier function. Front Microbiol 10:477
Schiavi E, Gleinser M, Molloy E, Groeger D, Frei R, Ferstl R et al (2016) The surface-associated exopolysaccharide of Bifidobacterium longum 35624 plays an essential role in dampening host proinflammatory responses and repressing local TH17 responses. Appl Environ Microbiol 82(24):7185–7196
Engevik MA, Luk B, Chang-Graham AL, Hall A, Herrmann B, Ruan W et al (2019) Bifidobacterium dentium fortifies the intestinal mucus layer via autophagy and calcium signaling pathways. mBio 10(3)
Feng Y, Wang Y, Wang P, Huang Y, Wang F (2018) Short-chain fatty acids manifest stimulative and protective effects on intestinal barrier function through the inhibition of NLRP3 inflammasome and autophagy. Cell Physiol Biochem 49(1):190–205
Ohata A, Usami M, Miyoshi M (2005) Short-chain fatty acids alter tight junction permeability in intestinal monolayer cells via lipoxygenase activation. Nutrition 21(7–8):838–847
Kareem KY, Hooi Ling F, Teck Chwen L, May Foong O, Anjas AS (2014) Inhibitory activity of postbiotic produced by strains of Lactobacillus plantarum using reconstituted media supplemented with inulin. Gut Pathog 6:23
Teame T, Wang A, Xie M, Zhang Z, Yang Y, Ding Q et al (2020) Paraprobiotics and postbiotics of probiotic Lactobacilli, their positive effects on the host and action mechanisms: a review. Front Nutr 7:570344
Cuevas-González PF, Liceaga AM, Aguilar-Toalá JE (2020) Postbiotics and paraprobiotics: from concepts to applications. Food Res Int 136:109502
Wegh CAM, Geerlings SY, Knol J, Roeselers G, Belzer C (2019) Postbiotics and their potential applications in early life nutrition and beyond. Int J Mol Sci 20(19)
Żółkiewicz J, Marzec A, Ruszczyński M, Feleszko W (2020) Postbiotics-a step beyond pre- and probiotics. Nutrients 12(8)
Nataraj BH, Ali SA, Behare PV, Yadav H (2020) Postbiotics-parabiotics: the new horizons in microbial biotherapy and functional foods. Microb Cell Fact 19(1):168
Hernández-Granados MJ, Franco-Robles E (2020) Postbiotics in human health: possible new functional ingredients? Food Res Int 137:109660
Moradi M, Molaei R, Guimarães JT (2021) A review on preparation and chemical analysis of postbiotics from lactic acid bacteria. Enzyme Microb Technol 143:109722
Cuevas-González PF, Aguilar-Toalá JE, García HS, González-Córdova AF, Vallejo-Cordoba B, Hernández-Mendoza A (2020) Protective effect of the intracellular content from potential probiotic bacteria against oxidative damage induced by acrylamide in human erythrocytes. Probiotics Antimicrob Proteins 12(4):1459–1470
González-González JN, Vallejo-Cordoba B, González-Córdova AF, Beltrán-Barrientos LM, García HS, Hernández-Mendoza A (2020) Effect of the intracellular content from Lactobacillus casei CRL-431 on the antioxidant properties of breast milk: Randomized double-blind controlled trial. LWT 130:109672
de Almada CN, Almada CN, Martinez RCR, Sant’Ana AS (2016) Paraprobiotics: evidences on their ability to modify biological responses, inactivation methods and perspectives on their application in foods. Trends Food Sci Technol 58:96–114
Aggarwal S, Sabharwal V, Kaushik P, Joshi A, Aayushi A, Suri M (2022) Postbiotics: from emerging concept to application. Front Sustain Food Syst 6
Talarico TL, Dobrogosz WJ (1989) Chemical characterization of an antimicrobial substance produced by Lactobacillus reuteri. Antimicrob Agents Chemother 33(5):674–679
Jones SE, Versalovic J (2009) Probiotic Lactobacillus reuteri biofilms produce antimicrobial and anti-inflammatory factors. BMC Microbiol 9:35
Cicenia A, Scirocco A, Carabotti M, Pallotta L, Marignani M, Severi C (2014) Postbiotic activities of lactobacilli-derived factors. J Clin Gastroenterol 48(Suppl 1):S18-22
Wang Y, Liu Y, Sidhu A, Ma Z, McClain C, Feng W (2012) Lactobacillus rhamnosus GG culture supernatant ameliorates acute alcohol-induced intestinal permeability and liver injury. Am J Physiol Gastrointest Liver Physiol 303(1):G32-41
Zhou X, Zhang K, Qi W, Zhou Y, Hong T, Xiong T et al (2019) Exopolysaccharides from Lactobacillus plantarum NCU116 enhances colonic mucosal homeostasis by controlling epithelial cell differentiation and c-Jun/Muc2 signaling. J Agric Food Chem 67(35):9831–9839
Li X, Zhang B, Hu Y, Zhao Y (2021) New insights into gut-bacteria-derived indole and its derivatives in intestinal and liver diseases. Front Pharmacol 12
Yu Y, Yang W, Bilotta AJ, Zhao X, Cong Y, Li Y (2021) L-lactate promotes intestinal epithelial cell migration to inhibit colitis. FASEB J 35(4):e21554
Kelly CJ, Zheng L, Campbell EL, Saeedi B, Scholz CC, Bayless AJ et al (2015) Crosstalk between microbiota-derived short-chain fatty acids and intestinal epithelial HIF augments tissue barrier function. Cell Host Microbe 17(5):662–671
Park JH, Kotani T, Konno T, Setiawan J, Kitamura Y, Imada S et al (2016) Promotion of intestinal epithelial cell turnover by commensal bacteria: role of short-chain fatty acids. PLoS ONE 11(5):e0156334
Isozaki S, Konishi H, Fujiya M, Tanaka H, Murakami Y, Kashima S et al (2021) Probiotic-derived polyphosphate accelerates intestinal epithelia wound healing through inducing platelet-derived mediators. Mediators Inflamm 2021:5582943
Chiu YH, Hsieh YJ, Liao KW, Peng KC (2010) Preferential promotion of apoptosis of monocytes by Lactobacillus casei rhamnosus soluble factors. Clin Nutr 29(1):131–140
Macho Fernandez E, Valenti V, Rockel C, Hermann C, Pot B, Boneca IG et al (2011) Anti-inflammatory capacity of selected lactobacilli in experimental colitis is driven by NOD2-mediated recognition of a specific peptidoglycan-derived muropeptide. Gut 60(8):1050–1059
Mohamadzadeh M, Pfeiler EA, Brown JB, Zadeh M, Gramarossa M, Managlia E et al (2011) Regulation of induced colonic inflammation by Lactobacillus acidophilus deficient in lipoteichoic acid. Proc Natl Acad Sci USA 108(Suppl 1):4623–30
Wolever TM, Fernandes J, Rao AV (1996) Serum acetate:propionate ratio is related to serum cholesterol in men but not women. J Nutr 126(11):2790–2797
Hamer HM, Jonkers DM, Bast A, Vanhoutvin SA, Fischer MA, Kodde A et al (2009) Butyrate modulates oxidative stress in the colonic mucosa of healthy humans. Clin Nutr 28(1):88–93
Liu Y, Wang J, Wu C (2021) Modulation of gut microbiota and immune system by probiotics, pre-biotics, and post-biotics. Front Nutr 8:634897
Depommier C, Everard A, Druart C, Plovier H, Van Hul M, Vieira-Silva S et al (2019) Supplementation with Akkermansia muciniphila in overweight and obese human volunteers: a proof-of-concept exploratory study. Nat Med 25(7):1096–1103
Depommier C, Van Hul M, Everard A, Delzenne NM, De Vos WM, Cani PD (2020) Pasteurized Akkermansia muciniphila increases whole-body energy expenditure and fecal energy excretion in diet-induced obese mice. Gut Microbes 11(5):1231–1245
Mulhall H, DiChiara JM, Huck O, Amar S (2022) Pasteurized Akkermansia muciniphila reduces periodontal and systemic inflammation induced by Porphyromonas gingivalis in lean and obese mice. J Clin Periodontol 49(7):717–729
Andresen V, Gschossmann J, Layer P (2020) Heat-inactivated Bifidobacterium bifidum MIMBb75 (SYN-HI-001) in the treatment of irritable bowel syndrome: a multicentre, randomised, double-blind, placebo-controlled clinical trial. Lancet Gastroenterol Hepatol 5(7):658–666
Nieto A, Mazón A, Nieto M, Calderón R, Calaforra S, Selva B et al (2021) Bacterial mucosal immunotherapy with MV130 prevents recurrent wheezing in children: a randomized, double-blind, placebo-controlled clinical trial. Am J Respir Crit Care Med 204(4):462–472
Jensen BAH, Holm JB, Larsen IS, von Burg N, Derer S, Sonne SB et al (2021) Lysates of Methylococcus capsulatus Bath induce a lean-like microbiota, intestinal FoxP3(+)RORγt(+)IL-17(+) Tregs and improve metabolism. Nat Commun 12(1):1093
Pivniouk V, Pivniouk O, DeVries A, Uhrlaub JL, Michael A, Pivniouk D et al (2022) The OM-85 bacterial lysate inhibits SARS-CoV-2 infection of epithelial cells by downregulating SARS-CoV-2 receptor expression. J Allergy Clin Immunol 149(3):923–33.e6
Mack I, Schwille-Kiuntke J, Mazurak N, Niesler B, Zimmermann K, Mönnikes H et al (2022) A nonviable probiotic in irritable bowel syndrome: a randomized, double-blind, placebo-controlled, multicenter study. Clin Gastroenterol Hepatol 20(5):1039–47.e9
Chen CY, Rao SS, Yue T, Tan YJ, Yin H, Chen LJ et al (2022) Glucocorticoid-induced loss of beneficial gut bacterial extracellular vesicles is associated with the pathogenesis of osteonecrosis. Sci Adv 8(15):eabg8335
Durant L, Stentz R, Noble A, Brooks J, Gicheva N, Reddi D et al (2020) Bacteroides thetaiotaomicron-derived outer membrane vesicles promote regulatory dendritic cell responses in health but not in inflammatory bowel disease. Microbiome 8(1):88
Hao H, Zhang X, Tong L, Liu Q, Liang X, Bu Y et al (2021) Effect of extracellular vesicles derived from Lactobacillus plantarum Q7 on gut microbiota and ulcerative colitis in mice. Front Immunol 12:777147
Suez J, Elinav E (2017) The path towards microbiome-based metabolite treatment. Nat Microbiol 2:17075
Hinrichsen F, Hamm J, Westermann M, Schröder L, Shima K, Mishra N et al (2021) Microbial regulation of hexokinase 2 links mitochondrial metabolism and cell death in colitis. Cell Metab 33(12):2355–66.e8
Rosser EC, Piper CJM, Matei DE, Blair PA, Rendeiro AF, Orford M et al (2020) Microbiota-derived metabolites suppress arthritis by amplifying aryl-hydrocarbon receptor activation in regulatory B cells. Cell Metab 31(4):837–51.e10
He Y, Fu L, Li Y, Wang W, Gong M, Zhang J et al (2021) Gut microbial metabolites facilitate anticancer therapy efficacy by modulating cytotoxic CD8(+) T cell immunity. Cell Metab 33(5):988–1000.e7
Ryu TY, Kim K, Han T-S, Lee M-O, Lee J, Choi J et al (2022) Human gut-microbiome-derived propionate coordinates proteasomal degradation via HECTD2 upregulation to target EHMT2 in colorectal cancer. ISME J 16(5):1205–1221
Duscha A, Gisevius B, Hirschberg S, Yissachar N, Stangl GI, Eilers E et al (2020) Propionic acid shapes the multiple sclerosis disease course by an immunomodulatory mechanism. Cell 180(6):1067–80.e16
Jensen SN, Cady NM, Shahi SK, Peterson SR, Gupta A, Gibson-Corley KN et al (2021) Isoflavone diet ameliorates experimental autoimmune encephalomyelitis through modulation of gut bacteria depleted in patients with multiple sclerosis. Sci Adv 7(28):eabd4595
Vuong HE, Pronovost GN, Williams DW, Coley EJL, Siegler EL, Qiu A et al (2020) The maternal microbiome modulates fetal neurodevelopment in mice. Nature 586(7828):281–286
Wang H, Rong X, Zhao G, Zhou Y, Xiao Y, Ma D et al (2022) The microbial metabolite trimethylamine N-oxide promotes antitumor immunity in triple-negative breast cancer. Cell Metab 34(4):581–94.e8
Guo H, Chou WC, Lai Y, Liang K, Tam JW, Brickey WJ et al (2020) Multi-omics analyses of radiation survivors identify radioprotective microbes and metabolites. Science 370(6516)
Campbell C, McKenney PT, Konstantinovsky D, Isaeva OI, Schizas M, Verter J et al (2020) Bacterial metabolism of bile acids promotes generation of peripheral regulatory T cells. Nature 581(7809):475–479
Song X, Sun X, Oh SF, Wu M, Zhang Y, Zheng W et al (2020) Microbial bile acid metabolites modulate gut RORγ+ regulatory T cell homeostasis. Nature 577(7790):410–415
Hang S, Paik D, Yao L, Kim E, Trinath J, Lu J et al (2019) Bile acid metabolites control TH17 and Treg cell differentiation. Nature 576(7785):143–148
Li W, Hang S, Fang Y, Bae S, Zhang Y, Zhang M et al (2021) A bacterial bile acid metabolite modulates T(reg) activity through the nuclear hormone receptor NR4A1. Cell Host Microbe 29(9):1366–77.e9
Sato Y, Atarashi K, Plichta DR, Arai Y, Sasajima S, Kearney SM et al (2021) Novel bile acid biosynthetic pathways are enriched in the microbiome of centenarians. Nature 599(7885):458–464
Wypych TP, Pattaroni C, Perdijk O, Yap C, Trompette A, Anderson D et al (2021) Microbial metabolism of L-tyrosine protects against allergic airway inflammation. Nat Immunol 22(3):279–286
Araújo JR, Tazi A, Burlen-Defranoux O, Vichier-Guerre S, Nigro G, Licandro H et al (2020) Fermentation products of commensal bacteria alter enterocyte lipid metabolism. Cell Host Microbe 27(3):358–75.e7
Mager LF, Burkhard R, Pett N, Cooke NCA, Brown K, Ramay H et al (2020) Microbiome-derived inosine modulates response to checkpoint inhibitor immunotherapy. Science 369(6510):1481–1489
Ma L, Li H, Hu J, Zheng J, Zhou J, Botchlett R et al (2020) Indole alleviates diet-induced hepatic steatosis and inflammation in a manner involving myeloid cell 6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3. Hepatology 72(4):1191–1203
Bell HN, Rebernick RJ, Goyert J, Singhal R, Kuljanin M, Kerk SA et al (2022) Reuterin in the healthy gut microbiome suppresses colorectal cancer growth through altering redox balance. Cancer Cell 40(2):185–200.e6
Lai HC, Lin TL, Chen TW, Kuo YL, Chang CJ, Wu TR et al (2022) Gut microbiota modulates COPD pathogenesis: role of anti-inflammatory Parabacteroides goldsteinii lipopolysaccharide. Gut 71(2):309–321
Freudenberg MA, Galanos C (1990) Bacterial lipopolysaccharides: structure, metabolism and mechanisms of action. Int Rev Immunol 6(4):207–221
Kawanabe-Matsuda H, Takeda K, Nakamura M, Makino S, Karasaki T, Kakimi K et al (2022) Dietary Lactobacillus-derived exopolysaccharide enhances immune-checkpoint blockade therapy. Cancer Discov 12(5):1336–1355
Mosca A, Abreu Y, Abreu AT, Gwee KA, Ianiro G, Tack J, Nguyen TVH et al (2022) The clinical evidence for postbiotics as microbial therapeutics. Gut Microbes 14(1):2117508
Kaji R, Kiyoshima-Shibata J, Nagaoka M, Nanno M, Shida K (2010) Bacterial teichoic acids reverse predominant IL-12 production induced by certain lactobacillus strains into predominant IL-10 production via TLR2-dependent ERK activation in macrophages. J Immunol 184(7):3505–3513
Kang SS, Sim JR, Yun CH, Han SH (2016) Lipoteichoic acids as a major virulence factor causing inflammatory responses via Toll-like receptor 2. Arch Pharm Res 39(11):1519–1529
Scheiman J, Luber JM, Chavkin TA, MacDonald T, Tung A, Pham L-D et al (2019) Meta-omics analysis of elite athletes identifies a performance-enhancing microbe that functions via lactate metabolism. Nat Med 25(7):1104–1109
El-Mokhtar MA, Hassanein KM, Ahmed AS, Gad GF, Amin MM, Hassanein OF (2020) Antagonistic activities of cell-free supernatants of lactobacilli against extended-spectrum β-lactamase producing Klebsiella pneumoniae and Pseudomonas aeruginosa. Infect Drug Resist 13:543–552
Gómez-Sala B, Herranz C, Díaz-Freitas B, Hernández PE, Sala A, Cintas LM (2016) Strategies to increase the hygienic and economic value of fresh fish: biopreservation using lactic acid bacteria of marine origin. Int J Food Microbiol 223:41–49
Singh N, Sharma C, Gulhane RD, Rokana N, Singh BP, Puniya AK et al (2018) Inhibitory effects of lactobacilli of goat’s milk origin against growth and biofilm formation by pathogens: an in vitro study. Food Biosci 22:129–138
Bajpai VK, Han JH, Rather IA, Park C, Lim J, Paek WK et al (2016) Characterization and antibacterial potential of lactic acid bacterium Pediococcus pentosaceus 4I1 isolated from freshwater fish Zacco koreanus. Front Microbiol 7:2037
Koohestani M, Moradi M, Tajik H, Badali A (2018) Effects of cell-free supernatant of Lactobacillus acidophilus LA5 and Lactobacillus casei 431 against planktonic form and biofilm of Staphylococcus aureus. Vet Res Forum 9(4):301–306
Xie C, Wang H-h, Deng S-l, Xu X-L (2016) The inhibition of cell-free supernatant of Lactobacillus plantarum on production of putrescine and cadaverine by four amine-positive bacteria in vitro. LWT - Food Sci Technol 67:106–11
Kousheh SA, Moradi M, Tajik H, Molaei R (2020) Preparation of antimicrobial/ultraviolet protective bacterial nanocellulose film with carbon dots synthesized from lactic acid bacteria. Int J Biol Macromol 155:216–225
Hamad GM, Abdelmotilib NM, Darwish AMG, Zeitoun AM (2020) Commercial probiotic cell-free supernatants for inhibition of Clostridium perfringens poultry meat infection in Egypt. Anaerobe 62:102181
Beristain-Bauza SC, Mani-López E, Palou E, López-Malo A (2016) Antimicrobial activity and physical properties of protein films added with cell-free supernatant of Lactobacillus rhamnosus. Food Control 62:44–51
Lee KJ, Park HW, Choi EJ, Chun HH (2016) Effects of CFSs produced by lactic acid bacteria in combination with grape seed extract on the microbial quality of ready-to-eat baby leaf vegetables. Cogent Food Agric 2(1):1268742
Shafipour Yordshahi A, Moradi M, Tajik H, Molaei R (2020) Design and preparation of antimicrobial meat wrapping nanopaper with bacterial cellulose and postbiotics of lactic acid bacteria. Int J Food Microbiol 321:108561
Lin T-H, Pan T-M (2019) Characterization of an antimicrobial substance produced by Lactobacillus plantarum NTU 102. J Microbiol Immunol Infect 52(3):409–417
Hartmann HA, Wilke T, Erdmann R (2011) Efficacy of bacteriocin-containing cell-free culture supernatants from lactic acid bacteria to control Listeria monocytogenes in food. Int J Food Microbiol 146(2):192–199
Ramezani M, Zainodini N, Hakimi H, Rezazadeh Zarandi E, Bagheri V, Bahramabadi R et al (2020) Cell-free culture supernatants of lactobacilli modify the expression of virulence factors genes in Staphylococcus aureus. Jundishapur J Microbiol 12:e96806
Hamad GM, Botros WA, Hafez E (2017) Combination of probiotic filtrates as antibacterial agent against selected some pathogenic bacteria in milk and cheese. Int J Dairy Sci 12:368–376
Moradi M, Tajik H, Mardani K, Ezati P (2019) Efficacy of lyophilized cell-free supernatant of Lactobacillus salivarius (Ls-BU2) on Escherichia coli and shelf life of ground beef. Vet Res Forum 10(3):193–198
Funding
This work is financially supported by the Qingdao Postdoctoral Applied Research Project (Grant No. RZ2200001423).
Author information
Authors and Affiliations
Contributions
Bing Liang wrote the draft with the support of Dongming Xing. Dongming Xing contributed to the conception of the study and made figures and tables. All authors reviewed and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liang, B., Xing, D. The Current and Future Perspectives of Postbiotics. Probiotics & Antimicro. Prot. 15, 1626–1643 (2023). https://doi.org/10.1007/s12602-023-10045-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-023-10045-x