Abstract
The use of in vitro systems that allow efficient selection of probiotic candidates with immunomodulatory properties could significantly minimize the use of experimental animals. In this work, we generated an in vitro immunoassay system based on porcine intestinal epithelial (PIE) cells and dextran sodium sulfate (DSS) administration that could be useful for the selection and characterization of potential probiotic strains to be used in inflammatory bowel disease (IBD) patients. Our strategy was based on two fundamental pillars: on the one hand, the capacity of PIE cells to create a monolayer by attaching to neighboring cells and efficiently mount inflammatory responses and, on the other hand, the use of two probiotic bifidobacteria strains that have been characterized in terms of their immunomodulatory capacities, particularly in mouse IBD models and patients. Our results demonstrated that DSS administration can alter the epithelial barrier created in vitro by PIE cells and induce a potent inflammatory response, characterized by increases in the expression levels of several inflammatory factors including TNF-α, IL-1α, CCL4, CCL8, CCL11, CXCL5, CXCL9, CXCL10, SELL, SELE, EPCAM, VCAM, NCF2, and SAA2. In addition, we demonstrated that Bifidobacterium breve M-16V and B. longum BB536 are able to regulate the C-jun N-terminal kinase (JNK) intracellular signalling pathway, reducing the DSS-induced alterations of the in vitro epithelial barrier and differentially regulating the inflammatory response in a strain-dependent fashion. The good correlation between our in vitro findings in PIE cells and previous studies in animal models and IBD patients shows the potential value of our system to select new probiotic candidates in an efficient way.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel disease (IBD) is a complex chronic inflammatory disorder that is considered a major public health concerns worldwide [1,2,3]. Crohn’s disease (CD) and ulcerative colitis (UC) are the predominant forms of IBD and are characterized by relapsing and remitting inflammation of the intestine. In susceptible individuals, the interaction of genetics with a wide range of environmental factors triggers a cascade of excessive and chronic inflammation, tissue damage, and impaired intestinal function. In this regard, two common features of IBD include the excessive apoptosis of intestinal epithelial cells (IECs) and the increased production of pro-inflammatory cytokines [4, 5]. In particular, tumor necrosis factor-α (TNF-α) has been found to be a major cytokine in the pathogenesis of IBD. TNF-α plays a central role in inducing apoptotic death in IECs, resulting in the destruction of intestinal epithelial layers [6]. The importance of TNF-α in IBD pathogenesis has been further underlined by the pronounced clinical improvement in mucosal healing that is achieved when anti-TNF-α antibody treatment is given to patients [7]. Moreover, in the last decade, it has been shown that the imbalance in pro- and anti-inflammatory cytokines and the alteration of all processes that are regulated by them in the intestinal mucosa are of fundamental importance in the generation and development of IBD [8].
The uncontrolled inflammatory response and the related intestinal damage have been objects of study of scientists seeking therapies to reduce IBD morbidities. In this regard, evidence indicates that probiotic strains with immunomodulatory capabilities are a realistic alternative as co-adjuvants in the therapy and prevention of IBD conditions [9, 10]. Several studies have indicated that immunomodulatory probiotic bifidobacteria strains are an interesting alternative for IBD treatment. Bifidobacterium animalis subsp. lactis BB12 has been shown to alleviate the intestinal alterations induced by dextran sodium sulfate (DSS) administration [11, 12]. The BB12 strain attenuated the reduction of colon length and the damage to the surface epithelium by diminishing the disruption of the cryptal glands and the apoptosis of IECs. Those beneficial effects were related to the control of the infiltration of inflammatory cells and the regulation of pro-inflammatory cytokine production [11, 12]. In a 2,4,6-trinitrobenzenesulfonic acid (TNBS)–induced colitis model, it was demonstrated that the administration of B. bifidum 231 to animals was able to reduce the intestinal inflammatory damage by reducing the levels of lipid peroxidation, nitric oxide (NO), and interleukin (IL)-1β and increasing the levels of glutathione and IL-10 [13]. It was also reported that B. animalis subsp. lactis CNCM-I2494 restored barrier function by normalizing the expression levels of several tight junction proteins, goblet cell populations, and intestinal cytokines in a model of dinitrobenzene sulfonic acid (DNBS)–induced colitis [14]. Furthermore, the CNCM-I2494 strain also restored the Th1/Th2 ratio within the CD4+ T cell populations in both the spleen and the mesenteric lymph nodes with subsequent increased production of IL-4, IL-5, and IL-10 that diminished Th1-mediated inflammation. These examples clearly show the potential of probiotic bifidobacteria to beneficially regulate both the innate and adaptive immune responses in the IBD context. Moreover, as has been demonstrated for several probiotic properties, the ability of bifidobacteria to positively influence the intestinal epithelial barrier and the immune responses is a strain-dependent characteristic. For example, while B. longum subsp. longum CCDM 372 confers no protection against acute DSS-induced colitis, its close relative B. longum CCM 7952 improves epithelial barrier functioning and prevents disease development [15]. Considering that the beneficial effect of probiotics is a strain-dependent property, it is necessary to search for strains that exert the optimal effect.
The efficacy of IBD treatments including probiotics has been tested mainly in mouse models [9]. Although no single murine model can fully represent all the complex features involved in human IBD, scientists can choose their colitis model based on the specific biological process they wish to explore. For example, the colitis models based on the administration of DSS are useful for the study of epithelial barrier function as well as barrier restoration following acute inflammation [16, 17]. Other models are needed if immune cell recruitment [18], Th1 or Th2 responses [9], or intestinal dysbiosis [19] is the focus of research. The use of these murine models has allowed selection and characterization in terms of their mechanisms of action of various probiotic strains with potential application in patients with IBD. However, the reduction in animal testing has become a central topic of debate in the scientific community [20]. Therefore, strategies that will result in fewer animals being used to obtain sufficient data to answer a research question or in maximizing the information obtained per animal and thus potentially limiting or avoiding the subsequent use of additional animals, without compromising animal welfare, are urgently needed.
In vitro immunoassay systems that allow an efficient selection of probiotic candidates could significantly minimize the use of murine models. Because of the anatomical and functional similarities of human and porcine intestine, pig has been considered an attractive model to study mechanisms involved in intestinal diseases. In this regard, in vitro immunoassay systems based on the use of an originally porcine intestinal epithelial (PIE) cell line have been developed by our group [21,22,23]. We reported that PIE cells show epithelial-like morphology and create a monolayer attaching to neighboring cells [21, 22, 24]. In addition, we demonstrated that PIE cells express active forms of several pattern recognition receptors (PRRs) including Toll-like receptor (TLR)-3 [22] and TLR4 [23]. Therefore, these cells are able to mount innate immune responses against beneficial and pathogenic microorganisms as well as several microbial-associated molecular patterns (MAMPs) [25,26,27]. In this work, we hypothesized that these characteristics of PIE cells can give us the possibility of conducting in vitro studies to evaluate the epithelial barrier function, the innate immune response, and the influence of immunomodulatory bifidobacteria on those parameters, in the context of DSS challenge. For this purpose, we selected two bifidobacteria strains that were shown to exert immunomodulatory effects in the context of IBD. B. breve M-16V was shown to reduce the intestinal inflammatory damage in DSS-treated weaning rats [28], while B. longum BB536 was shown to induce clinical remission in patients with UC by reducing inflammatory factors [29, 30].
Materials and Methods
Porcine Intestinal Epithelial Cells
The PIE cell line was originally established by our group from intestinal epithelia derived from an unsuckled neonatal piglet. [21]. The PIE cells were maintained in Dulbecco’s modified Eagle’s medium (DMEM) enriched with 10% fetal calf serum, 100 U/ml penicillin, and 100 mg/ml streptomycin (Gibco, Thermo Fisher Scientific Co.) and plated into collagen (Type III)-coated 250 ml flasks (Sumilon, Tokyo, Japan). After reaching confluence, the plate was washed twice with PBS and treated with buffer containing 0.1 M Na2HPO4·12H2O, 0.45 M sucrose, 0.36% EDTA 4Na, and BSA at 37 °C for 5 min. Then, PIE cells were treated with a trypsin solution containing 0.25% trypsin and 0.02% EDTA in PBS at 37 °C for 3 min, and the cells were collected by centrifugation (1000×g for 5 min at 4 °C). After counting their numbers, PIE cells were seeded in a new flask, and after overnight culture, the supernatant was removed and fresh DMEM was added for subsequent culturing. At least three consecutive passages were performed before the challenge experiments were conducted.
Immunomodulatory Effect of Bifidobacteria in PIE Cells
Two bifidobacterial strains were used for the present study: Bifidobacterium longum subsp. longum BB536 and Bifidobacterium breve M-16V. Both bacteria were isolated from the fecal samples of healthy babies [29, 31] and were selected because of their immunomodulatory properties in the context of IBD [28,29,30]. Cultures were kept freeze-dried and then rehydrated using the following medium: tryptone, 10.0 g; meat extract, 5.0 g; peptone, 15.0 g; and distilled water, 1 l, pH 7. Bacteria were cultured for 12 h at 37 °C (final log phase) in Man-Rogosa-Sharpe broth (MRS, Oxoid, Cambridge, UK). Bifidobacteria were harvested through centrifugation at 3000×g for 10 min, washed 3 times with sterile 0.01 mol/l phosphate buffer saline (PBS), pH 7.2, and suspended in appropriate medium for further experiments.
PIE cells were seeded at 3 × 104 cells per well in 12-well type I collagen-coated plates (Sumitomo Bakelite Co., Tokyo, Japan) and cultured for 3 days as explained before. After changing the medium, bifidobacteria (5 × 108 cells/ml) were added, and 48 h later, each well was washed vigorously with medium at least three times to eliminate all stimulants. Then, cells were stimulated with 5000 Da of DSS dissolved in DMEM and sterilized using DISMIC 25AS 0.45 μm (ADVANTEC, Tokyo, Japan). DSS 0.01% was used for the evaluation of transepithelial electrical resistance, flow cytometry, Western blot, and qRT-PCR as described below. PIE cell viability was measured by a commercially available kit (Cell Titer 96™ AQueous, Promega, Madison, USA) based on the physiologic reduction of MTS to formazan.
Assessment of Intestinal Epithelial Barrier Function
Transepithelial electrical resistance (TER) was used as a measure of barrier function in confluent PIE cell monolayers after challenge with 5000 Da of DSS. For growth on porous filters, PIE cells were grown in DMEM and plated at 1.0 × 106 cells on 0.4-μm PTFE membranes (Corning, NY, USA). Cellular TEERs were measured with an electrical resistance system, a Millicell ERS-2 Voltohmmeter (Merck Millipore, MA, USA). Cells with stable TER readings > 500 øcm were used (4–5 weeks post plating). To evaluate the stimulus effect on the epithelial barrier, TEER was measured at baseline and after 48 h of stimulation. The blank measurements (transwell without a cell monolayer) were subtracted from TEER values of each experimental condition and were adjusted for the filter surface (0.3 cm2). The values were expressed as ohms per square centimeter. The results represent the percentage of final TER increases with respect to their basal TER value.
Apoptosis Evaluation
The GFP-CERTIFIED Apoptosis/Necrosis detection kit (Enzo Life Sciences, Farmingdale, NY, USA) was used to evaluate apoptosis in DSS-challenged PIE cells. The cells (6.0 × 104 cells/2 ml) were seeded in Celtite C-1 collagen-coated 6-well plates (SUMILON, Tokyo, Japan) and cultured at 37 °C and 5% CO2. Apoptosis-positive controls were generated by the treatment of PIE cells with 1 mM staurosporine for 4 h. After stimulation, 1 ml of epithelial buffer was added to each well and incubated for 3 min. Cells were detached by adding 500 μl of trypsin for 1 min and centrifugation at 800 rpm for 5 min. The cell pellets were washed with PBS, mixed with Dual Detection Regent, and kept at room temperature for 15 min in the dark. The measurement was performed with BD Accuri C6 Plus (BD, NJ, USA) and analyzed with FLOWJO (FLOWJO, OR, USA).
Caspase 3/7 was evaluated by using the CellEvent Caspase-3/7 Green Flow Cytometry Assay Kit (Thermo Fisher Scientific, MA, USA). PIE cells (6.0 × 104 cells/2 ml) were treated with 1 μl of CellEvent Caspase-3/7 Green Detection Reagent and incubated at 37 °C for 25 min in the dark. Then, 1 μl of SYTOX AADvanced reagent was added and incubated at 37 °C for 5 min in the dark. The measurement was performed with BD Accuri C6 Plus (BD, NJ, USA) and analyzed with FLOWJO (FLOWJO, OR, USA).
Western Blot Analysis
PIE cells were stimulated with bifidobacteria (5.1 × 108 cells/well) for 48 h. Then, the cells were washed three times with DMEM to eliminate the bacteria and subsequently challenged with 0.1% DSS for 0, 10, 20, 30, and 60 min. The PIE cells were washed and re-suspended in 200 μl of Cell Lytic M cell lysis reagent (Sigma-Aldrich, St. Louis, MO, USA) containing protease and inhibitors of phosphates (Complete mini, PhosSTOP, Roche, Mannheim, Germany). Cells were transferred to 1.5 ml Eppendorf tubes and kept at 95 °C for 5 min in a water bath. The concentration of protein was estimated using a BCA assay kit (Pierce, Rockford, IL). The lysed samples (8 μg/sample) were loaded on 10% SDS-polyacrylamide gels, and separated proteins were transferred electrophoretically to a nitrocellulose membrane. The cells were rinsed with PBS and then lysed in RIPA buffer (PBS, 1% Nonidet P-40, 0.5% sodium deoxycholate, and 0.1% SDS) with protease inhibitor cocktail (Sigma Chemical Co.) at 4 °C. Total cell lysates were separated with 8% SDS-polyacrylamide gel electrophoresis and transferred to PVDF membrane.
Jun N-terminal protein kinase (JNK) was evaluated using anti-phosphorylated JNK antibodies (Santa Cruz Biotech). Blots were developed using an ECL Western blotting detection reagent kit (Amersham Pharmacia Biotech, Inc., Piscataway, NJ). The optical protein bands were detected by ECF substrate (GE Healthcare Japan Co., Tokyo, Japan) and estimated from the peak area of a densitogram by using ImageJ software (National Institute of Health, Bethesda, MD, USA).
Intracellular Ca2+ Flux in PIE Cells
Intracellular calcium mobilization was measured using the Fluo-4 Direct™ Calcium Assay Kits from Invitrogen according to the manufacturer’s instructions (Dojindo, Kumamoto, Japan) as described previously [32]. Briefly, PIE cells were plated in 96-well white-walled plates and grown to 90% confluence. Cells were serum-starved overnight and loaded with cell-permeant Fluo-4-AM diluted in calcium-free Hanks’ balanced salt solution supplemented with 20 mm HEPES buffer provided by the manufacturer. Intracellular calcium flux was measured by fluorescence spectroscopy every 5 s for a total of 220 s (Victor2 Wallac, PerkinElmer Life Sciences). Background fluorescence was measured 30 s before addition of DSS, and the average background was subtracted from each value.
Two-step qRT-PCR
Total RNA was isolated from each cell sample using TRIzol reagent (Invitrogen). Briefly, 100 μl of chloroform was added to samples and stirred. After 3 min standing, samples were centrifuged at 15,000 rpm, 15 min, 4 °C. The upper layer (water layer) was collected and mixed with the same amount of isopropanol. After standing for 10 min, samples were centrifuged at 15000 rpm, 15 min, and 20 °C. Supernatants were eliminated, and pellets were washed with 75% ethanol. After centrifugation (15,000 rpm, 15 min, 4 °C), the supernatants were eliminated, and pellets were dried in a 50 °C block incubator. Then, samples were diluted with DEPC water. Concentration and purity were measured by a NanoDrop ND-1000 Spectrophotometer (NanoDrop Technologies, Inc., Wilmington, NC, USA).
DNAs were synthesized using a Quantitect reverse transcription (RT) kit (Qiagen, Tokyo, Japan) according to the manufacturer’s protocol. Real-time quantitative polymerase chain reaction (PCR) was performed with an Applied Biosystems Real-time PCR System 7300 (Applied Biosystems, Warrington, UK) and the Platinum SYBR Green qPCR SuperMix-UDG (uracil-DNA glycosylase) with ROX (6-carboxyl-X-rhodamine) (Invitrogen). The primers for immune factors and β-actin are provided in Supplementary Table 1 or were described previously [25, 26]. The PCR cycling conditions were 5 min at 50 °C, followed by 5 min at 95 °C, and then 40 cycles of 15 s at 95 °C, 30 s at 60 °C, and 30 s at 72 °C. The reaction mixtures contained 2.5 μl of sample cDNA and 7.5 μl of master mix, which included the sense and antisense primers. According to the minimum information for publication of quantitative real-time PCR experiment guidelines, β-actin was used as a housekeeping gene because of its high stability across various porcine tissues [25, 26]. The expression of β-actin was used to normalize cDNA levels for differences in total cDNA levels in the samples.
Statistical Analysis
Statistical analysis was performed using GLM procedures of the SAS computer program. Mean values of relative mRNA or protein expression or mean fluorescence were compared using the Bonferroni correction and multicomparison tests. Differences were considered significant at P < 0.05.
Results
Immunomodulatory Bifidobacteria Diminish the DSS-Triggered Epithelial Barrier Alterations In vitro
In preliminary studies, we evaluated the response of PIE cell monolayers to challenge with different concentrations of DSS for 1, 3, or 6 h in terms of their viability. A dose-dependent effect was observed in the viability of PIE cells after the challenge with DSS, and no significant differences were found when 1, 3, and 6 h of stimulation were compared within the same dose of DSS (data not shown). Then, we selected 0.01% DSS for 6 h for our studies.
To evaluate the effect of immunomodulatory bifidobacteria, PIE cells were treated with the bacteria and stimulated with DSS, and their viability and the TER index were evaluated (Fig. 1). DSS stimulation significantly reduced the viability and the TER index of PIE cells when compared with unchallenged controls. However, PIE cells pre-stimulated with B. longum BB536 or B. breve M-16V showed improved cell viability and significantly higher values of the TER index than DSS controls (Fig. 1). Moreover, bifidobacteria-treated PIE cells had normal values of the TER index after the stimulation with DSS.
Effect of immunomodulatory bifidobacteria strains on the in vitro epithelial barrier alterations induced by dextran sodium sulfate (DSS) administration. Porcine intestinal epithelial (PIE) cells were stimulated with Bifidobacterium breve M-16V and B. longum BB536 (5 × 108 cells/ml) for 48 h and then challenged with 0.01% DSS for 6 h. PIE cells challenged only with DSS were used as controls. Cell viability, transepithelial electrical resistance (TER), apoptosis, and caspase 3/7 expression were determined in PIE cells after challenge with DSS. TER index values before and after DSS challenge are indicated with white and black bars, respectively. The results represent three independent experiments. Significant differences when compared with the DSS control group: *P < 0.05, **P < 0.01. Significant differences between the indicated groups: †P < 0.05
We also evaluated the effect of DSS in the induction of apoptosis in PIE cells. We performed flow cytometry studies using Annexin V as a probe for phosphatidylserine on the outer membrane of apoptotic cells as well as caspase 3/7 (Fig. 1). It was observed that DSS administration significantly increased apoptotic cells and the levels of caspase 3/7 when compared with unchallenged controls. However, the apoptosis induced by DSS was lower than that found in PIE cells treated with the well-known apoptosis inductor staurosporine (Fig. 1). Of note, the induction of apoptotic cells by DSS in bifidobacteria-treated PIE cells was significantly lower than that in DSS controls and resembled that found in unchallenged PIE cells when Annexin V was used (Fig. 1). However, only B. breve M-16V-treated PIE cells showed levels of caspase 3/7 that were lower than those of DSS controls, while no differences were found between DSS controls and B. longum BB536-treated PIE cells (Fig. 1).
Immunomodulatory Bifidobacteria Differentially Regulate the JNK Pathway in DSS-Challenged PIE Cells
The activation of C-jun N-terminal kinase (JNK) (Fig. 2) and intracellular Ca2+ mobilization (Fig. 3) were evaluated in PIE cells challenged with DSS. It was observed that the phosphorylated JNK (p-JNK) protein was increased in control PIE cells between 10 and 20 min (relative index of 3.2 in the peak) after DSS challenge (Fig. 2). The p-JNK returned to basal levels after 30 min in control DSS-challenged PIE cells. An earlier and lower increase (relative index of 1.7 in the peak) in p-JNK levels was detected in B. breve M-16V-treated PIE cells after DSS stimulation (Fig. 2). Moreover, in this experimental group, a significant reduction in the level of p-JNK was observed between 30 and 60 min. In B. longum BB536–treated PIE cells, the DSS challenge only induced a modest increase in the level of p-JNK after 60 min (Fig. 2).
Effect of immunomodulatory bifidobacteria strains on the activation of the C-jun N-terminal kinase (JNK) intracellular signalling pathway induced by dextran sodium sulfate (DSS) administration. Porcine intestinal epithelial (PIE) cells were stimulated with Bifidobacterium breve M-16V and B. longum BB536 (5 × 108 cells/ml) for 48 h and then challenged with 0.01% DSS. PIE cells challenged only with DSS were used as controls. JNK and phosphorylated JNK (p-JNK) were determined in PIE cells by Western blot analysis at different time points after challenge with DSS. The results represent three independent experiments. Significant differences when compared with the basal time (minute 0): *P < 0.05, **P < 0.01
Effect of immunomodulatory bifidobacteria strains on the intracellular Ca+2 influx induced by dextran sodium sulfate (DSS) administration. Porcine intestinal epithelial (PIE) cells were stimulated with Bifidobacterium breve M-16V and B. longum BB536 (5 × 108 cells/ml) for 48 h and then challenged with 0.01% DSS. PIE cells challenged only with DSS were used as controls. Intracellular Ca+2 influx was determined in PIE cells by fluorescence spectroscopy at different time points after the challenge with DSS. The results represent three independent experiments
The treatment of PIE cells with the immunomodulatory bifidobacteria strains did not induce modifications in the intracellular Ca2+ fluxes (Fig. 3). DSS stimulation significantly increased the intracellular Ca2+ fluxes in PIE cells in all experimental groups. However, lower intracellular Ca2+ fluxes were detected in bifidobacteria-treated PIE after DSS challenge when compared with controls (Fig. 3).
Immunomodulatory Bifidobacteria Differentially Regulate the DSS-Triggered Inflammatory Response in PIE Cells
Finally, we aimed to determine immune gene expression changes induced by DSS in PIE cells. For this purpose, qRT-PCR was performed to evaluate cytokines (TNF-α, IL-1α, TGF-β), chemokines (CCL4, CCL8, CCL11, CXCL5, CXCL9, CXCL10), and adhesion molecules (SELL, SELE, EPCAM, VCAM), as well as NCF1, NCF2, PPARγc, PPARα, and SAA2.
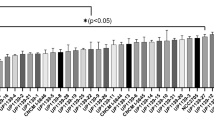
The challenge of PIE cells with DSS significantly increased the expression of TNF-α, IL-1α, and all chemokines evaluated when compared with unchallenged cells (Fig. 4). In B. longum BB536–treated PIE cells, the expression levels of TNF-α, CCL4, CCL8, CCL11, CXCL9, and CXCL10 were significantly lower than those in DSS controls. In addition, BB536-treated PIE cells had IL-1α expression levels that were higher than those in controls (Fig. 4). In B. breve M-16V–treated PIE cells, the expression levels of TNF-α, IL-1α, CCL4, CCL8, and CCL11 were significantly lower than those in DSS controls. In contrast, M-16V-treated PIE cells had CXCL5 and CXCL10 expression levels that were higher than those in DSS controls (Fig. 4). No significant variations in the expression of TGF-β were found when the different experimental groups were compared with unchallenged PIE cells (Fig. 4).
Effect of immunomodulatory bifidobacteria strains on inflammatory factor expression induced by dextran sodium sulfate (DSS) administration. Porcine intestinal epithelial (PIE) cells were stimulated with Bifidobacterium breve M-16V and B. longum BB536 (5 × 108 cells/ml) for 48 h and then challenged with 0.01% DSS for 6 h. PIE cells challenged only with DSS were used as controls. The expression of TNF-α, IL-1α, TGF-β, CCL4, CCL8, CCL11, CXCL5, CXCL9, and CXCL10 was determined in PIE cells by qRT-PCR after challenge with DSS. The results represent three independent experiments. Significant differences when compared with the DSS control group: *P < 0.05, **P < 0.01. Significant differences between the indicated groups: †P < 0.05
As shown in Fig. 5, significantly higher expression levels of SELL, SELE, VCAM, and EPCAM were found when PIE cells stimulated with DSS were compared with unchallenged cells. The expression levels of SELL and EPCAM in bifidobacteria-treated PIE cells were higher and lower than the DSS controls, respectively. No significant variations in the expression of VCAM were found when the bifidobacteria-treated cells were compared with DSS control PIE cells (Fig. 5). In addition, in B. breve M-16V-treated PIE cells, the expression levels of SELE were significantly lower than those in DSS controls, while B. longum BB536 induced no modification of this parameter (Fig. 5).
Effect of immunomodulatory bifidobacteria strains on inflammatory factor expression induced by dextran sodium sulfate (DSS) administration. Porcine intestinal epithelial (PIE) cells were stimulated with Bifidobacterium breve M-16V and B. longum BB536 (5 × 108 cells/ml) for 48 h and then challenged with 0.01% DSS for 6 h. PIE cells challenged only with DSS were used as controls. The expression of SELL, SELE, EPCAM, VCAM, NCF1, NCF2, PPARα, PPARγc, and SAA2 was determined in PIE cells by qRT-PCR after challenge with DSS. The results represent three independent experiments. Significant differences when compared with the DSS control group: *P < 0.05, **P < 0.01. Significant differences between the indicated groups: †P < 0.05
DSS stimulation also induced increases in the expression levels of NCF1, NCF2, PPARα, and SAA2 when compared with basal levels (Fig. 5). Lower expression levels of SAA2 and NCF2 were found in bifidobacteria-treated PIE cells when compared with DSS control cells. No significant variations in the expression of PPARγc were found when the different experimental groups were compared with unchallenged PIE cells (Fig. 5). In addition, no significant differences in the expression of NCF1 or PPARα were found when the bifidobacteria-treated groups were compared with DSS control PIE cells (Fig. 5).
Discussion
Murine models have allowed a significant improvement in our understanding of the cellular and molecular mechanisms involved in the development and progression of IBD. Moreover, these models have been key for finding therapies aimed at alleviating the physiological alterations produced by the disease, including the selection and characterization of probiotic candidates [9]. In this regard, one of the most important features of IBD is the alteration of the epithelial barrier function and the subsequent generation of uncontrolled inflammatory responses that further damage the intestinal mucosa [4, 5]. DSS-induced colitis models have been successfully used to reproduce those alterations and to evaluate therapeutic alternatives aimed at reducing them, including probiotics [16, 17]. However, because of the urgent need for strategies to minimize the numbers of animals being used in biomedical research, the development of highly efficient in vitro systems for probiotic evaluation is mandatory.
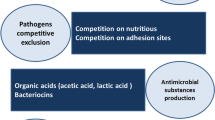
In this work, we generated an in vitro immunoassay system based on PIE cells and DSS administration that could be used for the selection and characterization of probiotic strains to be used in IBD patients. Our strategy was based on two previous findings: on the one hand, the capacity of PIE cells to create a monolayer by attaching to neighboring cells and efficiently mount inflammatory responses and, on the other hand, the use of two bifidobacteria strains that have been previously characterized in terms of their immunomodulatory capacities, particularly in IBD [28,29,30]. Our results clearly demonstrated that DSS administration can alter the epithelial barrier created in vitro by PIE cells and induce a potent inflammatory response. In addition, we demonstrated that B. breve M-16V and B. longum BB536 are able to reduce the DSS-induced alterations of the in vitro epithelial barrier and to differentially regulate the inflammatory response in a strain-dependent fashion (Fig. 6).
B. breve M-16V is an immunomodulatory bacterial strain that possesses a long tradition of use in neonatal intensive care units in some countries [28, 31, 33]. Transcriptomic microarray–based studies in neonatal and weaning rats demonstrated the anti-inflammatory effects of the M-16V strain [34]. Interestingly, the study also reported an upregulation in the expression of the claudin 1 gene, which is a major constituent of the tight junction complexes, indicating the ability of the M-16V strain to reinforce the epithelial barrier. Furthermore, by using a model of DSS administration in weaning rats, it was demonstrated that B. breve M-16V significantly improved body weight, reduced the disease activity index score, and repressed the intestinal inflammation severity and inflammation extent [28]. In this model, DSS increased the levels of intestinal TNF-α, IL-1α, IL-1β, MCP-1, and CX3CL1, and M-16V treatment was able to significantly reduce the production of IL-1β and CX3CL1. On the other hand, B. longum BB536 has been shown to be beneficial in patients with UC [29, 30]. It was reported that a higher proportion of patients with UC treated with the BB536 strain experienced clinical remission when compared with those receiving a placebo [30]. In addition, reduced levels of mucosal inducible inflammatory markers, including human β defensin, TNF-α, and IL-1α, were found in patients treated with the BB536 strain [29]. It was also reported that the administration of B. longum BB536 to mice resulted in increased gene expression of tight junction molecules (claudin 1 and ZO-1) [35]. In this work, we have advanced in the characterization of the beneficial effects of both B. breve M-16V and B. longum BB536 in the context of IBD by demonstrating in vitro their ability to differentially modulate the response of IECs to challenge with DSS.
Over the last few decades, studies on human intestinal tissue and in vivo mouse models have established epithelial barrier function, immune regulation, and tissue repair as key pillars of intestinal homeostasis controlling the host-microbe dialogue. Breakdown of these pathways and the cytokine networks by which they are regulated are a characteristic of IBD [8]. Apoptosis of IECs is a tightly regulated process in the normal intestinal epithelium, and increased cell death has been detected at inflammatory sites in both patients with IBD and a mouse model of colitis [4, 5]. Inflammatory cytokines play a central role in inducing apoptotic death in IECs, resulting in the destruction of intestinal epithelial layers [6]. Here, we were able to reproduce in vitro those relevant characteristics of the intestinal mucosa of IBD patients. In our hands, DSS administration to PIE cells significantly increased the numbers of apoptotic cells and diminished the TER index, indicating a clear alteration of the epithelial barrier. Moreover, gene expression studies revealed increased levels of TNF-α and IL-1α in DSS-challenged PIE cells that could be involved in epithelial damage. In this regard, earlier studies in T cell transfer colitis models showed increased amounts of TNF-α on the intestine, while TNF-α neutralization resulted in an attenuation of disease [36]. On the other hand, the deletion of the inflammasome component caspase-1 prevents the release of IL-1β and IL-18 and ameliorates DSS-induced colitis in mice [37]. Both B. breve M-16V and B. longum BB536 were able to suppress the alterations of the TER index and reduce the apoptosis of PIE cells. However, studies evaluating the expression of caspase 3/7 indicated that B. breve M-16V could be more efficient than the BB536 strain for reducing IEC apoptosis. This finding could be related to the differential ability of bifidobacteria to regulate TNF-α and IL-1α expression in DSS-challenged PIE cells. While the M-16V strain reduced the expression of both cytokines, B. longum BB536 only decreased TNF-α expression (Fig. 6). In line with our findings, it was shown that excessive TNF-α alters epithelial integrity and induces apoptosis in IECs, thus weakening barrier function [38, 39]. In addition, the IL-1 family cytokines IL-1β and IL-18 are produced by IECs and can act in a paracrine manner, exerting major epithelial barrier alterations through disruption of the maturation and function of IECs [40].
The ability of IECs to secrete chemokines in response to injury allows them to play an active role in shaping the nature of the local immune response. Following epithelial damage, there is a shift in the local mucosal immune system away from regulation and towards pro-inflammatory responses [41]. In the pathogenesis of IBD, chronic inflammation is driven and sustained in part by an increased production of chemokines from inflamed epithelium [42]. In this work, the challenge of PIE cells with DSS significantly increased their expression of CCL4, CCL8, CCL11, CXCL5, CXCL9, and CXCL10 as well as the adhesion molecules SELL, SELE, EPCAM, and VCAM, highlighting the role of IECs in the recruitment and activation of inflammatory leukocytes in IBD. Of note, bifidobacteria treatments were able to differentially regulate chemokines and adhesion molecule expression in DSS-challenged PIE cells. Interestingly, our experiments indicated that B. longum BB536 was more efficient than B. breve M-16V in reducing chemokine expression in PIE cells. Our results are in line with previous studies in the DSS model that revealed the ability of the M-16V strain to modulate the expression of only some chemokines [28]. It would be of value to evaluate the effect of both immunomodulatory bifidobacteria on the recruitment and activation of leukocytes and the connection of this effect to protection against intestinal damage in comparative studies in vivo. This is an interesting line of research that would allow us to advance the knowledge of the cellular mechanisms involved in the beneficial effects of bifidobacteria in IBD.
We also found that DSS challenge increased the expression of NCF2 and SAA2 and that both bifidobacteria strains were able to reduce those factors in DSS-challenged PIE cells. Genetic mutations in genes encoding components of the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase complex result in the development of chronic granulomatous disease, which is often characterized by an intestinal inflammation that is histologically similar to CD [43]. It was reported that a missense variant in the NCF2 gene, which codes for a cytosolic subunit of the multiprotein NADPH oxidase complex, predisposes patients to very early onset of IBD [44]. Although the NADPH oxidase complex is particularly important in phagocytes function, and alterations of the NCF2 gene result in a defective neutrophil respiratory burst, it has also been demonstrated that the epithelial NADPH system is involved in the pathogenesis of IBD. Studies in primary cultures of human colonic epithelial cells isolated from patients with active CD showed increased NADPH oxidase activity and overproduction of reactive oxygen species that contributed to epithelial damage [45]. In addition, microarray and quantitative PCR analyses performed in IECs isolated from mice challenged with DSS demonstrated alterations in the levels of miRNA directed to NCF2, indicating that the posttranscriptional regulation of this gene is altered, contributing to inflammation of the intestinal mucosa [46]. On the other hand, SAA is a non-specific acute-phase protein secreted in response to cytokines such as TNF-α, IL-6, and IL-1 [47]. The evaluation of serum concentrations of SAA has been suggested as a biomarker of disease activity in CD since high circulating SAA levels correlated with lack of mucosal healing [48]. Moreover, it was demonstrated that SAA participates in the inflammatory process in IBD by virtue of its ability to activate NF-κB signalling in IECs and improve the expression of pro-inflammatory cytokines [49]. The good correlation between these previous studies and our in vitro findings in PIE cells shows the potential value of our system to select new probiotic candidates in an efficient way.
JNK is an intracellular signalling factor that has been reported to be activated in the intestine of human IBD patients [50, 51]. The phosphorylation of JNK in the intestinal epithelium has been linked to the reduction of tight junction strength [52], the expression of pro-inflammatory cytokines such as IL-6 and TNF-α [53], and the induction of apoptosis [54]. In our in vitro model, a clear activation of the JNK pathway was observed in PIE cells after challenge with DSS. Moreover, we found that both B. longum BB536 and B. breve M-16V were able to differentially modulate the activation of this pathway, although strain-dependent differences were found. B. longum BB536 was more efficient than the M-16V strain at inhibiting the JNK pathway. Taking into consideration that both immunomodulatory bifidobacteria were equally effective at modulating TER alterations, and that the BB536 strain was more and less efficient at regulating inflammatory chemokine expression and apoptosis, respectively; when compared with the M-16V strain (Fig. 6), it can be concluded that other signalling pathways should be involved in the beneficial effects of bifidobacteria. In this sense, we previously evaluated the interaction of B. breve M-16V and B. longum BB536 with PIE cells and demonstrated that these bacteria are able to interact with TLR2 and upregulate the expression of negative regulators of the TLR signalling pathway. In this way, both strains modulate the subsequent TLR4 activation by reducing the activation of ERK and NF-κB pathways and the expression of inflammatory cytokines and chemokines [55]. Interestingly, B. longum BB536 efficiently inhibited the NF-κB pathway, while B. breve M-16V was more active in the inhibition of the ERK pathway. It is tempting to speculate that in the context of DSS stimulation, the regulation of the JNK and NF-κB pathways induced by B. longum BB536 significantly impacts the expression of inflammatory chemokines, while the regulation of the JNK and ERK pathways induced by B. breve M-16V efficiently modulates apoptosis of PIE cells. Further molecular studies are needed to clarify the strain-dependent effects. In addition, these results raise the question of whether a combined treatment with both immunomodulatory bifidobacteria strains would be much more effective than individual treatments to exert a beneficial effect in vivo.
Conclusion
In this work, we demonstrated that DSS administration can alter the epithelial barrier created in vitro by PIE cells and induce a potent inflammatory response, characterized by activation of the JNK signalling pathway, the induction of apoptosis, and increases in several inflammatory factors including TNF-α, IL-1α, CCL4, CCL8, CCL11, CXCL5, CXCL9, CXCL10, SELL, SELE, EPCAM, VCAM, NCF2, and SAA2. In addition, we demonstrated that the immunomodulatory strains B. breve M-16V and B. longum BB536 are able to regulate the JNK pathway in PIE cells, reducing the DSS-induced alterations of the in vitro epithelial barrier and differentially regulating the inflammatory response in a strain-dependent fashion. The good correlation between our in vitro findings in PIE cells and previous studies in animal models and IBD patients shows the potential value of our system to select new probiotic candidates. Further comparative studies that involve the use of bifidobacteria of the same species as those evaluated here and that do not have beneficial effects on the inflammatory response and/or the epithelial barrier in IBD models would be of great importance to position our in vitro system as a useful tool in the selection of potential probiotics for UC or CD.
References
Xavier RJ, Podolsky DK (2007) Unravelling the pathogenesis of inflammatory bowel disease. Nature 448:427–434. https://doi.org/10.1038/nature06005
Braus NA, Elliott DE (2009) Advances in the pathogenesis and treatment of IBD. Clin Immunol 132:1–9. https://doi.org/10.1016/j.clim.2009.02.006
Uhlig HH (2013) Monogenic diseases associated with intestinal inflammation: implications for the understanding of inflammatory bowel disease. Gut 62:1795–1805. https://doi.org/10.1136/gutjnl-2012-303956
Günther C, Neumann H, Neurath MF, Becker C (2013) Apoptosis, necrosis and necroptosis: cell death regulation in the intestinal epithelium. Gut 62:1062–1071. https://doi.org/10.1136/gutjnl-2011-301364
Hagiwara C, Tanaka M, Kudo H (2002) Increase in colorectal epithelial apoptotic cells in patients with ulcerative colitis ultimately requiring surgery. J Gastroenterol Hepatol 17:758–764. https://doi.org/10.1046/j.1440-1746.2002.02791.x
Goretsky T, Dirisina R, Sinh P, Mittal N, Managlia E, Williams DB, Posca D, Ryu H, Katzman RB, Barrett TA (2012) P53 mediates TNF-induced epithelial cell apoptosis in IBD. Am J Pathol 181:1306–1315. https://doi.org/10.1016/j.ajpath.2012.06.016
Bouma G, Strober W (2003) The immunological and genetic basis of inflammatory bowel disease. Nat Rev Immunol 3:521–533. https://doi.org/10.1038/nri1132
Maloy KJ, Powrie F (2011) Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature 474:298–306. https://doi.org/10.1038/nature10208
Martín R, Chain F, Miquel S, Motta JP, Vergnolle N, Sokol H, Langella P (2017) Using murine colitis models to analyze probiotics-host interactions. FEMS Microbiol Rev 035:49–70. https://doi.org/10.1093/femsre/fux035
Ganji-Arjenaki M, Rafieian-Kopaei M (2018) Probiotics are a good choice in remission of inflammatory bowel diseases: a meta analysis and systematic review. J Cell Physiol 233:2091–2103. https://doi.org/10.1002/jcp.25911
Imaoka A, Shima T, Kato K, Mizuno S, Uehara T, Matsumoto S, Setoyama H, Hara T, Umesaki Y (2008) Anti-inflammatory activity of probiotic Bifidobacterium: enhancement of IL-10 production in peripheral blood mononuclear cells from ulcerative colitis patients and inhibition of IL-8 secretion in HT-29 cells. World J Gastroenterol 14:2511–2516. https://doi.org/10.3748/wjg.14.2511
Chae JM, Heo W, Cho HT, Lee DH, Kim JH, Rhee MS, Park TS, Kim YK, Lee JH, Kim YJ (2018) Effects of orally-administered Bifidobacterium animalis subsp. lactis strain BB12 on dextran sodium sulfate-induced colitis in mice. J Microbiol Biotechnol 28:1800–1805. https://doi.org/10.4014/jmb.1805.05072
Satish Kumar CSV, Kondal Reddy K, Boobalan G, Gopala Reddy A, Sudha Rani Chowdhary CH, Vinoth A, Jayakanth K, Srinivasa Rao G (2017) Immunomodulatory effects of Bifidobacterium bifidum 231 on trinitrobenzenesulfonic acid-induced ulcerative colitis in rats. Res Vet Sci 110:40–46. https://doi.org/10.1016/j.rvsc.2016.10.010
Martín R, Laval L, Chain F et al (2016) Bifidobacterium animalis ssp. lactis CNCM-I2494 restores gut barrier permeability in chronically low-grade inflamed mice. Front Microbiol 7:608. https://doi.org/10.3389/fmicb.2016.00608
Srutkova D, Schwarzer M, Hudcovic T, Zakostelska Z, Drab V, Spanova A, Rittich B, Kozakova H, Schabussova I (2015) Bifidobacterium longum CCM 7952 promotes epithelial barrier function and prevents acute dss-induced colitis in strictly strain-specific manner. PLoS One 10:e0134050. https://doi.org/10.1371/journal.pone.0134050
Kiesler P, Fuss IJ, Strober W (2015) Experimental models of inflammatory bowel diseases. Cell Mol Gastroenterol Hepatol 1:154–170. https://doi.org/10.1016/j.jcmgh.2015.01.006
Lamas B, Richard ML, Leducq V, Pham HP, Michel ML, da Costa G, Bridonneau C, Jegou S, Hoffmann TW, Natividad JM, Brot L, Taleb S, Couturier-Maillard A, Nion-Larmurier I, Merabtene F, Seksik P, Bourrier A, Cosnes J, Ryffel B, Beaugerie L, Launay JM, Langella P, Xavier RJ, Sokol H (2016) CARD9 impacts colitis by altering gut microbiota metabolism of tryptophan into aryl hydrocarbon receptor ligands. Nat Med 22:598–605. https://doi.org/10.1038/nm.4102
Khor B, Gardet A, Xavier RJ (2011) Genetics and pathogenesis of inflammatory bowel disease. Nature 474:307–317. https://doi.org/10.1038/nature10209
Sokol H, Leducq V, Aschard H, Pham HP, Jegou S, Landman C, Cohen D, Liguori G, Bourrier A, Nion-Larmurier I, Cosnes J, Seksik P, Langella P, Skurnik D, Richard ML, Beaugerie L (2017) Fungal microbiota dysbiosis in IBD. Gut 66:1039–1048. https://doi.org/10.1136/gutjnl-2015-310746
Stokes WS (2002) Humane endpoints for laboratory animals used in regulatory testing. ILAR J 43:S31–S38. https://doi.org/10.1093/ilar.43.suppl_1.s31
Moue M, Tohno M, Shimazu T, Kido T, Aso H, Saito T, Kitazawa H (2008) Toll-like receptor 4 and cytokine expression involved in functional immune response in an originally established porcine intestinal epitheliocyte cell line. Biochim Biophys Acta 1780:134–144. https://doi.org/10.1016/j.bbagen.2007.11.006
Hosoya S, Villena J, Shimazu T, Tohno M, Fujie H, Chiba E, Shimosato T, Aso H, Suda Y, Kawai Y, Saito T, Alvarez S, Ikegami S, Itoh H, Kitazawa H (2011) Immunobiotic lactic acid bacteria beneficially regulate immune response triggered by poly(I:C) in porcine intestinal epithelial cells. Vet Res 42:111. https://doi.org/10.1186/1297-9716-42-111
Shimazu T, Villena J, Tohno M, Fujie H, Hosoya S, Shimosato T, Aso H, Suda Y, Kawai Y, Saito T, Makino S, Ikegami S, Itoh H, Kitazawa H (2012) Immunobiotic Lactobacillus jensenii elicits anti-inflammatory activity in porcine intestinal epithelial cells by modulating negative regulators of the Toll-like receptor signaling pathway. Infect Immun 80:276–288. https://doi.org/10.1128/IAI.05729-11
Ishizuka T, Kanmani P, Kobayashi H, Miyazaki A, Soma J, Suda Y, Aso H, Nochi T, Iwabuchi N, Xiao JZ, Saito T, Villena J, Kitazawa H (2016) Immunobiotic bifidobacteria strains modulate rotavirus immune response in porcine intestinal epitheliocytes via pattern recognition receptor signaling. PLoS One 11:e0152416. https://doi.org/10.1371/journal.pone.0152416
Kobayashi H, Albarracin L, Sato N, Kanmani P, Kober AKMH, Ikeda-Ohtsubo W, Suda Y, Nochi T, Aso H, Makino S, Kano H, Ohkawara S, Saito T, Villena J, Kitazawa H (2016) Modulation of porcine intestinal epitheliocytes immunetranscriptome response by Lactobacillus jensenii TL2937. Benef Microbes 7:769–782. https://doi.org/10.3920/BM2016.0095
Albarracin L, Kobayashi H, Iida H, Sato N, Nochi T, Aso H, Salva S, Alvarez S, Kitazawa H, Villena J (2017) Transcriptomic analysis of the innate antiviral immune response in porcine intestinal epithelial cells: influence of immunobiotic lactobacilli. Front Immunol 8:57. https://doi.org/10.3389/fimmu.2017.00057
Albarracin L, García-Castillo V, Masumizu Y et al (2020) Efficient selection of new immunobiotic strains with antiviral effects in local and distal mucosal sites by using porcine intestinal epitheliocytes. Front Immunol 11:543. https://doi.org/10.3389/FIMMU.2020.00543
Izumi H, Minegishi M, Sato Y, Shimizu T, Sekine K, Takase M (2015) Bifidobacterium breve alters immune function and ameliorates DSS-induced inflammation in weanling rats. Pediatr Res 78:407–416. https://doi.org/10.1038/pr.2015.115
Furrie E, Macfarlane S, Kennedy A et al (2005) Synbiotic therapy (Bifidobacterium longum/synergy 1) initiates resolution of inflammation in patients with active ulcerative colitis: a randomised controlled pilot trial. Gut 54:242–249. https://doi.org/10.1136/gut.2004.044834
Tamaki H, Nakase H, Inoue S, Kawanami C, Itani T, Ohana M, Kusaka T, Uose S, Hisatsune H, Tojo M, Noda T, Arasawa S, Izuta M, Kubo A, Ogawa C, Matsunaka T, Shibatouge M (2016) Efficacy of probiotic treatment with Bifidobacterium longum 536 for induction of remission in active ulcerative colitis: a randomized, double-blinded, placebo-controlled multicenter trial. Dig Endosc 28:67–74. https://doi.org/10.1111/den.12553
Abe F, Muto M, Yaeshima T, Iwatsuki K, Aihara H, Ohashi Y, Fujisawa T (2010) Safety evaluation of probiotic bifidobacteria by analysis of mucin degradation activity and translocation ability. Anaerobe 16:131–136. https://doi.org/10.1016/j.anaerobe.2009.07.006
Murofushi Y, Villena J, Morie K, Kanmani P, Tohno M, Shimazu T, Aso H, Suda Y, Hashiguchi K, Saito T, Kitazawa H (2015) The toll-like receptor family protein RP105/MD1 complex is involved in the immunoregulatory effect of exopolysaccharides from Lactobacillus plantarum N14. Mol Immunol 64:63–75. https://doi.org/10.1016/j.molimm.2014.10.027
Patole S, Keil AD, Chang A, Nathan E, Doherty D, Simmer K, Esvaran M, Conway P (2014) Effect of Bifidobacterium breve M-16V supplementation on fecal bifidobacteria in preterm neonates - a randomised double blind placebo controlled trial. PLoS One 9:e89511. https://doi.org/10.1371/journal.pone.0089511
Ohtsuka Y, Ikegami T, Izumi H, Namura M, Ikeda T, Ikuse T, Baba Y, Kudo T, Suzuki R, Shimizu T (2012) Effects of Bifidobacterium breve on inflammatory gene expression in neonatal and weaning rat intestine. Pediatr Res 71:46–53. https://doi.org/10.1038/pr.2011.11
Takeda Y, Nakase H, Namba K, Inoue S, Ueno S, Uza N, Chiba T (2009) Upregulation of T-bet and tight junction molecules by Bifidobactrium longum improves colonic inflammation of ulcerative colitis. Inflamm Bowel Dis 15:1617–1618. https://doi.org/10.1002/ibd.20861
Powrie F, Correa-Oliveira R, Mauze S, Coffman RL (1994) Regulatory interactions between CD45RBhigh and CD45RBlow CD4 + T cells are important for the balance between protective and pathogenic cell-mediated immunity. J Exp Med 179:589–600. https://doi.org/10.1084/jem.179.2.589
Siegmund B, Lehr HA, Fantuzzi G, Dinarello CA (2001) IL-1β-converting enzyme (caspase-1) in intestinal inflammation. Proc Natl Acad Sci U S A 98:13249–13254. https://doi.org/10.1073/pnas.231473998
Nenci A, Becker C, Wullaert A, Gareus R, van Loo G, Danese S, Huth M, Nikolaev A, Neufert C, Madison B, Gumucio D, Neurath MF, Pasparakis M (2007) Epithelial NEMO links innate immunity to chronic intestinal inflammation. Nature 446:557–561. https://doi.org/10.1038/nature05698
Pott J, Kabat AM, Maloy KJ (2018) Intestinal epithelial cell autophagy is required to protect against tnf-induced apoptosis during chronic colitis in mice. Cell Host Microbe 23:191–202.e4. https://doi.org/10.1016/j.chom.2017.12.017
Nowarski R, Jackson R, Gagliani N, de Zoete MR, Palm NW, Bailis W, Low JS, Harman CCD, Graham M, Elinav E, Flavell RA (2015) Epithelial IL-18 equilibrium controls barrier function in colitis. Cell 163:1444–1456. https://doi.org/10.1016/j.cell.2015.10.072
Habtezion A, Nguyen LP, Hadeiba H, Butcher EC (2016) Leukocyte trafficking to the small intestine and colon. Gastroenterology 150:340–354. https://doi.org/10.1053/j.gastro.2015.10.046
Trivedi PJ, Adams DH (2018) Chemokines and chemokine receptors as therapeutic targets in inflammatory bowel disease; pitfalls and promise. J Crohn's Colitis 12:641–652. https://doi.org/10.1093/ecco-jcc/jjx145
Marks DJB, Miyagi K, Rahman FZ, Novelli M, Bloom SL, Segal AW (2009) Inflammatory bowel disease in CGD reproduces the clinicopathological features of Crohn’s disease. Am J Gastroenterol 104:117–124. https://doi.org/10.1038/ajg.2008.72
Muise AM, Xu W, Guo CH, Walters TD, Wolters VM, Fattouh R, Lam GY, Hu P, Murchie R, Sherlock M, Gana JC, NEOPICS*, Russell RK, Glogauer M, Duerr RH, Cho JH, Lees CW, Satsangi J, Wilson DC, Paterson AD, Griffiths AM, Silverberg MS, Brumell JH (2012) NADPH oxidase complex and IBD candidate gene studies: identification of a rare variant in NCF2 that results in reduced binding to RAC2. Gut 61:1028–1035. https://doi.org/10.1136/gutjnl-2011-300078
Ramonaite R, Skieceviciene J, Kiudelis G, Jonaitis L, Tamelis A, Cizas P, Borutaite V, Kupcinskas L (2013) Influence of NADPH oxidase on inflammatory response in primary intestinal epithelial cells in patients with ulcerative colitis. BMC Gastroenterol 13:159. https://doi.org/10.1186/1471-230X-13-159
Lee J, Park EJ, Yuki Y, Ahmad S, Mizuguchi K, Ishii KJ, Shimaoka M, Kiyono H (2015) Profiles of microRNA networks in intestinal epithelial cells in a mouse model of colitis. Sci Rep 5:18174. https://doi.org/10.1038/srep18174
Florin THJ, Paterson EWJ, Fowler EV, Radford-Smith GL (2006) Clinically active Crohn’s disease in the presence of a low C-reactive protein. Scand J Gastroenterol 41:306–311. https://doi.org/10.1080/00365520500217118
Yarur AJ, Quintero MA, Jain A, Czul F, Barkin JS, Abreu MT (2017) Serum amyloid a as a surrogate marker for mucosal and histologic inflammation in patients with Crohn’s disease. Inflamm Bowel Dis 23:158–164. https://doi.org/10.1097/MIB.0000000000000991
Jijon HB, Madsen KL, Walker JW et al (2005) Serum amyloid A activates NF-κB and proinflammatory gene expression in human and murine intestinal epithelial cells. Eur J Immunol 35:718–726. https://doi.org/10.1002/eji.200425688
Mitsuyama K, Suzuki A, Tomiyasu N, Tsuruta O, Kitazaki S, Takeda T, Satoh Y, Bennett B, Toyonaga A, Sata M (2006) Pro-inflammatory signaling by Jun-N-terminal kinase in inflammatory bowel disease. Int J Mol Med 17:449–455. https://doi.org/10.3892/ijmm.17.3.449
Waetzig GH, Seegert D, Rosenstiel P, Nikolaus S, Schreiber S (2002) p38 mitogen-activated protein kinase is activated and linked to tnf-α signaling in inflammatory bowel disease. J Immunol 168:5342–5351. https://doi.org/10.4049/jimmunol.168.10.5342
Samak G, Chaudhry KK, Gangwar R, Narayanan D, Jaggar JH, Rao RK (2015) Calcium/Ask1/MKK7/JNK2/c-Src signalling cascade mediates disruption of intestinal epithelial tight junctions by dextran sulfate sodium. Biochem J 465:503–515. https://doi.org/10.1042/BJ20140450
Roy PK, Rashid F, Bragg J, Ibdah JA (2008) Role of the JNK signal transduction pathway in inflammatory bowel disease. World J Gastroenterol 14:200–202. https://doi.org/10.3748/wjg.14.200
Dhanasekaran DN, Reddy EP (2008) JNK signaling in apoptosis. Oncogene 27:6245–6251. https://doi.org/10.1038/onc.2008.301
Tomosada Y, Villena J, Murata K, Chiba E, Shimazu T, Aso H, Iwabuchi N, Xiao JZ, Saito T, Kitazawa H (2013) Immunoregulatory effect of bifidobacteria strains in porcine intestinal epithelial cells through modulation of ubiquitin-editing enzyme A20 expression. PLoS One 8:e59259. https://doi.org/10.1371/journal.pone.0059259
Funding
This study was supported by a Grant-in-Aid for Scientific Research (A) (19H00965), an Open Partnership Joint Projects of JSPS Bilateral Joint Research Projects from the Japan Society for the Promotion of Science (JSPS) and the Food Science Institute as well as the Foundation (Ryosyoku-Kenkyukai) to HK. This research was supported by grants from the project of NARO Bio-oriented Technology Research Advancement Institution (Research Program on the Development of Innovative Technology, No. 01002A) to HK. Md AI was supported by JSPS Postdoctoral Fellowship for Foreign Researchers, Program (No. 18F18081). This study was also supported by ANPCyT–FONCyT Grant PICT-2016-0410 to JV and by JSPS Core-to-Core Program, A. Advanced Research Networks entitled Establishment of International Agricultural Immunology Research-Core for a Quantum Improvement in Food Safety.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Md Islam Aminul is a JSPS Postdoctoral Fellow.
Electronic Supplementary Material
ESM 1
(DOCX 37 kb)
Rights and permissions
About this article
Cite this article
Sato, N., Yuzawa, M., Aminul, M.I. et al. Evaluation of Porcine Intestinal Epitheliocytes as an In vitro Immunoassay System for the Selection of Probiotic Bifidobacteria to Alleviate Inflammatory Bowel Disease. Probiotics & Antimicro. Prot. 13, 824–836 (2021). https://doi.org/10.1007/s12602-020-09694-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-020-09694-z