Abstract
Background
Emerging literature has demonstrated deficits in interoception (i.e., the perception of physical sensations from inside the body) in individuals with chronic pain conditions. Mind-body therapies (MBTs) are purported to improve chronic pain in part through improving or restoring interoceptive abilities. The present systematic review and meta-analysis aimed to examine changes in interoception in MBTs for chronic pain conditions.
Methods
A systematic search of PubMed, PsycINFO, Scopus, CINAHL, and ProQuest Dissertation and Theses was conducted from database inception to February 2023. English language intervention studies evaluating the effect of MBTs on interoception in adults with chronic pain conditions were examined. Changes in pain (severity and interference) following treatment were examined as secondary outcomes.
Results
A total of 11 studies (10 unique samples) were identified. Meta-analytic results reveal significant improvements in total interoceptive awareness (Becker’s d = 1.168, p < .01) as well as improvements in seven of eight subdomains of interoceptive awareness (ds = 0.28 to 0.81). MBTs were also associated with reductions in both pain intensity (d = -1.46, p = .01) and pain interference (d = -1.07, p < .001).
Conclusions
Preliminary research suggests that MBTs demonstrate improvements in interoceptive awareness and reduce pain in adults with chronic pain. Literature on changes in other domains of interoception, such as interoceptive accuracy, following MBTs is severely lacking. Although more rigorous studies are needed to corroborate results, the present findings lay an important foundation for future research to examine interoception as a possible underlying mechanism of MBTs to improve pain outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pain is an extremely prevalent, highly disabling, and economically costly health condition [1]. Many biopsychosocial factors have been proposed as underlying mechanisms in the maintenance of chronic pain. One such hypothesized maintaining factor is deficits in interoception (i.e., the perception of physical sensations from inside the body). Non-pharmacological pain interventions, particularly Mind-body therapies (MBTs), are purported to target the restoration of interoceptive processes [2, 3]. However, whether MBTs are effective in improving interoception, and whether changes in interoception in MBTs are also accompanied by pain reductions, remain unknown. Identifying mechanisms of change is important for treatment refinement and optimization [4]. Thus, the present study aims to address these two issues through a systematic review and meta-analysis of the literature on changes in interoception in individuals with chronic pain undergoing an MBT.
Chronic pain is defined as pain that persists over three months, beyond the healing phase of an injury [5]. Chronic pain is a major public health concern, with recent estimates suggesting up to 1 in 5 adults in the United States experience chronic pain [6]. Chronic pain is associated with numerous psychological, social, physical, and economic concerns [6,7,8,9,10]. Common pharmacologic interventions for pain (e.g., opioids) are often problematic due to their high addiction and abuse potential, side effects, and limited evidence of their long-term effectiveness [11]. Given these limitations, much attention has been dedicated to studying non-pharmacologic interventions for pain conditions, including psychological interventions (e.g., Cognitive Behavioral Therapy [12], Acceptance and Commitment Therapy [13]), and physical therapy interventions [14], among others.
Although several factors have been hypothesized as mechanisms of change in pain management interventions, the role of interoception in chronic pain conditions has received growing empirical attention. To date, interoception has been defined and operationalized in a variety of ways, complicating research across disciplines. For instance, Craig [15] conceptualized interoception as the sense of the physiological condition of the entire body and asserted that interoceptive information is essential for motivating behavior and maintaining homeostasis [15, 16]. Garfinkel [17] proposed a more differentiated model of interoception that includes three dimensions: interoceptive accuracy (one’s objective accuracy in detecting internal bodily sensations); interoceptive sensibility (one’s self-perceived dispositional tendency to be cognizant of/focused on interoceptive signals); and interoceptive awareness (one’s metacognitive awareness of their own interoceptive accuracy; hereafter referred to as metacognitive awareness). Calì and colleagues [18] proposed a bi-directional conceptual framework of interoceptive processes that includes interoceptive accuracy, one’s accuracy in perceiving interoceptive information, and interoceptive awareness, one’s awareness of the afferent information that arises from anywhere within the body, including higher mental processes such as emotion.
In an effort to clarify definitions of interoception and create a coherent construct, experts across a range of disciplines recently described interoception as an iterative process of noticing/attending to, appraising, and regulating bodily signals [19]. These processes are also all purported to be influenced by other factors and experiences such as contemplative practices [19]. Similarly, Mehling argued that interoceptive awareness (similar to but more comprehensive than Garfinkel’s narrower interoceptive sensibility) is itself a multidimensional construct that involves not only one’s tendency to be aware of internal sensations, but also one’s attentional, emotional, and regulatory responses towards those sensations [20,21,22].
Debate regarding how to appropriately measure interoception has also surfaced. Interoceptive accuracy is often assessed through objective measures such as heartbeat perception tasks [23,24,25], although the reliability and validity of these objective measures have been questioned [26]. Self-report measures are used to assess the dimension of interoceptive awareness/sensibility, although there is confusion surrounding this particular interoceptive dimension and its measurement, which is likely attributable in part to the conflation of the terms body awareness and interoceptive awareness. Several self-report body awareness questionnaires are based on older conceptualizations of interoception and/or tend to reflect only a unidimensional construct [27]. Therefore, the Multidimensional Assessment of Interoceptive Awareness (MAIA) [21] was developed to capture the multiple dimensions of interoceptive awareness and to distinguish between a maladaptive anxiety-related hypervigilance towards sensations and an adaptive, nonjudgmental, mindful awareness of these sensations [21]. Finally, interoceptive metacognitive awareness is typically measured by receiver operating characteristic (ROC) curve analysis to assess the extent to which confidence in interoceptive performance predicts accuracy on an interoceptive task [17]. However, studies have relatively rarely assessed the metacognitive awareness dimension of interoception.
For the present review and meta-analysis, we aimed to incorporate multiple views of interoception and thus operationalized interoception similar to Garfinkle’s three-dimensional model, consistent with other closely-related reviews [28]. The dimension of interoceptive sensibility was further expanded in accordance with both Calì’s [18] and Mehling’s [21] multidimensional definition that includes one’s self-reported tendency to not only notice internal signals but also one’s attentional, emotional, and regulatory style towards those signals. This more comprehensive construct better captures a purported key mechanism of change in Mind-body treatments and the multitude of psychological factors that contribute to an individual’s perception of pain. In the present review, we label that dimension interoceptive awareness.
With regard to its role in chronic pain conditions, a recent review indicated significant deficits in interoceptive processes in individuals with chronic pain, particularly in interoceptive accuracy [28]. Recent studies also suggest interoceptive awareness deficits in pain conditions [e.g., 29, 30], although this link remains less clear, with other studies not finding significant differences in pain compared to healthy populations [e.g., 31].
The experience of pain itself can be considered a form of interoceptive input that results from a multimodal integration of sensations, learned associations, memories, and emotions [32]. Several individual-level factors modulate the perception of pain, including attentional, emotional, and appraisal processes [33,34,35]. The perception of pain intensity is largely due to the way attention is focused on the pain. For instance, one may ignore the pain; focus on the pain with worry, rumination, or fear; or focus on the pain with mindful attention [36].
While seemingly contradictory that attention towards internal bodily sensations may actually benefit people with pain, attempts to suppress awareness of pain may actually be unhelpful [37, 38] and for individuals with a high level of catastrophic thinking about pain, mindfulness-based coping strategies may be more beneficial than distraction [39]. From a behavioral perspective, interoception plays a role in pain maintenance not through increased attention towards bodily sensations, but rather through learned avoidance of internal stimuli often associated with pain and the reinforcement of avoidance behaviors, resulting in a cycle that ultimately perpetuates fear of internal sensations and a catastrophic misinterpretation of pain [40]. Taken together, research implicates interoceptive alterations as an important factor in chronic pain conditions, suggesting that targeting the reparation of these processes in chronic pain treatments may be valuable.
Mind-body therapies (MBTs) are one category of non-pharmacologic interventions that have received growing attention for the treatment of chronic pain and are purported to improve interoceptive processes. MBTs (e.g., yoga, Tai Chi, etc.) have roots in ancient traditional Eastern practices, and in more recent decades have been incorporated into Western society and medical settings [41]. The American Psychological Association (APA) defines MBTs as “therapeutic approaches that focus on harnessing the power of the mind to bring about change in the body or achieve reduction of symptoms of disease or disorder [42]”. MBTs include but are not limited to yoga, tai chi, meditation, relaxation, and biofeedback [43]. Regarding MBTs for pain, research shows that long-term meditators [44] as well as regular yoga practitioners [45] have greater pain tolerance compared to non-practitioners and also demonstrate strengthened brain areas linked with interoceptive processes [44, 45].
Given that the primary problem in chronic pain conditions is not necessarily the pain itself but rather how individuals experience the sensations within their body [44, 46], interventions that teach individuals to experience their sensations in an accepting, nonjudgmental way may help to change their subjective experiences of pain. Indeed, MBTs have been shown to be effective treatments for chronic pain [e.g., 47] and improvement in interoception is hypothesized to be a key mechanism of Mind-body therapies [2]. Due to the interoceptive deficits in individuals with chronic pain [e.g., 28], Mind-body therapies may be especially useful for improving interoception, which in turn may mitigate or reduce pain. However, to date, no meta-analysis has statistically tested whether MBTs are associated with changes to interoception in chronic pain. The present systematic review and meta-analysis aims to fill this gap. Additionally, changes in two commonly-studied indices of pain (i.e., pain intensity and pain interference) will be evaluated as secondary outcomes within a subset of studies that also examined interoception to examine whether changes in interoception coincide with changes in pain in MBTs.
Methods
The study was pre-registered in PROSPERO prior to conducting the search (#CRD42021262472) and complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) guidelines. Search terms and strategies were finalized with the assistance of an academic librarian. Searches were conducted from database inception through February 2023 in five databases (CINAHL, PsycInfo, PubMed, SCOPUS, and ProQuest Dissertations and Theses). When applicable, both the Medical Subject Headings (MeSH) terms and the keywords were searched. The full search strings for each database can be found in the Appendix. The complete list of studies was first uploaded to RefWorks to remove duplicates, and then was imported into Rayyan [48] for title and abstract screening. Full texts of potentially relevant studies were retrieved and reviewed for eligibility. All studies were independently screened and coded by at least two of three authors (KG, SS, LL), and any discrepancies were discussed with a third author until a consensus about inclusion was reached.
Study Selection and Data Extraction
Studies were screened for eligibility according to the following criteria: a) authors reported a Mind-body therapy intervention; b) the primary target of treatment improvement was a chronic pain condition; c) one or more dimensions of interoception was quantitatively measured both pre- and post-intervention following our operationalization of the construct (e.g., multidimensional nature of interoceptive awareness had to be assessed); d) samples comprised adults 18 or older; and e) studies had to be available in English. For a depiction of the study selection process, see the PRISMA Flow Diagram [49] in Fig. 1.
For the present review, we were interested in interoceptive awareness as a multidimensional construct, including how internal signals are appraised and regulated, and beyond simply the self-reported tendency to notice internal symptoms or the maladaptive anxiety-related response to bodily sensations. Thus, to prevent confusion or contradictions in results, and consistent with previous related systematic reviews [28], studies that included only broad body awareness measures were excluded. One study [50] used the Scale of Body Connection, which is composed of two subscales: Body Awareness and Body Dissociation [SBC; 51]. The SBC was designed as a multidimensional measure of body awareness that includes the identification of inner sensory awareness, the overall emotional/physiologic state of the body, and attending to bodily information in daily life [51]. This measure was ultimately deemed eligible for the systematic review because it captures a multidimensional nature of interoceptive awareness as it was operationally defined for the present review. While we included the study that used the SBC in our literature review, we excluded it from meta-analyses because the subscale constructs were not comparable to those in all other included studies.
Data were extracted from eligible studies on sample characteristics, study design, intervention description, and measurement and outcomes of interoception and pain (Table 1). All extracted data was double-coded and compared for 100% accuracy before proceeding with analyses. Pain outcomes included in the present review included pain severity and interference; two authors agreed upon inclusion of specific pain measures that captured the two listed pain constructs. Consistent with previous studies [52], data on intention-to-treat (ITT) were used when possible. Where insufficient information to calculate standardized mean differences (SMD) was reported (e.g., subscale scores of MAIA), attempts were made to contact study authors and obtain the missing data. If the authors did not respond or indicated they could not provide the requested data in the allotted time frame, the studies were not included in the respective meta-analysis.
Risk of Bias Assessment
The quality of included studies was carefully and independently evaluated by two coders. Given the different study designs included in the review, two quality assessment tools were used where appropriate; for all RCTs, Cochrane Collaboration’s Risk of Bias-2 (RoB2) tool was used [53], and for single arm studies, the NIH Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group was used. This quality assessment approach is consistent with other recent reviews on Mind-body interventions for pain conditions [e.g., 54].
Meta-Analysis Methods
All raw scores and calculated effect size scores were double-coded by two authors. When there was a discrepancy in values between the two authors, a third author coded the values. All three authors (KG, SS, LL) had to come to a consensus about each value before proceeding. To standardize scores across measures, percent of maximum possible (POMP) mean and standard deviation scores were calculated for all interoception (primary) and pain (secondary) outcomes. To calculate effect sizes, we calculated standardized mean difference (SMD) scores, using a within-subject design. SMDs were calculated with Wilson’s effect size calculator [55] from pre- and post-intervention means and pre-intervention standard deviations, as recommended by Becker’s d [56] for calculating within-group effects. When ITT analysis was reported, pre-intervention Ns were used for calculations; otherwise, we used pre- and post-treatment Ns as provided. To calculate standard errors (SE), we used the formula referenced in Cochrane’s Handbook (i.e., (upper confidence interval – lower confidence interval) / 3.92) [57]. Positive effect sizes indicate an increase in the mean score. For the present study, only scores pre- and immediately post-treatment were used; long-term follow-up assessments were not examined.
After effect sizes and standard errors (SE) were calculated, the remaining analyses were performed in both JASP [58] and R statistical software, utilizing the “metafor” package [59]. Pre-post intervention effects and tests of heterogeneity were performed using the “rma” function within metafor. Funnel plots and Egger’s test were used to test for Funnel plot asymmetry to detect possible publication bias. For analyses in both statistical softwares, a restricted maximum likelihood estimation approach was employed. Due to power limitations, we were unable to test potential moderators of effects (e.g., age, gender, race, treatment duration); we report intercorrelations of these variables in Supplementary Table 1.
Results
Of the 512 non-duplicate studies, 385 were removed based on title and abstract. A total of 127 full-text articles were retrieved and examined for specific inclusion criteria. Of the 127 full-text studies screened, 11 met full inclusion criteria. Upon further review, two of the 11 studies that met inclusion criteria [60, 61] were based on participant data from the same study (main study findings and secondary analysis). Thus, while 11 studies met inclusion criteria, these studies represent only 10 unique participant samples.
Participant Characteristics
MBT groups ranged between 19–50 individuals. All samples comprised primarily female participants, with two including only female participants [62, 63]. Mean age of participants in the MBT groups was between 40.15 and 61.21 years. Of studies that did report race and ethnicity, most samples were primarily White and non-Hispanic, with only one study comprising a predominantly African American sample [64]. The remaining studies (6/11) did not report the specific racial or ethnic breakdown of their sample, although Roberts et al. [65] noted the majority of participants racially identified as White. Four study samples had chronic low back pain [63, 66,67,68]. Two samples had chronic nonspecific neck pain [50, 60]. One sample included breast cancer survivors with persistent post-surgical pain [62]. One study included samples with general chronic pain conditions [64], one study included participants with opioid-treated chronic pain [65], and one included participants with both chronic pain and comorbid depression [69].
Mind-body Therapy Interventions
Five studies investigated movement-based MBTs as the treatment condition. One study examined Qigong [62]. Two used the Feldenkrais method [63, 67], a Mind-body therapy method aimed at “increasing awareness through habitual movements and activities of daily life” [63]. One study evaluated Dance/Movement Therapy [64], and one used Tai Chi [60]. Three studies used mindfulness-based interventions as the treatment condition. One study used mindfulness-based cognitive therapy (MBCT; 69) another used self-compassion meditation [66], and the third used Mindfulness Oriented Recovery Enhancement (MORE; 65). Finally, two studies examined MBTs with a therapeutic touch-based component as the treatment condition; one explored massage therapy plus a preparatory phase that involved the active role of the patient engaging in dialogue with the practitioner regarding emotional and cognitive perceptions [68], and another used craniosacral therapy [50].
Risk of Bias
Among RCTs (n = 7), all studies were deemed low risk for the randomization process, and all but one [69] for missing outcome data. All seven studies were rated as having some concerns for deviations from intended interventions, primarily due to limited information provided about whether deviations occurred. For the domain assessing measurement of the outcome, one study was rated as low risk, four as having “some concerns”, and two as “high risk” (i.e., due to the self-report nature of the outcome and likelihood that assessment of the outcome was influenced by knowledge of intervention received). Finally, the majority (6/7) were coded as low risk for selection of the reported results. Among the three single-arm pre-post studies, overall quality was rated as “fair”; primary concerns for all three included the self-report nature of outcomes and low statistical power. Risk of bias assessments for individual studies are depicted in Supplementary Fig. 1 and Table 2.
Changes in Interoception from Pre- to Post-Treatment
Of the 10 independent studies, 9 used the MAIA [21] as a measure of interoception, reflecting the sub-dimension of interoceptive awareness. The MAIA is a self-report measure designed to measure and differentiate among multiple facets of interoceptive awareness. The MAIA yields eight subscales: Noticing: the awareness of uncomfortable, comfortable, and neutral body sensations; Not-Distracting: the tendency not to ignore or distract oneself from sensations of pain or discomfort; Not-Worrying: the tendency not to worry or experience emotional distress with sensations of pain or discomfort; Attention Regulation: the ability to sustain and control attention to body sensations; Emotional Awareness: the awareness of the connection between body sensations and emotional states; Self-Regulation: the ability to regulate distress by attention to body sensations; Body Listening: the active listening to the body for insight; and Trusting: the experience of one’s body as safe and trustworthy [21, 22]. There was some variability in the reporting of MAIA scores between studies; for instance, two studies [63, 68] reported MAIA total scores but did not report findings regarding the individual subscales, and one study [65] reported on overall interoceptive changes in a latent variable constructed from the MAIA (See Table 1). Attempts were made to retrieve additional scores from authors prior to conducting analyses. As noted, one study [50] used the Scale of Body Connection (Body Awareness and Body Dissociation subscales) [51]. Finally, no studies assessed interoceptive accuracy nor interoceptive metacognitive awareness.
Meta-analyses revealed evidence for short-term effects of MBTs on changes in interoceptive awareness from pre- to post-treatment (see Fig. 2). MBTs were associated with increases in interoception total scores that were large in effect size (Becker’s d = 1.168, p = .003, 95% CI [0.390, 1.945], k = 4), and changes for seven of the eight interoceptive awareness subscales that were of small-moderate effect size: Not-Worrying (d = .393, p = .008, 95% CI [0.102, 0.684], k = 4); Not-Distracting (d = .275, p = .047, 95% CI [0.004, 0.545], k = 5) Trusting (d = .541, p = .029, 95% CI [0.056, 1.026], k = 4); Self-Regulation (d = .684, p = .0001, 95% CI [0.333, 1.034], k = 5); Emotional Awareness (d = .377, p = .019, 95% CI [0.062, 0.691], k = 5); Attention Regulation (d = .641, p < .001, 95% CI [0.363, 0.918], k = 5); Body Listening (d = .806, p < .001, 95% CI [0.328, 1.284], k = 4). The Noticing subscale was the only subscale that did not demonstrate significant pre-post-treatment change (d = .227, p = .098, 95% CI [-0.042, 0.496], k = 5).
Heterogeneity Across Studies
We also tested for heterogeneity across studies. Significant heterogeneity suggests that the findings may be context dependent, as certain trends were not seen uniformly across samples. With regard to interoception scores, only interoception total scores demonstrated significant heterogeneity (Q = 17.022, p < .001; tau2 = .518; I2 = 82.55%, 95% CI [45.34%, 98.75%]). We did not observe significant heterogeneity in any of the interoception subscale scores, including Noticing (Q = .757, p = .944; tau2 = 0; I2 = 0.00%, 95% CI [0.00%, 37.45%]), Not-Distracting (Q = .917, p = .922; tau2 = 0; I2 = 0.00%, 95% CI [0.00%, 49.86%]), Not-Worrying (Q = 1.975, p = .578; tau2 = 0; I2 = 0.00%, 95% CI [0.00%, 88.52%]), Trusting (Q = 7.253, p = .064; tau2 = 0.146; I2 = 60.20%, 95% CI [0.00%, 97.57%]), Self-regulation (Q = 6.003, p = .199; tau2 = 0.053; I2 = 33.21%, 95% CI [0.00%, 92.38%]), Emotional Awareness (Q = 4.245, p = .374; tau2 = 0.028; I2 = 21.62%, 95% CI [0.00%, 84.92%]), Attention Regulation (Q = 3.987, p = .408; tau2 = 0; I2 = 0.00%, 95% CI [0.00%, 88.67%]), and Body Listening (Q = 6.713, p = .082; tau2 = 0.133; I2 = 56.74%, 95% CI [0.00%, 97.54%]). However, the heterogeneity statistic I2 must be interpreted with caution in the present study given the limited number of studies included in the meta-analyses [70].
Publication Bias
We used Egger’s Test to test for publication bias across studies for each scale (see Fig. 3 for funnel plots). We found that there was evidence of publication bias in pain intensity (z = -2.437, p = .015) but not in pain interference (z = -.417, p = .676). We did not see evidence of publication bias in interoception total scores (z = -.437, p = .662), nor in any of the interoception subscales, including Noticing (z = -.244, p = .807), Not-Distracting (z = .226, p = .821), Not-Worrying (z = 1.176, p = .240), Trusting (z = 1.161, p = .245), Self-regulation (z = 1.665, p = .096), Emotional Awareness (z = 1.918, p = .055), Attention Regulation (z = 1.153, p = .249), and Body Listening (z = 1.019, p = .308).
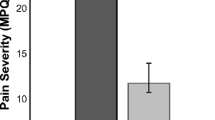
Changes in Pain Severity and Interference from Pre- to Post-Treatment
Six studies reported mean changes in pain severity and pain interference. Measures assessing each construct are reported in Table 1. Meta-analytic results revealed a significant decrease in pain intensity from pre- to post-intervention across studies (Becker’s d = -1.462, p = .012, 95% CI [-2.609, -0.315], k = 6). Additionally, there was a significant decrease in pain interference scores from pre- to post-intervention (d = -1.072, p < .001, 95% CI [-1.565, -0.579], k = 6). There was significant heterogeneity across studies in both pain intensity (Q = 69.528, p < .001; tau2 = 1.937, s.e. = 1.300; I2 = 94.93%, 95% CI [86.67%, 99.20%]) and pain interference (Q = 20.220, p = .001; tau2 = .285, s.e. = .240; I2 = 75.73%, 95% CI [36.85%, 96.07%]). Based on Egger’s test, there was evidence of potential publication bias in pain intensity (z = -2.437, p = .015) but not in pain interference (z = -.417, p = .676).
Finally, only three studies assessed whether interoception was associated with pain outcomes. Paolucci et al. [67] found that the post-treatment MAIA Noticing score was associated with change in pain between post-treatment and long-term follow-up. Only Lauche et al. [61] and Berry et al. [66] assessed change in MAIA subscales as a predictor of pain outcomes. Lauche et al. [61] found a non-significant relation between changes in MAIA and pain intensity, while Berry et al. [66] found that increased pain anticipation response in the ventral posterior cingulate cortex was associated with an increase in the Body Listening subscale. Berry et al. [66] did not assess the relationship between changes in MAIA and changes in self-reported pain.
Discussion
To our knowledge, this is the first systematic review and meta-analysis to examine changes in interoception in MBTs for chronic pain. Overall, results of the systematic review and meta-analysis found preliminary evidence that participants with chronic pain improve in interoceptive awareness following MBTs. Consistent with hypothesized mechanisms [19], interventions aiming to cultivate more adaptive interoceptive abilities do tend to show improvements in these areas, at least regarding interoceptive awareness, and also appear to be clinically useful in the treatment of pain. Yet whether MBTs demonstrate changes in other interoception dimensions (i.e., accuracy, metacognitive awareness) warrants further study.
More specifically, results reveal that MBTs are associated with improvements in overall interoceptive awareness (as measured by a total score of the multidimensional construct) as well as specific changes in most subdimensions of interoceptive awareness, namely Not-Worrying, Trusting, Self-Regulation, Emotional Awareness, Attention Regulation, and Body Listening. The only interoceptive awareness subdimension to not demonstrate significant change from pre- to post-treatment across studies was the Noticing subscale (i.e., the awareness of uncomfortable, comfortable, and neutral body sensations). This finding is particularly noteworthy given that the Noticing subscale is arguably the only subscale that is not just focused on adaptive relations to internal sensations, in that it encompasses awareness of not just comfortable and neutral but also uncomfortable bodily sensations. Thus, MBTs are associated with changes in many facets of interoceptive awareness without necessarily invoking increased awareness of uncomfortable sensations (which tend to already be heightened in individuals with chronic pain).
Importantly, in addition to improvements in interoceptive awareness across multiple pain conditions (e.g., CLBP, neck pain, persistent post-surgical pain), MBTs were also accompanied by pain reductions in the reviewed studies. Findings that MBTs are generally helpful in reducing pain is consistent with other recent reviews [71, 72], and the present findings also demonstrate simultaneous improvements in interoception within those treatments. Whether or not changes in interoception account for changes in pain remains to be determined.
This meta-analysis is not without limitations. First, significant heterogeneity in meta-analytic results suggest that the effects of these studies may be context dependent; however, the heterogeneity statistic used in this analysis (I2) is known to be biased in analyses with small numbers of studies and thus should be interpreted with caution [70]. Given the limited studies to date that met inclusion criteria and that had sufficient data, and given moderate risk of bias among most studies, more rigorous research examining changes in interoceptive awareness in MBTs is needed to determine between-intervention effects on change (i.e., are specific MBTs more effective at increasing interoceptive awareness?).
Studies included in this review were limited by their sample size and characteristics. All of the samples were primarily female, and thus, the generalizability of findings are limited. It is unclear whether MBTs produce equivalent interoceptive changes in individuals who do not identify as female, or whether there are gender differences in responses to MBTs. It is also important to note that several studies did not report on race, and of those that did, all but one recruited predominantly White samples. As is common in clinical trials more broadly [73], studies included in this review thus demonstrate an underrepresentation of individuals with marginalized racial/ethnic identities and as such, are limited in terms of generalizability of findings. Among the myriad factors that can be attributed to this discrepancy include systemic oppression and related barriers to participation (e.g., transportation, childcare, work-related demands, distrust of researchers) as well as lack of strategies used in research settings to promote inclusion [74]. Additionally, and more specific to MBTs, willingness to participate may also be influenced by perceptions of who engages in MBTs [75]. Systematic reviews such as this one are critical for identifying groups for which evidence is lacking and guiding areas of future research to fill these gaps [76]; additional research successfully employing strategies for recruiting more diverse samples is sorely needed.
We also observed inconsistent reporting of interoception results (e.g., total scores only; medians rather than means), and therefore several studies could not be analyzed in all parts of the meta-analyses. Due to power limitations, we were unable to examine potential moderators of effects, which would provide additional important information about for whom these treatments are most effective in improving interoception and reducing pain. All studies included in the analyses used the MAIA as a measure of interoceptive awareness. Although the MAIA has been validated across many populations, some studies show that the Not-Distracting and Not-Worrying factors are only weakly associated with the other six MAIA subscales, and thus researchers could consider excluding those subscales from assessments of “pure interoception” [77]. Additionally, although the MAIA has been translated into 30 languages, some translated versions have failed to demonstrate the 8-factor model and have instead found a reduced number of factors [e.g., 78]. Thus, we must ensure that measures used in cross-cultural studies capture the same construct, as one’s cultural background could influence the way individuals respond to the same questions. Lastly, the MAIA is only a measure of interoceptive awareness and does not measure other aspects of interception. Research has not assessed changes in other aspects of interoception such as interoceptive accuracy, for which pain populations have demonstrated a significant deficit [28]. Thus, whether MBTs improve patients’ interoceptive accuracy remains largely unknown, indicating a major gap in the literature.
Additionally, it is critical to note that although change in interoception is presumed to be a mechanism of change in MBTs for pain conditions, no studies in this review analyzed interoceptive changes as a mediator between treatment and pain outcomes, which is an important step in identifying true mechanisms [4]. More research is needed to determine whether changes in interoception actually lead to pain reduction (i.e., whether it is truly a mechanism of change or just an ancillary construct that changes in response to MBTs but does not actually explain patients’ improvements in pain).
Overall, MBTs were associated with increased interoceptive awareness as well as reductions in pain. Examining changes in interoception is an important initial step in understanding how MBTs might bring about clinical change, which can inform efforts to further optimize treatments for chronic pain patients. However, additional studies with appropriate statistical techniques to test interoception as a mechanism of change (i.e., mediation analyses) are needed. Thus, while the results presented here are promising and interoceptive factors are purported to be a key mechanism of these interventions, research in this area is still relatively limited.
Finally, given the increasing recognition of interoception as a transdiagnostic factor in myriad mental and physical health conditions [79, 80], the present findings provide important insight and considerations for the field of behavioral medicine more broadly. Our results suggest that interoceptive awareness warrants additional consideration as a potential therapeutic mechanism in other MBTs focused on pain and perhaps as well on interventions focused on other targets, such as eating disorders, obesity, inflammation, and stress.
Overall, based on the findings and gaps in the literature identified by the present systematic review, several suggestions for future research include: (i) use more rigorous study designs (i.e., RCTs) and larger sample sizes that are adequately powered to detect significant effects; (ii) examine changes in different facets of interoception, such as interoceptive accuracy (e.g., heartbeat perception tasks); (iii) studies that include the MAIA should a) use the most updated version (MAIA-2) [17], and b) report changes in the eight subscales, rather than just total scores, to facilitate a more comprehensive understanding of changes in interoceptive awareness; (iv) statistically test interoception as a mechanism of change in MBTs; (v) increase transparency of racial and ethnic identities of participants and recruit more diverse samples; and (vi) work towards a consensus on the operationalization and measurement of interoception for use across scientific disciplines to help limit contradictions and confusion in the literature.
References
Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults — United States, 2016. MMWR. 2018;67:1001–6.
Mehling WE. If it all comes down to bodily awareness, how do we know? Assessing bodily awareness Kinesiol Rev. 2020;9:254–60.
Rivest-Gadbois E, Boudrias M-H. What are the known effects of yoga on the brain in relation to motor performances, body awareness and pain? A narrative review Complement Ther Med. 2019;44:129–42.
Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol. 2007;3:1–27.
Apkarian AV, Baliki MN, Geha PY. Towards a theory of chronic pain. Prog Neurobiol. 2009;87:81–97.
Yong RJ, Mullins PM, Bhattacharyya N. Prevalence of chronic pain among adults in the United States. Pain. 2022;163:e328–32.
Dueñas M, Ojeda B, Salazar A, et al. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457–67.
Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13:715–24.
Greenberg EN. The consequences of chronic pain. J Pain Palliat Care Pharmacother. 2012;26:64–7.
Niv D, Kreitler S. Pain and quality of life. Pain Pract. 2001;1:150–61.
Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: A systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2015;162:276–86.
Ehde DM, Dillworth TM, Turner JA. Cognitive-Behavioral Therapy for individuals with chronic pain. Am Psychol. 2014;69:153–66.
McCracken LM, Vowles KE. Acceptance and Commitment Therapy and mindfulness for chronic pain. Am Psychol. 2014;69:178–87.
Shipton EA. Physical therapy approaches in the treatment of low back pain. Pain Ther. 2018;7:127–37.
Craig AD. Interoception: The sense of the physiological condition of the body. Curr Opin Neurobiol. 2003;13:500–5.
Craig AD. How do you feel - now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10:59–70.
Garfinkel SN, Seth AK, Barrett AB, et al. Knowing your own heart: Distinguishing interoceptive accuracy from interoceptive awareness. Biol Psychol. 2015;104:65–74.
Calì G, Ambrosini E, Picconi L, et al. Investigating the relationship between interoceptive accuracy, interoceptive awareness, and emotional susceptibility. Front Psychol. 2015;6:1202.
Farb N, Daubenmier J, Price CJ, et al. Interoception, contemplative practice, and health. Front Psychol. 2015;6:763.
Mehling W. Differentiating attention styles and regulatory aspects of self-reported interoceptive sensibility. Philos Trans R Soc Lond B Biol Sci. 2016;371:20160013.
Mehling WE, Price C, Daubenmier JJ, et al. The Multidimensional Assessment of Interoceptive Awareness (MAIA). PLoS ONE. 2012;7:e48230.
Mehling WE, Acree M, Stewart A, Silas J, Jones A. The Multidimensional Assessment of Interoceptive Awareness, Version 2 (MAIA-2). PLoS ONE. 2018;13:e0208034.
Katkin ES, Morell MA, Goldband S, et al. Individual differences in heartbeat discrimination Psychophysiol. 1982;19:160–6.
Schandry R. Heart beat perception & emotional experience. Psychophysiol. 1981;18:483–8.
Whitehead WE, Drescher VM, Heiman P, et al. Relation of heart rate control to heartbeat perception. Biofeedback Self-Regul. 1977;2:371–92.
Zamariola G, Maurage P, Luminet O, et al. Interoceptive accuracy scores from the heartbeat counting task are problematic. Biol Psychol. 2018;137:12–7.
Mehling WE, Wrubel J, Daubenmier JJ, et al. Body awareness: A phenomenological inquiry into the common ground of mind-body therapies. Philos Ethics Humanit Med. 2011;6:6.
Di Lernia D, Serino S, Riva G. Pain in the body. Altered interoception in chronic pain conditions: A systematic review. Neurosci Biobehav Rev. 2016;71:328–41.
Schmitz N, Napieralski J, Schroeder D, et al. Interoceptive sensibility, alexithymia, and emotion regulation in individuals suffering from fibromyalgia. Psychopathol. 2021;54:144–9.
Valenzuela-Moguillansky C, Reyes-Reyes A, Gaete MI. Exteroceptive and interoceptive body-self awareness in fibromyalgia patients. Front Hum Neurosci. 2017;11:117.
Di Lernia D, Lacerenza M, Ainley V, et al. Altered interoceptive perception and the effects of interoceptive analgesia in musculoskeletal, primary, and neuropathic chronic pain conditions. J Pers Med. 2020;10:201.
Ceunen E, Vlaeyen JWS, Diest IV. On the origin of interoception. Front Psychol. 2016;7:743.
Gedney JJ, Logan H. Perceived control and negative affect predict expected and experienced acute clinical pain: A structural modeling analysis. Clin J Pain. 2007;23:35.
Tang J, Gibson SJ. A psychophysical evaluation of the relationship between trait anxiety, pain perception, and induced state anxiety. J Pain. 2005;6:612–9.
Wiech K, Ploner M, Tracey I. Neurocognitive aspects of pain perception. Trends Cogn Sci. 2008;12:306–13.
Mehling W, Daubenmier J, Price, et al. Self-reported interoceptive awareness in primary care patients with past or current low back pain. J Pain Res. 2013:403.
Cioffi D, Holloway J. Delayed costs of suppressed pain. J Pers Soc Psychol. 1993;64:274–82.
Johnson MH. How does distraction work in the management of pain? Curr Pain Headache Rep. 2005;9:90–5.
Prins B, Decuypere A, Damme SV. Effects of mindfulness and distraction on pain depend upon individual differences in pain catastrophizing. Eur J Pain. 2014;18:1307–15.
De Peuter S, Diest IV, Vansteenwegen D, et al. Understanding fear of pain in chronic pain: Interoceptive fear conditioning as a novel approach. Eur J Pain. 2011;15:889–94.
Garfinkel M, Schumacher HR. Yoga Rheum Dis Clin N Am. 2000;26:125–32.
American Psychological Association (APA). Mind-body intervention. n.d.
Rice BI. Mind-body interventions. Diabetes Spectr. 2001;14:213–2017.
Grant JA, Courtemanche J, Duerden EG, et al. Cortical thickness and pain sensitivity in zen meditators: Mindfulness training and emotion regulation. Emot. 2010;10:43–53.
Villemure C, Ceko M, Cotton VA, et al. Insular cortex mediates increased pain tolerance in yoga practitioners. Cereb Cortex. 2014;24:2732–40.
Williams JMG. Mindfulness and psychological process Emot. 2010;10:1–7.
Cramer H, Lauche R, Haller H, et al. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013;29:450–60.
Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan—A web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Haller H, Lauche R, Cramer H, et al. Craniosacral therapy for the treatment of chronic neck pain: A randomized sham-controlled trial. Clin J Pain. 2016;32:441–9.
Price CJ, Thompson EA. Measuring dimensions of body connection: body awareness and bodily dissociation. J Altern Complement Med. 2007;13:945–53.
Tran US, Birnbaum L, Burzler MA, et al. Self-reported mindfulness accounts for the effects of mindfulness interventions and nonmindfulness controls on self-reported mental health: A preregistered systematic review and three-level meta-analysis of 146 randomized controlled trials. Psychol Bull. 2022;148:86–106.
Sterne JAC, Savović J, Page MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ Online. 2019;366: l4898.
Evans S, Fernandez S, Olive L, et al. Psychological and mind-body interventions for endometriosis: A systematic review. J Psychosom Res. 2019;124:109756.
Lipsey MW, Wilson DB. Practical meta-analysis. Reprinted. CA: Sage; 2006.
Becker BJ. Synthesizing standardized mean-change measures. Br J Math Stat Psychol. 1988;41:257–78.
Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
JASP Team. JASP (Version 0.17) [Computer software] 2023.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48.
Lauche R, Stumpe C, Fehr J, et al. The effects of Tai Chi and neck exercises in the treatment of chronic nonspecific neck pain: A randomized controlled trial. J Pain. 2016;17:1013–27.
Lauche R, Wayne P, Fehr J, et al. Does postural awareness contribute to exercise-induced improvements in neck pain intensity? A secondary analysis of a randomized controlled trial evaluating Tai Chi and neck exercises. Spine. 2017;42:1195–200.
Osypiuk K, Ligibel J, Giobbie-Hurder A, et al. Qigong mind-body exercise as a biopsychosocial therapy for persistent post-surgical pain in breast cancer: A pilot study. Integr Cancer Ther. 2020;19:1534735419893766.
Ahmadi H, Adib H, Selk-Ghaffari M, et al. Comparison of the effects of the Feldenkrais method versus core stability exercise in the management of chronic low back pain: A randomised control trial. Clin Rehabil. 2020;34:1449–57.
Shim M, Johnson RB, Gasson S, et al. A model of dance/movement therapy for resilience-building in people living with chronic pain. Eur J Integr Med. 2017;9:27–40.
Roberts RL, Ledermann K, Garland EL. Mindfulness-oriented recovery enhancement improves negative emotion regulation among opioid-treated chronic pain patients by increasing interoceptive awareness. J Psychosom Res. 2022;152:110677.
Berry MP, Lutz J, Schuman-Olivier Z, et al. Brief self-compassion training alters neural responses to evoked pain for chronic low back pain: A pilot study. Pain Med. 2020;21:2172–85.
Paolucci T, Zangrando F, Iosa M, et al. Improved interoceptive awareness in chronic low back pain: A comparison of Back school versus Feldenkrais method. Disabil Rehabil. 2017;39:994–1001.
Zangrando F, Piccinini G, Tagliolini C, et al. The efficacy of a preparatory phase of a touch-based approach in treating chronic low back pain: A randomized controlled trial. J Pain Res. 2017;10:941–9.
de Jong M, Lazar SW, Hug K, et al. Effects of Mindfulness-Based Cognitive Therapy on body awareness in patients with chronic pain and comorbid depression. Front Psychol. 2016;7:967.
von Hippel PT. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med Res Methodol. 2015;15:35.
Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Ann Behav Med. 2017;51:199–213.
Garland EL, Brintz CE, Hanley AW, et al. Mind-body therapies for opioid-treated pain: A systematic review and meta-analysis. Arch Intern Med. 2020;180:91–105.
Oh SS, Galanter J, Thakur N, et al. Diversity in clinical and biomedical research: A promise yet to be fulfilled. PLoS Med. 2015;12:e1001918.
Passmore SR, Kisicki A, Gilmore-Bykovskyi A, et al. “There’s not much we can do…” Researcher-level barriers to the inclusion of underrepresented participants in translational research. J Clin Transl Sci. 2022;6:e4.
Park CL, Braun T, Siegel T. Who practices yoga? A systematic review of demographic, health-related, and psychosocial factors associated with yoga practice. J Behav Med. 2015;38:460–71.
Johnson BT, Hennessy EA. Systematic reviews and meta-analyses in the health sciences: Best practice methods for research syntheses. Soc Sci Med. 1982;2019(233):237–51.
Ferentzi E, Olaru G, Geiger M, et al. Examining the factor structure and validity of the Multidimensional Assessment of Interoceptive Awareness. J Pers Assess. 2021;103:675–84.
Shoji M, Mehling WE, Hautzinger M, et al. Investigating Multidimensional Interoceptive Awareness in a Japanese population: Validation of the Japanese MAIA-J. Front Psychol. 2018;9:1855.
Herbert BM, Pollatos O, Klusmann V. Interoception and health. Eur J Health Psychol. 2020;27:127–31.
Quadt L, Critchley HD, Garfinkel SN. Interoception and emotion: Shared mechanisms and clinical implications. In Tsakiris, De Preester, editors. The interoceptive mind: From homeostasis to awareness. Oxford University Press; 2018, p. 123–43.
Funding
This work was supported by the National Institutes of Health F31AT012315 to KEG.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
For this type of study formal consent is not required.
Informed Consent
For this type of study formal consent is not required.
Research Involving Human Participants and/or Animals
This article does not contain any studies conducted with human participants by any of the authors.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gnall, K.E., Sinnott, S.M., Laumann, L.E. et al. Changes in Interoception in Mind-body Therapies for Chronic Pain: A Systematic Review and Meta-Analysis. Int.J. Behav. Med. (2024). https://doi.org/10.1007/s12529-023-10249-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s12529-023-10249-z