Abstract
Functional constipation has a high prevalence in both adults and children affecting quality of life. Evidence suggests that probiotics can reduce the symptoms of constipation. As the effects of probiotics are strain specific, the efficacy of Bacillus coagulans Unique IS2 in the treatment of functional constipation in adults was evaluated. Subjects (n = 100) diagnosed with functional constipation were supplemented with either B. coagulans Unique IS2 (2 billion CFU) or placebo capsules once daily for 4 weeks. Subjects were evaluated for treatment success (defined as three or more spontaneous stools per week), stool consistency, difficulty of defecation, defecation and abdominal pain. By the end of the fourth week, there was a statistically significant (p < 0.001) increase in number of bowel movements in the probiotic treated group as compared to placebo. Ninety eight percent of subjects in the probiotic group achieved normal stool consistency as compared to placebo (74%). Moreover, there was relief from symptoms of incomplete evacuation, painful defecation and abdominal pain associated with constipation in probiotic treated group as compared to placebo. In conclusion, B. coagulans Unique IS2 significantly decreased the symptoms of constipation indicating effectiveness of the strain in the treatment of constipation.
Trial registration: CTRI/2017/11/010539.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional constipation or chronic idiopathic constipation (CIC) is a symptom-based gastrointestinal disorder without an organic origin. It has a prevalence of 14% in adults which represents a huge health care burden [1, 2]. Apart from having a negative impact on the health-related quality of life (QOL) and imposing an economic burden on the individual, constipation is a worldwide problem that is common across all ages and cultures [3, 4]. It is characterised by infrequent bowel movements, usually fewer than three per week, and symptoms may also include hard stools, a feeling of incomplete evacuation, abdominal discomfort, bloating and distension [5]. The management of functional constipation still remains a challenge, with up to 47% of patients not finding relief from treatments which include bulking agents, osmotic laxatives and stool softeners [6,7,8].
Probiotics are ‘live microorganisms that, when administered in adequate amounts, confer a health benefit on the host’ [9]. Some of these beneficial effects include regulation of hypertension and lipid levels, diabetes and obesity [10,11,12,13]; attenuation of renal calculi [14]; and restoration of digestive health including constipation [15,16,17]. Probiotic supplementation has been found to be efficacious in decreasing intestinal transit times [18]. Mechanism of action of probiotics in alleviating constipation includes modification of the gastrointestinal microbiota which is altered in constipation [19,20,21]. Metabolites produced by probiotic may alter gut function, including sensation and motility [21]. Production of lactic acid and short-chain fatty acids reduces luminal pH, which enhances colonic peristalsis and hence shortens gut transit time (GTT) leading to improved bowel movements [2].
The most widely used probiotic strains are the Lactobacilli and Bifidobacteria [22]. However, Bacillus spp. are gaining a lot of attention as they are stable at room temperature [23, 24]. Bacillus coagulans Unique IS2 is a spore-forming, shelf-stable probiotic strain with established safety and efficacy in the treatment of diarrhoea, bacterial vaginosis and irritable bowel syndrome (IBS) [25,26,27]. Being a spore former, B. coagulans Unique IS2 is resistant to acidic conditions of the stomach and bile acids. It reaches the intestine without any loss of viability where it produces lactic acid. It has been deposited with the American Type Culture Collection (ATCC; ATCC PTA 11748) and Microbial Type Culture Collection (MTCC; MTCC 5260). As B. coagulans Unique IS2 has been found to improve digestive health (viz. diarrhoea and IBS in children and adults), it was of interest to study its efficacy in yet another function of digestive health, i.e. constipation.
Materials and Methods
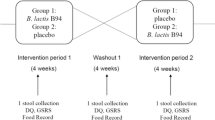
Study Design
This double-blind, randomised, placebo-controlled, parallel group multicentric study was conducted at two sites, viz., MV Hospital and Research Centre, and KRM Hospital and Research, Lucknow, India (December 2017 to August 2018). This outpatient study was conducted in compliance with the code of conduct for research involving human volunteers as issued by the International Conference on Harmonisation-Good Clinical Practice (ICH-GCP), Indian Council of Medical Research guidelines (ICMR; ethical guidelines for biomedical research on human subjects) and the principles of the Declaration of Helsinki. Informed consent forms were approved by the ethical committees of both the hospitals and the trial was registered prospectively with the clinical trial registry of India (CTRI/2017/11/010539). The study was initiated after obtaining informed consent.
Sample Size
Sample size was calculated to be 50 subjects per arm in order to detect a difference based on the primary endpoint, using a two-tailed test with 90% power, alpha risk of 5% and a drop-out of 20%. Total, enrolled subjects were 100 with 50 in each group.
Study Population
Overall, 101 subjects were screened from which 100 subjects who met the inclusion/exclusion criteria were enrolled in the study (one subject excluded due to not meeting inclusion criteria). The ITT (intention-to-treat) population consisted of randomised subjects who received one dose of either B. coagulans Unique IS2 (2 billion CFU) capsule (n = 50) or placebo (n = 50) with a post-baseline efficacy assessment. The strength (2 billion CFU) of B. coagulans in the capsule was confirmed by plating a serially diluted sample on GYE (glucose yeast extract) agar. The PP (per protocol) population consisted of subjects, both B. coagulans Unique IS2 (n = 50) and placebo (n = 50) having completed the study without any major protocol deviation. All efficacy analyses were performed on ITT population which remained the same as PP population due to no major protocol deviations.
Of the 100 patients, 50 received probiotic, B. coagulans Unique IS2 capsules (2 × 109 CFU) and 50 received placebo daily for up to 4 weeks (Fig. 1). The mean age of total patients was 43.92 ± 11.74 years (range, 18–64 years); 59 (59%) patients were males and 41 (41%) were females. The mean age of patients who received B. coagulans Unique IS2 was 42.54 ± 12.16 years (range, 18–64 years) and placebo was 45.30 ± 11.33 years (range, 24–64 years). Thirty four (68%) patients were males and 16 (32%) patients were females in B. coagulans Unique IS2 group, whereas 25 (50%) patients were males and 25 (50%) were females in placebo (Table 1).
Inclusion criteria: subjects of either sex between 18 and 65 years of age with diagnosis as functional constipation according to Rome Criteria III; should not have/had any major illnesses; willing to give written informed consent and follow study procedures. Exclusion criteria: subjects who had undergone major abdominal surgery; documented history of slow colonic transit; presence of any concomitant diseases such as organic GI diseases and/or lactose and gluten intolerance; medical or psychiatric illness; clinical features suggestive of alarming symptoms (rectal bleeding, weight loss etc.); family history of peptic ulcer, colorectal cancer or IBD, abnormal laboratory data or thyroid function; participation in any clinical trial or usage of any investigational product in the past 90 days; known or expected hypersensitivity to any of the active substances or excipients; used any probiotic formulation in the past 30 days; pregnant or lactating; allergic or atopic to any of the ingredients of the study medication.
Randomisation
After having obtained signed, written informed consent, subjects underwent a screening examination. Subjects complying with inclusion/exclusion criteria were enrolled and randomised by block randomisation to one of the two treatment arms. Based on SAS 9.4 randomisation, numbers for two treatment groups were generated. Randomisation was conducted using opaque sealed envelopes that were indistinguishable between groups in order for the investigators also to be blinded to the treatment. Each envelope had the assignment of the patient (probiotic or placebo treatment) with 50 envelopes for each group. The sealed envelopes were provided to the clinical site. The investigators assigned investigational products to patients based on the randomisation numbers. Both groups were characteristically similar pertaining to age, sex and weight of the patient.
Study Follow-up Visits and Treatments
The duration of treatment was for a period of 28 days with a follow up until the end of treatment. Bacillus coagulans Unique IS2 or placebo capsules were administered once daily for up to 28 days. As this was an outpatient study, four visits were mandatory and recorded; visit 1 was for screening and treatment initiation (day 1), visit 2 was follow-up 1 (day 8 ± 2), visit 3 was follow-up 2 (day 15 ± 2) and visit 4 was end of study (day 29 ± 2).
Efficacy and Safety Measurement Criteria
Primary efficacy endpoint was treatment success (defined as three or more spontaneous stools per week). The secondary efficacy endpoints were changes from baseline to end of treatment in stool frequency, stool consistency (as assessed by Bristol stool form scale), difficulty in degree of defecation–sensation of incomplete evacuation (CCS scale, constipation scoring system), defecation pain (CCS scale) and abdominal pain (CCS scale). Safety endpoints included the incidences of treatment-emergent adverse events, abnormal vital signs and clinically significant changes from baseline in physical examination.
Statistical Methods
All efficacy analyses were performed on ITT population which remained the same as PP population due to no major protocol deviations. Primary endpoint qualitative data was defined as number and percentages, and the data was compared using unpaired t test at 5% level of significance between groups. The secondary endpoint data was also interpreted as descriptive data for scores as n, mean, median, standard deviation and range (minimum and maximum). Data was analysed using unpaired t test at 5% level of significance between groups.
Evaluation of Results
The main criteria in the evaluation of results was to see if there was an improvement in the primary efficacy parameter, i.e. treatment success based on stool frequency (three or more spontaneous stools per week). As the study was a randomised, double-blind study, the differences observed between the two groups (probiotic and placebo) could be ascribed solely to the effect of the treatment as bias was removed. To arrive at the required sample size for the study (50 subjects/arm), sample size calculations were used to arrive at the sample size to identify a significant result in this primary outcome measure.
Results
Primary Efficacy
Treatment Success Based on Stool Frequency (Defined as Three or More Spontaneous Stools per Week)
In patients receiving B. coagulans Unique IS2 capsules, the bowel frequency was 0.90 ± 0.73 (week 1), 1.66 ± 1.81 (week 2), 4.16 ± 1.98 (week 3) and 5.98 ± 1.57 (week 4) spontaneous stools per week. In the placebo group, bowel frequency was 0.94 ± 0.86 (week 1), 1.62 ± 1.78 (week 2), 2.34 ± 1.31 (week 3) and 3.12 ± 1.18 (week 4) spontaneous stools per week (Fig. 2a, Table S1). At week 3 and week 4, there was a significant improvement (p < 0.001) in mean frequency of spontaneous stools per week in patients receiving B. coagulans Unique IS2 capsules as compared to placebo.
Secondary Efficacy
Stool Consistency
Stool consistency was assessed by Bristol stool form scale (Table S2) which categorises the stool into seven types on a scale of 1–7 (hard to loose): 1 and 2 indicate constipation (hard stool), 3 and 4 the ideal stool and 5, 6 and 7 indicating loose and watery stool. The stool consistency improved significantly in the probiotic treated group of the functionally constipated subjects from the third week onwards. At week 3, B. coagulans Unique IS2 treated group had a mean stool score of 2.28 ± 0.60, whereas the mean score in placebo group was 2.06 ± 0.43 (p = 0.041). By week 4, the mean stool score in B. coagulans Unique IS2 treated group had increased to 3.02 ± 0.57, whereas in the placebo group, it was 2.65 ± 0.58 (p = 0.021) (Fig. 2b). There was thus an increase in the percentage of patients with normal stool in the B. coagulans unique IS2 treated group (Table 2) as compared to placebo group (98% vs. 74%).
Difficulty in Degree of Defecation and Sensation of Incomplete Evacuation (CSS Scale)
The sensation of incomplete evacuation was assessed through constipation scoring system (CSS) scale (Table S3). The CSS score ‘completeness: feeling incomplete evacuation’ score was a scale of 0–4 with higher CSS scores indicating more severe constipation (0, never; 1, rarely; 2, sometimes; 3, usually; and 4, always). In patients receiving B. coagulans Unique IS2 capsules, there was a significant decrease as compared to placebo in the feeling of incomplete evacuation as assessed by constipation scoring system. By visit 3, B. coagulans Unique IS2 treated group had a mean score of 1.32 ± 0.51 as compared to placebo which was 1.62 ± 0.73 (p = 0.019), and by visit 4, in the B. coagulans Unique IS2 treated group, the score had further dropped to 0.88 ± 0.39 as compared to placebo which was 1.04 ± 0.73 (p = 0.034) (Fig. 3a).
Defecation Pain (CSS Scale)
The severity of constipation symptom ‘difficulty: painful evacuation effort’ was assessed through CSS scale (Table S4). The CSS ‘difficulty: painful evacuation effort’ score was a scale of 0–4 with higher CSS scores indicating more severe pain (0, never; 1, rarely; 2, sometimes; 3, usually; and 4, always). By visit 3, B. coagulans Unique IS2 treated group had a mean score of 1.16 ± 0.58 as compared to placebo which was 1.50 ± 0.84 (p = 0.021), and by visit 4, in B. coagulans Unique IS2 treated group, the score had further dropped to 0.66 ± 0.52 as compared to placebo which was 0.98 ± 0.62 (p = 0.006) (Fig. 3b).
Abdominal Pain (CSS Scale)
The severity of constipation symptom ‘pain: abdominal pain’ was assessed through CSS scale (Table S5). The CSS ‘pain: abdominal pain’ score was a scale of 0–4 with higher CSS scores indicating more severe pain (0, never; 1, rarely; 2, sometimes; 3, usually; and 4, always). By visit 3, B. coagulans Unique IS2 treated group had a mean score of 0.94 ± 0.68 as compared to placebo which was 1.1 ± 0.84 (p = 0.038) and by visit 4, in B. coagulans Unique IS2 treated group, the score had further dropped to 0.38 ± 0.49 as compared to placebo which was 0.8 ± 0.81 (p = 0.002) (Fig. 4).
Adverse Events
No serious adverse events were observed during the trial. There were three patients from the placebo group who had reported mild adverse events during the study. One patient had mild fever (pyrexia) and two patients had reported headache from placebo group which the investigator had considered as not related to study drug. The vital parameters in both groups remained within normal and acceptable clinical range throughout the study duration (Table S6).
Discussion
In the present study, adults with functional constipation who received B. coagulans Unique IS2 capsules had improved bowel movements as compared to group fed with placebo. Probiotic capsules have an advantage over other forms of treatment in that they are generally safe and do not have any side effects [28]. There have been a few studies with other stains of B. coagulans in constipation. A clinical study with a limited number of subjects (20 healthy adults) on the effects of B. coagulans SANK 70258 (1 × 108 CFU/day for 2 weeks) on faecal properties and defecation frequency revealed that the ingestion of B. coagulans SANK 70258 in persons whose defecation frequency was relatively low led to an improvement of faecal shape, change of faecal colour from dark brown to yellowish brown, decrease of faecal odour and faecal pH, and an increase in defecation frequency [29]. The number of subjects, however, was too small to conclude on efficacy.
In another study, the effect of a Lilac LAB (B. coagulans lilac-01 and okara (soy pulp) powder) on bowel movements/faecal properties was studied through a double-blind placebo-controlled randomised trial on healthy Japanese volunteers with tendency for constipation (n = 297) [30]. The subjects in the test group ingested 2 g/day okara powder and B. coagulans Lilac LAB (1 × 108 CFU) once a day for 2 weeks. The placebo group was given okra powder only. In the test group of functionally constipated subjects, the changes in the average scores of self-reported faecal size, sensation of incomplete evacuation and defecation frequency were significantly improved compared to the placebo group (p < 0.05); faecal colour and odour also tended to improve (p = 0.07). The faecal size also tended to improve compared to the placebo group (p = 0.06 and p = 0.07, respectively) [30]. Lilac LAB was effective in improving bowel movements and faecal properties in functionally constipated persons. No clear-cut evidence on the efficacy of B. coagulans in constipation has been obtained as in the clinical studies conducted so far; either the sample size was too small or it was used in combination with a prebiotic [29, 30].
Members of the genera Lactobacillus and Bifidobacterium are well-investigated probiotics for functional constipation [31]. The administration of L. casei Shirota in patients (n = 35) with chronic constipation for 5 weeks resulted in significant (p < 0.003) improvement in defecation frequency and stool consistency as compared to placebo [32]. In another study, 2-week supplementation of either 1010 CFU/100 ml of Bifidobacterium animalis subsp. lactis GCL2505 or a milk product without bacteria as a placebo in patients (n = 17) with constipation significantly increased defecation frequency and the amount of stool [33]. Recently, Yoon et al. [34] showed that Streptococcus thermophilus MG510 and Lactobacillus plantarum LRCC5193 significantly improved stool consistency in patients with chronic constipation. A recent study, however, showed no significant effects of B. lactis DN-173010 and Lactobacillus casei rhamnosus Lcr35 on functional constipation when compared with placebo [35, 36].
The effects of probiotics are strain specific [37] and hence it was of importance to study the efficacy of B. coagulans Unique IS2 in the treatment of constipation. It is very important that the safety of the probiotic strain is established before it is recommended for human consumption [38]. Bacillus coagulans Unique IS2 is very well characterised with established probiotic properties [39], whole-genome sequencing and safety studies in rats (acute and repeat dose toxicity) have further established its safety [40, 41].
In the present investigation, we have shown that B. coagulans Unique IS2 (2 billion CFU) significantly improved the number of bowel movements per week and therefore helped ease constipation. There was also a significant improvement in the stool consistency and feeling of incomplete evacuation as compared to the placebo group with a decrease in abdominal pain and defecation pain from the third week onwards.
Conclusion
The present study suggests that B. coagulans Unique IS2, a clinically proven and safe probiotic, can be used in the treatment of constipation.
References
Suares NC, Ford AC (2011) Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol 106(9):1582–1591. https://doi.org/10.1038/ajg.2011.164
Dimidi E, Christodoulides S, Fragkos KC, Scott SM, Whelan K (2014) The effect of probiotics on functional constipation in adults: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr 100(4):1075–1084. https://doi.org/10.3945/ajcn.114.089151
Wald A, Scarpignato C, Kamm MA, Mueller-Lissner S, Helfrich I, Schuijt C, Bubeck J, Limoni C, Petrini O (2007) The burden of constipation on quality of life: results of a multinational survey. Aliment Pharmacol Ther 26:227–236. https://doi.org/10.1111/j.1365-2036.2007.03376.x
Dennison C, Prasad M, Lloyd A, Bhattacharyya SK, Dhawan R, Coyne K (2005) The health-related quality of life and economic burden of constipation. Pharmacoeconomics 23(5):461–476. https://doi.org/10.2165/00019053-200523050-00006
Lindberg G, Hamid SS, Malfertheiner P, Thomsen OO, Fernandez LB, Garisch J, Thomson A, Goh KL, Tandon R, Fedail S, Wong BC, Khan AG, Krabshuis JH, LeMair A (2011) World gastroenterology organisation global guideline: constipation—a global perspective. J Clin Gastroenterol 45(6):483–487. https://doi.org/10.1097/MCG.0b013e31820fb914
American college of gastroenterology chronic constipation task force (2005) An evidence-based approach to the management of chronic constipation in North America. Am J Gastroenterol 100(S1):S1–S4. https://doi.org/10.1111/j.1572-0241.2005.50613_1.x
Basilisco G, Coletta M (2013) Chronic constipation: a critical review. Dig Liver Dis 45(11):886–893. https://doi.org/10.1016/j.dld.2013.03.016
Johansen JF, Kralstein J (2007) Chronic constipation: a survey of the patient perspective. Aliment Pharmacol Ther 25(5):599–608. https://doi.org/10.1111/j.1365-2036.2006.03238.x
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, Morelli L, Canani RB, Flint HJ, Salminen S, Calder PC, Sanders MA (2014) The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol 11:506–514. https://doi.org/10.1038/nrgastro.2014.66
Lollo PC, Morato PN, Moura CS, Almada CN, Felicio TL, Esmerino EA, Barros ME, Amaya FJ, Sant'Ana AS, Raices RR, Silva MCC, Cruz AG (2015) Hypertension parameters are attenuated by the continuous consumption of probiotic Minas cheese. Food Res Int 76(3):611–617. https://doi.org/10.1016/j.foodres.2015.07.015
Moura CS, Lollo PC, Morato PN, Esmerino EA, Margalho LP, Santos-Junior VA, Coimbra PT, Cappato LP, Silva MC, Garcia-Gomes AS, Granato D, Bolini HMA, Sant’Ana AS, Cruz AG, Amaya-Farfan J (2016) Assessment of antioxidant activity, lipid profile, general biochemical and immune system responses of Wistar rats fed with dairy dessert containing Lactobacillus acidophilus La-5. Food Res Int 90:275–280. https://doi.org/10.1016/j.foodres.2016.10.042
Mostafai R, Nachvakc SM, Mohammadi R, Rocha RS, da Silva MC, Esmerino EA, Nascimento KO, Cruz AG, Mortazavian AM (2019) Effects of vitamin D-fortified yogurt in comparison to oral vitamin D supplement on hyperlipidemia in pre-diabetic patients: a randomized clinical trial. J Funct Foods 52:116–120. https://doi.org/10.1016/j.jff.2018.10.040
Sperry MF, Silva HL, Balthazar CF, Esmerino EA, Verruck S, Prudencio ES, Neto RP, Tavares MI, Peixoto JC, Nazzaro F, Rocha RS, Moraes J, Gomes ASG, Raices RSL, Silva MC, Granato D, Pimentel TC, Freitas MQ, Cruz AG (2018) Probiotic Minas Frescal cheese added with L. casei 01: physicochemical and bioactivity characterization and effects on hematological/biochemical parameters of hypertensive overweighted women–a randomized double-blind pilot trial. J Funct Foods 45:435–443. https://doi.org/10.1016/j.jff.2018.04.015
Martins AA, Santos-Junior VA, Filho ERT, Silva HLA, Ferreira MVS, Graça JS, Esmerino EA, Lollo PCB, Freitas MQ, Sant'Ana AS, Costa LEO, Raices RSL, Silva MC, Cruz AG, Barros ME (2018) Probiotic Prato cheese consumption attenuates development of renal calculi in animal model of urolithiasis. J Funct Foods 49:378–383. https://doi.org/10.1016/j.jff.2018.08.041
Ibarra A, Latreille-Barbier M, Donazzolo Y, Pelletier X, Ouwehand AC (2018) Effects of 28-day Bifidobacterium animalis subsp. lactis HN019 supplementation on colonic transit time and gastrointestinal symptoms in adults with functional constipation: a double-blind, randomized, placebo-controlled, and dose-ranging trial. Gut Microbes 9(3):236–251. https://doi.org/10.1080/19490976.2017.1412908
Kim SE, Choi SC, Park KS, Park MI, Shin JE, Lee TH, Jung KW, Koo HS, Myung SJ (2015) Change of fecal flora and effectiveness of the short-term VSL# 3 probiotic treatment in patients with functional constipation. J Neurogastroenterol Motil 21(1):111–120. https://doi.org/10.5056/jnm14048
Martínez-Martínez MI, Calabuig-Tolsa R, Cauli O (2017) The effect of probiotics as a treatment for constipation in elderly people: a systematic review. Arch Gerontol Geriatr 71:142–149. https://doi.org/10.1016/j.archger.2017.04.004
Miller LE, Zimmermann AK, Ouwehand AC (2016) Contemporary meta-analysis of short-term probiotic consumption on gastrointestinal transit. World J Gastroenterol 22(21):5122–5131. https://doi.org/10.3748/wjg.v22.i21.5122
Khalif IL, Quigley EMM, Konovitch EA, Maximova ID (2005) Alterations in the colonic flora and intestinal permeability and evidence of immune activation in chronic constipation. Dig Liver Dis 37(11):838–849. https://doi.org/10.1016/j.dld.2005.06.008
Zoppi G, Cinquetti M, Luciano A, Benini A, Muner A, Bertazzoni-Minelli E (1998) The intestinal ecosystem in chronic functional constipation. Acta Paediatr 87(8):836–841. https://doi.org/10.1111/j.1651-2227.1998.tb01547.x
Choi CH, Chang SK (2015) Alteration of gut microbiota and efficacy of probiotics in functional constipation. J Neurogastroenterol Motil 21(1):4–7. https://doi.org/10.5056/jnm14142
Champagne CP, Cruz AG, Daga M (2018) Strategies to improve the functionality of probiotics in supplements and foods. Curr Opin Food Sci 22:160–166. https://doi.org/10.1016/j.cofs.2018.04.008
Elshaghabee FMF, Rokana N, Gulhane RD, Sharma C, Panwar H (2017) Bacillus as potential probiotics: status, concerns, and future perspectives. Front Microbiol 8:1490. https://doi.org/10.3389/fmicb.2017.01490
Ahire JJ, Patil KP, Chaudhari BL, Chincholkar SB (2011) Bacillus spp. of human origin: a potential siderophoregenic probiotic bacteria. Appl Biochem Biotechnol 164(3):386–400. https://doi.org/10.1007/s12010-010-9142-6
Sudha RM, Bhonagiri S (2012) Efficacy of Bacillus coagulans strain unique IS-2 in the treatment of patients with acute diarrhea. Int J Probiotics Prebiotics 7(1):33–37
Sudha RM, Yelikar KA, Deshpande S (2012) Clinical study of Bacillus coagulans unique IS-2 (ATCC PTA-11748) in the treatment of patients with bacterial vaginosis. Indian J Microbiol 52(3):396–399. https://doi.org/10.1007/s12088-011-0233-z
Sudha MR, Jayanthi N, Aasin M, Dhanashri RD, Anirudh T (2018) Efficacy of Bacillus coagulans unique IS2 in treatment of irritable bowel syndrome in children: a double blind, randomised placebo controlled study. Benefic Microbes 9(4):563–572. https://doi.org/10.3920/BM2017.0129
Govender M, Choonara YE, Kumar P, du Toit LC, van Vuuren S, Pillay V (2014) A review of the advancements in probiotic delivery: conventional vs. non-conventional formulations for intestinal flora supplementation. AAPS PharmSciTech 15(1):29–43. https://doi.org/10.1208/s12249-013-0027-1
Ara K, Meguro S, Hase T, Tokimitsu I, Otsuji K, Kawai S, Ito S, Iino H (2002) Effect of spore-bearing lactic acid-forming bacteria (Bacillus coagulans SANK 70258) administration on the intestinal environment, defecation frequency, fecal characteristics and dermal characteristics in humans and rats. Microb Ecol Health Dis 14(1):4–13. https://doi.org/10.1080/089106002760002694
Minamida K, Nishimura M, Miwa K, Nishihira J (2015) Effects of dietary fiber with Bacillus coagulans lilac-01 on bowel movement and fecal properties of healthy volunteers with a tendency for constipation. Biosci Biotechnol Biochem 79(2):300–306. https://doi.org/10.1080/09168451.2014.972331
Ohkusa T, Koido S, Nishikawa Y, Sato N (2019) Gut microbiota and chronic constipation: a review and update. Front Med 6:19. https://doi.org/10.3389/fmed.2019.00019
Koebnick C, Wagner I, Leitzmann P, Stern U, Zunft HJ (2003) Probiotic beverage containing Lactobacillus casei Shirota improves gastrointestinal symptoms in patients with chronic constipation. Can J Gastroenterol 17(11):655–659. https://doi.org/10.1155/2003/654907
Ishizuka A, Tomizuka K, Aoki R, Nishijima T, Saito Y, Inoue R, Ushida K, Mawatari T, Ikeda T (2012) Effects of administration of Bifidobacterium animalis subsp. lactis GCL2505 on defecation frequency and bifidobacterial microbiota composition in humans. J Biosci Bioeng 113(5):587–591. https://doi.org/10.1016/j.jbiosc.2011.12.016
Yoon JY, Cha JM, Oh JK, Tan PL, Kim SH, Kwak MS, Jeon JW, Shin HP (2018) Probiotics ameliorate stool consistency in patients with chronic constipation: a randomized, double-blind, placebo-controlled study. Dig Dis Sci 63(10):2754–2764. https://doi.org/10.1007/s10620-018-5139-8
Tabbers MM, Chmielewska A, Roseboom MG, Crastes N, Perrin C, Reitsma JB, Szajewska H (2011) Benninga MA (2011) fermented milk containing Bifidobacterium lactis DN-173 010 in childhood constipation: a randomized, double-blind, controlled trial. Pediatrics 127(6):e1392–e1399. https://doi.org/10.1542/peds.2010-2590
Wojtyniak K, Horvath A, Dziechciarz P, Szajewska H (2017) Lactobacillus casei rhamnosus Lcr35 in the management of functional constipation in children: a randomized trial. J Pediatr 184:101–105. https://doi.org/10.1016/j.jpeds.2017.01.068
McFarland LV, Evans CT, Goldstein EJC (2018) Strain-specificity and disease-specificity of probiotic efficacy: a systematic review and meta-analysis. Front Med 5:124. https://doi.org/10.3389/fmed.2018.00124
Saarela MH (2018) Safety aspects of next generation probiotics. Curr Opin Food Sci 30:8–13. https://doi.org/10.1016/j.cofs.2018.09.001
Ratna Sudha M, Chauhan P, Dixit K, Babu S, Jamil K (2010) Molecular typing and probiotic attributes of a new strain of Bacillus coagulans–unique IS2: a potential biotherapeutic agent. Genet Eng Biotechnol J 7:1–20
Upadrasta A, Pitta S, Madempudi RS (2016) Draft genome sequence of the spore-forming probiotic strain Bacillus coagulans unique IS2. Genome Announc 4(2):e00225–e00216. https://doi.org/10.1128/genomeA.00225-16
Sudha RM, Sunita M, Sekhar BM (2016) Safety studies of Bacillus coagulans unique IS2 in rats: morphological, biochemical and clinical evaluations. Int J Probiotics Prebiotics 11:43
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was conducted in compliance with the code of conduct for research involving human volunteers as issued by the International Conference on Harmonisation–Good Clinical Practice (ICH-GCP), Indian Council of Medical Research guidelines (ICMR; ethical guidelines for biomedical research on human subjects) and the principles of the Declaration of Helsinki. Informed consent forms were approved by the ethical committees of study sites and the trial was registered prospectively with the clinical trial registry of India (CTRI/2017/11/010539). The study was initiated after obtaining informed consent.
Competing Interests
R.S.M., J.N. and J.J.A. are employed by Unique Biotech Ltd. which is a manufacturer of probiotics. They wish to state that the study was conducted independently with no intervention on their part during the duration of the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 26 kb)
Rights and permissions
About this article
Cite this article
Madempudi, R.S., Neelamraju, J., Ahire, J.J. et al. Bacillus coagulans Unique IS2 in Constipation: A Double-Blind, Placebo-Controlled Study. Probiotics & Antimicro. Prot. 12, 335–342 (2020). https://doi.org/10.1007/s12602-019-09542-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-019-09542-9