Abstract
Distal radius fractures are increasingly treated by internal fixation, but there have been relatively few studies relating to functional outcome at 12 months or more. The aim of this study was to ascertain the patient reported function of the wrist at a minimum of 12 months following fixation of a distal radius fracture, the time taken to return to work, and the complication rate. We conducted a retrospective review of 187 consecutive patients treated by a specialist hand and wrist trauma team at a tertiary referral unit over a 5 year period. Mean age was 57.3 years (range 16–93). Median time to surgery was 4 days (interquartile range 2–9). Median follow up was 31 months (interquartile range 23–41 months). The median PRWE score was 3; (range 0–83). There was no difference in outcome in patients who had surgery delayed by greater than 2 weeks (p > 0.05). The median time to return to work was 5 weeks (interquartile range 1–8 weeks). There were 15 complications (8 %) including 3 tendon injuries. We have demonstrated an early return to work in patients who were employed, a low complication rate, and highly favourable functional outcomes at a mean of 30 months postoperatively. We recommend the use of the DVR plate and involvement of a dedicated hand and wrist trauma team for treatment of unstable fractures of the distal radius.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the distal radius are common injuries [1] with displaced and/or intra-articular fractures with joint incongruence frequently requiring operative fixation to achieve a good outcome. A range of treatment options are available to surgeons, most commonly including closed reduction and application of cast, percutaneous wire fixation [2], external fixation [3–5], and open reduction and internal fixation [6–8]. There has been debate as to the ideal treatment modality in unstable injuries as no clear evidence for any one treatment has been demonstrated.
In recent years there has been a shift towards anatomically contoured volar locking plates, which have the advantage of providing metaphyseal fixation with the implant residing on the concave volar surface of the distal radius. Placement at this site reduces the risk of dorsal soft tissue irritation previously seen in dorsal plating systems (e.g. Pi, dorsal, columnar) and makes use of an anatomical recess, which reduces the risk of flexor tendon irritation.
Good clinical results have been reported with volar locking plate devices [6, 7]. Furthermore, comparative clinical data examining the use of locking plate devices versus percutaneous treatment [9] and external fixation [10] has also been favourable, demonstrating an earlier return to a higher level of function. A number of authors have examined the biomechanical advantages of volar plating over other devices, also with favourable results [11–14].
There are relatively few studies in the literature relating to results of treatment by dedicated hand trauma teams. The more widespread use of volar locking plates and an increase in the volume of fractures being treated with internal fixation has lead to hand surgeons performing this procedure with increased frequency. It was noted in our unit that the complication rate following internal fixation of distal radius fracture was lower than that reported in the literature, and many patients were achieving an early return to work, highly satisfied with their outcome and with good level of function. The aim of this study was to ascertain the patient reported function of the wrist at a minimum of 12 months following fixation of a distal radius fracture, the time taken to return to work, and the complication rate, in patients treated exclusively by hand surgeons in a specialist hand and wrist trauma unit.
Methods
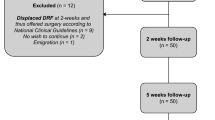
We retrospectively reviewed the first 259 consecutive patients presenting with an unstable fracture of the distal radius to the Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry, UK, treated by internal fixation using a volar locking plate. Inclusion criteria for this study included adult patients, fracture of the distal end of the radius, no contraindications to surgery. Fractures were deemed unstable if there was significant dorsal comminution, if there was a displaced intra-articular component to the fracture, or if closed reduction and cast application had been attempted but failed or had re-displaced. Patients meeting these criteria underwent fixation with a volar locking plate (DVR plate, Biomet, Bridgend, UK - see Fig. 1). A small number of patients underwent fixation with an alternative implant if there was extensive diaphyseal involvement or if the correct size or side DVR plate were not available. Exclusion criteria included fractures fixed with another implant, fractures of the radial shaft and patients not treated by the hand and wrist team.
All patients were admitted via the hand and wrist trauma clinic at our institution, or as tertiary referrals from other hospitals within the region. Decision to manage injuries with internal fixation was made by a consultant surgeon and patients were operated on the next available operating list. Patients with 3 of the following criteria were offered surgery: a significant articular step (2 mm or greater), significant dorsal comminution, dorsal angulation greater than 20°, ulna styloid fracture and age greater than 60. Most patients were treated within 2 weeks of injury unless other circumstances prevented this (e.g. late presentation, unavailable operating list, secondary procedure after failure of primary procedure). All procedures were conducted by, or under the supervision of, one of the consultant orthopaedic surgeons with a specialist interest in hand surgery.
Patients were counselled preoperatively by a member of the surgical team regarding the risks and benefits of surgery, and informed consent was obtained. The procedure was performed under general anaesthesia or regional anaesthesia, under tourniquet control at 250 mmHg, with patients supine and the arm on an arm-table.
All patients underwent fixation via a volar approach (see Fig. 2), using the flexor carpi radialis (FCR) approach described by Orbay [15]. Having exposed the distal radius, the metaphyseal fracture fragments were denuded sufficiently to allow anatomical reduction. This was generally performed by elevation of the periosteum across to the sigmoid notch and to the radial side to expose and subsequently reduce separate radial styloid fragments. Release of the brachioradialis tendon was performed as necessary to facilitate reduction of radial translation of the metaphysis or of a separate radial styloid fragment.
a The FCR approach using a longitudinal incision over the FCR tendon. b FCR tendon is retracted ulnarward and the deep fascia is divided. c The flexor compartment musculature is bluntly swept ulnarward. d The pronator quadratus is then incised in an L shape along the watershed line to reveal the metaphyseal fragments. e An approprately sized plate is selected and its size and position checked fluoroscopically. f Metaphyseal fixation is achieved initially and the plate used to lever the distal fragment down to restore volar tilt
The metaphyseal region was fixed to the plate first, to allow levering down of the fracture fragments before fixation to the shaft, facilitating restoration of volar tilt (see Fig. 3). This was also done with initial K wire fixation to the plate of all main fragments, followed by metaphyseal peg insertion. After fluoroscopic check of plate and screw placement relative to the wrist, the plate and metaphysis were subsequently levered down to the level of the shaft and secured with screws using eccentric drilling of the direct compression holes to increase radial length as required. After a further fluoroscopic check, to ensure adequate restoration of anatomy, including both length and metaphyseal tilt, final shaft screws were subsequently inserted. As a rule, unicortical drilling of the metaphysis was used in all cases to prevent extensor tendon damage.
Following skin closure a dorsal plaster of paris (POP) splint was applied and patients were discharged when comfortable the following morning. On occasion patients were discharged the same day if they were operated on in the morning and were comfortable later that day. All patients were seen prior to discharge by a member of the hand therapy team and given a series of passive and active movements of the fingers, and advice regarding elevation in the initial postoperative period and the need for compliance with rehabilitation protocol to gain an optimal outcome. POP splints were removed at 2 weeks for wound examination, and a removable wrist splint was then applied until the 6 week clinical review.
Patients were followed up clinically at 6 and 12 weeks, and at 6 months and 1 year. Data relating regarding return to work and early complications were compiled prospectively. Patients were subsequently sent a questionnaire at the time of conducting this study including a patient related wrist evaluation (PRWE) questionnaire, a patient satisfaction score, and questionnaire relating to any complications that may have occurred between clinic discharge and the questionnaire being sent. Data were compiled and statistics were calculated using Microsoft Excel.
Results
259 patients were initially included in the study, of which 187 responses were received for the questionnaire. The response rate was 72.2 %. The patients who did not respond to postal questionnaire were subsequently excluded from the study. The 72 patients excluded from the study were of comparable age and sex distribution.
The mean age of the patients was 57.3 years (Range 16–93). The median inpatient stay was 1 day, (range 1–6, mode 1 day). Median time to surgery was 4 days (interquartile range 2–9). Median follow up was 31 months (interquartile range 23–41 months). Using the AO classification, 56/187 injuries were type A3, 4/187 type B1, 15/187 type B2, 19/187 type C1, 41/187 type C2, and 52/187 were type C3 (see Table 1).
The mean PRWE score at the time of follow up questionnaire was 12.2 (range 0–86; standard deviation 19.29). Median PRWE score was 3 (see Fig. 4).126/187 patients had an excellent outcome (PRWE score ≤10, 67 % 16/187 had a satisfactory score (PRWE score 11–20, 9 %), and 45/187 achieved a poor score (PRWE >20; 24 %) (see Table 2). A total of 14 patients experienced a delay between injury and surgery of greater than 14 days. In these patients, mean PRWE was 26 (range 0–90). There was no significant difference in PRWE score between delayed patients and those operated on within 14 days (Mann Whitney U; p = 0.9). 71 out of 78 patients (91 %) returned to the same means of employment as before surgery. Of the patients who were returning to work, the median time to return to work was 5 weeks (interquartile range 1–8 weeks). There was no difference in outcome in patients who had surgery delayed by greater than 2 weeks (p > 0.05).
There were 15 complications in total (8 %). Six (3.8 %) patients had extensor tendon irritation, of which two patients required surgery using an extensor indicis proprius transfer. One further patient had a spontaneous EPL rupture, which was not associated with prominent metal work, also requiring tendon transfer. Five (2.7 %) patients had symptoms relating to median nerve compression postoperatively. Of these, two patients underwent carpal tunnel decompression with complete resolution of symptoms. The other three settled spontaneously. Two (1.2 %) patients developed Complex Regional Pain Syndrome (CRPS), requiring referral to a pain management clinic and additional physiotherapy, which settled within 6 months. One patient developed a minor superficial wound infection.
In all, 11 (5.9 %) patients had removal of their metalwork, 6 for tendon irritation, 4 for wrist stiffness, and 1 for peg penetration into the joint.
A casenote review of patients excluded from the study revealed a satisfactory outcome in 54/72, who were discharged after 12 weeks. A further 2 patients were listed for plate removal due to stiffness and 1 underwent carpal tunnel release due to due symtoms of persistent median nerve compression. The remaining 15 cases had no available records due to non-attendance or follow up elsewhere.
Discussion
A number of authors have reported good results following internal fixation of the distal radius using this technique. Orbay and Fernandez [16], in their original series of 31 fractures in 29 patients reported excellent results in 19 and good in 12 according to Garland and Werley functional scales, at a mean follow up time of 12.5 months postoperatively. In a further study reviewing outcomes in an elderly patient group aged over 75 years, similarly good clinical data was reported, with final mean range of motion (mean) of 58° dorsiflexion, 55° volar flexion, 80° pronation and 76° supination [17]. Ibrahim et al. treated 129 patients treated with a DVR plate for dorsally displaced distal radius fractures the authors noted a comparative ROM of 70 %, 88 %, and 98 % compared with the contralateral side at 6, 12 and 26 weeks postoperatively. The mean PRWE score demonstrated only minimal disability at 26 weeks [18]. The present study, which has the largest study population treated with a DVR plate analysed to date, with the longest follow up time, shows comparable results, with the majority of patients scoring 0–10 on PRWE. It is worth noting that the mean time taken to return to work, in patients who were employed, is shorter in the present series than most in the literature. Furthermore, few studies have reported outcomes at greater than 12 months, and our data demonstrate that good results appear to be maintained for considerably longer than 12 months, which is the follow up time seen most commonly in comparable studies. Several other authors have reported good clinical outcomes, but without reporting on return to work [19, 20].
Despite positive results for internal fixation, debate exists as to whether this technique represents first line treatment for displaced, unstable fractures. Marcheix compared palmar fixed angle locking plate fixation to Kirshner wire fixation in a prospective randomized trial, reporting improved functional results (DASH and Herzog scores), with a plate, with better maintenance of reduction [21]. However, equivalent functional scores have also been reported when comparing locking plate fixation to external fixation [22, 23], or to conservative treatment [24]. The latter of these studies, however, was in an elderly group of patients. We have shown in the present study that internal fixation following distal radius fractures allows a return to a normal, or near normal, level of function in approximately 6 weeks with a return to work at a mean of 40 days.
The complication rate following locked volar plating of distal radius fractures is variable. Bentohami et al. have reported an overall complication rate of 16.5 %, in a systemic review of outcomes and complications following DRF fixation. [25]. We have noted an incidence of complications of 8 %, reflecting a low overall complication rate owing to a lack of flexor tendon injuries and a lower rate of CRPS than other studies. Flexor tendon injury following DRF fixation has been reported by various authors [25–27] with prominence of the plate and poor implant placement implicated in the aetiology of this complication [28–30]. In the present series we have noted an incidence of flexor tendon injury of 0 % at a mean follow up time of 30 months and a minimum of 12. It is worth noting that with a response rate of 72.2 % some cases may have been missed due to the methodology of the study. However, in our opinion, the absence of flexor tendon problems in the 187 cases studied is likely to be a reflection of the plate design, and accurate positioning intra-operatively. The DVR plate has a thin distal metaphyseal edge which sits up to the watershed line in the concavity of the volar metaphysis of the distal radius, ensuring little or no implant prominence if the implant is positioned correctly.
We have seen an incidence of extensor tendon injury of 3.8 %, which is lower than figures reported in the literature. Al-Rashid et al. [31] reported an incidence of extensor tendon rupture of 8.6 % of 35 cases (three cases) treated with an AO volar locking plate, citing screw penetration of the dorsal cortex and careless drilling technique as principle causes. Other authors reporting extensor tendon irritation and ruptures have cited similar reasons [32–35]. It is worth noting that extensor tendon injury has also been reported in 5 % of undisplaced distal radius fractures, most likely due to extensor irritation over dorsal callus formation [36]. The cases we have seen with extensor ruptures in this study both had prominent pegs at the level of the dorsal cortex. A third spontaneous rupture was seen, not relating to prominent hardware, which may be related to irregular dorsal cortical bone during fracture healing or due to a vascular insult at the time of injury. The lower incidence of extensor problems in the present study is likely to be reflection of our default operative technique, with unicortical drilling of the metaphysis and careful measurement of screw length, ensuring minimal risk of extensor compartment penetration by either drill bit or screw. Despite the policy of unicortical drilling, two extensor tendon injuries were seen in relation to prominent pegs dorsally, which highlights the need for great care both when drilling and when measuring peg/ screw length.
The relatively low percentage of cases complicated by CRPS (1.2 %) postoperatively is likely to be due to the early mobilisation and involvement of dedicated hand therapists from the immediate postoperative period. All cases were operated on by surgeons with a subspecialty interest in hand and wrist trauma, and it is also likely that efficient technique and careful handling of tissues contributed to the low incidence of CRPS.
We acknowledge a number of clear limitations to our study. The retrospective design of a questionnaire study has meant that a higher proportion of cases than we hoped were lost to follow up. Additionally, this has meant that functional outcomes have been assessed using a patient assessed outcome measure, which in turn has resulted in a loss some objectivity in data collection, as well as the loss of accurate measurement of range of movement data. However, in our opinion, accurate representation of wrist motion is of limited relevance, as a return to normal activity and function is of greater importance, both reported here. Moreover, the functional results seen in this study are highly favourable, at a mean follow up time which is amongst the longest in the literature. The absence of a control group in the study has also limited the conclusion that can be drawn, and further prospective and comparative studies are needed to ascertain whether dedicated hand and wrist trauma teams achieve improved outcomes compared to general trauma teams.
We recommend involvement hand and wrist surgery teams and attention to unicortical drilling and correct plate placement in the operative treatment of unstable distal radius fractures. With this strategy we have shown a favourable complication rate and excellent functional outcomes, with an expeditious return to work in those who are employed, compared with other studies reported in the literature.
References
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37:691–697
Handoll HH, Vaghela MV, Madhok R (2007) Percutaneous pinning for treating distal radial fractures in adults. Cochrane Database Syst Rev 18:CD006080
Cui Z, Yu B, Hu Y, Lin Q, Wang B (2012) Dynamic versus static external fixation for unstable distal radius fractures: an up-to-date meta-analysis. Injury 43:1006–1013
McQueen MM (2005) Non-spanning external fixation of the distal radius. Hand Clin 21:375–380
Hayes AJ, Duffy PJ, McQueen MM (2008) Bridging and non-bridging external fixation in the treatment of unstable fractures of the distal radius: a retrospective study of 588 patients. Acta Orthop 79:540–547
Figl M, Weninger P, Liska M, Hofbauer M, Leixnering M (2009) Volar fixed-angle plate osteosynthesis of unstable distal radius fractures: 12 months results. Arch Orthop Trauma Surg 129:661–669
Osada D, Kamei S, Masuzaki K, Takai M, Kameda M, Tamai K (2008) Prospective study of distal radius fractures treated with a volar locking plate system. J Hand Surg [Am] 33:691–700
Rozental TD, Blazar PE (2006) Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg [Am] 31:359–365
Rozental TD, Blazar PE, Franko OI, Chacko AT, Earp BE, Day CS (2009) Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am 91:1837–1846
Grewal R, MacDermaid JC, King GJ, Faber KJ (2011) Open reduction and internal fixation versus percutaneous pinning with external fixation of distal radius fractures: a prospective, randomized clinical trial. J Hand Surg [Am] 36:1899–1906
Dahl WJ, Nassab PF, Burgess KM, Postak PD, Evans PJ, Seitz WH, Greenwald AS, Lawton JN (2012) Biomechanical properties of fixed-angle volar distal radius plates under dynamic loading. J Hand Surg [Am] 37:1381–1387
Klos K, Rausch S, Loffler M, Frober R, Hofmeier K, Lenz M, Hofmann GO, Muckley T (2010) A biomechanical comparison of a biodegradable volar locked plate with two titanium volar locked plates in a distal radius fracture model. J Trauma 68:984–991
Sobky K, Baldini T, Thomas K, Bach J et al (2007) Biomechanical comparison of different volar fracture fixation plates for distal radius fractures. Hand 3:96–101
Strauss EJ, Banerjee D, Kummer FJ, Tejwani NC (2008) Evaluation of a novel, nonspanning external fixator for treatment of unstable extra-articular fractures of the distal radius: biomechanical comparison with a volar locking plate. J Trauma 64:975–981
Orbay JL, Badia A, Indriago IR, Infante A et al (2005) The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech Hand Upper Extrem Surg 5:204–211
Orbay JL, Fernandez DL (2002) Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg [Am] 27:205–215
Orbay JL, Fernandez DL (2004) Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg [Am] 29:96–102
Ibrahim I, Alsey K, Naqui SZ, Pendlebury G, Warner J (2012) Short term outcomes following distal volar radial (DVR) plating of distal radius fractures. J Bone Joint Surg Br 94; SUPPIV: 142
Lazano-Calderon SA, Souer S, Mudgal C, Jupiter J, Ring D (2008) Wrist mobilization following volar plate fixation of fractures of the distal part of the radius. J Bone Joint Surg Am 90:1297–1304
Tarallo L, Adani R, Mugnai R, Catani F (2011) The treatment of distal radius articular fractures of C1-C2 type with DVR plate: analysis of 40 cases. Musculoskelet Surg 95:225–230
Marcheix PS, Dotzis A, Benko PE, Siegler J, Arnaud JP, Charissoux JL (2010) Extension fractures of the distal radius in patients older than 50: a prospective randomized study comparing fixation using mixed pins or a palmar fixed-angle plate. J Hand Surg Eur 35:646–651
Pino S, Bonilla JC, BOrras JE, Punet E, Vila J, Hernandez JA (2011) Comparative study of distal radius fracture treated with volar plate or external fixation. J Bone Joint Surg Br 93; SUPPII: 169
Wilcke M, Abbaszadegan H, Adolphson P (2011) Wrist function recovers more rapidly after volar locked plating than after external fixation but the outcomes are similar after 1 year. Acta Orthop 82:76–81
Arora R, Lutz M, Deml C, Krappinger D et al (2011) A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am 93:2146–2153
Bentohami A, de Burlet K, de Korte N, van den Bekerom MP, Goslings JC, Schep NW (2013) Complications following volar locking plate fixation for distal radial fractures: a systematic review. J Hand Surg Eur
Valbuena SE, Cogswell LK, Baraziol R, Vealenti P (2010) Rupture of flexor tendon following volar plate of distal radius fracture. Report of five cases. Chir Main 29:109–113
Casaletto JA, Machin D, Leung R, Brown DJ (2009) Flexor pollicis longus tendon ruptures after palmar plate fixation of fractures of the distal radius. J Hand Surg Eur 34:471–474
Imatani J, Akita K, Yamaguchi K, Shimizu H, Kondou H, Ozaki T (2012) An anatomical study of the watershed line on the volar distal aspect of the radius: implications for plate placement and avoidance of tendon ruptures. J Hand Surg [Am] 37:1550–1554
Matityahu AM, Lapalme SN, Seth A, Marmor MT, Buckley JM, Lattanza LL (2013) How placement affects force and contact pressure between a volar plate of the distal radius and the flexor pollicis longus tendon: a biomechanical investigation. J Hand Surg Eur 38:144–150
Soong M, van Leerdam R, Guitton TG, Got C, Katarincic J, Ring D (2011) Fracture of the distal radius: risk factors for complications after locked volar plate fixation. J Hand Surg [Am] 36:3–9
Al-Rashid M, Theivandran K, Craigen MAC (2006) Delayed ruptures of the extensor tendon secondary to the use of volar locking compression plates for distal radius fractures. J Bone Joint Surg (Br) 88:1610–1612
Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabi M (2007) Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma 21:316–322
Benson EC, DeCarvalho A, Mikola EA, Veith JM, Moneim MS (2006) Two potential causes of EPL rupture after distal radius volar plate fixation. Clin Orthop Relat Res 451:218–222
Falla JM, Koniuch MP, Moed BR (1993) Extensor pollicis longus rupture at the tip of a prominent fixation screw: report of three cases. J Hand Surg [Am] 18:648–651
Perry DC, Machin DM, Casaletto JA, Brown DJ (2011) Minimising the risk of extensor pollicis longus rupture following volar plate fixation of distal radius fractures: a cadaveric study. Ann R Coll Surg Engl 93:57–60
Roth KM, Blazar PE, Earp BE, Han R, Leung A (2012) Incidence of extensor pollicis longus tendon rupture after nondisplaced distal radius fractures. J Hand Surg [Am] 37:942–947
Statement of Ethical Standards
All human studies were approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons included in the study gave their informed consent prior to their inclusion.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
MacFarlane, R.J., Miller, D., Wilson, L. et al. Functional Outcome and Complications at 2.5 Years Following Volar Locking Plate Fixation of Distal Radius Fractures. J Hand Microsurg 7, 18–24 (2015). https://doi.org/10.1007/s12593-014-0155-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12593-014-0155-1