Abstract
Introduction
Direct Digital Radiography (DDR) has dramatically impacted medical imaging by providing fast, high-quality radiographic images. It offers several advantages: instant image acquisition, efficient image storage and transmission, advanced image processing algorithms, and dose reduction capabilities. However, the misuse of DDR can lead to suboptimal image quality and diagnostic errors. This paper explores the uses and misuse of DDR in medical imaging.
Methods
To understand the current knowledge, attitudes, and practices (KAP) of radiographers regarding DDR, an exploratory cross-sectional survey was conducted. The survey collected demographic information and assessed participants' practices in DDR.
Results
A total of 157 radiographers participated in the study. 50% of participants had formal training in DR, 34.4% manually collimated the X-ray beam most of the time, whilst 32.5% admitted they sometimes used image crop instead of manual collimation. 45.2% relied on automatic exposure devices, and 55.4% mentioned that they modified the exposure manually. 36.9% used image processing tools. 30.6% consistently monitored their repeat rate, whilst 12.1% mentioned they never did.
Conclusion
The findings highlight the importance of continuous education and training to ensure the optimal use of DDR. There is a need for improved knowledge and skills in areas such as collimation, exposure optimisation, and image processing. Future research and educational initiatives should address these issues to ensure DDR's safe and effective use in clinical practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Direct Digital Radiography (DDR) has revolutionised medical imaging with its ability to rapidly generate high-quality radiographic images, becoming an indispensable tool for diagnosing a wide range of medical conditions. Alongside its undeniable benefits, DDR has also introduced new challenges and potential pitfalls.
One of the critical advantages of DDR is its ability to produce digital images instantly. Unlike traditional radiography, DDR eliminates the need for film processing, reducing the time required for image acquisition and interpretation. The digital format allows for efficient storage, retrieval, and transmission of images, enabling quick access to patient information and facilitating remote consultations. Moreover, DDR systems often employ advanced image processing algorithms, enhancing the visibility of anatomical structures and improving diagnostic accuracy. Furthermore, DDR offers dose reduction capabilities, particularly compared to conventional radiography. The technology optimises dose by adjusting exposure parameters in real-time, minimising radiation exposure to patients and radiographers.
Despite these advantages, the misuse of DDR can lead to suboptimal image quality and diagnostic errors. Improper positioning, suboptimal exposure settings, and artefacts caused by patient motion can result in images with reduced diagnostic value. Additionally, the digital nature of DDR images can introduce new challenges in image manipulation and interpretation. Inadequate post-processing techniques or excessive image enhancement can distort anatomical structures, potentially leading to misdiagnosis or unnecessary interventions.
The optimal use of DDR requires continuous education and training for radiographers to acquire new abilities and maintain the highest image quality [1, 2]. The literature recommends formal education, continuous medical education, and vendor training [3, 4]. There is a definite and widespread need for thorough, hands-on teaching of digital image technologies. For example, radiographers crop (DDR) images to obtain better X-ray images instead of utilising better collimation settings, which shows an apparent lack of knowledge and skills [5, 6].
Literature shows that (DDR) has reduced ionising radiation to patients while maintaining diagnostic quality images. However, suboptimum techniques are in action within the DDR environment, where radiographers may increase radiation doses due to favouring superior image quality, known as 'dose creep'. Hayre [6] paper identifies two issues related to X-ray exposures in contemporary radiographic practice: the lack of autonomy concerning X-ray exposures within the general imaging environment and the failure of some radiographers to alter 'pre-set' X-ray exposures, which may result in images of suboptimum diagnostic quality [6].
Hayre et al. [8] paper highlights the importance of radiographers having an adequate knowledge base with DDR technology to produce images of diagnostic quality. It emphasises the need for radiographers to be aware of the potential danger of over-repeating X-ray examinations with no added benefit. The paper suggests that DDR may alleviate patient discomfort by enabling 'quick' repeats. Still, radiographers should critically reflect upon the potential pitfalls and near misses associated with image acquisition using DDR. In essence, the current research landscape primarily emphasizes the merits of DDR, but it falls short in providing a well-rounded understanding of the technology by not addressing the potential issues, challenges, or the educational demands necessary for its effective and safe implementation in the field of medical imaging. This gap in the literature underscores the significance of further research that encompasses all facets of DDR technology, which the paper in question aims to fill.The findings of this paper initiate discussions about the importance of continuous skills improvement required to operate DDR equipment and forestalling radiation incidents in the future [8].
The study aimed to analyse radiographers' knowledge, attitudes, and practices (KAP) regarding digital radiography (DR) in medical imaging.
2 Methods
2.1 Study design
An exploratory cross-sectional survey was used to analyse the participants’ knowledge (K) of DDR, attitudes (A), and practices (P) (KAP). A cross-sectional study design is commonly used to collect data at a specific point in time, providing a snapshot of the knowledge, attitudes, and practices (KAP) of the study population. In this design, data is collected from participants at a single time point, allowing researchers to examine the relationships and prevalence of the variables of interest at that moment.
2.2 Sampling and study population
The eligibility to participate in the study included radiographers who practice across hospitals and medical centres working in the United Arab Emirates (UAE) during the data collection period from August to October 2022. Before participating, the participants received information on the study that outlined the study’s objectives and signed a consent form. The consent form guaranteed that their participation would be kept entirely private and that they would be allowed to leave the study at any time before the final submission of the survey. Direct distribution of the online survey using the Google Forms link was used to solicit participation.
2.3 Data instruments
A structured survey designed based on the study's aims and reviewing previous similar studies is a common and effective approach in survey research. This process helps ensure that the survey instrument aligns with the study's specific objectives and captures relevant variables and constructs. The survey recorded the participants’ opinions based on declarative statements. Before survey development, the researchers gathered preliminary information and conducted a literature review about DDR practices [1, 3, 6, 9,10,11]. Validity and reliability assessment from the pilot study involves evaluating the quality and consistency of the survey instrument. Two radiographers, four radiology managers, and two senior faculty members in clinical and academic institutions piloted the survey. The researchers identify and address potential issues with the survey, ensuring that it is valid, reliable, and suitable for measuring the knowledge, attitudes, and practices (KAP) of the target population effectively.
The survey was designed in three sections. Section 1 collected the participants’ demographic information, including age, qualification, work experiences, and the country where they obtained the terminal academic degree. This section also included questions about whether participants practised conventional radiography and had formal DDR training. Section 2 identified the participants’ current practices on collimation, radiation exposures, image processing, and image quality. Finally, Section 3 of the survey captured the participants’ knowledge using ten multiple-choice questions.
2.4 Ethical approval
The University of Sharjah Research Ethics Committee approved the study. Accordingly, the study’s objectives, procedures, and methodology followed the rules and regulations (reference number: REC-20–05-06–01).
2.5 Data analysis
Data from completed online surveys were transferred manually to Excel (Microsoft, Redmond, WA, USA) and then to SPSS version 23.0 (SPSS, Chicago, IL, USA) for statistical analysis. Before analysis, all variables were reviewed for accuracy of data entry and missing values. For the knowledge assessment, the overall percentage of participants who gave correct answers was computed for each question. The score was transformed into a percentage by dividing the total score by the maximum possible score multiplied by 100. Accordingly, scores were categorised into poor knowledge = ≤ 40%, moderate knowledge = 41–70%, and good knowledge = ≥ 71% or [12]. A chi-squared test of independence was used to analyse the individual questions. Mann–Whitney and Kruskal–Wallis tests were used to compare group responses. The overall value for statistical significance was P < 0.05.
3 Results
3.1 Demographics
A total of 157 participants met the inclusion and exclusion criteria and were therefore included in the study. The participants’ ages ranged from 18 to 65 years, and almost 38.2% (n = 60) were between the ages of 26 and 35. In terms of qualification, most of the participants completed a bachelor’s degree (B.Sc.) in radiography 80.3% (n = 126), followed by an equal number of 8.9% (n = 14) who completed a diploma and master’s degree. In addition, the results showed that respondents with a range of experience of 1–5 years were 44.6% (n = 70). The participants obtained their terminal degrees from different countries and were categorised into three categories: 29.3% (n = 46) from India, 22.3% (n = 35) from the Philippines, and 48.4% (n = 76) from Middle Eastern countries (Table 1).
3.2 DDR practice and training
Three questions in this section collected responses to assess the participants’ practice and training in DDR. The study showed that 70% (n = 110) of the participants had previously practised conventional radiography (film processing). Equal responses were received from the participants for both questions regarding training on DDR and radiation safety (Fig. 1).
3.3 DDR collimation practice
Three questions in this section gathered responses on a 4-point Likert scale, assessing the practice of proper collimation among the participants. Values assigned were: 1 = ‘Never’, 2 = ‘Sometimes’, 3 = ‘Most of the Times’ and 4 = ‘Always’. When the participants were asked if they adhered to proper collimation, the most common response was ‘Most of the time’, as stated by 34.4% (n = 54). On enquiring if the participants used image crops instead of proper collimation, 32.5% (n = 51) sometimes stated, and 31.8% (n = 50) mentioned most of the time. 38.2% (n = 60) said they sometimes opted for image cropping instead of collimation to avoid cutting regions of interest (see Table 2).
3.4 DDR exposure, practice
The participants were asked if they used higher kVp and lower mAs and if they monitored and considered the exposure index; the most popular response was sometimes given by 39.5% (n = 62) and 45.2% (n = 71) of respondents, respectively. Of the radiographers, 34.3% (n = 54) mentioned updating exposure factors to obtain optimum image quality and avoid excessive radiation. Further, 45.2% (n = 71) stated that they sometimes depended on automatic exposure, and 55.4% (n = 87) identified that they modified the exposure manually. Finally, 38.2% (n = 60) of the participants stated they sometimes use the 15% exposure factor rule (see Table 3).
3.5 DDR image processing and quality
This section had two questions, each capturing data on image processing and quality. Among the participants, 36.9% (n = 58) stated they use image processing tools like windowing, while 35.7% (n = 56) also stated they sometimes use them. On the other hand, only 30.6% (n = 48) of the radiographers said they continuously monitored their repeat rate, while 12.1% (n = 19) mentioned they never did (Table 4).
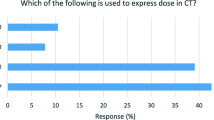
3.6 DDR knowledge assessment
Ten questions in this section had only one answer for each. The questions and the frequencies of correct and incorrect responses are given in Table 5. There were only five questions for which most respondents stated the correct answer. When asked whether the statement DDR increases image dynamic range was true or false, 95.5% (n = 150) of the participants stated it was true correctly. Further, 78.3% (n = 123) gave the correct response, true, for the statements that image artefacts can be due to image plates and image artefacts can be the results of image processing algorithms. When the radiographers were asked which of the following actions digital image processing could not do, 78.3% (n = 123) chose the correct response: increase patient dose’.
Each correct answer was given a score of 1, calculating the total score for the knowledge assessment. The minimum possible score was 0, and the maximum score was 10. A maximum score of 10 was obtained by 1.3% (n = 2) of the participants, and 5.1% (n = 8) of the participants scored a minimum of 3. The most common score of 6 was obtained by 32.5% (n = 51) of the participants.
Only 1.3% (n = 2) of participants could score 100%, while 5.1% (n = 8) scored the lowest score of 30%. The most popular score was 60%, by 32.5% (n = 51) of the respondents. The two participants who achieved 100% scores did not belong to the same demographics but stated affirmatively that they had previous experience in CR but did not have formal training in DDR or its safe use.
The distribution of the score ranges is shown in Fig. 2. Only 11.5% (n = 18) of the participants had good knowledge, while 16.6% (n = 26) had poor knowledge. The study revealed that among the 18 participants who had good knowledge, 9.6% (n = 15) had a bachelor’s degree, 1.3% (n = 2) had a master’s degree, and 0.6% (n = 1) had a diploma. Further, of the participants who scored > 70%, 7.0% (n = 11) had 1–5 years of experience, and 1.9% (n = 3) had 6–10 years of experience. Most participants, 22.9% (n = 36), had more than 11 years of experience and needed better knowledge.
4 Association between demographics, knowledge, and scores
Kruskal–Wallis H and Mann–Whitney U tests were conducted to analyse any statistically significant differences in the scores concerning the participants’ demographics and knowledge. The Kruskal–Wallis H test concluded that there was no statistically significant difference in the scores between the different education qualifications, x2 (3) = 2.589, p = 0.459. The test further concluded no statistically significant difference in the score between the different years of work experience, x2 (3) = 5.894, p = 0.117, and no statistically significant difference between the different age groups, x2 (3) = 1.988, p = 0.575.
The Mann–Whitney U test suggested no difference in the scores of those who practised and did not practice conventional radiography before (U = 2359.5, p = 0.273). Likewise, there was no difference in the scores of those who have received/did not receive formal training in digital radiography (U = 2956.0, p = 0.578). Further, the test also concluded that there was no difference in the scores of those who received/did not have formal training in radiation safety of digital radiography (U = 3079.0, p = 0.993).
5 Discussion
The results from this study are discussed concerning the participants’ practises, awareness, attitudes, and knowledge of DDR, along with the background variables captured through demographic-based questions. DDR has been widely used in practice in recent years. Therefore, radiographers with more than 11 years of experience were expected to know/practise CR compared to those with less than ten years of experience. The results showed that 86.5% (n = 45) of the participants with more than 11 years of experience and 61.9% (n = 65) of the participants with less than ten years of experience had practised CR. Nonetheless, the constraints of the traditional system impart valuable insights into the correct practices of collimation and exposure parameters, which can be effectively incorporated into the use of DDR. Interestingly, a noteworthy observation is that 50% of the participants lacked formal training in DDR and DDR radiation safety.
Proper collimation in Direct Digital Radiography (DDR) is essential for three key reasons. Firstly, it minimizes unnecessary radiation exposure, adhering to the ALARA principle. Secondly, it enhances image quality by reducing scatter radiation, aiding accurate diagnosis. Lastly, it ensures compliance with best practices and regulatory standards, contributing to safe and consistent radiographic procedures. Proper collimation is required to limit the tissue area exposed to irradiation and subject patients to lower radiation doses. Furthermore, it reduces scattered radiation and increases image quality by increasing contrast [7]. Studies have shown that most unnecessary doses to patients require more collimation. Nevertheless, the perceived importance of collimation among radiographers has changed following the widespread use of DDR, as cropping unwanted image regions is often used instead of tight collimation [3]. In our study, 64.3% (n = 101) stated they adhere to proper collimation very often/always. Still, on the contrary, 57.9% (n = 91) agreed they overuse the image crop instead of using proper collimation most of the time/always, and 45.9% (n = 72) relied more on image cropping to retain the ROI and avoid repeat exposure. This is comparable to the study by Morrison et al., where half of the radiographer’s stated that they used electronic cropping in pediatrics’ radiography more than 75% of the time [13].
Most participants in our study stated that they sometimes depended on automatic exposure and modified it manually. In addition, 61.2% (n = 96) stated that they often update exposure factors to obtain optimum image quality and avoid excessive radiation to the patient. The responses showed an optimistic practice among the participants to alternate between manual and automatic exposure settings, prioritising image quality and radiation safety, which has been concluded as a requirement for radiographers by McFadden et al. [14].
Most of the participants in our study stated that they use image processing tools that allow them to achieve optimal image quality with a reasonable dose level. It also raises the hazard of dose creep in practice, an unnoticed increase in exposure over time due to the decoupling of exposure factors and image brightness and contrast. In addition, most participants needed formal training in DDR and radiation safety in DDR. This training and formal education can increase their awareness of proper collimation and exposure parameters. Further, quality control programs should be part of the clinical routine, ensuring dose control and assessing dose-relevant parameters [15].
Nonetheless, the non-parametric analysis found no significant difference in the scores between educational qualifications or other demographics.
6 Limitations
This study was limited to radiographers’ responses to quantitative results. Future studies to include observations of current practice and a survey to collect radiology managers’ opinions should be conducted for better understanding and future recommendations.
7 Conclusion
DDR has mostly replaced CR and has many advantages for radiology and healthcare services. Digital images can easily be displayed on monitors, enhanced, processed, archived, and transmitted. In addition, digital images can be integrated into different advanced artificial intelligence applications to assist in image interpretation and analysis. The digital transformation results in subtle changes in radiographer curriculum, practice and workload. The study results raised concerns about the radiographer’s current knowledge and practice in DDR. The researchers believe the reasons may be due to a lack of training, professionalism, monitoring and negligence [16].
8 Recommendations
Proper education and training courses should be designed in collaboration with professional bodies and academic institutes to improve radiographers’ knowledge and skills. Universities and professional bodies should emphasise teaching students about excellent digital radiography practices and explain the typical errors radiographers make when performing digital radiography. Additionally, it is crucial to regularly track the development and improvement of radiographers’ radiographic examination quality by closely observing their work and performing routine quality assurance checks on their images.
Data availability
The data supporting this study's findings are available on request from the corresponding author (MMA).
References
Ball S, McKerrow M, Murphy A. Do radiographers collimate? A retrospective analysis of radiographic collimation of common musculoskeletal examinations at an adult trauma centre. J Med Radiat Sci. 2022;1–9.
Bansal GJ. Digital radiography. A comparison with modern conventional imaging. Postgrad Med J. 2006;82(969):425–8.
Demaio DN, Herrmann T, Noble LB, Orth D, Peterson P, Young J, et al. Best practices in digital radiography. Radiol Technol. 2019;91(2):198–201.
Abuzaid MM, Elshami W, Tekin HO. Infection control and radiation safety practices in the radiology department during the COVID-19 outbreak. PLoS ONE. 2022;17(12): e0279607.
Casey B. Digital radiography may be leading to “collimation creep.” AuntMinnie. 2019.
Hayre CM. “Cranking up”, “whacking up” and “bumping up”: X-ray exposures in contemporary radiographic practice. Radiography. 2016;22(2):194–8.
Moifo B, Tene U, MoulionTapouh JR, Samba Ngano O, Tchemtchoua Youta J, Simo A, et al. Knowledge on irradiation, medical imaging prescriptions, and clinical imaging referral guidelines among physicians in a sub-saharan african country (Cameroon). Radiol Res Pract. 2017;2017:1–7.
Hayre CM, Eyden A, Blackman S, Carlton K. Image acquisition in general radiography: The utilisation of DDR. Radiography [Internet]. 2017;23(2):147–52. Available from: https://doi.org/10.1016/j.radi.2016.12.010.
Alsleem H, Davidson R, Al-Dhafiri B, Alsleem R, Ameer H. Evaluation of radiographers’ knowledge and attitudes of image quality optimisation in paediatric digital radiography in Saudi Arabia and Australia: a survey-based study. J Med Radiat Sci. 2019;66(4):229–37.
Eduardo C, Dias M, Bezzina P, Portelli JL, Eduardo C, Dias M, et al. Gonad contact shielding in digital radiography: a questionnaire survey. Eur J Radiol [Internet]. 2022;110620. Available from: https://doi.org/10.1016/j.ejrad.2022.110620.
Butt A, Savage NW. Digital display monitor performance in general dental practice. Aust Dent J. 2015;60(2):240–6.
Abuzaid MM, Elshami W, Noorajan Z, Khayal S, Sulieman A. Assessment of the professional practice knowledge of computed tomography preceptors. Eur J Radiol Open. 2020;7.
Morrison G, John SD, Goske MJ, Charkot E, Herrmann T, Smith SN, et al. Pediatric digital radiography education for radiologic technologists: Current state. Pediatr Radiol. 2011;41(5):602–10.
Mc Fadden S, Roding T, de Vries G, Benwell M, Bijwaard H, Scheurleer J. Digital imaging and radiographic practise in diagnostic radiography: An overview of current knowledge and practice in Europe. Radiography. 2018;24(2):137–41.
Uffmann M, Schaefer-Prokop C. Digital radiography: The balance between image quality and required radiation dose. Eur J Radiol. 2009;72(2):202–8.
Abuzaid MM, Tamam N, Elshami W, Ibham M, Aljamal M, Khayal S, Abdullah A, Hamd Z, Pedersen MRV. Exploring Radiographers’ Engagement in Research: Motivation and Barriers in Five Arab Countries. Healthcare. 2023;11:2735. https://doi.org/10.3390/healthcare11202735.
Funding
NA.
Author information
Authors and Affiliations
Contributions
All authors participated in the project development, data collection, and manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
IRB statement
Study approved by the institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abuzaid, M.M., Elshami, W., Abdelrazig, A. et al. Direct digital radiography: Exploring applications, misuse, and training needs in medical imaging. Health Technol. 13, 1025–1032 (2023). https://doi.org/10.1007/s12553-023-00791-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-023-00791-x