Abstract
Cardiac excitation involves the generation of action potential by individual cells and the subsequent conduction of the action potential from cell to cell through intercellular gap junctions. Excitation of the cellular membrane results in opening of the voltage-gated L-type calcium ion (Ca2+) channels, thereby allowing a small amount of Ca2+ to enter the cell, which in turn triggers the release of a much greater amount of Ca2+ from the sarcoplasmic reticulum, the intracellular Ca2+ store, and gives rise to the systolic Ca2+ transient and contraction. These processes are highly regulated by the autonomic nervous system, which ensures the acute and reliable contractile function of the heart and the short-term modulation of this function upon changes in heart rate or workload. It has recently become evident that discrete clusters of different ion channels and regulatory receptors are present in the sarcolemma, where they form an interacting network and work together as a part of a macro-molecular signalling complex which in turn allows the specificity, reliability and accuracy of the autonomic modulation of the excitation–contraction processes by a variety of neurohormonal pathways. Disruption in subcellular targeting of ion channels and associated signalling proteins may contribute to the pathophysiology of a variety of cardiac diseases, including heart failure and certain arrhythmias. Recent methodological advances have made it possible to routinely image the topography of live cardiomyocytes, allowing the study of clustering functional ion channels and receptors as well as their coupling within a specific microdomain. In this review we highlight the emerging understanding of the functionality of distinct subcellular microdomains in cardiac myocytes (e.g. T-tubules, lipid rafts/caveolae, costameres and intercalated discs) and their functional role in the accumulation and regulation of different subcellular populations of sodium, Ca2+ and potassium ion channels and their contributions to cellular signalling and cardiac pathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Until recently, the prevailing concept of cardiac electrophysiology has been that ion channels and receptors are freely mobile in the plasma membrane. However, this simple “random collision model” (Hackenbrock et al. 1986) is inadequate to explain the emerging experimental results which highlight microdomain-specific regulation of heart physiology. It has been recognized that discrete clusters of different ion channels exist along the sarcolemma, and studies in recent years have greatly extended our understanding of how specific subcellular localization impacts channel function and regulation (Zaccolo and Pozzan 2002; Warrier et al. 2007; Saucerman et al. 2014). In addition, many ion channels form a protein-interacting network where they work together as a part of a macro-molecular signalling complex (Willoughby and Cooper 2007; Best and Kamp 2012; Cerrone and Delmar 2014). This protein–protein interaction is tightly controlled and regulated by a variety of signalling pathways, such as adrenergic, muscarinic, adenosine, prostaglandin, angiotensin pathways, among others. The diversity of cellular responses achieved with a limited pool of secondary messengers is made possible through the organization of essential signal components, in particular microdomains such as specific membrane-based structures, including T-tubules (Kamp and Hell 2000), lipid rafts/caveolae (Balijepalli et al. 2006; Pani and Singh 2009), costameres (Hong et al. 2014) and intercalated discs (Sato et al. 2011; Cerrone and Delmar 2014). In addition to these physical compartments, scaffolding proteins (such as A-kinase-anchoring proteins, caveolins and focal adhesion kinase) facilitate the formation of multi-protein complexes which create further segregation and refinement in intracellular and cell-to-cell signalling. During pathological remodelling, cell structural integrity is altered and ion channel redistribution occurs, with loss of the protein–protein interaction (Nattel et al. 2007). Disruption of normal subcellular targeting of ion channels and associated signalling proteins may contribute to the pathophysiology of a variety of cardiac diseases, including heart failure and certain arrhythmias (Schaper et al. 2002).
The spatial compartmentation of macro-molecular signalling complexes was first assessed by immunofluorescence microscopy (Grabner et al. 1998), but this approach was unable to provide information on the functionality of channel and receptors proteins within a subcellular domain. The resulting images are likely to represent mixed populations of both functional and silent channels and receptors, as well as those in reserve pools waiting to be recruited under changing physiological or pathological conditions. Recent methodological advances have made it possible to routinely image the topography of a live cardiomyocyte and study the clustering of functional ion channels and receptors as well as their coupling within a specific microdomain (Bhargava et al. 2013). In this review we highlight the emerging understanding of distinct subcellular microdomains in cardiomyocytes and of their functional role in the accumulation and regulation of distinct subcellular populations of different ion channels and regulatory receptors as well as their differing regulatory pathways and contributions to cellular signalling.
Transverse tubules
Transverse tubules (T-tubules) are invaginations of the surface membrane that occur at each Z-disk, resulting in the formation of both transverse and longitudinal elements throughout the cardiac myocyte (Fawcett and McNutt 1969). The highly organized system of T-tubules forms a three-dimensional (3D) network which allows synchronization of myofilament contraction within the whole cell. The T-tubule system forms tight couplings with the sarcoplasmic reticulum (SR) membrane, termed dyads, and conducts an electrical impulse that triggers calcium ion (Ca2+)-dependant Ca2+ release from the SR (Kaftan et al. 1996). Synchronized Ca2+ release during each membrane excitation allows co-ordinated contraction among the many contractile units within each working ventricular myocyte in each heartbeat. Ultimately, synchronized myofilament contraction within and among millions of working cardiac myocytes will enable the heart muscle to generate the maximal contractile force.
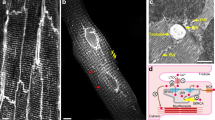
The T-tubule network is traditionally visualized by conventional epifluorescent or confocal imaging of fluorescently labelled cells and electron microscopy techniques. However, a recently developed technique, scanning ion conductance microscopy (SICM), which is a non-contact scanning microscopy technique based on the principle that the flow of ions through the nanopipette filled with electrolytes decreases when the pipette approaches the surface of the sample, enables 3D visualization of surface structures on live cardiomyocytes (Hansma et al. 1989; Korchev et al. 1997; Bhargava et al. 2013). The result is a 3D topography image of live cells (Fig. 1a–c). In SICM, a sharp borosilicate glass nanopipette (inner diameter 100 nm) mounted on a three-axis piezo-actuator scans the sample of interest and the ion current is measured between the pipette tip and the sample. To begin scanning, the pipette is moved towards the sample, thus decreasing the pipette–sample distance. A distance-modulated feedback control system keeps the ionic conductance and sample–pipette distance constant. Thus, the pipette never touches the sample, but stops at a distance equivalent to the inner radius of the pipette (Novak et al. 2009), thus allowing noncontact scanning. During scanning, the sample is moved laterally in the X and Y directions while the pipette is not moved laterally, only vertically (Z direction) (Novak et al. 2009). The corresponding vertical and lateral displacements are recorded and used to build a 3D image of the sample surface. The pipette’s inner tip diameter varies from 20 to 100 nm (Rheinlaender and Tilman 2009). As the resolution depends on the radius of the pipette inner tip, SICM can obtain a maximal resolution of 13 nm (Shevchuk et al. 2006). SICM represents an alternative to conventional high-resolution microscopy (Fig. 1a–d), especially in imaging topography of live biological samples. A regular structure of lines of T-tubule openings forming Z-grooves, as well as the areas between them, termed crests, are clearly visible on SICM topography images of adult cardiomyocytes (Fig. 1a). These T-tubule openings are spaced 2 μm apart, similar to the internal T-tubule structures.
Loss of transverse tubules (T-tubules) and surface topography changes in ventricular myocytes from the failing human heart. Scanning ion conductance microscopy (SICM) images from the surface of myocytes isolated from nonfailing (a) and failing (b) human hearts. Black dotted line represents the linear selection presented as a 1-dimensional (1D) surface contour map from nonfailing (c) and failing (e) human myocytes. d, f Confocal images after staining with di-8-ANNEPPS in human nonfailing (d) and failing myocytes (f). g, h T-tubule (g) and Z-groove (h) ratios in myocytes isolated from patients with dilated cardiomyopathy (DCM), heart failure (HF) secondary to ischaemic heart disease (IHD) or hypertrophic obstructive cardiomyopathy (HOCM); NF nonfailing. i Prolonged contraction time to peak (TTP) and relaxation times (R50 and R90) in failing human myocytes (solid bars, n = 12) compared with nonfailing human myocytes (open bars, n = 6). **P < 0.01 vs. nonfailing. From Lyon et al. (2009)
The dogma that T-tubules are present only in ventricular myocytes and are either absent or less developed in atrial, pacemakers or conducting tissue (Ayettey and Navaratnam 1978; Huser et al. 1996; Cordeiro et al. 2001) has largely been disputed. Some studies have shown that the T-tubule network is present in atrial tissue of both small (Kirk et al. 2003) and large mammalians and humans (Richards et al. 2011). Recently, we found that approximately half of rat atrial myocytes have a T-tubular network (Glukhov et al. 2013). Among atrial myocytes with T-tubules, we distinguished those with organized T-tubular networks similar to those identified in ventricular myocytes, and those with disorganized T-tubules. The left atrium contains more cells with an organized T-tubule system than the right atrium.
The organized T-tubule structure is critical for normal excitation–contraction coupling and cardiac function. T-tubules have been shown to accumulate a number of molecules that are important in Ca2+ signalling, such as L-type calcium channels (LTCCs), sodium ion (Na+)/Ca2+ exchanger (NCX), β2 adrenergic receptors, protein kinase A (PKA) and other regulatory proteins, many of them in a signalosome with the LTCCs (Davare et al. 2001). All together, these molecules form macromolecular signalling complexes targeted to specific membrane domains (Best and Kamp 2012). Clustering of these macromolecular complexes is essential for the proper timing of molecular events that couple electric activation with the contraction of the cardiac myocyte, and for autonomic regulation of excitation–contraction coupling.
L-type calcium channels
Each LTCC is composed of a single pore forming α1 and smaller auxiliary β and α2δ subunits (Best and Kamp 2012); in some tissues the γ subunit is also present (Catterall 2000; Kamada et al. 2004). The α1 subunit is the main pore-forming structure and contains specific sites that interact with auxiliary subunits, binding sites for activators and blockers and PKA (Hell et al. 1993, 1995). Cav1.2 (α1C, encoded by the CACNΑ1C gene) is the predominant α1 subunit expressed in ventricular myocytes; however, in atrial tissue both Cav1.2 and Cav1.3 subunits (α1D, encoded by CACNA1D) are present (Mikami et al. 1989). Although the α1 subunit largely determines the current gating of the channel, the auxiliary subunits affect the voltage-dependence, the rate of activation and the kinetics of current inactivation of the channel (Lacerda et al. 1991; Birnbaumer et al. 1998). The auxiliary subunits also determine the increase in current density (Singer et al. 1991; Hermosilla et al. 2011) and the open probability and the duration of the current (Singer et al. 1991; Kamp et al. 1996), and enhance ligand binding to the α1 subunit (Chien et al. 1995). For example, both functional and radio-ligand binding studies have provided evidence that Ca2+ channel inhibition is affected by the interaction between the Cavα1 and Cavβ subunits of the channel (Mitterdorfer et al. 1994). The apparent sensitivity of Cav1.2 channels to verapamil has been observed to be almost 14-fold higher if the Cavα1 subunit of the Cav1.2 channel is co-expressed with the Cavβ3 as compared with sole Cavα1 expression (Lacinova et al. 1995). In addition, Cavβ subunits promote trafficking of the channel complex to the plasma membrane and modulate gating properties of the channel (Rickert and Fischer 1975; Chien et al. 1995; Kamp et al. 1996; Bichet et al. 2000).
Specific phosphorylation of amino acid residues in the carboxyl terminus of the Cavβ2 subunit, in contrast to other Cavβ subunits, has been described as an important determinant of the difference seen among Cavβ subunits in terms of Cav1.2 regulation by PKA (Gerhardstein et al. 1999). Four main categories of modulating effects have been observed (Foell et al. 2004): (1) changes in channel gating; (2) alterations in membrane trafficking and localization of channels; (3) regulation of channels by second messenger systems; (4) alterations in drug block properties. To date, four β subunit isoforms (β1–β4) have been described which are coded by distinct genes (CACNB1–4, respectively) that undergo alternative splicing to generate at least 18 unique β subunit isoforms in the human myocardium (Foell et al. 2004). The human heart expresses a number of Cavβ1 (Collin et al. 1993), Cavβ2a (Perez-Reyes et al. 1992) and Cavβ3 isoforms (Hullin et al. 2003), while rabbit and rat hearts show only Cavβ2 expression (Hullin et al. 1992; Haase et al. 2000).
Co-expression of Cavβ subunits with the pore-forming Cav1.2 subunit has multiple functional effects. Co-expression of human Cavβ1b and Cavβ1d subunits increases single-channel activity of the rabbit LTCC α1c-subunit in HEK-293 cells (Cohen et al. 2005). An increased activity of the α1c-subunit co-expressed with Cavβ2a also occurs in COS-7 cells (Kamada et al. 2004). Current characteristics of the α1c subunit co-expressed with β2a have been found to differ from those of native channels (Birnbaumer et al. 1998; Yamada et al. 2001; Kamada et al. 2004). The β2c subunit has also been found to be expressed in rat ventricular myocytes. Whole-cell patch clamp recordings demonstrated that the inactivation kinetics of recombinant channels co-expressed with β2c subunits differ from those with β2a subunits but are comparable to those of the native cells (Yamada et al. 2001).
Immunolabelling analysis of canine ventricular membrane fractions demonstrated that all four Cavβ subunits are expressed at the protein level and that the Cavβ subunits show differential subcellular localization (Foell et al. 2004). In the ventricles, Cavβ1b, Cavβ2 and Cavβ3 are predominantly localized to the T-tubule, whereas Cavβ1a and Cavβ4 are more prevalent on the surface of the cell (Foell et al. 2004). Earlier investigations showed that Cavβ2 and α1C subunits co-localize on T-tubule membranes in rabbit ventricular myocytes (Gao et al. 1997). Interestingly, atrial and ventricular myocytes show different levels of mRNA of the β2 subunits. For example, the expression of β2 subunits is significantly higher in the ventricle than in atrium, while β4 is highly expressed in atria than in ventricles (Chu et al. 2004).
Immunostaining studies of ventricular cells (Scriven et al. 2000; Brette and Orchard 2003; Brette et al. 2006) demonstrated that approximately 80 % of all LTCCs are located in T-tubules in close proximity to the Ca2+ sensing and release units, the ryanodine receptors (RyRs) at the SR (Smyrnias et al. 2010). Such T-tubule organization allows the electrical impulse to be conducted effectively into the cell interior, where Ca2+ influx triggers the opening of RyRs and subsequent release of Ca2+ from SR stores, which in turn brings about cell contraction (Kaftan et al. 1996). Detailed descriptions of the microarchitecture of the dyads and LTCC–RyR interaction are provided by Winslow and Greenstein (2011) and Scriven et al. (2013).
Until recently, spatial distribution of LTCCs on the cellular membrane was assessed by immunolabelling or electron microscopy techniques that are unable to provide information on the functionality of the visualized proteins. As a result, the observed images likely represent mixed populations of both functional and silent channels, as well as those in reserve pools waiting to be recruited under changing physiological or pathological conditions (Gu et al. 2002). However, recent methodological developments now enable study of the clustering of functional ion channels within specific microdomains (Bhargava et al. 2013; Novak et al. 2013). To examine the distribution of functional ion channels on a cellular membrane, we used a combination of SICM and conventional patch clamp in a technique which we refer to as super-resolution scanning patch clamp (Bhargava et al. 2013). In this method the same glass nanopipette is used to image the surface of the cell (as described earlier in this review) and to record ion channel current, thereby enabling registration of a single channel activity from the precise location. In brief, the first step is to generate a high-resolution topographical image of the cell surface, as described above (Fig. 2a, left). The tip of the pipette is then clipped using a software-controlled movement of the piezo-actuator. Technical details of the development of this method are described in Novak et al. (2013). After generating the topographical image of the cardiac myocyte surface, the pipette (internal diameter approx. 100 nm) is moved to an area clear of cells or debris. At that coordinate, the pipette is lowered onto the solid surface of the dish at high velocity and the tip of the pipette is clipped in a controlled manner (Fig. 2a, middle). The pipette resistance is continuously monitored and the clipping can be repeated until the current through the pipette reaches the desired level (this correlates with the desired pipette tip diameter). The pipette is then repositioned to the specific location on the cell surface that has been selected based on the topography image recorded previously with the sharp pipette (Fig. 2a, right). The lateral error of repositioning depends on the accuracy of the X–Y piezo-actuators, and in our experience is about ±2 nm (Novak et al. 2013).
Super-resolution scanning patch-clamp reveals distribution of functional L-type calcium (Ca2+) channels in ventricular myocytes. a A sharp high-resistance pipette used to resolve the topographical structure of the myocytes. The pipette is moved to a cell-free area on the dish and the fall rate is increased to clip the pipette tip. The pipette is then returned to the surface of choice, and patch clamp can be performed with a wider pipette tip. b Functional L-type Ca2+ channels recorded in the T-tubule (left panel) and crest (right panel). c Occurrence of functional L-type Ca2+ channels (LTCC) recorded in T-tubules and crest in rat adult ventricular myocytes. From Bhargava et al. (2013)
Using this new method, Bhargava et al. (2013) recently assessed the likelihood of detecting LTCCs in discrete regions of the sarcolemma. The distribution of functional LTCCs recorded in dyadic (T-tubules) and extradyadic (crest of the sarcolemma) microdomains in rat adult ventricular myocytes are shown in Fig. 2b, c. Of 30 patches formed with a clipped pipette (Rp = 30–35 MΩ) in the crest region, only two showed channel activity (6.6 %) as opposed to a higher LTCC activity observed in 23 of 80 patches in T-tubules (28.75 %; P < 0.02) (Fig. 2c). The low occurrence of channels at the crest, their sensitivity to isoproterenol and their biophysical properties are all consistent with the notion that the obtained recordings are from LTCCs, with nanoscale spatial resolution (Chen-Izu et al. 2000; Gu et al. 2002).
Of note, the probability of recording LTCCs on the surface of neonatal rat ventricular myocytes, which lack T-tubular structures (Haddock et al. 1999), was 30.8 % (LTCC activity observed in 4/13 separate recordings; Bhargava et al. 2013), suggesting that the structural organization of the T-tubule coincides with increased clustering of functional LTCCs at that specific location. Lack of a regular T-tubular system in atrial myocytes has been thought to underlie their unique Ca2+ signalling (Dobrev et al. 2009). Thus, differential subcellular distribution of LTCCs and their coupling to RyRs of the SR have been proposed in atrial myocytes (Trafford et al. 2013). Using super-resolution scanning patch clamp, Glukhov et al. (2013) recently uncovered that in atrial myocytes functional LTCCs appear at similar frequency in both T-tubules and in the crest areas of the sarcolemma, in contrast to observations made in ventricular myocytes where LTCCs were found in a previous investigation to cluster predominantly in T-tubules (Bhargava et al. 2013). Interestingly, atrial LTCCs found in the crest have a lower amplitude at more negative voltages than the LTCCs recorded in the T-tubules, possibly due to either their differential structure (Foell et al. 2004) or to various subcellular environments within the specific microdomains (Best and Kamp 2012).
Ca2+ efflux
The T-tubular network is not only an important site for Ca2+ influx prior to contraction, but also for Ca2+ extrusion during diastole. Chase and Orchard (2011) demonstrated that T-tubules are responsible for approximately 71 % of trans-sarcolemmal Ca2+ extrusion. Ca2+ efflux occurs by three main routes: re-sequestration of Ca2+ into SR via a Ca-ATPase (SERCA), Ca2+ removal from the cell by NCX and plasmalemmal Ca2+-ATPase (PMCA). By using pharmacological separation as well as a detubulation procedure, Chase and Orchard (2011) demonstrated that in rat ventricular myocytes the SR is responsible for 86 % of cytoplasmic calcium removal, NCX for 8 % and Ca2+-ATPase for 6 %. These authors also demonstrated that Ca2+ extrusion via the sarcolemmal Ca2+-ATPase occurs only at the T-tubules and is not regulated by basal PKA activity, while Ca2+ extrusion via NCX occurs across both the surface (34 %) and T-tubule membranes (66 %), but predominantly across the T-tubule membrane due, in part, to localized stimulation of NCX by PKA at the T-tubules. These results agree with previous estimates obtained by co-immunolocalization analysis (Scriven et al. 2000; Thomas et al. 2003). In addition to local positive control of SR Ca2+ release by LTCC, NCX that is located closely to the junctional SR has been proposed to negate local Ca2+-induced Ca2+ release by suppressing SR Ca2+ leakage and Ca2+ sparks throughout the period of rest (Bovo et al. 2014). It should be noted that the fraction of Ca2+ that is reuptaken into the SR by SERCA or extruded from the cell by NCX and PMCA may vary significantly depending on the animal species. In rats and mice, Ca2+ removal mechanisms predominantly rely on SERCA activity, whereas in larger species (e.g. rabbit, human), there is a significant contribution of NCX to cytosolic Ca2+ concentration ([Ca2+]I) regulation. As shown by Bassani et al. (1994) the fractions of Ca2+ transported during a twitch by the SR, NCX and slow systems are 70, 28 and 2 %, respectively, in rabbit myocytes and 92, 7 and 1 %, respectively, in rat myocytes. This leads to the proposal that spatial organization of the Ca2+ extrusion mechanisms may vary from species to species similar to Ca2+ influx mechanisms. Detailed reviews of recent and ongoing discoveries that focus on the dyad structure and function can be found elsewhere (Cannell and Kong 2012; Scriven et al. 2013; Sipido et al. 2013; Sipido and Cheng 2013).
A small fraction of brain-type tetrodotoxin-sensitive Na+ channels has recently been located within the T-tubules (Lin et al. 2011). These channels are thought to be involved in modulation of local Na+/Ca2+ signalling (Radwanski et al. 2012), as it will be discussed later in this review in the section describing microdomain-specific distribution of Na+ sodium channels.
T-tubule loss in cardiac disease
Numerous heart diseases are associated with a progressive loss of the T-tubular structure. In this review, we focus on cardiac remodelling caused by heart failure and atrial fibrillation as major causes of morbidity and mortality. The most common “stressors” of both heart failure and atrial fibrillation remodelling include tachycardia and volume or pressure overload. Specific stressors, such as diastolic dysfunction, ischaemia and valve insufficiency, increase pressure and/or volume load on the chambers. These specific factors trigger intracellular changes, such as cardiac myocyte growth, hypertrophy, necrosis and apoptosis, as well as changes in metabolism and in the expression of cellular ionic channels and hormones. Such changes create a substrate for remodelling with structural, functional, electrical, metabolic and neurohormonal consequences.
Heart failure is characterized by a weakened myocardial contractile force, partially due to abnormal excitation–contraction coupling resulting in reduced SR Ca2+ release (Bito et al. 2008; Lyon et al. 2009, 2011). Cardiac myocyte micro-architecture is critically important to the efficacy of Ca2+-induced Ca2+ release and the stability of the amplification mechanism. Chronic heart failure is characterized by a reduction of T-tubule density in rodent failing hearts (Louch et al. 2006; Song et al. 2006). Cardiac myocytes isolated from failing spontaneous hypertensive rats demonstrated temporal delay in excitation–contraction coupling related to increased spatial separation of the junctional SR from the T-tubule membrane (Song et al. 2006; Heinzel et al. 2008), with an associated increase in spontaneous Ca2+-release events (Ca2+ sparks) (Song et al. 2006). Experimental disruption of T-tubule structures by either prolonged culturing or osmotic shock produces changes similar to those observed in heart failure, with dyssynchronous release of Ca2+ leading to a slow Ca2+ transient as well as diminished contractile amplitude and a prolonged contraction cycle (Lipp et al. 1996; Brette et al. 2004, 2005).
In one of the studies carried out by our group, we confirm the loss of T-tubule structures in ventricular myocytes from patients with heart disease (Fig. 1) in a cell population typical of myocytes isolated from failing human ventricle, as evidenced by contractile properties (Lyon et al. 2009). Interestingly, T-tubule changes were seen not only in ischaemic and dilated cardiomyopathy but also in myocytes isolated from sections taken during septal reduction from hearts with hypertrophic obstructive cardiomyopathy. We also found that T-tubule loss cannot be considered to be an isolated phenomenon in the failing human heart; rather, it occurs as part of a general disruption of the sarcolemma. Significant changes to the remaining sarcolemmal architecture included loss of Z-grooves and reduced depth of the remaining Z-grooves interconnecting the T-tubule openings in failing ventricular myocytes (Fig. 1). The observed pathological changes in surface structure appeared to be independent of the underlying etiology. Similar changes were observed in the ventricular myocytes from the infarcted failing rat hearts, with Z-groove structures markedly disrupted. Parallels between the human and rat myocytes suggest that the surface structure alterations are an integral part of the remodelling process that occurs during cardiac failure.
Reduction of the T-tubular network in ventricular myocytes leads to spatial heterogeneity of Ca2+ transient alternans (Lipp et al. 1996), underlining the importance of this system for excitation–contraction coupling. Thus, loss of T-tubules is a key component of the electrophysiological coupling required for dyad formation. However, it remains unknown how this loss of structural organization affects the spatial location and activity of LTCCs. Alteration of single-channel activity and regulation of macroscopic LTCC current have been reported in heart failure, although the data are divergent (Benitah et al. 2010). Also, some studies have reported a decrease in LTCC current density (Santos et al. 1995; Aimond et al. 1999), while others found no change in macroscopic LTCC current (Song et al. 2005). It has been hypothesized (Benitah et al. 2002; Bito et al. 2008) that the communication between LTCCs and other proteins involved in excitation–contraction coupling is impaired in heart failure, but as yet the underlying mechanism has not been elucidated.
Several proteins have been implicated in tubulogenesis, including titin cap protein (telethonin, TCAP), junctophilin subtype 2 (JPH2) and the Bin/amphiphysin/Rvs (BAR) domain protein amphiphysin II (AmpII or BIN1) [reviewed in Ibrahim et al. (2011) and Trafford et al. (2013)]. Telethonin is a stretch-sensitive Z-disc protein that binds to proteins in the T-tubule membrane (Knoll et al. 2002). Telethonin is known to play an important role in the response to cardiac overload, and mutations in telethonin can give rise to both hypertrophic and dilated cardiomyopathy, possibly related to altered stretch-sensing properties (Hayashi et al. 2004). In a study using telethonin knock-out mice, Ibrahim et al. (2013) recently demonstrated that the loss of telethonin from cardiomyocytes is associated initially with an isolated T-tubule defect, including the loss of both T-tubule density and regularity, as well as with severe loss of cell surface ultrastructure, with minor Ca2+ handling changes and normal heart and cellular function. This defect becomes worse with ageing and is associated with significant changes in Ca2+ cycling. With the recent discovery that truncating mutations in titin are a common cause of dilated cardiomyopathy (Herman et al. 2012), and earlier work documenting telethonin mutations in dilated cardiomyopathy, the titin–telethonin axis is emerging as a powerful regulator of cardiac structure and function, in particular in response to mechanical load variation.
JPH2, which is positioned near RyR and in the dyadic cleft, has been invoked as a key regulator, although much of the evidence is still associative. The cytoplasmic domain of this protein has been suggested to have a high affinity to membrane phospholipids and can create structural junctions with T-tubules or with the surface sarcolemma. JPH2 has also been shown to play a critical role in T-tubule maturation (Reynolds et al. 2013). Loss of JPH2 expression results in T-tubule remodeling after pressure overload, as demonstrated by studies in cultured myocytes and a transgenic mouse model expressing JPH2 short-interfering RNA (Wei et al. 2010). Zhang et al. (2014) recently reported that JPH2 is required for the protective effect of microtubule depolymerization on T-tubule structure after cardiac stress. These authors identified altered JPH2 localization from the T-tubule membrane to the surface plasma membrane in response to stresses that induce microtubule densification. Overexpression of JPH2 has been shown to provide significant protective benefits after pressure overload, stabilizing the T-tubule network and attenuating heart failure after cardiac stress (Guo et al. 2014).
In addition to JPH2, recent studies have suggested that the membrane scaffolding protein BIN1 is another important regulator of T-tubule structure and function. BIN1 is known to induce membrane invaginations (Butler et al. 1997) and initiate tubulogenesis in skeletal muscle cells (Lee et al. 2002). It deforms the membrane bilayer through interaction between its N-terminal positively charged BAR domain and acidic phospholipids within the cell membrane (Lee et al. 2002). BIN1 can induce LTCC-enriched membrane folds in cell lines and immature muscle cells (Hong et al. 2010). In adult cardiomyocytes, BIN1 localizes to cardiac T-tubules and facilitates cytoskeleton-based Ca2+ channel trafficking to the T-tubule membrane (Hong et al. 2010). The expression of BIN1 is transcriptionally decreased in acquired human and experimental animal heart failure, a condition that is also associated with both intracellular accumulation of LTCCs and abnormal T-tubule morphology (Hong et al. 2012b). In mice with cardiac BIN1 deletion, T-tubule folding is decreased, which does not change overall cardiomyocyte morphology but leads to free diffusion of local extracellular Ca2+ and potassium (K+) ions, prolonging action-potential duration and increasing susceptibility to ventricular arrhythmias (Hong et al. 2014).
In heart failure, the potentiation of LTCC current by beta-adrenergic regulation is lost, indicating phosphorylation defects (Zhang et al. 1995; Aimond et al. 1999). We recently demonstrated that β2 adrenergic receptors (β2ARs) are located in the T-tubule openings on the surface of healthy ventricular myocytes (Fig. 3), which was confirmed by a localized response of a second messenger, cAMP (Nikolaev et al. 2010). Interestingly, in failing cardiac myocytes, β2ARs redistribute from the T-tubule microdomains and are detected elsewhere across the plasma membrane, which correlates with impaired cAMP signalling through these receptors. An association between β2ARs and LTCCs within the Ca2+ signalling complex in neurons has been previously shown (Davare et al. 2001), leading to the hypothesis that the relocalization of β2ARs in heart failure may be accompanied by relocalization of LTCCs to the sarcolemma, thereby possibly explaining the loss of LTCC communication with RyRs in dyads. Our preliminary results obtained from both the rat model of heart failure (Bhargava et al. 2012) and patients with dilated cardiomyopathy (Sanchez-Alonso et al. 2014) confirm this hypothesis. On a molecular level, Hullin et al. (1999) reported that human failing ventricular cells demonstrated a decrease in expression of auxiliary β subunits and that at the same time the mRNA level of the a1c subunit remained unchanged. In a subsequent study in human failing ventricular myocytes, Hullin et al. (2007) showed an increased expression of the auxiliary β2 subunit.
Nano-scale relocalization of β2 adrenergic receptors (AR) in rat ventricular myocytes during heart failure. a Functional localization of βAR-induced cAMP signalling and the principle of the combined nanoscale SICM–Förster resonance energy transfer (FRET) approach. Typical SICM image of a rat myocyte shows defined morphological structures that are used to position the nanopipette and to stimulate receptors in a highly localized fashion. Receptor activity is measured by monitoring the production of cAMP by Epac2-camps, a FRET-based cAMP sensor that changes its conformation and fluorescence properties upon activation—i.e. cAMP binding. b, c Differences in spatial organization of cAMP signalling in myocytes from healthy rats and rats with HF. b Local stimulation (isoproterenol (ISO) + β1-antagonist (CGP)] of β2ARs in the T-tubule of a healthy myocyte demonstrates a locally confined cAMP response detectable only at the site of stimulation (arrow, n ≥ 7). The graph shows changes in the FRET ratio [yellow fluorescent protein (YFP)/cyan fluorescent protein (CFP)]measured in five different regions (differently coloured ovals, left). c β2AR stimulation in a detubulated area of a failing cell induces a global cAMP signal propagating throughout the cytosol (n ≥ 7). From Nikolaev et al. (2010)
A 45 % decrease in T-tubule density in the sheep model of persistent atrial fibrillation has been associated with fewer LTCC–RyR couplings and reduced efficiency of the excitation–contraction coupling (Lenaerts et al. 2009). In a sheep model of heart failure, T-tubules were found to be disrupted more dramatically in atrial than in ventricular myocytes (Louch et al. 2004, 2006; Dibb et al. 2009). This effect occurs as a result of T-tubule structural degradation and cellular hypertrophy. Naturally, this loss of T-tubules and disruption in dyad coupling are accompanied by dramatic changes in the spatial profile of the systolic Ca2+ transient.
At present LTCC regulation in atrial myocytes remains largely unknown as does their structural change during pathology. However, there are a few reports of patients with atrial fibrillation showing a marked reduction of LTCC current density (Bosch et al. 1999) and increased activity of single LTCCs (Klein et al. 2003). Klein et al. (2003) suggested that one possible mechanism of the increased single channel open probability during atrial fibrillation might involve a reduced activity of phosphatase 2A which is responsible for channel dephosphorylation.
Caveolae
While the T-tubule/SR interface represents a prime locus of signalling cascades compartmentation leading to excitation–contraction coupling, another membrane structure which is of key importance in the spatial control of signalling in the cardiac myocyte is the caveola. Caveolae are invaginations of the plasma membrane rich in cholesterol, glycophospholipids and lipid-anchored proteins (Razani et al. 2002; Cohen et al. 2004; Gratton et al. 2004; Harvey and Calaghan 2012). Caveolin, the main protein component of caveolae, recruits components of various signalling pathways, including GI proteins, endothelial (Lisanti et al. 1994) nitric oxide synthase (Barouch et al. 2002; Feron and Balligand 2006) and several protein kinases. Three genes (CAV1–3) encode six known caveolin subtypes (caveolin-1α and -1β; caveolin-2α,-2β and -2γ; caveolin-3) that are variably distributed in different tissues (Razani et al. 2002). Caveolin (Cav) 1 and Cav2 are expressed in most cell types, whereas expression of Cav3 is restricted to cardiac, skeletal and smooth muscle types, as well as some types of neurons; Song et al. 1996; Razani et al. 2002; Boulware et al. 2007). The lack of morphologically distinct caveolae in skeletal muscle from Cav3 knockout mice highlights the importance of caveolin in caveola formation (Galbiati et al. 2001). Neonatal ventricular myocytes lack T-tubules but have an increased density of caveolae. T-tubular development in striated muscle depends on cholesterol and Cav3 (Parton et al. 1997; Razani et al. 2002), suggesting that caveolae may be a developmental precursor of T-tubules and share some of their functions. Along with the essential scaffolding protein Cav3, a number of different ion channels and transporters have been found to localize to caveolae in ventricular myocytes, including Ca2+ and Na+ channels, pacemaker channels (HCN4), Na+/Ca2+ exchanger and others (Balijepalli and Kamp 2008). Closely associated with these channels are specific macromolecular signaling complexes that provide highly localized regulation of the channels.
In addition to the presence of critical subpopulation of LTCCs localized to dyadic junctions, extradyadic LTCCs associated with district regions of the surface membrane have also been distinguished (Balijepalli et al. 2006; Makarewich et al. 2012). Several methods, including co-immunoprecipitation (Balijepalli et al. 2006; Shibata et al. 2006), immunofluorescence (Balijepalli et al. 2006; Cavalli et al. 2007) and caveolae-specific inhibition of LTCCs (Makarewich et al. 2012) have been used to demonstrate the presence of LTCCs within caveolae in ventricular myocytes. The presence of Cav3 has been used as a marker of the localization of proteins to caveolae versus non-caveolar lipid rafts. Using the super-resolution scanning patch clamp technique, we have recently provided the first direct evidence of caveola-specific localization and regulation of functional LTCCs in atrial cardiomyocytes (Glukhov et al. 2014). These extradyadic channels were completely abolished following caveola disruption by methyl-β-cyclodextrin treatment.
The function of LTCCs localized in caveolar structures remain open to question. It has been proposed that some LTCCs housed in Cav3–rich signalling microdomains could play an important role in the modulation of Ca2+ signalling, particularly in cells lacking T-tubules, such as atrial (Schulson et al. 2011) and neonatal ventricular (Lohn et al. 2000) myocytes. Our recent data (Glukhov et al. 2014) indicate that caveola-targeted LTCCs might be responsible for an abundant peripheral (nonjunctional) focal Ca2+ release (Ca2+ sparks) in atrial myocytes, probably via inositol 1,4,5-trisphosphate (IP3)-dependent activation of nonjunctional RyRs (Woo et al. 2003; Wang et al. 2005). Recently, using a caveola-targeted LTCC antagonist, Makarewich et al. (2012) demonstrated in ventricular myocytes that the Ca2+ influx through LTCCs within caveola signaling domains can activate pathological cardiac hypertrophic signalling. Notably, the authors demonstrated that this Ca2+ influx can be selectively blocked without reducing cardiac contractility (Makarewich et al. 2012).
Ca2+ can also enter cardiac myocytes not only through LTCCs, but also through the voltage-operated T-type Ca2+channel (TTCC). These channels are expressed throughout cardiac development until the end of the fetal/neonatal period (Niwa et al. 2004) when their expression decreases, with subsequent low expression in the atria and pacemaker cells of normal adults and no expression at all in normal adult ventricular myocytes. TTCCs can reappear when the heart is subjected to pathological stressors, such as myocardial infarction (Huang et al. 2000) or atrial fibrillation (Fareh et al. 1999). Three TTCC genes have been identified, but only Cav3.1 (α1G) and Cav3.2 (α1H) have been found in the heart (Niwa et al. 2004). All TTCCs have similar biophysical properties, including activation at more negative voltages and faster inactivation than LTCCs. In contrast to LTCCs, immunocytochemical labelling of Cav3.1 revealed the presence of TTCCs primarily on the surface sarcolemma of ventricular myocytes, with less staining within the T-tubules (Jaleel et al. 2008). This observation has led to the hypothesis that nonjunctional localization of TTCCs could explain their lower efficiency in excitation–contraction coupling compared to LTCCs (Sipido et al. 1998; Zhou and January 1998; Jaleel et al. 2008). It has been recently demonstrated that the TTCCs are localized to caveolar microdomains in the ventricular myocytes and that Cav3 interacts with the Cav3.2 channel and regulates its function (Markandeya et al. 2011).
Re-expression of TTCCs under pathological stresses suggests that TTCCs play a role in cardiac hypertrophy and failure (Chiang et al. 2009; Kinoshita et al. 2009). However, results from experiments aimed at assessing the role of Ca2+ influx through TTCCs in pathological hypertrophy remain controversial, with some investigators proposing that TTCCs diminish hypertrophy (Nakayama et al. 2009) and others highlighting a greater role of LTCCs in this process (Jaleel et al. 2008). There is also some evidence that Ca2+ entry through Ca2+-permeable, nonselective cation transient receptor potential (TRP) channels can promote cardiomyocyte hypertrophy via activation of the calcineurin (Cn)–nuclear factor of activated T cells (NFAT) signalling pathway (Nakayama et al. 2006). The TRP canonical (TRPC) channel family has seven family members, with TRPC1 (namely, C3-7) being expressed in the heart (Wu et al. 2010). TRPCs are expressed at very low levels in normal adult cardiac myocytes, but the expression and activity of select isoforms seems to increase in pathological hypertrophy and heart failure (Bush et al. 2006). Using methyl-β-cyclodextrin treatment as well as a caveola-targeted LTCC inhibitor, Rem1-265-Cav, Makarewich et al. (2014) recently reported that TRPCs and LTCCs work in a coordinated fashion to activate Cn-NFAT signalling and that this interaction is targeted to caveola microdomains. Although TRPC channels are typically recorded in the plasma membrane or in specialized lipid microdomains containing caveolae (Lockwich et al. 2000; Makarewich et al. 2014), other authors have reported a non-caveola localization of certain TRPC isoforms (Goel et al. 2007; Jiang et al. 2014).
Since a variety of different ion channels are localized to caveola microdomains, it has been proposed that caveola-specific ion channel remodelling can be critical to pathological remodelling and the genesis of arrhythmias. The extent to which caveolar ion channels contribute to these conditions is only just emerging. Given that ion channels co-localize with Cav3 in caveolae, their pathological modifications may underlie arrhythmia mechanisms in clinical conditions such as hypertension, diabetes, ischaemic heart disease and heart failure. Structural remodelling of caveolae has been observed during certain cardiac pathologies. The distribution of Cav3 protein is dramatically altered in heart failure, with an increased proportion of Cav3 in the detergent-soluble fraction (Ratajczak et al. 2003). Interestingly, pharmacological drugs widely used for the prevention of cardiovascular disease, such as statins and atorvastatin, which directly act on the cholesterol synthesis pathway and lipids rafts, affect caveolar turnover by limiting their endocytosis (Goebel et al. 2005; Peivandi et al. 2005).
Mutations in CAV3 have been linked to the long QT (LQT) syndrome phenotype associated with a two- to threefold increase in late Na+ current (I Na,late) compared with wild-type Cav3 (Vatta et al. 2006). Vaidyanathan et al. (2013) have shown that Kir2.1 loss of function is additive to the increase described previously in late I Na, prolonging repolarization and leading to arrhythmia generation in Cav3-mediated LQT9. Similar increases in late I Na as well as reduced L-type calcium current (I Ca,L) and potassium current I to, but no changes in I K1, have been observed in Cav3-/- mice (Markandeya et al. 2013).
Intercalated discs
Coordinated contraction of the heart depends on proper mechanical and electrical coupling between all cardiac myocytes. Cardiac myocytes are connected end to end by a specialized structure called the intercalated disc that serves as an organizing centre for various cell-surface proteins, including junctional complexes critical for cell–cell attachment and cell–cell communication (Spach et al. 1981). Mechanical attachment is provided by desmosomes and adherens junctions, whereas gap junctions provide a pathway for the passage of ions and small molecules between cells (Sato et al. 2011).
Sodium channels
Voltage-gated Na+ (NaV) channels play a critical role in the rising phase of the action potential and thus in cardiac electrical propagation. They are composed of one large pore-forming α-subunit and one or more smaller ancillary β-subunits (Catterall 1992; Isom et al. 1994). Several α-subunit isoforms have been identified with distinct patterns of development and localization in various tissues, with different physiological and pharmacological properties (Fozzard and Hanck 1996). Isoforms preferentially expressed in the central nervous system, i.e. Nav1.1, Nav1.2, Nav1.3, and NaV1.6, are inhibited by nanomolar concentrations of tetrodotoxin, such as the isoform present in adult skeletal muscle (NaV1.4). In contrast, the primary cardiac isoform, NaV1.5, requires micromolar concentrations of tetrodotoxin for inhibition (Fozzard and Hanck 1996).
The tetrodotoxin-resistant NaV1.5 is most prominent in various cardiac preparations, but recent studies indicate that the tetrodotoxin-sensitive brain-type isoforms are also present in the conduction system (Baruscotti et al. 1997; Maier et al. 2003; Lei et al. 2004; Haufe et al. 2005) and ventricular myocytes (Dhar Malhotra et al. 2001; Maier et al. 2004; Duclohier 2005; Haufe et al. 2005). The growing body of experimental results indicates that these isoforms have distinct subcellular localizations and functions. Immunocytochemistry studies show that NaV1.1, NaV1.3 and NaV1.6 are present uniformly across the sarcolemma in the T-tubular system, whereas NaV1.5 channels are clustered primarily at unique sites within the intercalated discs (Cohen 1996; Maier et al. 2002, 2004).
Using the cell-attached macropatch configuration technique, Lin et al. (2011) demonstrated that tetrodotoxin-sensitive channels are located only in the cell midsection region of ventricular myocytes—and not in Purkinje myocytes—whereas tetrodotoxin-resistant Na+ channels are present in both cell midsection and intercalated disc regions, but their biophysical properties differ depending on location. These authors also showed that a large fraction of tetrodotoxin-resistant NaV1.5 channels in the cell midsection region of ventricular myocytes are inactivated at normal resting potential, leaving most of the burden of excitation to tetrodotoxin-resistant channels in the intercalated disc region. Structurally, the NaV1.5 channels located within the intercalated discs associate with ankyrin-G, synapse-associated protein 97 and junctional proteins (Malhotra et al. 2004; Lowe et al. 2008; Petitprez et al. 2011; Sato et al. 2011). whereas those at the lateral membranes associate with the syntrophin–dystrophin complex (Petitprez et al. 2011).
The role of brain-type tetrodotoxin-sensitive Na+ channels remains unknown in ventricular myocytes. These channels contribute only minimally to the Na+ current under normal conditions but may represent a functional reserve that can be upregulated by exogenous factors (Cerrone and Delmar 2014). It has been suggested that these channels may contribute to excitation–contraction coupling by coordinating and synchronizing the action potential from the sarcolemma into the interior via the T-tubules (Maier et al. 2002; Duclohier 2005). This mechanism is believed to underlie the synchronous Ca2+ release from the SR which results in ventricular contractions. A possible role of tetrodotoxin-sensitive Na+ channels in excitation–contraction coupling has been recently observed by Radwanski et al. (2012) in isolated ventricular myocytes and trabeculae from mice harbouring a point mutation in calsequestrin protein (Casq2-R33Q). Using nanomolar concentrations of tetrodotoxin, these authors demonstrated a modulation of local Na+/Ca2+ signalling and a decrease in spontaneous Ca2+ waves, independent of SR Ca2+ load, direct RyR2 inhibition or reduced excitability. In addition, neuronal Na+ current augmentation with β-pompilidotoxin resulted in a significant increase in both Ca2+ spark frequency and amplitude and reduced SR Ca2+ load.
Brain-type tetrodotoxin-sensitive Na+ channels have been shown to be involved in the electrical activity of the pacemaker cells. In the rabbit, experimental evidence suggests that although I Na is absent in the center of the node, it is present at the periphery (Honjo et al. 1996). Block of I Na by 20 μM tetrodotoxin slows pacemaking at the periphery (Kodama et al. 1997). I Na may be more important in the mouse sinus node: block of both tetrodotoxin-resistant and -sensitive components slows pacemaking by approximately one third and also increases the sinus node conduction time, i.e. the time taken for the action potential to propagate out of the node (Lei et al. 2004). It is possible, therefore, that I Na plays two roles in the node: in pacemaking, especially in the mouse, and in action potential conduction between the node and surrounding atrial myocardium through specialized conduction pathways (Lei et al. 2004; Dobrzynski et al. 2007; Fedorov et al. 2012). Additionally, since pacemaker myocytes appear to lack the T-tubular system, the location of tetrodotoxin-sensitive Na+ channels in these cells remains questionable.
Until recently, with a few exceptions, the general view was that each molecule within the intercalated disc had a single function. The emerging concept, however, is that the different components of intercalated discs do not act alone—rather, they interact and work together as part of a “connexome,” a protein interacting network that regulates excitability, cell–cell adhesion and intercellular coupling in the heart (Cerrone and Delmar 2014). For example, disruption of desmosomal integrity could alter the Na+ current.
Sato et al. (2009) showed that I Na was significantly decreased in ventricular myocytes lacking the desmosomal protein PKP2. In this study, macropatch recordings of PKP2-haploinsufficient myocytes showed that I Na amplitude was reduced only from the region of the intercalated disc, and super-resolution scanning patch clamp revealed that the decreased I Na at the intercalated disc was not consequent to reduced single-channel unitary conductance. Using super-resolution fluorescence microscopy with direct stochastic optical reconstruction, Cerrone et al. (2014) demonstrated that reduced PKP2 abundance correlated with increased distance between the microtubule plus-end tracking protein EB-1 and N-cadherin-rich sites. Based on these results, these authors proposed that PKP2 is part of the molecular complex that captures the microtubule plus-end at the intercalated disc, thus allowing for delivery of its cargo, including NaV1.5 (Shaw et al. 2007; Casini et al. 2010).
Moreover, it has been shown that Na+ channels located within the intercalated discs can coprecipitate with connexins and with N-cadherin (Malhotra et al. 2004). Using transgenic mice overexpressing a mutation in another desmosomal protein, desmoglein-2, Rizzo et al. (2012) demonstrated a prolonged ventricular activation time, decreased conduction velocity, decreased upstroke velocity and decreased I Na amplitude. Similarly, Gomes et al. (2012) reported that patients with arrhythmogenic right ventricular cardiomyopathy harbouring desmoplakin-2 mutations presented regional conduction delay in the right ventricle, inducible ventricular tachycardia associated with mislocalization and reduced intercalated disc expression of Cx43. These authors demonstrated that haploinsufficiency of desmoplakin also led to heterogeneous NaV1.5 distribution. Based on these data, it has been proposed that there is a “triad” of interacting complexes at the intercalated discs formed by molecules originally defined under the function of Na+ channels, gap junctions or desmosomes.
Gap junctions
Gap junction channels connect the cytoplasmic compartments of adjacent cells and allow the intercellular flow of ions. In the heart, gap junction channels are critical for the efficient propagation of the action potential throughout the myocardium (Severs 2000). An individual channel is created by stable, noncovalent interactions of two hemichannels, referred to as connexons. Each connexon (Cx) is composed of six Cx proteins. In the mammalian heart, gap junction channels are primarily composed of three different Cx proteins: Cx43, Cx40 and Cx45. Cx43 is the main constituent of the cardiac gap junction, and in rodents, it is expressed in all atrial and ventricular myocytes. Cx40 is expressed in atrial myocytes, while Cx45 is expressed in the conduction system.
In cardiomyopathies, Cx43 is often downregulated or mislocalized to the lateral membranes instead of being restricted to the intercalated discs (Kostin et al. 2003). Cx43 expression has been reported to be reduced in a variety of animal models of heart failure (Akar et al. 2004; Poelzing and Rosenbaum 2004) and in the human failing heart (Kostin et al. 2003; Ai and Pogwizd 2005; Bruce et al. 2008). A 50 % reduction of Cx43 protein expression and a 40 % reduction of Cx43 mRNA have been reported in human congestive heart failure (Dupont et al. 2001; Poelzing and Rosenbaum 2004).
Some pathological conditions have been linked to the relocalization of Cx43 proteins from the intercalated discs to the lateral membrane. This lateralization is associated with the loss of gap junction coupling between myocytes, resulting in conduction block and reentrant arrhythmias. Using a double-immunostaining of Cx43 with a structural protein, N-cadherin, as a marker of intercalated disks of myocytes, it has been possible to visualize and estimate the transverse-oriented localization of Cx43 by determining its colocalization with N-cadherin (Fig. 4a). Cardiac N-cadherin is an integral part of the intercalated disc junction and is essential for the adherens junctions in myocyte, Cx43 delivery at the cell–cell contact regions and, therefore, the establishment of Cx43 intercellular channels (Shaw et al. 2007; Casini et al. 2010). Conditional deletion of this important adherens junctional protein in the adult mouse heart leads to a complete dissolution of the intercalated disc structure and a significant decrease in Cx43 expression. In that mouse model, N-cadherin deletion results in dilated cardiomyopathy, a slowing-down of conduction and higher conduction anisotropy—and thus spontaneous ventricular tachycardia and arrhythmic death (Li et al. 2005). The intracellular co-assembly of connexins and cadherins is required for gap junction and adherens junction formation, a process that likely underlies the intimate association between electrical gap junction and mechanical adherens junction formation (Wei et al. 2005). It has been demonstrated that some lateralized Cx43 cannot be a part of functional gap junctions (Fig. 4a–c) (Glukhov et al. 2012). These Cx43 are located outside of the intercalated discs on the lateral myocyte membrane or within the myocytes, perhaps representing a trafficking of Cx43 (Smyth et al. 2010).
Conduction remodelling in human end-stage nonischaemic left ventricular cardiomyopathy. a Immunostaining for connexin 43 (Cx43) and N-cadherin (N-cad). Examples (magnification 100×) with split red (Cx43) and green (N-cad) channels. Red arrows Cx43 co-localized with N-cad, white arrows Cx43 not co-localized with N-cad. b Summarized data for transmural expression of Cx43 that is not co-localized with N-cad (relative to total amount of Cx43 at different transmural layers; in percentage of wedge depth) *P < 0.05 for failing hearts (filled circle) vs. nonfailing hearts (open circles). c Average data for Cx43 expression measured by Western blot. *P < 0.05 for failing hearts vs. nonfailing hearts. GAPDH Glyceraldehyde 3-phosphate dehydrogenase, Epi subepicardium, Endo subendocardium. d Western blot analysis. For Epi and Endo expression of Cx43, different phosphorylated bands for the Cx43 protein were observed, namely, the relatively high-molecular-weight and high phosphorylated isoforms (P1, P2) and the relatively low-molecular-weight and dephosphorylated isoform (P0). e Redistribution of phosphorylated isoforms of Cx43 during HF in the Epi and Endo. **P < 0.001 for failing hearts (filled column) vs. nonfailing hearts (open column). f Optical mapping of the epicardial surface of the transplanted human heart. Preparation of the epicardial optical mapping of the isolated, left ventricle free wall (marked by dotted line on the top panel) was conducted by using high-resolution optical mapping with voltage-sensitive fluorescent dye. RV Right ventricle, RA right atrium. Bottom panel Optical field of view (OFV 35 × 35 mm) is denoted by square. g Colour isochronal map represents epicardial activation of isolated left ventricle free wall preparation shown in panel f. Activation pattern is shown for fast (S1S1 = 280 ms) pacing. Two optical action potential (OAP) recordings (circled 1 and 2) collected from the labelled areas are shown below the activation map. The gradual shortening of pacing interval depressed conduction velocity along the transverse direction and resulted in increased conduction anisotropy without any conduction abnormalities. h Pacing-induced discordant conduction alternans and occurrence of the transverse conduction block in a failing human heart. Two OAP recordings (circled 1 and 2) collected from the labelled areas are shown below the activation map. Epicardial optical mapping revealed a considerable conduction delay in the transversal direction. Progressive shortening of the pacing cycle length from 1,000 to 350 ms (shown on top panels) led to occurrence of beat-to-beat discordant conduction alternans with a 2:1 conduction block along the transverse direction. OAPs corresponding to the reconstructed activation and action potential duration (APD) distribution maps are marked by pink dotted rectangles. Adapted from Glukhov et al. (2012)
Cx43 is a phosphoprotein, with multiple phosphorylation sites for both serine/threonine, as well as for tyrosine phosphorylation (Lampe and Lau 2004). It has been shown that Cx43 is differentially phosphorylated at a dozen or more serine residues throughout its life cycle (Lampe and Lau 2004). However, the regulation of Cx43 by phosphorylation is a profoundly complex process, with some sites being positive regulators, leading to increased conductance, whereas others are negative regulators, leading to closure of the channel. Cx43 phosphorylation regulates the properties of Cx43, including its assembly, trafficking, turnover and electrical and metabolic coupling (van Veen et al. 2006). Factors and conditions altering the phosphorylation pattern of Cx43 can also alter its properties and, by extension, affect heart function. Re-distribution of phosphorylated and de-phosphorylated Cx43 isoforms has been observed in both humans and animal models of heart failure, with the higher molecular-weight and higher phosphorylated (P1 and P2) Cx43 isoforms being downregulated, and the lower molecular-weight and dephosphorylated (P0) isoform being upregulated (Fig. 4d, e) (Glukhov et al. 2012).
Cx43 lateralization around cardiac myocytes has been reported in human dilated (Kitamura et al. 2002) and hypertrophic (Dupont et al. 2001) cardiomyopathies, both of which in association with fibrosis. Lateralization of Cx43 is believed to be associated with non-functional and/or de-phosphorylated states of Cx43. It remains debatable whether these lateral structures represent functional gap junctions or gap junction subunits that have been disassembled by lateralization or internalization. Whatever the case, the consequence of such an alteration could be a profound change in uniform anisotropy with the potential to give rise to arrhythmogenicity (Fig. 4f–h) (Glukhov et al. 2012). At this point, it is important to note the study by Wiegerinck et al. (2009) on the explanted hearts of patients with end-stage of heart failure. Using rotigaptide, a compound belonging to a group of antiarrhythmic substances derived from AAP10 (Muller et al. 1997), these authors obtained an increase in ventricular conduction on the epicardium and a decrease in the percentage of sites with conduction slowing throughout the mapped area. The mechanism by which rotigaptide improves gap junctional conductance is probably related to phosphorylation of Cx43 at Ser297 and at the protein kinase C (PKC)-sensitive site Ser368 (Dhein et al. 2003). Based on these results, Wiegerinck et al. (2009) suggested that treatment with rotigaptide may cause phosphorylation of the dephosphorylated Cx43 and therefore increase conduction in the hearts of patients with heart failure. Despite these promising results, further studies must be done to directly determine to what extent these changes in distribution and phosphorylation contribute to altered conduction and arrhythmogenesis.
Recent studies have demonstrated that loss of Cx43 expression leads to reduced I Na amplitude in ventricular (Danik et al. 2008; Jansen et al. 2012) and atrial myocytes (Desplantez et al. 2012). Moreover, the data suggest a fundamental, gap junction-independent role for Cx43 in cardiac electrophysiology, where this protein is also relevant for the K+ channels (Danik et al. 2008).
Potassium channels
In contrast to the Ca2+ and Na+ channels, the spatial localization of which in cardiac myocytes is quite defined, microdomain-specific distribution of K+ channels is less studied. All data on the targeting of K+ channels to specific structural proteins and membrane microdomains have been obtained utilizing a variety of biochemical and molecular imaging techniques, with almost no evidence for the functionality of these channels based on their cellular location. As a result, the findings reported by different studies remain controversial, probably because of differences in antibody specificity, accessibility of epitopes with different fixation procedures and the potentially dynamic nature of K+ channel localization (reviewed in Balijepalli and Kamp 2008). Here, we highlight the evidence available to date on the identification of several major potassium channels responsible for I to, I K, IK1 and I K,ATP repolarizing ion currents and their localization.
I to
Rapidly activating and inactivating cardiac “transient” outward K+ currents, I to, are present in most mammalian cardiac myocytes and make a major contribution to the early phase of action potential repolarization and to plateau potentials (reviewed in Nerbonne and Kass 2005). It is generally accepted that pore-forming (α) subunits of the KV4 subfamily, KV4.2 (KCND2) and KV4.3 (KCND3), encode I to,f and that KV1.4 (KCNA4) encodes I to,s channels. Komukai et al. (2002) demonstrated that the current is distributed uniformly between the T-tubules and the surface membrane. This distribution is consistent with earlier results from immunolabelling experiments demonstrating KV4.2 expression in both T-tubules and intercalated discs (Barry et al. 1995; Takeuchi et al. 2000) and the even distribution of KV1.4 over the peripheral sarcolemma and the T-tubules (but not in axial tubules), as well as the intercalated disk (O’Connell et al. 2008).
I K
The delayed rectifier K+ current, I K, is responsible for the late repolarization phase of the action potential and regulates action potential duration in many species. Three components of this voltage-dependent current have been described after a kinetic analysis: the ultra-rapidly activating delayed rectifier current I Kur, the rapidly activating I Kr and the slowly activating I Ks delayed rectifier currents.
The KV1.5 K+ channel is expressed predominantly in the atrial myocardium and is responsible for the ultrarapid component of the delayed rectifier K+ current, I Kur. Initially targeted to caveolae structures (Folco et al. 2004; Shibata et al. 2006), KV1.5 channels have been later targeted mainly to intercalated disc regions independent of caveolae as well as some cell surface localization, likely within the lipid rafts (Mays et al. 1995; Eldstrom et al. 2006). However, spatial localization of KV1.5 channels remains open to question.
The voltage-gated KV11.1 (hERG) channel is expressed in all types of cardiac myocytes throughout the heart and is responsible for the rapid component of the delayed rectifier current, I Kr. Balijepalli et al. (2007), using discontinuous sucrose density gradients, showed in canine ventricular tissue and HEK 293 cells that KV11.1 channels are present in cholesterol- and sphingolipid-enriched membrane fractions, but that they are not associated with Cav3 based on a lack of co-immunoprecipitation, suggesting KV11.1 localization in lipid rafts. However, a later study by Guo et al. (2012) revealed that Cav3, hERG and ubiquitin-ligase Nedd4-2 interact with each other and form a functional complex in rat and rabbit ventricular tissues and HEK 293 cells expressing both hERG and Cav3. Further studies are thus needed to support localization of KV11.1 channels to lipid raft/caveolae structures.
The KCNQ1 gene encodes the pore-forming subunit of the K+ channel KV7.1 or KVLQT1, which is responsible for the slow component of the delayed rectifier current, I Ks. These channels are found in caveolar membrane fractions (Balijepalli et al. 2007). Nakamura et al. suggested that the presence of KV7.1 channels in caveolae plays an important role in stimulation of I Ks by progesterone, through PI3K/Akt-dependent activation of eNOS and subsequent S-nitrosylation of the channel.
It should be noted that detubulation (depletion of T-tubules) of rat ventricular myocytes does not affect whole-cell I K current (Komukai et al. 2002), suggesting a predominantly extradyadic location of functional KV1.5, KV11.1, and KV7.1 K+ channels.
I K1
Inward rectifier K+ channels are encoded by the Kir2.x family of genes, and Kir2.1 is responsible for I K1 which maintains the resting membrane potential and contributes to terminal repolarization. Immunolabelling experiments have produced controversial results showing the expression of Kir2.1 subunits in both T-tubules and the surface membrane (Clark et al. 2001; Leonoudakis et al. 2001; O’Connell et al. 2008). At the same time, the detubulation procedure was observed not to alter I K1 density (Komukai et al. 2002), suggesting that functional I K1 channels are predominantly located outside of the T-tubules. Although Vaidyanathan et al. (2013) found that Cav3 mutations associated with long QT 9 syndrome (LQT9) resulted an approximately 30–60 % reduction in I K1 density, Markandeya et al. (2013) observed no changes in I K1 current density in Cav3-/- mouse ventricular myocytes. These results suggest that the extra-caveolae locations of these channels are likely to be in noncaveolar lipid rafts. Asimaki et al. (2014) recently reported that a cardiac myocyte–specific mutation in the gene encoding plakoglobin, namely, the intercalated disc-associated structural protein described above, resulted in a 80 % decrease in I K1 current density, which may also indicate a intercalated disc-targeted population of I K1 channels (Chan et al. 2011).
K ATP
In the adult ventricular myocyte, the ATP-sensitive K+ channels, KATP, consist of Kir6.2 and the sulfonylurea receptor 2 (SUR2) subunits. I K,ATP responds to the metabolic state of the cell and plays a role in shortening the action potential during ischaemia (Zingman et al. 1985). The data currently available on the localization of KATP channels in the cardiac sarcolemma are controversial. Initially, KATP was localized to Cav3-enriched microdomains (Garg et al. 2009); however, more recent reports demonstrate two distinct populations of KATP channels, with one associated with ankyrin-B localized to the lateral sides and T-tubules of cardiac myocytes (Li et al. 2010) and the others co-localized with ankyrin-G at the intercalated discs (Hong et al. 2012a). At the same time, disrupting caveolae by either methyl-β-cyclodextrin or Cav3 siRNA did not alter the amplitude of pinacidil-evoked KATP currents (Garg et al. 2009) which may additionally indicate that KATP channels are located outside of the caveolae microdomains. It has been recently reported that atrial myocytes specifically express the SUR1 subunit of KATP channels (Glukhov et al. 2010); this may alter the localization of KATP channels in atrial myocytes which are known to possess a high level of caveolae structures and lack a regular T-tubule network.
Conclusions
In cardiac myocytes, a variety of ion channels and regulatory receptors are spatially compartmentalized to multiple distinct subcellular microdomains, and this compartmentalization may impact their function and regulation. Importantly, many of these proteins form an interacting network where they work together as a part of a macro-molecular signalling complex. A number of important protein-interacting networks have been identified in cardiac myocytes that associate with unique macromolecular signalling complexes and scaffolding proteins, which in turn enables spatiotemporal modulation of cellular electrophysiology and contraction. These include complexes located in T-tubules, lipid rafts/caveolae, costameres and intercalated discs where they are associated with different structural proteins. Such organization allows the specificity, reliability and accuracy of the autonomic modulation of excitation–contraction processes by a variety of neurohormonal pathways, either via direct interaction or by second messengers through different G-protein-coupled receptors. In this respect, microdomain-specific localization of certain G-protein-coupled receptors as well as subcellular compartmentation of a variety of second messengers and kinases should also be acknowledged. However, discussion of the latter is beyond the scope of this current review and has been reviewed elsewhere (Insel et al. 2005; Zhang and Mende 2011; Harvey and Calaghan 2012; Stangherlin and Zaccolo 2012).
The spatial compartmentation of macro-molecular signalling complexes is traditionally assessed by a variety of immune- and biochemical techniques. The resulting images are likely to represent mixed populations of both functional and silent channels and receptors, as well as those in the reserve pools, and thus lack information on the functionality of these proteins. The emerging imaging modalities, such as super-resolution scanning patch clamp and Förster resonance energy transfer (FRET)-based sensors, seem to be promising to explore microdomain-specific functionality of different ion channels and provide direct evidence on protein–protein interaction.
In conclusion, all of the above considerations demonstrate the importance and the complexity of the microdomain-specific modulation and remodelling of ion channel biophysical properties. This extends beyond the classical concept of electrical remodelling in cardiac disease according to which dysfunction can be explained by straightforward increases or decreases in protein expression alone. Thus, a better understanding of the various subcellular macro-molecular signalling complexes may enable new therapeutic approaches for predicting and ameliorating the risk of sudden cardiac death and malignant arrhythmias in patients with cardiac diseases.
References
Ai X, Pogwizd SM (2005) Connexin 43 downregulation and dephosphorylation in nonischemic heart failure is associated with enhanced colocalized protein phosphatase type 2A. Circ Res 96(1):54–63
Aimond F, Alvarez JL, Rauzier JM, Lorente P, Vassort G (1999) Ionic basis of ventricular arrhythmias in remodeled rat heart during long-term myocardial infarction. Cardiovasc Res 42(2):402–415
Akar FG, Spragg DD, Tunin RS, Kass DA, Tomaselli GF (2004) Mechanisms underlying conduction slowing and arrhythmogenesis in nonischemic dilated cardiomyopathy. Circ Res 95(7):717–725
Asimaki A, Kapoor S, Plovie E et al (2014) Identification of a new modulator of the intercalated disc in a zebrafish model of arrhythmogenic cardiomyopathy. Sci Transl Med 6(240):240ra274
Ayettey AS, Navaratnam V (1978) The T-tubule system in the specialized and general myocardium of the rat. J Anat 127(Pt 1):125–140
Balijepalli RC, Kamp TJ (2008) Caveolae, ion channels and cardiac arrhythmias. Prog Biophys Mol Biol 98(2–3):149–160
Balijepalli RC, Foell JD, Hall DD, Hell JW, Kamp TJ (2006) Localization of cardiac L-type Ca2+ channels to a caveolar macromolecular signaling complex is required for beta(2)-adrenergic regulation. Proc Natl Acad Sci USA 103(19):7500–7505
Balijepalli RC, Delisle BP, Balijepalli SY et al (2007) Kv11.1 (ERG1) K+ channels localize in cholesterol and sphingolipid enriched membranes and are modulated by membrane cholesterol. Channels (Austin) 1(4):263–272
Barouch LA, Harrison RW, Skaf MW et al (2002) Nitric oxide regulates the heart by spatial confinement of nitric oxide synthase isoforms. Nature 416(6878):337–339
Barry DM, Trimmer JS, Merlie JP, Nerbonne JM (1995) Differential expression of voltage-gated K+ channel subunits in adult rat heart. Relation to functional K+ channels? Circ Res 77(2):361–369
Baruscotti M, Westenbroek R, Catterall WA, DiFrancesco D, Robinson RB (1997) The newborn rabbit sino-atrial node expresses a neuronal type I-like Na+ channel. J Physiol 498(Pt 3):641–648
Bassani JW, Bassani RA, Bers DM (1994) Relaxation in rabbit and rat cardiac cells: species-dependent differences in cellular mechanisms. J Physiol 476(2):279–293
Benitah JP, Kerfant BG, Vassort G, Richard S, Gomez AM (2002) Altered communication between L-type calcium channels and ryanodine receptors in heart failure. Front Biosci 7:e263–e275
Benitah JP, Alvarez JL, Gomez AM (2010) L-type Ca2+ current in ventricular cardiomyocytes. J Mol Cell Cardiol 48(1):26–36
Best JM, Kamp TJ (2012) Different subcellular populations of L-type Ca2+ channels exhibit unique regulation and functional roles in cardiomyocytes. J Mol Cell Cardiol 52(2):376–387
Bhargava A, O’Hara T, Sikkel MB, Lyon AR, Trayanova NA, Gorelik J (2012) Nanoscale movement of L-type calcium channels in the cardiomyocyte membrane can contribute to arrhythmia during heart failure. Circulation 126, A11953
Bhargava A, Lin X, Novak P et al (2013) Super-resolution scanning patch clamp reveals clustering of functional ion channels in adult ventricular myocyte. Circ Res 112(8):1112–1120
Bichet D, Cornet V, Geib S et al (2000) The I-II loop of the Ca2+ channel alpha1 subunit contains an endoplasmic reticulum retention signal antagonized by the beta subunit. Neuron 25(1):177–190
Birnbaumer L, Qin N, Olcese R et al (1998) Structures and functions of calcium channel beta subunits. J Bioenerg Biomembr 30(4):357–375
Bito V, Heinzel FR, Biesmans L, Antoons G, Sipido KR (2008) Crosstalk between L-type Ca2+ channels and the sarcoplasmic reticulum: alterations during cardiac remodelling. Cardiovasc Res 77(2):315–324
Bosch RF, Zeng X, Grammer JB, Popovic K, Mewis C, Kuhlkamp V (1999) Ionic mechanisms of electrical remodeling in human atrial fibrillation. Cardiovasc Res 44(1):121–131
Boulware MI, Kordasiewicz H, Mermelstein PG (2007) Caveolin proteins are essential for distinct effects of membrane estrogen receptors in neurons. J Neurosci 27(37):9941–9950
Bovo E, de Tombe PP, Zima AV (2014) The role of dyadic organization in regulation of sarcoplasmic reticulum Ca2+ handling during rest in rabbit ventricular myocytes. Biophys J 106(9):1902–1909
Brette F, Orchard C (2003) T-tubule function in mammalian cardiac myocytes. Circ Res 92(11):1182–1192
Brette F, Salle L, Orchard CH (2004) Differential modulation of L-type Ca2+ current by SR Ca2+ release at the T-tubules and surface membrane of rat ventricular myocytes. Circ Res 95(1):e1–e7
Brette F, Despa S, Bers DM, Orchard CH (2005) Spatiotemporal characteristics of SR Ca2+ uptake and release in detubulated rat ventricular myocytes. J Mol Cell Cardiol 39(5):804–812
Brette F, Salle L, Orchard CH (2006) Quantification of calcium entry at the T-tubules and surface membrane in rat ventricular myocytes. Biophys J 90(1):381–389
Bruce AF, Rothery S, Dupont E, Severs NJ (2008) Gap junction remodelling in human heart failure is associated with increased interaction of connexin43 with ZO-1. Cardiovasc Res 77(4):757–765
Bush EW, Hood DB, Papst PJ et al (2006) Canonical transient receptor potential channels promote cardiomyocyte hypertrophy through activation of calcineurin signaling. J Biol Chem 281(44):33487–33496
Butler MH, David C, Ochoa GC et al (1997) Amphiphysin II (SH3P9; BIN1), a member of the amphiphysin/Rvs family, is concentrated in the cortical cytomatrix of axon initial segments and nodes of ranvier in brain and around T tubules in skeletal muscle. J Cell Biol 137(6):1355–1367
Cannell MB, Kong CH (2012) Local control in cardiac E-C coupling. J Mol Cell Cardiol 52(2):298–303
Casini S, Tan HL, Demirayak I et al (2010) Tubulin polymerization modifies cardiac sodium channel expression and gating. Cardiovasc Res 85(4):691–700
Catterall WA (1992) Cellular and molecular biology of voltage-gated sodium channels. Physiol Rev 72[4 Suppl]:S15–S48
Catterall WA (2000) Structure and regulation of voltage-gated Ca2+ channels. Annu Rev Cell Dev Biol 16:521–555
Cavalli A, Eghbali M, Minosyan TY, Stefani E, Philipson KD (2007) Localization of sarcolemmal proteins to lipid rafts in the myocardium. Cell Calcium 42(3):313–322
Cerrone M, Delmar M (2014) Desmosomes and the sodium channel complex: implications for arrhythmogenic cardiomyopathy and Brugada syndrome. Trends Cardiovasc Med 24(5):184–190
Cerrone M, Lin X, Zhang M et al (2014) Missense mutations in plakophilin-2 cause sodium current deficit and associate with a brugada syndrome phenotype. Circulation 129(10):1092–1103
Chan FC, Cheng CP, Wu KH et al (2011) Intercalated disc-associated protein, mXin-alpha, influences surface expression of Ito currents in ventricular myocytes. Front Biosci (Elite Ed) 3:1425–1442
Chase A, Orchard CH (2011) Ca efflux via the sarcolemmal Ca ATPase occurs only in the T-tubules of rat ventricular myocytes. J Mol Cell Cardiol 50(1):187–193
Chen-Izu Y, Xiao RP, Izu LT et al (2000) Gi-dependent localization of beta(2)-adrenergic receptor signaling to L-type Ca2+ channels. Biophys J 79(5):2547–2556
Chiang CS, Huang CH, Chieng H et al (2009) The CaV3.2 T-type Ca2+ channel is required for pressure overload-induced cardiac hypertrophy in mice. Circ Res 104(4):522–530
Chien AJ, Zhao X, Shirokov RE et al (1995) Roles of a membrane-localized beta subunit in the formation and targeting of functional L-type Ca2+ channels. J Biol Chem 270(50):30036–30044
Chu PJ, Larsen JK, Chen CC, Best PM (2004) Distribution and relative expression levels of calcium channel beta subunits within the chambers of the rat heart. J Mol Cell Cardiol 36(3):423–434
Clark RB, Tremblay A, Melnyk P, Allen BG, Giles WR, Fiset C (2001) T-tubule localization of the inward-rectifier K(+) channel in mouse ventricular myocytes: a role in K(+) accumulation. J Physiol 537(Pt 3):979–992
Cohen SA (1996) Immunocytochemical localization of rH1 sodium channel in adult rat heart atria and ventricle. Presence in terminal intercalated disks. Circulation 94(12):3083–3086
Cohen AW, Hnasko R, Schubert W, Lisanti MP (2004) Role of caveolae and caveolins in health and disease. Physiol Rev 84(4):1341–1379
Cohen RM, Foell JD, Balijepalli RC, Shah V, Hell JW, Kamp TJ (2005) Unique modulation of L-type Ca2+ channels by short auxiliary beta1d subunit present in cardiac muscle. Am J Physiol Heart Circ Physiol 288(5):H2363–H2374
Collin T, Wang JJ, Nargeot J, Schwartz A (1993) Molecular cloning of three isoforms of the L-type voltage-dependent calcium channel beta subunit from normal human heart. Circ Res 72(6):1337–1344
Cordeiro JM, Spitzer KW, Giles WR, Ershler PE, Cannell MB, Bridge JH (2001) Location of the initiation site of calcium transients and sparks in rabbit heart Purkinje cells. J Physiol 531(Pt 2):301–314
Danik SB, Rosner G, Lader J, Gutstein DE, Fishman GI, Morley GE (2008) Electrical remodeling contributes to complex tachyarrhythmias in connexin43-deficient mouse hearts. FASEB J 22(4):1204–1212
Davare MA, Avdonin V, Hall DD et al (2001) A beta2 adrenergic receptor signaling complex assembled with the Ca2+ channel Cav1.2. Science 293(5527):98–101
Desplantez T, McCain ML, Beauchamp P et al (2012) Connexin43 ablation in foetal atrial myocytes decreases electrical coupling, partner connexins, and sodium current. Cardiovasc Res 94(1):58–65
Dhar Malhotra J, Chen C, Rivolta I et al (2001) Characterization of sodium channel alpha- and beta-subunits in rat and mouse cardiac myocytes. Circulation 103(9):1303–1310
Dhein S, Larsen BD, Petersen JS, Mohr FW (2003) Effects of the new antiarrhythmic peptide ZP123 on epicardial activation and repolarization pattern. Cell Commun Adhes 10(4–6):371–378
Dibb KM, Clarke JD, Horn MA et al (2009) Characterization of an extensive transverse tubular network in sheep atrial myocytes and its depletion in heart failure. Circ Heart Fail 2(5):482–489
Dobrev D, Teos LY, Lederer WJ (2009) Unique atrial myocyte Ca2+ signaling. J Mol Cell Cardiol 46(4):448–451
Dobrzynski H, Boyett MR, Anderson RH (2007) New insights into pacemaker activity: promoting understanding of sick sinus syndrome. Circulation 115(14):1921–1932
Duclohier H (2005) Neuronal sodium channels in ventricular heart cells are localized near T-tubules openings. Biochem Biophys Res Commun 334(4):1135–1140
Dupont E, Matsushita T, Kaba RA et al (2001) Altered connexin expression in human congestive heart failure. J Mol Cell Cardiol 33(2):359–371
Eldstrom J, Van Wagoner DR, Moore ED, Fedida D (2006) Localization of Kv1.5 channels in rat and canine myocyte sarcolemma. FEBS Lett 580(26):6039–6046
Fareh S, Benardeau A, Thibault B, Nattel S (1999) The T-type Ca(2+) channel blocker mibefradil prevents the development of a substrate for atrial fibrillation by tachycardia-induced atrial remodeling in dogs. Circulation 100(21):2191–2197
Fawcett DW, McNutt NS (1969) The ultrastructure of the cat myocardium. I. Ventricular papillary muscle. J Cell Biol 42(1):1–45
Fedorov VV, Glukhov AV, Chang R (2012) Conduction barriers and pathways of the sino-atrial pacemaker complex: their role in normal rhythm and atrial arrhythmias. Am J Physiol Heart Circ Physiol 302(9):H1773–H1783
Feron O, Balligand JL (2006) Caveolins and the regulation of endothelial nitric oxide synthase in the heart. Cardiovasc Res 69(4):788–797
Foell JD, Balijepalli RC, Delisle BP et al (2004) Molecular heterogeneity of calcium channel beta-subunits in canine and human heart: evidence for differential subcellular localization. Physiol Genomics 17(2):183–200
Folco EJ, Liu GX, Koren G (2004) Caveolin-3 and SAP97 form a scaffolding protein complex that regulates the voltage-gated potassium channel Kv1.5. Am J Physiol Heart Circ Physiol 287(2):H681–H690
Fozzard HA, Hanck DA (1996) Structure and function of voltage-dependent sodium channels: comparison of brain II and cardiac isoforms. Physiol Rev 76(3):887–926
Galbiati F, Engelman JA, Volonte D et al (2001) Caveolin-3 null mice show a loss of caveolae, changes in the microdomain distribution of the dystrophin-glycoprotein complex, and t-tubule abnormalities. J Biol Chem 276(24):21425–21433
Gao T, Puri TS, Gerhardstein BL, Chien AJ, Green RD, Hosey MM (1997) Identification and subcellular localization of the subunits of L-type calcium channels and adenylyl cyclase in cardiac myocytes. J Biol Chem 272(31):19401–19407
Garg V, Jiao J, Hu K (2009) Regulation of ATP-sensitive K+ channels by caveolin-enriched microdomains in cardiac myocytes. Cardiovasc Res 82(1):51–58
Gerhardstein BL, Puri TS, Chien AJ, Hosey MM (1999) Identification of the sites phosphorylated by cyclic AMP-dependent protein kinase on the beta 2 subunit of L-type voltage-dependent calcium channels. Biochemistry 38(32):10361–10370
Glukhov AV, Flagg TP, Fedorov VV, Efimov IR, Nichols CG (2010) Differential K(ATP) channel pharmacology in intact mouse heart. J Mol Cell Cardiol 48(1):152–160
Glukhov AV, Fedorov VV, Kalish PW et al (2012) Conduction remodeling in human end-stage nonischemic left ventricular cardiomyopathy. Circulation 125(15):1835–1847
Glukhov AV, Balycheva M, Schobesberger S et al (2013) Distinct distribution of functional calcium channels revealed by super-resolution scanning patch-clamp in adult rat atrial cardiomyocytes. Circulation 128: A10467
Glukhov AV, Balycheva M, Bhogal N et al (2014) Caveolae specific location of L-type calcium channels and their role in atrial calcium cycling. Circulation 130, A15399
Goebel J, Logan B, Forrest K, Mieczkowski A, Roszman TL, Wills-Karp M (2005) Atorvastatin affects interleukin-2 signaling by altering the lipid raft enrichment of the interleukin-2 receptor beta chain. J Investig Med 53(6):322–328
Goel M, Zuo CD, Sinkins WG, Schilling WP (2007) TRPC3 channels colocalize with Na+/Ca2+ exchanger and Na+ pump in axial component of transverse-axial tubular system of rat ventricle. Am J Physiol Heart Circ Physiol 292(2):H874–H883
Gomes J, Finlay M, Ahmed AK et al (2012) Electrophysiological abnormalities precede overt structural changes in arrhythmogenic right ventricular cardiomyopathy due to mutations in desmoplakin-A combined murine and human study. Eur Heart J 33(15):1942–1953
Grabner M, Dirksen RT, Beam KG (1998) Tagging with green fluorescent protein reveals a distinct subcellular distribution of L-type and non-L-type Ca2+ channels expressed in dysgenic myotubes. Proc Natl Acad Sci USA 95(4):1903–1908
Gratton JP, Bernatchez P, Sessa WC (2004) Caveolae and caveolins in the cardiovascular system. Circ Res 94(11):1408–1417
Gu Y, Gorelik J, Spohr HA et al (2002) High-resolution scanning patch-clamp: new insights into cell function. FASEB J 16(7):748–750
Guo J, Wang T, Li X et al (2012) Cell surface expression of human ether-a-go-go-related gene (hERG) channels is regulated by caveolin-3 protein via the ubiquitin ligase Nedd4-2. J Biol Chem 287(40):33132–33141
Guo A, Zhang X, Iyer VR et al (2014) Overexpression of junctophilin-2 does not enhance baseline function but attenuates heart failure development after cardiac stress. Proc Natl Acad Sci USA 111(33):12240–12245
Haase H, Pfitzmaier B, McEnery MW, Morano I (2000) Expression of Ca(2+) channel subunits during cardiac ontogeny in mice and rats: identification of fetal alpha(1C) and beta subunit isoforms. J Cell Biochem 76(4):695–703
Hackenbrock CR, Chazotte B, Gupte SS (1986) The random collision model and a critical assessment of diffusion and collision in mitochondrial electron transport. J Bioenerg Biomembr 18(5):331–368
Haddock PS, Coetzee WA, Cho E et al (1999) Subcellular [Ca2+]i gradients during excitation-contraction coupling in newborn rabbit ventricular myocytes. Circ Res 85(5):415–427
Hansma PK, Drake B, Marti O, Gould SA, Prater CB (1989) The scanning ion-conductance microscope. Science 243(4891):641–643
Harvey RD, Calaghan SC (2012) Caveolae create local signalling domains through their distinct protein content, lipid profile and morphology. J Mol Cell Cardiol 52(2):366–375
Haufe V, Cordeiro JM, Zimmer T et al (2005) Contribution of neuronal sodium channels to the cardiac fast sodium current INa is greater in dog heart Purkinje fibers than in ventricles. Cardiovasc Res 65(1):117–127
Hayashi T, Arimura T, Itoh-Satoh M et al (2004) Tcap gene mutations in hypertrophic cardiomyopathy and dilated cardiomyopathy. J Am Coll Cardiol 44(11):2192–2201
Heinzel FR, Bito V, Biesmans L et al (2008) Remodeling of T-tubules and reduced synchrony of Ca2+ release in myocytes from chronically ischemic myocardium. Circ Res 102(3):338–346
Hell JW, Yokoyama CT, Wong ST, Warner C, Snutch TP, Catterall WA (1993) Differential phosphorylation of two size forms of the neuronal class C L-type calcium channel alpha 1 subunit. J Biol Chem 268(26):19451–19457
Hell JW, Yokoyama CT, Breeze LJ, Chavkin C, Catterall WA (1995) Phosphorylation of presynaptic and postsynaptic calcium channels by cAMP-dependent protein kinase in hippocampal neurons. EMBO J 14(13):3036–3044
Herman DS, Lam L, Taylor MR et al (2012) Truncations of titin causing dilated cardiomyopathy. N Engl J Med 366(7):619–628
Hermosilla T, Moreno C, Itfinca M et al (2011) L-type calcium channel beta subunit modulates angiotensin II responses in cardiomyocytes. Channels (Austin) 5(3):280–286
Hong TT, Smyth JW, Gao D et al (2010) BIN1 localizes the L-type calcium channel to cardiac T-tubules. PLoS Biol 8(2):e1000312
Hong M, Bao L, Kefaloyianni E et al (2012a) Heterogeneity of ATP-sensitive K+ channels in cardiac myocytes: enrichment at the intercalated disk. J Biol Chem 287(49):41258–41267
Hong TT, Smyth JW, Chu KY et al (2012b) BIN1 is reduced and Cav1.2 trafficking is impaired in human failing cardiomyocytes. Heart Rhythm 9(5):812–820
Hong T, Yang H, Zhang SS et al (2014) Cardiac BIN1 folds T-tubule membrane, controlling ion flux and limiting arrhythmia. Nat Med 20(6):624–632
Honjo H, Boyett MR, Kodama I, Toyama J (1996) Correlation between electrical activity and the size of rabbit sino-atrial node cells. J Physiol 496(Pt 3):795–808
Huang B, Qin D, Deng L, Boutjdir M, El-Sherif N (2000) Reexpression of T-type Ca2+ channel gene and current in post-infarction remodeled rat left ventricle. Cardiovasc Res 46(3):442–449
Hullin R, Singer-Lahat D, Freichel M et al (1992) Calcium channel beta subunit heterogeneity: functional expression of cloned cDNA from heart, aorta and brain. EMBO J 11(3):885–890
Hullin R, Asmus F, Ludwig A, Hersel J, Boekstegers P (1999) Subunit expression of the cardiac L-type calcium channel is differentially regulated in diastolic heart failure of the cardiac allograft. Circulation 100(2):155–163
Hullin R, Khan IF, Wirtz S et al (2003) Cardiac L-type calcium channel beta-subunits expressed in human heart have differential effects on single channel characteristics. J Biol Chem 278(24):21623–21630
Hullin R, Matthes J, von Vietinghoff S et al (2007) Increased expression of the auxiliary beta(2)-subunit of ventricular L-type Ca(2)+ channels leads to single-channel activity characteristic of heart failure. PLoS One 2(3):e292
Huser J, Lipsius SL, Blatter LA (1996) Calcium gradients during excitation-contraction coupling in cat atrial myocytes. J Physiol 494(Pt 3):641–651
Ibrahim M, Gorelik J, Yacoub MH, Terracciano CM (2011) The structure and function of cardiac t-tubules in health and disease. Proc Biol Sci 278(1719):2714–2723
Ibrahim M, Siedlecka U, Buyandelger B et al (2013) A critical role for Telethonin in regulating t-tubule structure and function in the mammalian heart. Hum Mol Genet 22(2):372–383
Insel PA, Head BP, Ostrom RS et al (2005) Caveolae and lipid rafts: G protein-coupled receptor signaling microdomains in cardiac myocytes. Ann N Y Acad Sci 1047:166–172
Isom LL, De Jongh KS, Catterall WA (1994) Auxiliary subunits of voltage-gated ion channels. Neuron 12(6):1183–1194
Jaleel N, Nakayama H, Chen X et al (2008) Ca2+ influx through T- and L-type Ca2+ channels have different effects on myocyte contractility and induce unique cardiac phenotypes. Circ Res 103(10):1109–1119
Jansen JA, Noorman M, Musa H et al (2012) Reduced heterogeneous expression of Cx43 results in decreased Nav1.5 expression and reduced sodium current that accounts for arrhythmia vulnerability in conditional Cx43 knockout mice. Heart Rhythm 9(4):600–607
Jiang Y, Huang H, Liu P et al (2014) Expression and localization of TRPC proteins in rat ventricular myocytes at various developmental stages. Cell Tissue Res 355(1):201–212
Kaftan E, Marks AR, Ehrlich BE (1996) Effects of rapamycin on ryanodine receptor/Ca(2+)-release channels from cardiac muscle. Circ Res 78(6):990–997
Kamada Y, Yamada Y, Yamakage M et al (2004) Single-channel activity of L-type Ca2+ channels reconstituted with the beta2c subunit cloned from the rat heart. Eur J Pharmacol 487(1–3):37–45
Kamp TJ, Hell JW (2000) Regulation of cardiac L-type calcium channels by protein kinase A and protein kinase C. Circ Res 87(12):1095–1102
Kamp TJ, Perez-Garcia MT, Marban E (1996) Enhancement of ionic current and charge movement by coexpression of calcium channel beta 1A subunit with alpha 1C subunit in a human embryonic kidney cell line. J Physiol 492(Pt 1):89–96
Kinoshita H, Kuwahara K, Takano M et al (2009) T-type Ca2+ channel blockade prevents sudden death in mice with heart failure. Circulation 120(9):743–752
Kirk MM, Izu LT, Chen-Izu Y et al (2003) Role of the transverse-axial tubule system in generating calcium sparks and calcium transients in rat atrial myocytes. J Physiol 547(Pt 2):441–451
Kitamura H, Ohnishi Y, Yoshida A et al (2002) Heterogeneous loss of connexin43 protein in nonischemic dilated cardiomyopathy with ventricular tachycardia. J Cardiovasc Electrophysiol 13(9):865–870
Klein G, Schroder F, Vogler D et al (2003) Increased open probability of single cardiac L-type calcium channels in patients with chronic atrial fibrillation. role of phosphatase 2A. Cardiovasc Res 59(1):37–45
Knoll R, Hoshijima M, Hoffman HM et al (2002) The cardiac mechanical stretch sensor machinery involves a Z disc complex that is defective in a subset of human dilated cardiomyopathy. Cell 111(7):943–955
Kodama I, Nikmaram MR, Boyett MR, Suzuki R, Honjo H, Owen JM (1997) Regional differences in the role of the Ca2+ and Na+ currents in pacemaker activity in the sinoatrial node. Am J Physiol 272(6 Pt 2):H2793–H2806
Komukai K, Brette F, Yamanushi TT, Orchard CH (2002) K(+) current distribution in rat sub-epicardial ventricular myocytes. Pflugers Arch 444(4):532–538
Korchev YE, Bashford CL, Milovanovic M, Vodyanoy I, Lab MJ (1997) Scanning ion conductance microscopy of living cells. Biophys J 73(2):653–658
Kostin S, Rieger M, Dammer S et al (2003) Gap junction remodeling and altered connexin43 expression in the failing human heart. Mol Cell Biochem 242(1–2):135–144
Lacerda AE, Kim HS, Ruth P et al (1991) Normalization of current kinetics by interaction between the alpha 1 and beta subunits of the skeletal muscle dihydropyridine-sensitive Ca2+ channel. Nature 352(6335):527–530
Lacinova L, Ludwig A, Bosse E, Flockerzi V, Hofmann F (1995) The block of the expressed L-type calcium channel is modulated by the beta 3 subunit. FEBS Lett 373(2):103–107
Lampe PD, Lau AF (2004) The effects of connexin phosphorylation on gap junctional communication. Int J Biochem Cell Biol 36(7):1171–1186
Lee E, Marcucci M, Daniell L et al (2002) Amphiphysin 2 (Bin1) and T-tubule biogenesis in muscle. Science 297(5584):1193–1196
Lei M, Jones SA, Liu J et al (2004) Requirement of neuronal- and cardiac-type sodium channels for murine sinoatrial node pacemaking. J Physiol 559(Pt 3):835–848
Lenaerts I, Bito V, Heinzel FR et al (2009) Ultrastructural and functional remodeling of the coupling between Ca2+ influx and sarcoplasmic reticulum Ca2+ release in right atrial myocytes from experimental persistent atrial fibrillation. Circ Res 105(9):876–885
Leonoudakis D, Mailliard W, Wingerd K, Clegg D, Vandenberg C (2001) Inward rectifier potassium channel Kir2.2 is associated with synapse-associated protein SAP97. J Cell Sci 114(Pt 5):987–998
Li J, Patel VV, Kostetskii I et al (2005) Cardiac-specific loss of N-cadherin leads to alteration in connexins with conduction slowing and arrhythmogenesis. Circ Res 97(5):474–481
Li J, Kline CF, Hund TJ, Anderson ME, Mohler PJ (2010) Ankyrin-B regulates Kir6.2 membrane expression and function in heart. J Biol Chem 285(37):28723–28730
Lin X, Liu N, Lu J et al (2011) Subcellular heterogeneity of sodium current properties in adult cardiac ventricular myocytes. Heart Rhythm 8(12):1923–1930
Lipp P, Huser J, Pott L, Niggli E (1996) Spatially non-uniform Ca2+ signals induced by the reduction of transverse tubules in citrate-loaded guinea-pig ventricular myocytes in culture. J Physiol 497(Pt 3):589–597
Lisanti MP, Scherer PE, Vidugiriene J et al (1994) Characterization of caveolin-rich membrane domains isolated from an endothelial-rich source: implications for human disease. J Cell Biol 126(1):111–126
Lockwich TP, Liu X, Singh BB, Jadlowiec J, Weiland S, Ambudkar IS (2000) Assembly of Trp1 in a signaling complex associated with caveolin-scaffolding lipid raft domains. J Biol Chem 275(16):11934–11942
Lohn M, Furstenau M, Sagach V et al (2000) Ignition of calcium sparks in arterial and cardiac muscle through caveolae. Circ Res 87(11):1034–1039
Louch WE, Bito V, Heinzel FR et al (2004) Reduced synchrony of Ca2+ release with loss of T-tubules-a comparison to Ca2+ release in human failing cardiomyocytes. Cardiovasc Res 62(1):63–73
Louch WE, Mork HK, Sexton J et al (2006) T-tubule disorganization and reduced synchrony of Ca2+ release in murine cardiomyocytes following myocardial infarction. J Physiol 574(Pt 2):519–533
Lowe JS, Palygin O, Bhasin N et al (2008) Voltage-gated Nav channel targeting in the heart requires an ankyrin-G dependent cellular pathway. J Cell Biol 180(1):173–186
Lyon AR, MacLeod KT, Zhang Y et al (2009) Loss of T-tubules and other changes to surface topography in ventricular myocytes from failing human and rat heart. Proc Natl Acad Sci USA 106(16):6854–6859
Lyon AR, Bannister ML, Collins T et al (2011) SERCA2a gene transfer decreases sarcoplasmic reticulum calcium leak and reduces ventricular arrhythmias in a model of chronic heart failure. Circ Arrhythm Electrophysiol 4(3):362–372
Maier SK, Westenbroek RE, Schenkman KA, Feigl EO, Scheuer T, Catterall WA (2002) An unexpected role for brain-type sodium channels in coupling of cell surface depolarization to contraction in the heart. Proc Natl Acad Sci USA 99(6):4073–4078
Maier SK, Westenbroek RE, Yamanushi TT et al (2003) An unexpected requirement for brain-type sodium channels for control of heart rate in the mouse sinoatrial node. Proc Natl Acad Sci USA 100(6):3507–3512
Maier SK, Westenbroek RE, McCormick KA, Curtis R, Scheuer T, Catterall WA (2004) Distinct subcellular localization of different sodium channel alpha and beta subunits in single ventricular myocytes from mouse heart. Circulation 109(11):1421–1427
Makarewich CA, Correll RN, Gao H et al (2012) A caveolae-targeted L-type Ca(2)+ channel antagonist inhibits hypertrophic signaling without reducing cardiac contractility. Circ Res 110(5):669–674
Makarewich CA, Zhang H, Davis J et al (2014) Transient receptor potential channels contribute to pathological structural and functional remodeling after myocardial infarction. Circ Res 115(6):567–580
Malhotra JD, Thyagarajan V, Chen C, Isom LL (2004) Tyrosine-phosphorylated and nonphosphorylated sodium channel beta1 subunits are differentially localized in cardiac myocytes. J Biol Chem 279(39):40748–40754
Markandeya YS, Fahey JM, Pluteanu F, Cribbs LL, Balijepalli RC (2011) Caveolin-3 regulates protein kinase A modulation of the Ca(V)3.2 (alpha1H) T-type Ca2+ channels. J Biol Chem 286(4):2433–2444
Markandeya YS, Feng L, Vaidyanathan R et al (2013) Caveolin-3 regulates cardiac repolarization by integrated regulation of multiple ionic currents. Circulation 128:A15009
Mays DJ, Foose JM, Philipson LH, Tamkun MM (1995) Localization of the Kv1.5 K+ channel protein in explanted cardiac tissue. J Clin Invest 96(1):282–292
Mikami A, Imoto K, Tanabe T et al (1989) Primary structure and functional expression of the cardiac dihydropyridine-sensitive calcium channel. Nature 340(6230):230–233
Mitterdorfer J, Froschmayr M, Grabner M, Striessnig J, Glossmann H (1994) Calcium channels: the beta-subunit increases the affinity of dihydropyridine and Ca2+ binding sites of the alpha 1-subunit. FEBS Lett 352(2):141–145
Muller A, Schaefer T, Linke W et al (1997) Actions of the antiarrhythmic peptide AAP10 on intercellular coupling. Naunyn Schmiedebergs Arch Pharmacol 356(1):76–82
Nakamura H, Kurokawa J, Bai CX et al (2007) Progesterone regulates cardiac repolarization through a nongenomic pathway: an in vitro patch-clamp and computational modeling study. Circulation 116(25):2913–2922
Nakayama H, Wilkin BJ, Bodi I, Molkentin JD (2006) Calcineurin-dependent cardiomyopathy is activated by TRPC in the adult mouse heart. FASEB J 20(10):1660–1670
Nakayama H, Bodi I, Correll RN et al (2009) alpha1G-dependent T-type Ca2+ current antagonizes cardiac hypertrophy through a NOS3-dependent mechanism in mice. J Clin Invest 119(12):3787–3796
Nattel S, Maguy A, Le Bouter S, Yeh YH (2007) Arrhythmogenic ion-channel remodeling in the heart: heart failure, myocardial infarction, and atrial fibrillation. Physiol Rev 87(2):425–456
Nerbonne JM, Kass RS (2005) Molecular physiology of cardiac repolarization. Physiol Rev 85(4):1205–1253
Nikolaev VO, Moshkov A, Lyon AR et al (2010) Beta2-adrenergic receptor redistribution in heart failure changes cAMP compartmentation. Science 327(5973):1653–1657
Niwa N, Yasui K, Opthof T et al (2004) Cav3.2 subunit underlies the functional T-type Ca2+ channel in murine hearts during the embryonic period. Am J Physiol Heart Circ Physiol 286(6):H2257–H2263
Novak P, Li C, Shevchuk AI et al (2009) Nanoscale live-cell imaging using hopping probe ion conductance microscopy. Nat Methods 6(4):279–281
Novak P, Gorelik J, Vivekananda U et al (2013) Nanoscale-targeted patch-clamp recordings of functional presynaptic ion channels. Neuron 79(6):1067–1077
O’Connell KM, Whitesell JD, Tamkun MM (2008) Localization and mobility of the delayed-rectifer K+ channel Kv2.1 in adult cardiomyocytes. Am J Physiol Heart Circ Physiol 294(1):H229–H237
Pani B, Singh BB (2009) Lipid rafts/caveolae as microdomains of calcium signaling. Cell Calcium 45(6):625–633
Parton RG, Way M, Zorzi N, Stang E (1997) Caveolin-3 associates with developing T-tubules during muscle differentiation. J Cell Biol 136(1):137–154
Peivandi AA, Huhn A, Lehr HA et al (2005) Upregulation of phospholipase d expression and activation in ventricular pressure-overload hypertrophy. J Pharmacol Sci 98(3):244–254
Perez-Reyes E, Castellano A, Kim HS et al (1992) Cloning and expression of a cardiac/brain beta subunit of the L-type calcium channel. J Biol Chem 267(3):1792–1797
Petitprez S, Zmoos AF, Ogrodnik J et al (2011) SAP97 and dystrophin macromolecular complexes determine two pools of cardiac sodium channels Nav1.5 in cardiomyocytes. Circ Res 108(3):294–304
Poelzing S, Rosenbaum DS (2004) Altered connexin43 expression produces arrhythmia substrate in heart failure. Am J Physiol Heart Circ Physiol 287(4):H1762–H1770
Radwanski P, Brunello L, Priori SG et al (2012) Local Na+/Ca2+ signaling contributes to the propensity for arrhythmogenic spontanous Ca2+ waves during catecholaminergic polymorphic ventricular tachycardia (CPVT). Circulation 126:A17691
Ratajczak P, Damy T, Heymes C et al (2003) Caveolin-1 and -3 dissociations from caveolae to cytosol in the heart during aging and after myocardial infarction in rat. Cardiovasc Res 57(2):358–369
Razani B, Woodman SE, Lisanti MP (2002) Caveolae: from cell biology to animal physiology. Pharmacol Rev 54(3):431–467
Reynolds JO, Chiang DY, Wang W et al (2013) Junctophilin-2 is necessary for T-tubule maturation during mouse heart development. Cardiovasc Res 100(1):44–53
Rheinlaender JS, Tilman E (2009) Image formation, resolution, and height measurement in scanning ion conductance microscopy. J Appl Phys 105(9):094905 24
Richards MA, Clarke JD, Saravanan P et al (2011) Transverse tubules are a common feature in large mammalian atrial myocytes including human. Am J Physiol Heart Circ Physiol 301(5):H1996–H2005
Rickert DE, Fischer LJ (1975) Cyproheptadine and beta cell function in the rat: insulin secretion from pancreas segments in vitro. Proc Soc Exp Biol Med 150(1):1–6
Rizzo S, Lodder EM, Verkerk AO et al (2012) Intercalated disc abnormalities, reduced Na(+) current density, and conduction slowing in desmoglein-2 mutant mice prior to cardiomyopathic changes. Cardiovasc Res 95(4):409–418
Sanchez-Alonso JL, Bhogal N, Glukhov AV, Punjabi PP, Gorelik J (2014) Microdomain specific modulation of single L-type calcium channels revealed by super-resolution scanning patch-clamp in human failing cardiomyocytes. Heart Rhythm. http://ondemand.hrsonline.org/common/presentation-detail.aspx/15/23/1387/9549
Santos PE, Barcellos LC, Mill JG, Masuda MO (1995) Ventricular action potential and L-type calcium channel in infarct-induced hypertrophy in rats. J Cardiovasc Electrophysiol 6(11):1004–1014
Sato PY, Musa H, Coombs W et al (2009) Loss of plakophilin-2 expression leads to decreased sodium current and slower conduction velocity in cultured cardiac myocytes. Circ Res 105(6):523–526
Sato PY, Coombs W, Lin X et al (2011) Interactions between ankyrin-G, Plakophilin-2, and Connexin43 at the cardiac intercalated disc. Circ Res 109(2):193–201
Saucerman JJ, Greenwald EC, Polanowska-Grabowska R (2014) Mechanisms of cyclic AMP compartmentation revealed by computational models. J Gen Physiol 143(1):39–48
Schaper J, Kostin S, Hein S, Elsasser A, Arnon E, Zimmermann R (2002) Structural remodelling in heart failure. Exp Clin Cardiol 7(2–3):64–68
Schulson MN, Scriven DR, Fletcher P, Moore ED (2011) Couplons in rat atria form distinct subgroups defined by their molecular partners. J Cell Sci 124(Pt 7):1167–1174
Scriven DR, Dan P, Moore ED (2000) Distribution of proteins implicated in excitation-contraction coupling in rat ventricular myocytes. Biophys J 79(5):2682–2691
Scriven DR, Asghari P, Moore ED (2013) Microarchitecture of the dyad. Cardiovasc Res 98(2):169–176
Severs NJ (2000) The cardiac muscle cell. Bioessays 22(2):188–199
Shaw RM, Fay AJ, Puthenveedu MA, von Zastrow M, Jan YN, Jan LY (2007) Microtubule plus-end-tracking proteins target gap junctions directly from the cell interior to adherens junctions. Cell 128(3):547–560
Shevchuk AI, Frolenkov GI, Sanchez D et al (2006) Imaging proteins in membranes of living cells by high-resolution scanning ion conductance microscopy. Angew Chem Int Ed Engl 45(14):2212–2216
Shibata EF, Brown TL, Washburn ZW, Bai J, Revak TJ, Butters CA (2006) Autonomic regulation of voltage-gated cardiac ion channels. J Cardiovasc Electrophysiol 17[Suppl 1]:S34–S42
Singer D, Biel M, Lotan I, Flockerzi V, Hofmann F, Dascal N (1991) The roles of the subunits in the function of the calcium channel. Science 253(5027):1553–1557
Sipido KR, Cheng H (2013) T-tubules and ryanodine receptor microdomains: on the road to translation. Cardiovasc Res 98(2):159–161
Sipido KR, Carmeliet E, Van de Werf F (1998) T-type Ca2+ current as a trigger for Ca2+ release from the sarcoplasmic reticulum in guinea-pig ventricular myocytes. J Physiol 508(Pt 2):439–451
Sipido KR, Acsai K, Antoons G, Bito V, Macquaide N (2013) T-tubule remodelling and ryanodine receptor organization modulate sodium-calcium exchange. Adv Exp Med Biol 961:375–383
Smyrnias I, Mair W, Harzheim D, Walker SA, Roderick HL, Bootman MD (2010) Comparison of the T-tubule system in adult rat ventricular and atrial myocytes, and its role in excitation-contraction coupling and inotropic stimulation. Cell Calcium 47(3):210–223
Smyth JW, Hong TT, Gao D et al (2010) Limited forward trafficking of connexin 43 reduces cell-cell coupling in stressed human and mouse myocardium. J Clin Invest 120(1):266–279
Song KS, Scherer PE, Tang Z et al (1996) Expression of caveolin-3 in skeletal, cardiac, and smooth muscle cells. Caveolin-3 is a component of the sarcolemma and co-fractionates with dystrophin and dystrophin-associated glycoproteins. J Biol Chem 271(25):15160–15165
Song LS, Pi Y, Kim SJ et al (2005) Paradoxical cellular Ca2+ signaling in severe but compensated canine left ventricular hypertrophy. Circ Res 97(5):457–464
Song LS, Sobie EA, McCulle S, Lederer WJ, Balke CW, Cheng H (2006) Orphaned ryanodine receptors in the failing heart. Proc Natl Acad Sci USA 103(11):4305–4310
Spach MS, Miller WT 3rd, Geselowitz DB, Barr RC, Kootsey JM, Johnson EA (1981) The discontinuous nature of propagation in normal canine cardiac muscle. Evidence for recurrent discontinuities of intracellular resistance that affect the membrane currents. Circ Res 48(1):39–54
Stangherlin A, Zaccolo M (2012) Phosphodiesterases and subcellular compartmentalized cAMP signaling in the cardiovascular system. Am J Physiol Heart Circ Physiol 302(2):H379–H390
Takeuchi S, Takagishi Y, Yasui K, Murata Y, Toyama J, Kodama I (2000) Voltage-gated K(+)Channel, Kv4.2, localizes predominantly to the transverse-axial tubular system of the rat myocyte. J Mol Cell Cardiol 32(7):1361–1369
Thomas MJ, Sjaastad I, Andersen K et al (2003) Localization and function of the Na+/Ca2+−exchanger in normal and detubulated rat cardiomyocytes. J Mol Cell Cardiol 35(11):1325–1337
Trafford AW, Clarke JD, Richards MA, Eisner DA, Dibb KM (2013) Calcium signalling microdomains and the t-tubular system in atrial mycoytes: potential roles in cardiac disease and arrhythmias. Cardiovasc Res 98(2):192–203
Vaidyanathan R, Vega AL, Song C et al (2013) The interaction of caveolin 3 protein with the potassium inward rectifier channel Kir2.1: physiology and pathology related to long qt syndrome 9 (LQT9). J Biol Chem 288(24):17472–17480
van Veen TA, van Rijen HV, Jongsma HJ (2006) Physiology of cardiovascular gap junctions. Adv Cardiol 42:18–40
Vatta M, Ackerman MJ, Ye B et al (2006) Mutant caveolin-3 induces persistent late sodium current and is associated with long-QT syndrome. Circulation 114(20):2104–2112
Wang YG, Dedkova EN, Ji X, Blatter LA, Lipsius SL (2005) Phenylephrine acts via IP3-dependent intracellular NO release to stimulate L-type Ca2+ current in cat atrial myocytes. J Physiol 567(Pt 1):143–157
Warrier S, Ramamurthy G, Eckert RL, Nikolaev VO, Lohse MJ, Harvey RD (2007) cAMP microdomains and L-type Ca2+ channel regulation in guinea-pig ventricular myocytes. J Physiol 580(Pt.3):765–776
Wei CJ, Francis R, Xu X, Lo CW (2005) Connexin43 associated with an N-cadherin-containing multiprotein complex is required for gap junction formation in NIH3T3 cells. J Biol Chem 280(20):19925–19936
Wei S, Guo A, Chen B et al (2010) T-tubule remodeling during transition from hypertrophy to heart failure. Circ Res 107(4):520–531
Wiegerinck RF, de Bakker JM, Opthof T et al (2009) The effect of enhanced gap junctional conductance on ventricular conduction in explanted hearts from patients with heart failure. Basic Res Cardiol 104(3):321–332
Willoughby D, Cooper DM (2007) Organization and Ca2+ regulation of adenylyl cyclases in cAMP microdomains. Physiol Rev 87(3):965–1010
Winslow RL, Greenstein JL (2011) Cardiac myocytes and local signaling in nano-domains. Prog Biophys Mol Biol 107(1):48–59
Woo SH, Cleemann L, Morad M (2003) Spatiotemporal characteristics of junctional and nonjunctional focal Ca2+ release in rat atrial myocytes. Circ Res 92(1):e1–e11
Wu X, Eder P, Chang B, Molkentin JD (2010) TRPC channels are necessary mediators of pathologic cardiac hypertrophy. Proc Natl Acad Sci USA 107(15):7000–7005
Yamada Y, Nagashima M, Tsutsuura M et al (2001) Cloning of a functional splice variant of L-type calcium channel beta 2 subunit from rat heart. J Biol Chem 276(50):47163–47170
Zaccolo M, Pozzan T (2002) Discrete microdomains with high concentration of cAMP in stimulated rat neonatal cardiac myocytes. Science 295(5560):1711–1715
Zhang P, Mende U (2011) Regulators of G-protein signaling in the heart and their potential as therapeutic targets. Circ Res 109(3):320–333
Zhang XQ, Moore RL, Tillotson DL, Cheung JY (1995) Calcium currents in postinfarction rat cardiac myocytes. Am J Physiol 269(6 Pt 1):C1464–C1473
Zhang C, Chen B, Guo A et al (2014) Microtubule-mediated defects in junctophilin-2 trafficking contribute to myocyte transverse-tubule remodeling and Ca2+ handling dysfunction in heart failure. Circulation 129(17):1742–1750
Zhou Z, January CT (1998) Both T- and L-type Ca2+ channels can contribute to excitation-contraction coupling in cardiac Purkinje cells. Biophys J 74(4):1830–1839
Zingman LV, Alekseev AE, Hodgson-Zingman DM, Terzic A (2007) ATP-sensitive potassium channels: metabolic sensing and cardioprotection. J Appl Physiol 103(5):1888–1893
Acknowledgements
We thank Ms Navneet Bhogal and Dr Ivan Diakonov for helpful discussion and correction of the manuscript.
Compliance with Ethics Guidelines
ᅟ
Funding
This work was primarily supported by Wellcome Trust WT090594 and British Heart Foundation12/18/30088 to JG.
Conflict of interest
Marina Balycheva, Giuseppe Faggian, Alexey V. Glukhov, and Julia Gorelik declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human or animal subjects performed by theany of the authors.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Special Issue: Biophysics of Human Heart Failure
Rights and permissions
About this article
Cite this article
Balycheva, M., Faggian, G., Glukhov, A.V. et al. Microdomain–specific localization of functional ion channels in cardiomyocytes: an emerging concept of local regulation and remodelling. Biophys Rev 7, 43–62 (2015). https://doi.org/10.1007/s12551-014-0159-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12551-014-0159-x