Abstract
Myocardial strain measurement with two-dimensional speckle-tracking echocardiography (2D-STE) is of paramount importance in the early detection of subclinical left ventricular (LV) systolic dysfunction and the prediction of patient outcomes in various types of heart disease, especially when assessed with global longitudinal strain (GLS). The routine application of myocardial strain parameters requires the definition of normal values and an understanding of their reliabilities. One of the most important potential limitations to widespread clinical application of this technique is inter-vendor differences in normal strain values. Recent clinical reports indicate that the smallest differences were noted in GLS measurements among three orthogonal directions. Because the contribution of circumferential fibers to LV myocardial thickening is greater than that of longitudinal fibers, patients who have a reduced LV ejection fraction can have impaired global circumferential strain (GCS), which reflects more advanced intrinsic myocardial systolic dysfunction and is thus closely related to a poor prognosis. Since STE-derived strain analysis allows us to define the timing of the regional myocardial peak systolic deformation, it permits the assessment of LV mechanical dyssynchrony. The severity of LV mechanical dyssynchrony in the short axis plane, i.e., radial and/or circumferential strain imaging, is favorable for predicting the clinical response to cardiac resynchronization therapy. GLS in the right ventricular (RV) four-chamber view has recently been used as a surrogate for global RV function because longitudinal shortening is the major contributor to overall RV performance. Finally, 2D-STE can be used to quantify and characterize RV mechanical dyssynchrony in various diseases including acute pulmonary thromboembolism and chronic pulmonary hypertension.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Left ventricular ejection fraction (LVEF) has been widely used to define systolic function, assess prognosis, and select patients for therapeutic interventions. However, it gives limited insight into direction-based myocardial systolic function. Two-dimensional (2D) speckle tracking echocardiography (STE) is a non-Doppler, and thereby angle-independent technique based on frame-by-frame tracking of tiny echo-dense speckles within the myocardium, with subsequent measurement of myocardial motion and deformation. Strain is used to describe local shortening and lengthening of the myocardium as a measure of regional myocardial function in the longitudinal, circumferential, and radial directions. Speckle-tracking technology analyzes Lagrangian strain, in which the end-diastolic tissue dimension represents the unstressed, initial material length as a fixed reference throughout the cardiac cycle (Fig. 1). The accuracy, validity and clinical applications of STE-derived strain measurement have rapidly been accumulating since its introduction. Especially, global longitudinal strain (GLS) has emerged as a more sensitive index of myocardial systolic function than LVEF. The superior prognostic value of GLS over either LVEF or wall motion score index in various heart diseases with a wide range of LVEFs has been reported. STE can also be applied to analyzing right ventricular (RV) myocardial deformation. Since longitudinal shortening is the major contributor to overall RV performance, GLS in the RV four-chamber view has recently been used as a surrogate for global RV function and as a predictor of the clinical outcomes of patients with various heart diseases.
Examples of strain images (top) and time-strain curves (bottom) from a normal subject in the longitudinal (left), circumferential (middle) and radial directions (right). A six-segment model of the left ventricle is created by the tracking algorithm after manual delineation of the endocardial border. White dotted lines in the time-strain curves indicate global longitudinal (bottom left) and circumferential (bottom center) strain
STE-derived strain analysis has another important advantage over conventional eye-ball or LVEF-derived functional assessments. Time-strain curves allow physicians to assess timing of the regional myocardial peak systole deformation, and therefore enable the assessment of mechanical dyssynchrony in both the left and right ventricles.
The present review focused on the physiology of myocardial strain and the technical features of strain imaging using STE, considering their strengths and weaknesses in the assessment of various heart diseases and potential future clinical applications.
Normal strain values
The routine application of myocardial strain parameters in clinical practice requires the definition of a normal range and understanding of its reliability. Yingchoncharoen et al. performed a meta-analysis of 24 eligible articles including 28 valid datasets published between 2009 and 2011, and found that the reported normal GLS (n = 2,597) was −19.7 % [95 % confidence interval (CI) −20.4 to −18.9 %], normal GCS (n = 599) was −23.3 % (95 % CI −24.6 to −22.1 %) and normal GRS (n = 568) was 47.3 % (95 % CI 43.6–51.0 %) [1], indicating narrower normal variations in GLS and GCS than in GRS.
One of the most important potential limitations to widespread clinical application of this technique is inter-vendor differences in normal strain values, as highlighted by several investigators. Takigiku et al. determined the normal range of 2D-STE-derived LV strain and their vendor-specific differences in a multicenter prospective study in 817 Japanese healthy subjects (age range 0–88 years) using an ultrasound system from one of the three different vendors [2]. They showed that the normal values of GLS (Vendor 1: −21.3 ± 2.1 %, Vendor 2: −18.9 ± 2.5 % and Vendor 3: −19.9 ± 2.4 %), GCS (Vendor 1: −22.8 ± 2.9 %, Vendor 2: −22.2 ± 3.2 % and Vendor 3: −30.5 ± 3.8 %) and GRS (Vendor 1: 54.6 ± 12.6 %, Vendor 2: 36.3 ± 8.2 % and Vendor 3: 51.4 ± 8.0 %) were significantly different between the three vendors with the smallest differences in GLS measurements. They also demonstrated that the feasibility for strain measurements was also different among the three vendors (Vendor 1: 83 %, Vendor 2: 70 % and Vendor 3: 88 %, p < 0.01). Very recently, Farsalinos et al. demonstrated that the absolute differences in 62 volunteers between nine different vendors for average GLS value were up to 3.7 and 3.5 % strain units from the average of two or three apical views (GLSAV) and from the four-chamber view (GLS4CH), respectively [3]. They also found that intra- and inter-observer relative mean errors were lower than those for LVEF and most other conventional echocardiographic parameters. In view of these recent findings, 2D-STE-derived strain, especially GLS, can be safely used in routine clinical practice, but the system and software from the same vendor should be used for longitudinal follow-up in the same patients. As the left ventricle is composed of 3 myocardial layers (inner layer, mid-wall layer and outer layer), the degree of transmural gradient of systolic strain and the layer-to-layer interactions can be different among the three orthogonal directions, which may contribute to the direction-specific differences in the extent of inter-vendor variation.
Age and gender differences
Age- and gender-differences in cardiac structure and LV diastolic function are well recognized in healthy subjects. Sun et al. reported that GLS became less negative with aging, while the GCS became more negative and the GRS remained unchanged [4]. Zghal et al. reported that GLS was less negative in elderly subjects (75–95 years) than in young subjects (17–45 years) but there was no significant change in GCS and GRS [5]. It is assumed that GLS can be much more sensitive to aging-associated changes in LV systolic function than GCS and GRS.
Recently, Cheng et al. performed 2D-STE examinations in 793 healthy adults (64 % women) between 45 and 84 years of age, and found that women had 1.7 % greater GLS (p < 0.0001), 3.2 % greater GCS (p < 0.0001) and 2.9 % greater GRS (p = 0.024) compared with men in multivariate analyses [6]. Interestingly, the result from the HUNT-study showed that myocardial deformation was consistently higher in women, except in the group of participants aged >60 years [7]. It is well recognized that parameters of early LV diastolic relaxation assessed by mitral inflow and mitral annular velocities decline with age, and women have greater LV relaxation than men until the menopause. As LV relaxation occurs in a series of energy-consuming steps and is physiologically coupled to contraction [8], the age and gender-related differences in indices of LV myocardial systolic strain values shown in these studies make good sense from a pathophysiological perspective.
Subclinical heart disease and heart failure with preserved LVEF
The myocardial fibers are roughly longitudinally oriented in the subendocardium, and therefore GLS strongly reflects subendocardial function. Since the subendocardium is often the earliest myocardial layer affected in many disease processes, GLS is the most sensitive marker of subclinical or latent LV systolic dysfunction. Hypertension and diabetes mellitus (DM) induce progressive impairment of longitudinal shortening and play important roles in the development of heart failure (HF), with a complex interplay. Ishizu et al. measured LV GLS and GCS using 2D-STE in Dahl salt-sensitive rats during the full time course of disease development, and demonstrated that progressive impairment of GLS occurred from an early stage in parallel to the subendocardial fibrosis, and that abnormality of GLS was associated with chamber diastolic stiffness [9]. Enomoto et al. demonstrated that GLS was significantly impaired in normotensive patients with type-2 DM, and that blood pressure and body mass index were independently associated with reduced GLS in those patients [10].
Hypertension, DM, and aging are the most common causes of HF with preserved ejection fraction (HFpEF), which is a prevalent and growing public health problem associated with significant morbidity and increased risks of in-hospital, short-term, and long-term mortality [11]. Although diastolic dysfunction is widely considered a key pathophysiologic mediator of HFpEF, the majority of patents with HFpEF also have systolic myocardial dysfunction when assessed by 2D-STE. Several studies have demonstrated that impaired GLS is a more sensitive marker of impaired systolic performance than LVEF. Shah et al. assessed GLS using 2D-STE at baseline in 447 patients with HFpEF (LVEF ≥45 %) enrolled in the treatment of preserved cardiac function heart failure with an aldosterone antagonist (TOPCAT) trial [12]. They demonstrated that impaired GLS, defined as an absolute GLS <15.8 %, was present in 52 % of patients and was predictive of the composite outcome of cardiovascular death, HF hospitalization, or aborted cardiac arrest (adjusted hazard ratio: 2.14, 95 % CI 1.26–3.66, p = 0.005), cardiovascular death alone (adjusted hazard ratio: 3.20, 95 % CI 1.44–7.12, p = 0.004), and HF hospitalization alone (adjusted hazard ratio: 2.23, 95 % CI 1.16–4.28, p = 0.016) after adjustment for clinical and conventional echocardiographic variables. They also found that GLS was the strongest echocardiographic predictor of the composite outcome. Interestingly, 66 % of patients with impaired GLS had “normal” LVEF ≥55 %, and 43 % of patients with LVEF ≥55 % had abnormal GLS [12]. The unadjusted and adjusted associations of GLS with cardiovascular outcomes were similar in the subgroup of patients with LVEF ≥55 %. The authors concluded that GLS provides functional and prognostic information distinct from LVEF. As the underlying pathophysiology of HFpEF is complex and heterogeneous, the incremental value of GLS beyond conventional measures of LV function warrants further investigation across a broad spectrum of HFpEF. In addition, it should be noted that the progression of left ventricular hypertrophy (LVH) contributes to worsening of not only longitudinal but also circumferential and radial strain in HFpEF.
Early detection and differentiation of cardiomyopathies
2D-STE-derived strain assessments allow the early detection and differential diagnosis of various types of cardiomyopathies. Hypertrophic cardiomyopathy (HCM) is a genetic disorder characterized by LVH and myocardial disarray, and several studies have reported that GLS are reduced in HCM, even though LVEF is preserved. 2D-STE is also useful for familial screening to identify HCM patients at an early stage among asymptomatic mutation carriers. Yiu et al. enrolled sixteen HCM families with pathogenic mutation, comprising 46 patients who fulfilled the criteria for HCM phenotype expression (Mut+/Phen+), 47 patients without phenotype expression (Mut+/Phen−) and 25 control subjects [13]. Although all three groups had similar LV dimensions and LVEF, global and basal anteroseptal longitudinal strains were the most impaired in Mut+/Phen+ patients compared to the other two groups. Interestingly, basal anteroseptal strain was lower in Mut+/Phen− patients (−14.1 ± 3.8 %, p < 0.01) as compared to controls (−19.9 ± 2.9 %), suggesting a subclinical segmental systolic dysfunction.
Differential diagnosis primarily by non-invasive echocardiography examination is fundamental because the therapeutic strategy and patient prognosis vary depending on the cause of LVH (Fig. 2). Sun et al. revealed that patients with biopsy-proven cardiac amyloidosis have all strain parameters (longitudinal, circumferential, and radial strain) profoundly impaired compared with HCM and LVH secondary to pressure overload [14].
Cardiotoxicity from cancer therapy has become a leading cause of morbidity and mortality in survivors in exchange for the decreased cancer death rates over the past decades [15]. The most commonly used definition of cardiotoxicity is a reduction of LVEF >5 to LVEF <55 % with symptoms of heart failure, or an asymptomatic reduction of LVEF of >10 to a LVEF <55 % [16], but the reduction in LVEF is often a late phenomenon. The results from the meta-analysis suggested that an early relative reduction in GLS of between 10 and 15 % during cancer therapy is the most useful parameter for the prediction of cardiotoxicity [15].
Valvular heart disease
In valvular heart disease, LV dysfunction is frequently subclinical despite normal LVEF. Aortic stenosis (AS) and primary mitral regurgitation (MR) are the two most common types of VHD. It is recognized that GLS is a sensitive marker of preclinical systolic dysfunction in patients with AS [17]. Paradoxical low-flow, low-gradient (LFLPG) severe AS despite preserved (≥50 %) LVEF is a relatively new entity that is characterized by a discordant grade of AS severity between the aortic valve area (AVA) and the trans-aortic mean pressure gradient. The majority of published studies in western countries have reported that patients with paradoxical LFLPG severe AS have a worse prognosis if treated medically rather than surgically, suggesting a more advanced stage of AS. However, a very recent retrospective multicenter study from Japan revealed that the prognoses of LFLPG severe AS were better than those of high-gradient severe AS and similar to those of moderate AS, being better than in Western populations [18]. Sato et al. further demonstrated that GLS stratified the high-risk group of paradoxical LFLPG severe AS for future adverse outcomes [19]. They found that the impaired GLS subgroup (absolute value of GLS ≤17 %) had a smaller AVA index, higher LV mass index, higher E/e′, and lower overall 2-year event-free survival (57 vs. 97 %; p < 0.001) than the preserved GLS group (absolute value of GLS >17 %) when paradoxical LFLPG severe AS patients were divided into two groups according to GLS. Therefore, paradoxical LFLPG severe AS can comprise mixed groups with different LV mechanical properties associated with different prognoses.
In severe MR, LV systolic function is often overestimated when assessed by LVEF because of an abnormally low afterload and excessive preload, even if alterations in LV contractility develop. Several recent studies have demonstrated that pre-operative GLS at rest and during exercise but not LVEF provides accurate information about the presence of contractile reserve and predicts changes in post-operative LV function. Witkowski et al. demonstrated in 233 patients with moderate–severe organic MR who underwent successful mitral valve repair that an absolute value of GLS <19.9 % was a major independent predictor of long-term LV dysfunction defined as LVEF <50 % during follow up (34 ± 20 months) after adjustment for parameters currently implemented into guidelines [20].
Heart failure with reduced LVEF
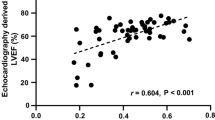
Because the contribution of circumferential fiber to LV myocardial thickening is greater than that of longitudinal fibers, patients with low LVEF have reduced LV myocardial thickening and thereby can have impaired GCS, which reflects more advanced intrinsic myocardial systolic dysfunction and is thus closely related to a poor prognosis. Cho et al. firstly demonstrated that GCS was an independent predictor of cardiac events during 39 ± 17 months of follow-up regardless of age, LVEF, and E/e′, and had greater prognostic power than GLS or LVEF in 201 HF patients with LVEF of 34 ± 13 % [21]. Tanaka et al. recently revealed that absolute GCS ≥5.4 % was an independent and the best predictor of LV reverse remodeling with 91 % sensitivity, 82 % specificity, and an area under the curve of 0.896 (p < 0.0001) in 70 consecutive patients with newly diagnosed dilated cardiomyopathy (LVEF of 28 ± 8 %) during 8.1 ± 5.2 months of follow-up after initiation of the maintenance dose of beta blockers [22].
LV dyssynchrony
LV mechanical dyssynchrony is mainly caused by electrical abnormalities in the ventricular myocardium, typically with left bundle branch block (LBBB). Cardiac resynchronization therapy (CRT) is an established therapeutic option for advanced HF patients with wide QRS duration but the prevalence of non-response to this therapy remains as high as 30 to 35 %. Therefore, persistent efforts have been made to quantify and characterize LV mechanical dyssynchrony by using echocardiography for a better understanding of the pathophysiology and for optimal patient selection of CRT and sites of LV lead placement. The septal flash followed by late systolic contraction in the LV free wall is a typical dyssynchrony pattern of LBBB, but the severity and patterns of LV mechanical dyssynchrony vary between patients, depending on the QRS configuration, heart failure etiology, regional intrinsic myocardial function and other pathophysiological factors. Among the three components of LV deformation, radial strain imaging may be the most feasible for quantifying and characterizing LV dyssynchrony and most applicable for the prediction of successful CRT (Fig. 3). Suffoletto et al. reported that 2D-strain-derived LV dyssynchrony, defined as a time difference in peak anteroseptum to posterior wall strain ≥130 ms, was associated with LVEF response to CRT [23]. Alternatively, circumferential strain can be useful for predicting clinical response to CRT because radial thickening theoretically mirrors circumferential shortening in the same image plane [24]. The regional time-strain curve is sometimes complex, showing multiple peaks especially in the septal segments, and therefore accurate identification of first peak including the pre-ejection phase of these segments is important for the precise dyssynchrony measurement.
An example of radial strain images of early systole (top left) and late systole (bottom left) and corresponding time-strain curves (right) obtained from the short-axis view in a patient with a low left ventricular (LV) ejection fraction and left bundle branch block. The septum contracts in the early systolic phase (yellow arrows) followed by late systolic contraction in the LV free wall (red arrows)
RV function
Accurate echocardiographic assessment of global RV function is difficult because of its complex geometry, and retrosternal position of the right ventricle limits echocardiographic imaging. GLS in the RV four-chamber view has recently been used as a surrogate of global RV function because longitudinal shortening is the major contributor to overall RV performance. RV GLS excluding the interventricular septum has recently been reported to have prognostic value in various disease states including heart failure, acute myocardial infarction, pulmonary hypertension, and amyloidosis, and to predict RV failure after LV-assistance device implantation. Establishment of the normal values and associated variations of STE-derived RV GLS is essential for its routine clinical application. Pooled data suggest that a global longitudinal RV free wall strain <20 % in absolute value is abnormal. Chia et al. performed RV functional assessment in 142 healthy adult volunteers aged between 20 and 81 years, and revealed that the average of RV GLS was 27.3 ± 3.3 (male: 26.9 ± 3.1, female: 27.8 ± 3.5) in absolute value, with a reduction with age [25].
Sugiura et al. firstly quantified and characterized RV systolic dysfunction and regional non-uniformity in the setting of acute RV pressure overload by STE in patients with acute pulmonary thromboembolism (APTE) [26]. RV regional time-strain curves in APTE typically show reduced and delayed RV free wall peak systolic strain, especially in the mid-basal segments (Fig. 4), which return to normal values after the amelioration of acute RV pressure overload by primary treatment. Chronic pulmonary hypertension also induces RV longitudinal strain abnormality [27]. Fine et al. performed prospective peak RV longitudinal systolic strain measurement in 575 patients (mean age 56 ± 18 years; 63 % women) with known or suspected PH [28]. Eighteen-month survival was 92, 88, 85, and 71 % according to RV strain quartile (p < 0.001), with a 1.46 higher risk of death (95 % CI 1.05–2.12) per 6.7 % decline in RV strain. In addition, RV strain predicted survival when adjusted for pulmonary pressure, pulmonary vascular resistance, and right atrial pressure, and provided incremental prognostic value over conventional clinical and echocardiographic variables. They concluded that RV free-wall systolic strain is feasible and is a powerful predictor of the clinical outcome of patients with known or suspected PH.
Examples of longitudinal strain images (top) and time-strain curves (bottom) obtained from the right ventricular (RV) four-chamber views in a normal subject (left) and a patient with acute pulmonary thromboembolism (right). White arrows indicate reduced and delayed RV free wall peak systolic strain in the mid-basal segments
Future perspectives
Segmental strain measurement can be useful for detecting myocardial ischemia but it is not commonly incorporated in daily clinical practice. Recent meta-analysis demonstrated that GLS measurements at rest have only modest diagnostic accuracy in predicting coronary artery disease among patients presenting with acute or chronic chest pain [29]. Layer-specific myocardial strain can now be measured, and this technique can provide better diagnostic performance of stress echocardiography for the diagnosis of coronary artery disease. In addition, layer-specific myocardial strain assessment can help us better understand the pathophysiologic mechanisms of heart diseases. Okada et al. measured peak systolic strains of the three orthogonal directions at inner layer, mid-wall and outer layer in 41 HCM patients and 27 control subjects [30]. They demonstrated that not only GLS in all three layers but also GCS in the mid and outer layers were reduced, whereas GCS in the inner layer was preserved in patients with HCM compared with those in control subjects. They further revealed that maintenance of GCS in the inner layer was associated with preserved LVEF in HCM. Due to smaller radius of the circumferential than longitudinal curvature in the left ventricle, development of concentric LV geometry may allow the maintenance of circumferential endocardial shortening by layer-to-layer interactions despite the decrease in active shortening of abnormally thickened myocardial fibers. These results can provide thorough insight into compensatory mechanisms for preserving the normal LVEF in patients with LVH.
STE-derived strain rate imaging provides quantitative measures of the speed of myocardial deformation using the same technique, the same axis, and the same cardiac cycle as strain imaging, which allows more sensitive and earlier detection of myocardial ischemia and subtle changes in LV systolic and diastolic function. Since impairment of regional relaxation occurs in an early phase of myocardial ischemia, assessment of the peak strain rate during the early diastole obtained from time-strain rate curves in daily clinical practice can be useful for detecting subtle and latent coronary artery disease.
The combination of STE-derived strain and displacement imaging can be useful for discriminating active myocardial contraction from passive or translational wall motion. Dohi et al. firstly demonstrated that displacement imaging clearly represents paradoxical interventricular septal motion, whereas strain imaging showed normal timing of the intrinsic contraction in patients with pulmonary hypertension [31]. These results indicate that paradoxical interventricular septal motion is induced by external force and/or interventricular pressure interaction without intrinsic contractile dyssynchrony in the setting of RV pressure overload (Fig. 5).
Examples of radial displacement (left top) and strain images (right top) and corresponding time-strain curves (bottom) obtained from the short-axis view in a patient with idiopathic pulmonary arterial hypertension. Displacement imaging clearly represents paradoxical interventricular septal motion (white arrows), whereas strain imaging showed normal timing of intrinsic contraction
Three-dimensional (3D)-STE was recently introduced and has been used as a novel method to image global LV and RV kinetics. Implementation of this new technique might lead to a better understanding of the pathophysiologies of various types of heart disease.
Conclusions
GLS undoubtedly provides important information on LV function and prognosis, distinct from LVEF, in various heart diseases, especially when LVEF is preserved. Because GLS has the narrowest normal variation as well as the lowest inter-software and inter-vendor variability among the three components of LV deformation, it can be safely used in routine clinical practice, but a set of system and software from the same vendor should be used for longitudinal follow-up in the same patients. GLS can be also useful for quantifying global RV systolic function and regional heterogeneity. GCS has relatively narrow normal variations and low inter-software and inter-vendor variability, and can be used as an independent prognosticator in patients with reduced LVEF. Radial strain imaging appears to be more specific for quantifying and characterizing LV dyssynchrony, and is applicable for the prediction of successful CRT. 2D-STE-derived strain feasibly identifies and quantifies direction-specific myocardial deformation patterns, which can help physicians and sonographers better understand the pathophysiologic mechanism of myocardial dysfunction and provide better individual management.
References
Yingchoncharoen T, Agarwal S, Popovic ZB, et al. Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr. 2013;26:185–91.
Takigiku K, Takeuchi M, Izumi C, et al. Normal range of left ventricular 2-dimensional strain: Japanese Ultrasound Speckle Tracking of the Left Ventricle (JUSTICE) study. Circ J. 2012;76:2623–32.
Farsalinos KE, Daraban AM, Unlu S, et al. Head-to-head comparison of global longitudinal strain measurements among nine different vendors: the EACVI/ASE inter-vendor comparison study. J Am Soc Echocardiogr. 2015;28(1171–81):e1172.
Sun JP, Lee AP, Wu C, et al. Quantification of left ventricular regional myocardial function using two-dimensional speckle tracking echocardiography in healthy volunteers–a multi-center study. Int J Cardiol. 2013;167:495–501.
Zghal F, Bougteb H, Reant P, et al. Assessing global and regional left ventricular myocardial function in elderly patients using the bidimensional strain method. Echocardiography. 2011;28:978–82.
Cheng S, Larson MG, McCabe EL, et al. Age- and sex-based reference limits and clinical correlates of myocardial strain and synchrony: the Framingham Heart Study. Circ Cardiovasc Imaging. 2013;6:692–9.
Dalen H, Thorstensen A, et al. Segmental and global longitudinal strain and strain rate based on echocardiography of 1266 healthy individuals: the HUNT study in Norway. Eur J Echocardiogr. 2010;11:176–83.
Takamura T, Dohi K, Onishi K, et al. Left ventricular contraction-relaxation coupling in normal, hypertrophic, and failing myocardium quantified by speckle-tracking global strain and strain rate imaging. J Am Soc Echocardiogr. 2010;23:747–54.
Ishizu T, Seo Y, Kameda Y, et al. Left ventricular strain and transmural distribution of structural remodeling in hypertensive heart disease. Hypertension. 2014;63:500–6.
Enomoto M, Ishizu T, Seo Y, et al. Subendocardial systolic dysfunction in asymptomatic normotensive diabetic patients. Circ J. 2015;79:1749–55.
Kraigher-Krainer E, Shah AM, Gupta DK, et al. Impaired systolic function by strain imaging in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2014;63:447–56.
Shah AM, Claggett B, Sweitzer NK, et al. Prognostic importance of impaired systolic function in heart failure with preserved ejection fraction and the impact of spironolactone. Circulation. 2015;132:402–14.
Yiu KH, Atsma DE, Delgado V, et al. Myocardial structural alteration and systolic dysfunction in preclinical hypertrophic cardiomyopathy mutation carriers. PLoS One. 2012;7:e36115.
Sun JP, Stewart WJ, Yang XS, et al. Differentiation of hypertrophic cardiomyopathy and cardiac amyloidosis from other causes of ventricular wall thickening by two-dimensional strain imaging echocardiography. Am J Cardiol. 2009;103:411–5.
Thavendiranathan P, Poulin F, Lim KD, et al. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol. 2014;63(25 Pt A):2751–68.
Seidman AD, Fornier MN, Esteva FJ, et al. Weekly trastuzumab and paclitaxel therapy for metastatic breast cancer with analysis of efficacy by HER2 immunophenotype and gene amplification. J Clin Oncol. 2001;19:2587–95.
Galli E, Lancellotti P, Sengupta PP, et al. LV mechanics in mitral and aortic valve diseases: value of functional assessment beyond ejection fraction. JACC Cardiovasc Imaging. 2014;7:1151–66.
Yamashita E, Takeuchi M, Seo Y, et al. Prognostic value of paradoxical low-gradient severe aortic stenosis in Japan: Japanese Multicenter Aortic Stenosis Study, Retrospective (JUST-R) Registry. J Cardiol. 2015;65:360–8.
Sato K, Seo Y, Ishizu T, et al. Prognostic value of global longitudinal strain in paradoxical low-flow, low-gradient severe aortic stenosis with preserved ejection fraction. Circ J. 2014;78:2750–9.
Witkowski TG, Thomas JD, Debonnaire PJ, et al. Global longitudinal strain predicts left ventricular dysfunction after mitral valve repair. Eur Heart J Cardiovasc Imaging. 2013;14:69–76.
Cho GY, Marwick TH, Kim HS, et al. Global 2-dimensional strain as a new prognosticator in patients with heart failure. J Am Coll Cardiol. 2009;54:618–24.
Tanaka H, Matsumoto K, Sawa T, et al. Evaluation of global circumferential strain as prognostic marker after administration of beta-blockers for dilated cardiomyopathy. Int J Cardiovasc Imaging. 2014;30:1279–87.
Suffoletto MS, Dohi K, Cannesson M, et al. Novel speckle-tracking radial strain from routine black-and-white echocardiographic images to quantify dyssynchrony and predict response to cardiac resynchronization therapy. Circulation. 2006;113:960–8.
Maruo T, Seo Y, Yamada S, et al. The speckle tracking imaging for the assessment of cardiac resynchronization therapy (START) study. Circ J. 2015;79:613–22.
Chia EM, Hsieh CH, Boyd A, et al. Effects of age and gender on right ventricular systolic and diastolic function using two-dimensional speckle-tracking strain. J Am Soc Echocardiogr. 2014;27(1079–86):e1071.
Sugiura E, Dohi K, Onishi K, et al. Reversible right ventricular regional non-uniformity quantified by speckle-tracking strain imaging in patients with acute pulmonary thromboembolism. J Am Soc Echocardiogr. 2009;22:1353–9.
Ichikawa K, Dohi K, Sugiura E, et al. Ventricular function and dyssynchrony quantified by speckle-tracking echocardiography in patients with acute and chronic right ventricular pressure overload. J Am Soc Echocardiogr. 2013;26:483–92.
Fine NM, Chen L, Bastiansen PM, et al. Outcome prediction by quantitative right ventricular function assessment in 575 subjects evaluated for pulmonary hypertension. Circ Cardiovasc Imaging. 2013;6:711–21.
Norum IB, Ruddox V, Edvardsen T, et al. Diagnostic accuracy of left ventricular longitudinal function by speckle tracking echocardiography to predict significant coronary artery stenosis. A systematic review. BMC Med Imaging. 2015;15:25.
Okada K, Yamada S, Iwano H, et al. Myocardial shortening in 3 orthogonal directions and its transmural variation in patients with nonobstructive hypertrophic cardiomyopathy. Circ J. 2015;79:2471–9.
Dohi K, Onishi K, Gorcsan J 3rd, et al. Role of radial strain and displacement imaging to quantify wall motion dyssynchrony in patients with left ventricular mechanical dyssynchrony and chronic right ventricular pressure overload. Am J Cardiol. 2008;101:1206–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K.D. received lecture fees of equal to or more than 500,000 yen from Otsuka Pharma Inc. in 2015. M.I. received lecture fees of more than 500,000 yen from Daiichi Sankyo Co. Ltd. and Mochida Pharmaceutical Co., Ltd. in 2015. M.I. received a single-year research grant for the Department of Cardiology and Nephrology, Mie University Graduate School of Medicine, of equal to or more than 2 million yen, from Bristol-Myer K.K., AstraZeneca K.K., MSD K.K. and BIOTRONIK JAPAN. INC. in 2015. No relevant conflicts of interest related to the article were disclosed by the authors.
Rights and permissions
About this article
Cite this article
Dohi, K., Sugiura, E. & Ito, M. Utility of strain-echocardiography in current clinical practice. J Echocardiogr 14, 61–70 (2016). https://doi.org/10.1007/s12574-016-0282-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-016-0282-8