Abstract
Background
Youth who face adversity are at a disproportionate risk for poor sleep health across the life course. Identifying whether the association between adversity and poor sleep varies based upon age and sex is needed. This study aims to explore sex and age as moderators between social risk and sleep in a sample of U.S. youth.
Methods
This study analyzed data of 32,212 U.S. youth (6–17 years) whose primary caregiver participated in the 2017–2018 National Survey of Children’s Health. A social cumulative risk index (SCRI) score was calculated from 10 parental, family, and community risk indicators. Nighttime sleep duration was the number of hours the child slept during the past week. Weeknight sleep irregularity was operationalized as whether the child sometimes/rarely/never went to bed at the same time. Generalized logistic regression models estimated associations between SCRI and sleep duration/irregularity, with age and sex as moderators.
Results
Age moderated the association between SCRI and short sleep (OR = 1.12, p < 0.001), such that the magnitude of the SCRI-sleep relationship was 12% greater in school-age children. Sex was not a significant moderator. In stratified models by age group, age was positively associated with short sleep in both groups, with a greater magnitude in school-age children. Female school-age children were less likely to have short sleep than males.
Conclusions
Younger children with greater social cumulative risk factors may be more vulnerable to short sleep duration. Further research into the mechanisms underlying the relationships between social risk and sleep health in school-age children is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nine in every ten children and adolescents (6-17 years) in the United States (U.S.) do not get sufficient sleep for their age. Moreover, approximately 50% have an irregular (or variable) sleep schedule that reduces overall sleep quality [1]. Poor sleep health (i.e., inadequate sleep duration, sleep irregularity, poor sleep quality) in childhood and adolescence weakens age-appropriate cognitive [2], socio-emotional [3], and physical development [4], and predicts poor health [5] and greater risk of death and disability in adulthood [6]. Importantly, sleep deprivation (i.e., obtaining inadequate sleep duration) is disproportionately represented in youth who face adversity. Specifically, adolescents who are a member of an ethnic or minority group, live in a family experiencing socioeconomic disadvantage, live in an unsafe neighborhood or have a parent with low educational status and/or poor mental health have an increased likelihood of inadequate sleep [7,8,9].
Youth is a critical window of opportunity to circumvent the negative effects of poor sleep health in at-risk populations across the lifespan [6, 10]. A necessary preliminary step in this feat is identifying whether the association between adversity and poor sleep health varies based upon age and sex, so that particularly vulnerable groups are prioritized in future sleep interventions. To this end, the present study aimed to explore sex and age as moderators between social risk and sleep duration/irregularity in a U.S. sample of youth aged 6–17 years.
Social Cumulative Risk and Sleep
The Cumulative Risk Model [11] proposes that children who experience a greater number of risk factors at multiple levels, including individual (e.g., discrimination due to membership of socially constructed racial and ethnic minority groups) [8, 12], caregiver (e.g., mental health symptoms, educational level) [13], family (e.g., low-income, conflict, parenting stress, lack of support) [14,15,16] and community (e.g., unsafe neighborhood) [17] levels, have an increased likelihood of developing poor sleep health and negative health outcomes [6, 17]. There is a lack of consensus surrounding which and how many factors should be included in cumulative risk models, however, most incorporate multi-level factors. The conceptual framework suggests that the more social risk factors a child encounters, the more overwhelmed their stress-response system becomes, and the less likely they are able to maintain their bioregulatory systems, such as sleep [18]. The cumulative risk perspective posits the necessity of using composite risk scores that capture distal and proximal levels of risk, versus examining singular risk factors when testing the association between social risk and health outcomes such as sleep deprivation [11, 13, 14]. Similarly, it highlights the consideration of additive risk versus risk clusters, as the number of risk factors may pose more of a risk to developmental outcomes than co-occurring risks [18].
Cross-sectional studies conducted among toddler [19], preschool [20] and school-age children [21] have found that cumulative social risk integrating caregiver (e.g., marital, educational and employment status) and family (e.g., household poverty and stress) factors are associated with decreased actigraphy-derived sleep duration [21] and parent report of child sleep problems [19, 20]. Similarly, in a cross-sectional study of preschoolers, each additional social cumulative risk factor (including distressed neighborhood) was associated with a 9–18% increased likelihood of a caregiver reported sleep concern (e.g., poor sleep health habits, pediatric insomnia and obstructive sleep apnea symptoms) [13]. Longitudinal evidence has also highlighted that childhood adversities (e.g., parental loss and adjustment, child maltreatment and exposure to violence) predicts sleep disturbances in youth [22]. These studies point to the necessary consideration of multiple risk factors when assessing the association between social risk and child sleep deprivation.
The Contribution of Sex and Age to Sleep Deprivation in Youth
A necessary next step in the exploration of cumulative risk and sleep deprivation is the consideration of whether such associations may vary based on age and sex. Prior research that has examined the contribution of age and sex to sleep deprivation among at-risk populations have reported mixed results. For example, among adolescents from families who face adversity, some studies have found shorter sleep duration in males [23], while others have found shorter sleep duration in females [24]. In terms of age, the risk for short sleep duration has been found to increase with increasing age in populations who are of low socioeconomic status and non-White [12, 24,25,26].
There are a broader range of studies that examined sex and age in association with sleep deprivation using large, national datasets representative of the general U.S. population, with consistent findings described above among at-risk samples. For sex, adolescent females have been found to have shorter sleep duration compared to males [27,28,29]. In terms of age, most national studies found older children to be at greater risk for short sleep duration, compared to their younger counterparts [29,30,31]. It is important to note that developmentally, sleep duration needs decrease with age. The American Academy of Sleep Medicine (AASM) recommends that school-age children obtain 9–12 h of sleep, and adolescents obtain 8–10 h of sleep per 24 h to promote optimal health [32]. Yet, prior research indicates that school-age children and adolescents alike are not obtaining these recommended durations, with adolescents being at a greater risk for short sleep than school-age children [1]. Elucidating age and sex differences in sleep health may provide insight into the role of sleep deprivation in population health disparities [10, 33].
Sleep Irregularity in Youth
An independent predictor of sleep deprivation is sleep irregularity, which is not as extensively studied as sleep duration in the sleep health literature [34]. Going to bed within one hour of the prior night’s bedtime on a nightly basis is crucial to development, as it helps with circadian alignment and the ability to obtain adequate nightly sleep duration [34]. Consideration of sleep irregularity is particularly pressing among adolescents, who experience a delayed sleep phase in conjunction with puberty [35, 36], resulting in later bedtimes and a desire for later wake times [37]. However, early school start times decrease the feasibility of later waketime, resulting in shorter sleep duration [38]. Amplifying this delayed circadian phase are environmental factors including less parental oversight of bedtime, increased academic load, excessive nighttime technology use, work and social obligations [39]. Furthermore, the biology of the human brain changes significantly during adolescence. The most marked decline in non-rapid eye movement (NREM) sleep (i.e., restorative sleep phase as detected by electroencephalogram [EEG]) that allows the body to enter a deep sleep and feel more rested in the morning, occurs in adolescence versus any other time in the life course [40]. These maturational changes in sleep brain waves coupled with irregular sleep schedules position adolescents to obtain inadequate and poor-quality sleep [40].
The “24/7” lifestyle of adolescence [41], makes this developmental stage particularly vulnerable to sleep irregularity [24, 42]. Alarmingly, recent data suggests that sleep irregularity may be a stronger prognostic indicator of poor health in young adults than sleep duration [43]. Moreover, the examination of sleep irregularity is particularly pressing among at-risk populations, who may face barriers such as working multiple jobs, shift-work or room sharing due to overcrowding, all of which may inhibit sleep regularity [44].
Given this under-studied sleep metric, few studies have examined sex and age in association with sleep irregularity. Those that have, found no significant association between sex and sleep irregularity [33, 45] nor age and sleep irregularity [14, 34]. Further examination of these associations and characterization of sleep health, beyond the more common sleep duration metric, is a public health priority [10].
Current Study
Improving sleep health in children and adolescents from families facing adversities could have a profound effect on improving health across the lifespan and ameliorating health disparities [10]. Limiting the potential to improve sleep health in populations experiencing adversities, is a lack of consideration of social risk and sleep health as multidimensional domains, as well as poor understanding about the extent to which age and sex may modify the association of social risk on multiple dimensions of sleep health [10, 33]. To address these gaps, this study used a social cumulative risk measure [46, 47] that encompassed caregiver, family and community factors among a nationally representative U.S. sample of children and adolescents. Moreover, this study considered the sleep health metrics of duration as well as irregularity. The aim of this study was to identify whether the association between social risk and sleep duration/irregularity varied based on the age and sex of youth. The study hypothesis was that age and sex would be significant moderators such that the relationship between cumulative risk and short sleep duration would be greater in adolescents versus school-age children and in females versus males. This hypothesis was based on prior findings in national samples, since studies examining sex differences in at-risk samples had small sample sizes [n = 246 [23], n = 500 [24]]. Additionally, an alternative hypothesis was that age and sex will not moderate the association between social cumulative risk and sleep irregularity, given that current research has found insignificant direct associations between these variables [14, 33, 34, 45].
Methods
Participants and Procedures
Data were obtained from the National Survey of Children’s Health (NSCH) 2017–2018 combined dataset, available from the Health Resources and Services Administration’s Maternal and Child Health Bureau (HRSA MCHB) and the U.S. Census Bureau (https://www.childhealthdata.org) [48]. The NSCH is the largest national-level and state-level survey with data on the well-being of children and adolescents aged 0–17 years, as well as the health care needs of their families and communities in the U.S. Participants were drawn from a sample of households from the Census Master Address File across 50 states and the District of Columbia. Selection of households were stratified by state, neighborhood poverty and child presence, with one child randomly selected from multiple children households [48]. Primary caregivers completed questions about the child’s mental and physical health, insurance coverage and characteristics of the child’s family and neighborhood [48].
Using cross-sectional design, this secondary data analysis included a nationally representative sample of 32,212 children aged 6–17 years who had complete data on sleep duration, sleep regularity and social cumulative risk indicators. The mean age of participants was 12.13 years (SD = 3.45), and nearly half (48.90%) were female. Eighty-two percent of participants reported at least one social risk factor, such as non-White (51.73%), parental education level ≤ high school (26.74%), family income below 200% FPL (Federal Poverty Line: 39.21%), and living in an unsafe neighborhood (28.50%). There were no significant differences in age and daily activity levels, but there were sex and resilience differences between participants with (n = 32,212) and without (n = 4,785) complete data. These variables were adjusted for in analyses. The proportion of non-White race was higher in participants without complete data.
Measures
Social Cumulative Risk Index
Larson et al. created a social cumulative risk index (SCRI) consisting of eight social risk variables present in the 2003 NSCH dataset, and found that children with more than six social risk factors were 17.31 times more likely to be of poorer health compared to those with no risk factors [46]. More recently, Yang and colleagues amended the SCRI by including two additional social risks factors (related to parenting) using 2011–2012 NSCH dataset [47]. To date, the SCRI has not been examined using NSCH data with sleep as an outcome, yet it aligns with other cumulative risk indexes used in association with sleep [17].
Thus, in line with Yang et al. [47], 10 social risk variables were dichotomized as follows: (1) Household Education (1 = ≤ high school education, 0 = > high school education); (2) Family Income (1 = ≤ 200% FPL, 0 = ≥ 200% FPL: calculated as the ratio of total family income and the family poverty threshold, and reported as a rounded percentage [48]); (3) High Level of Parent Aggravation (1 = one or more ‘usually/always’ responses to three forms of stress [child much harder to care for than most children, parent feeling anger with the child, and child does things that bothers the parent], 0 = no ‘usually/always’ response; (4) Racial and Ethnic Minority Group Membership (1 = non-White, 0 = White). Of note, race and ethnicity are social constructs that consider social groupings made up of cultural and societal practices, norms, values, and belief systems (12); (5) Children’s Health Insurance (1 = currently uninsured, 0 = currently insured); (6) Poor Coping with Parenting Demands (1 = ‘not well at all/not well/somewhat well’, 0 = ‘very well’); (7) Suboptimal Maternal Mental Health Status (1 = ‘poor/fair/good’, 0 = ‘very good/excellent’); (8) No Social Support (1 = not having someone to turn to for emotional support regarding parenting, 0 = having someone); (9) Domestic Violence (1 = child seeing parental violence, 0 = not seeing parental violence); (10) Neighborhood Safety (1 = ‘never/sometimes safe’, 0 = ‘usually/always safe’) [47].
A SCRI score was calculated for each child by summing all 10 dichotomized social risk factors. For each risk factor, if the risk was present the child received a ‘1’ and if it was not present, the child received a ‘0’. Possible scores ranged from 0–10, suggesting the number of social risk factors each child had [47].
Sleep Duration
Sleep duration was obtained by parent-report to the question “During the past week, how many hours of sleep did this child get during an average day (counting both nighttime sleep and naps)?”. Responses for this question were separated into seven categories: 1 = less than 7 h, 2 = 7 h, 3 = 8 h, 4 = 9 h, 5 = 10 h, 6 = 11 h, and 7 = 12 or more hours. HRSA MCHB then dichotomized sleep duration to determine whether children were getting age-appropriate recommended sleep duration, based on AASM guidelines (1 = child sleeps the recommended age-appropriate hours on most weeknights, 2 = child sleeps less than recommended age-appropriate hours on most weeknights) [48].
Sleep Irregularity
Sleep irregularity was obtained by parent-report of “How often does this child go to bed at about the same time on weeknights?” Responses for this question were separated into five categories: 1 = always, 2 = usually, 3 = sometimes, 4 = rarely, 5 = never. Sleep irregularity was characterized by whether the child went to bed “sometimes/rarely/never” about the same time each weeknight [49].
Covariates
Covariates were chosen based on published literature and available variables in the dataset [23, 34, 42]. Specifically, physical activity was controlled for given its association with sleep duration and sleep regularity [23, 34]. Physical activity was obtained by parent answers to the question “During the past week, on how many days did this child exercise, play a sport, or participate in physical activity for at least 60 min?” Responses to this question were separated into 4 categories: 1 = 0 days, 2 = 1–3 days, 3 = 4–6 days, 4 = every day.
Family resilience was included as a covariate given its protective effect on family social risk [13], and its positive association with sleep [42, 50]. Family resilience was a composite measure based on responses to the following four survey items: “When your family faces problems, how often are you likely to do each of the following?”: (a) Talk together about what to do, (b) Work together to solve our problems, (c) Know we have strengths to draw on, (d) Stay hopeful even in difficult times. Response options to the four items are 1 = none of the time, 2 = some of the time, 3 = most of the time, or 4 = all of the time. Family resilience was then dichotomized into answering “all or most of the time” to all 4 survey items (optimal), versus answering “all or most of the time” to only 0–3 items (suboptimal).
Statistical Analysis
Stata 16 (svy package) was used to conduct data analysis, with adjustments for complex stratified survey design (cluster: household, stratum: state) and sampling weights. Sample characteristics were summarized using weighted means and percentages. At the bivariate level, SCRI and sample characteristics were compared between the sleep groups (sufficient vs. short, regular vs. irregular) using Chi-square and Mann–Whitney U tests. Accounting for age, sex, physical activity, and family resilience, two logistic regression models estimated the association of SCRI (independent variable) with short sleep and irregular sleep (dependent variables), respectively. Next, interaction terms between [1] SCRI and age groups (NSCH classification: 1 = children aged 6–11 years, 2 = adolescents aged 12–17 years) [51, 2] SCRI and sex (1 = males, 2 = females) were added into the models separately to test the moderating effect of age and sex. Wald test was performed to examine the interaction terms, with p < 0.05 indicating a significant interaction. Additionally, the Archer Lemeshow goodness-of-fit statistic was used under complex sampling to test the overall model fit, with p > 0.05 indicating a good fit. Significant interactions were further examined and illustrated using Stata's margins plots command.
Given the unique developmental changes in childhood and adolescence, we repeated analyses in subsamples of children and adolescents, respectively. Age was used as a continuous variable in these stratified multivariate models. All test values were 2-sided, with the significance level set at α = 0.05.
Results
One-third of children and adolescents slept shorter than recommended age-appropriate hours; however, most participants always/usually went to bed at the same time on weeknights (87.57%). Table 1 shows counts and weighted percentages of sample characteristics by sleep groups. A greater proportion of adolescents than children reported irregular sleep (16.34% vs. 7.45%, respectively; χ2 = 606.59, p < 0.001). Short sleepers (2.54 ± 1.64 vs. 1.93 ± 1.63, z = -26.70, p < 0.001) and irregular sleepers (2.96 ± 1.74 vs. 2.03 ± 1.62, z = -30.12, p < 0.001) had significantly greater mean SCRI scores compared with those who had sufficient and regular sleep. Figure 1 shows the distribution of SCRI over sleep groups. In terms of individual SCRI factors, children who were non-White or lacked health insurance reported higher proportions of short and irregular sleep (p’s < 0.05) compared with their counterparts.
Distribution of Social Cumulative Risk Index (SCRI) Scores in Sleep Groups (Weighted Values). Note. Lines across the box indicate the median, and error bars show upper and lower whiskers adjacent values. Dots reflect outliers which were kept in analyses since their removal yielded similar results. The mean SCRI scores were significantly higher in short and irregular sleepers
For household SCRI factors, children whose families had income < 200% FPL, lived in an unsafe neighborhood, received ≤ a high school education, lacked social support, experienced high levels of parental aggravation or domestic violence, and whose mother had suboptimal mental health and poor coping also had a higher proportion of short and irregular sleep (p’s < 0.05) (Table 1). As shown in Table 2, the differences in SCRI scores remained statistically significant in logistic regression models on short and irregular sleep, controlling for age, sex, physical activity, and family resilience. Specifically, each point increase in SCRI was associated with a 16% and 25% increase in the odds of short sleep (OR = 1.16, p < 0.001) and irregular sleep (OR = 1.25, p < 0.001), respectively.
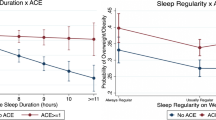
Age was a significant modifier of the association between SCRI and short sleep (OR = 1.12, p < 0.001) but not SCRI and irregular sleep (OR = 0.98, p = 0.72) (Table 2, Model 2). Specifically, the average magnitude of the relationship between SCRI scores and short sleep was 12% greater in school-age children than adolescents. The margins plot (Fig. 2) shows the marginal effects of age on sleep with 95% confidence intervals when SCRI scores were held constant at different values. The probability of having short sleep was greater in school-age children, especially when SCRI was ≥ 2, and the gap between age groups became larger with increasing SCRI scores.
Interaction Between SCRI Scores and Age Groups on Short Sleep. Note. The margins plot is derived using the Margins command in Stata based on logistic regression with complex survey design. The x-axis is the SCRI score and the y-axis is the probability of short sleep. Error bars show upper and lower whiskers adjacent values
The Archer-Lemeshow test suggests that models were a good fit for the data (p > 0.05) and adding the interaction term between age and SCRI showed a statistically significant improvement in the logistic regression model fit predicting short sleep (Wald test, p < 0.05). There was no significant interaction between sex and SCRI on short sleep or irregular sleep (p > 0.05). In logistic regression models, children and adolescents who did exercise (> 60 min) at least one day per week (versus no exercise) and those from families with optimal resilience (versus suboptimal resilience) tended to have decreased odds of short sleep and irregular sleep (p < 0.05).
Table 3 shows results of the sensitivity analyses. The associations between SCRI and short or irregular sleep in children (6–11 years old) and adolescents (12–17 years old) were consistent with the interaction analyses using the whole sample. Whereas the relationship between SCRI and short sleep was stronger in children (OR = 1.31, p < 0.001) than adolescents (OR = 1.13, p < 0.001), associations between SCRI and irregular sleep were similar between age groups (OR = 1.30, p’s < 0.05). Female sex (versus male sex) was associated with lower odds of short sleep in children (OR = 0.84, p = 0.04) but not adolescents (OR = 1.06, p = 0.56). Neither age (continuous variable) nor sex significantly modified the SCRI-sleep relationship in children and adolescents (p > 0.05, data not presented in table), respectively.
Discussion
Bivariate findings indicated that families with social risks had a higher proportion of children who achieved short and/or irregular sleep. Results of the moderation analyses showed age as a significant moderator of the association between SCRI and short sleep, such that the magnitude of the SCRI-sleep relationship was greater in school-age children compared to adolescents. Age did not significantly moderate the association between SCRI and sleep irregularity. Finally, sex was not a significant moderator of the association between SCRI and sleep duration nor sleep irregularity. These moderation findings were supported by the sensitivity analyses with the magnitude of the SCRI-sleep relationship remaining greater in school-age children versus adolescents. A unique finding of the stratified analysis was female children having a decreased risk for short sleep than their male counterparts.
The Role of Sex and Age on Sleep in Youth
For the sleep duration outcome, our main results did not support the a priori hypothesis. The primary study hypothesis was that the relationship between cumulative risk and short sleep duration would be greater in adolescents versus school-age children and females versus males. Instead, the main findings and sensitivity analysis revealed the association between SCRI and short sleep duration was greater in school-age children versus adolescents. Further, the stratified analysis found that female children (not adolescents) had lower odds of short sleep duration compared to male children. These findings are contradictory to the current literature. In nationally representative German samples, no sex differences were found in child sleep duration [26, 52]. Whereas among nationally representative U.S. samples of adolescents, greater odds of shorter sleep duration were reported in females versus males [24, 29]. This discordance in findings warrants further exploration of the underlying mechanisms between cumulative risk, sleep duration, and sex to identify at which developmental stage sex-related sleep disparities may emerge.
Similarly, our finding that the magnitude of the SCRI-sleep duration relationship was more pronounced in school-age children versus adolescents, was unexpected given current literature highlighting an increased risk of short sleep in older children [12, 31, 45]. Notably, however, in stratified analysis, older age was associated with greater odds of short sleep in children and adolescents, respectively (see Table 3), which aligns with current work [29,30,31]. Our novel finding that the relationship between SCRI and sleep duration is magnified in school-age children is supported by the Cumulative Risk Model. It is possible that young children are particularly vulnerable to the effects of social risk on short sleep, as adolescents may experience more protective factors, such as peer support, engagement in extracurricular activities, and better developed emotional regulation, that may make them more resilient against the cumulative effects of adversity on health outcomes [18, 53]. Given that the risk for sleep disparities begin in early childhood, this finding supports the implementation of sleep interventions starting in childhood [13, 44]. Indeed, sleep habits are established early in life and are often carried into adolescence and ultimately adulthood [5]. Therefore, sleep habits of school-age children may be more amenable than adolescents, and improving such habits may attenuate the association between cumulative risk and short sleep duration.
Our finding that the relationship between cumulative risk and sleep irregularity did not vary based on youth sex and age is consistent with the current literature finding no direct relationship between youth sex and sleep irregularity [33, 45], nor youth age and sleep irregularity [14, 34]. Our findings extend the current literature, however, by beginning to explore at-risk subgroups, based on age and sex, within a nationally representative U.S. sample. Our stratified analysis highlighted how when multivariate analyses were conducted in children and adolescents separately, increasing age was as a risk factor for sleep irregularity (see Table 3). This finding is timely, as sleep irregularity is emerging as an integral sleep health metric that may have worse developmental implications than short sleep duration [30, 33, 43, 45]. However, much of the extant research is based upon cross-sectional design [28, 30, 33, 45] and self-report [4, 28, 30], making this a continued gap with further research needed to explore objectively measured sleep irregularity using longitudinal design, especially among at-risk populations, where it may be particularly relevant [34].
Strengths and Limitations
The findings of our study must be interpreted in the context of its design and measurement limitations. The cross-sectional design inhibits the examination of casual relationships. The interplay between cumulative social and biological risk and child sleep duration/irregularity is likely dynamic and complex, requiring a variety of assessment methods completed over time [13]. Moreover, intraindividual differences cannot be examined across developmental trajectories, making it difficult to characterize longitudinal changes in sleep duration and irregularity [27]. Similarly, cross-sectional design prohibits the capture of general sleep trends across the week, weekdays versus weekends, or seasonality differences [26].
Regarding measurement limitations, using a single item to capture sleep duration and sleep irregularity limits construct variability and may impede its proper capture. Indeed, classifying sleep irregularity as the standard deviation in actigraphy or sleep diary captured sleep onset time over an extended period of time (including weekends) is more reliable than a one-item sleep regularity measure [34]. Capturing weeknight and weekend sleep is prudent in adolescents who are at risk for “social jetlag” that contributes to later sleep onset and waketimes on the weekends [30]. Additionally, relying on parental self-report and using subjective as opposed to objective measures of sleep, may contribute to shared method variance between sleep and cumulative risk [13]. Furthermore, parent-reported sleep data generally overestimate sleep duration and underestimate bedtime irregularity [30], and are subject to recall and/or social desirability bias [45]. This implies that most likely more than one-third of this nationally representative sample slept less than the recommended age-appropriate hours, and less than the majority of participants always/usually went to bed at the same time. Adolescence is a developmental period of independence and parents may be unaware of their child’s sleep patterns [1, 49]. Having adolescents self-report on their sleep duration/irregularity through validated measures is beneficial. Also, we did not examine long-sleepers separately due to how sleep duration was collected (i.e., we were unable to identify those who slept 12 h or more). In terms of the SCRI, classifying risk based on the number of risk factors across domains precludes the possibility of uncovering underlying mechanisms through examining possible synergistic or interactive effects among distal and proximal risk factors [18]. Moreover, future studies should examine the reliability and validity of the SCRI for capturing social risks in a nationally representative sample. Finally, missing values may influence the representativeness of study sample, which in turn, has an impact on the generalizability of study findings.
Despite the above limitations, there are major strengths of our study including the use of a large, U.S. dataset which increases the generalizability of our results. Additionally, using ten constructs to capture caregiver, family, and community risk factors, is a measurement strength and adds to the literature on disparate sleep outcomes. Finally, examining moderation in relation to sleep irregularity is novel and necessary, as it may be more amenable than duration to sleep intervention [34].
Future Research
Understanding temporal parameters (e.g., duration of risk exposure, age when exposed to risk) will elucidate the amplification of risk and possible underlying biological and psychological processes that account for social risk factors on sleep outcomes [18]. Similarly, examination of different clusters or combinations of risk factors in association with sleep outcomes may help inform interventions, as social factors deemed to pose the most risk may be targeted in addition to sleep habits [18]. Further decomposing the SCRI and examining social risks as moderators would help inform how different social advantages and disadvantages for different groups may interact with other social risk factors on sleep outcomes [13]. In terms of the examination of sex as a moderator, it would be worthwhile to explore if results remain when gender (e.g., self-identification as male or female) is studied. Finally, parallel to the consideration of risk factors, it is important to identify resilience factors that could protect against the development of short and irregular sleep throughout childhood and adolescence [13].
Conclusion
The established associations between adversity, poor sleep and subsequent development of health disparities across the life course highlights the critical need of addressing sleep in the most at-risk groups as a potential mechanism to ameliorate disparity development [10]. The current study explored whether the association between social risk and short sleep duration/irregularity varied based on age or sex among a U.S. sample. Age was a significant moderator of SCRI and short sleep, such that the magnitude of the association was greater in school-age children than adolescents. Age did not moderate the association between SCRI and sleep irregularity, and sex was also not a significant moderator. These findings highlight how school-age children with social cumulative risk factors are at risk for short sleep duration. This suggests that childhood represents a critical period for early intervention and prevention of short sleep duration. Focusing on ways to support children with multiple social risks prior to adolescence, may serve to prevent sleep, and ultimately, health disparities [10].
Data Availability
This manuscript uses secondary data from the publicly available dataset NSCH. Data and materials to replicate the findings here are available at the following URL: https://www.childhealthdata.org/help/dataset. The analytic code necessary to reproduce the analyses presented in this paper is available from the second author.
References
Buxton OM, Chang AM, Spilsbury JC, Bos T, Emsellem H, Knutson KL. Sleep in the modern family: Protective family routines for child and adolescent sleep. Sleep Health. 2015;1(1):15–27. https://doi.org/10.1016/j.sleh.2014.12.002.
Turnball K, Reid GJ, Morton JB. Behavioral sleep problems and their potential impact on developing executive function in children. Sleep. 2013;36(7):1077–84. https://doi.org/10.5665/sleep.2814.
Hysing M, Sivertsen B, Garthus-Niegel S, Eberhard-Gran M. Pediatric sleep problems and social-emotional problems. A population-based study. Infant Behav Dev. 2016;42:111–8. https://doi.org/10.1016/j.infbeh.2015.12.005.
Chaput J, Gray CE, Poitras VJ, et al. Systematic review of the relationships between sleep duration and health indicators in the early years (0–4 years). BMC Public Health. 2017;17(Suppl 5):91–107. https://doi.org/10.1186/s12889-017-4850-2.
Fernandez-Mendoza J, Calhoun SL, Puzino K, et al. Objective short sleep duration predicts the evolution of poor sleep into insomnia in the transition from childhood to young adulthood: The penn state child cohort. Sleep Med. 2019;64(1):S113. https://doi.org/10.1093/sleep/zsaa150.
Grandner MA, Hale L, Moore M, Patel NP. Mortality associated with short sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14:191–203. https://doi.org/10.1016/j.smrv.2009.07.006.
Schmeer KK, Tarrence J, Browning CR, Calder CA, Ford JL, Boettner B. Family contexts and sleep during adolescence. SSM Popul Health. 2019;7:004–4. https://doi.org/10.1016/j.ssmph.2018.11.004.
Guglielmo D, Gazmararian JA, Chung J, Rogers AE, Hale L. Racial/ethnic sleep disparities in US school-aged children and adolescents: A review of the literature. Sleep Health. 2018;4(1):68–80. https://doi.org/10.1016/j.sleh.2017.09.005.
Troxel WM, Shih RA, Ewing B, Tucker JS, Nugroho A, D’Amico EJ. Examination of neighborhood disadvantage and sleep in a multi-ethnic cohort of adolescents. Health Place. 2017;45:39–45. https://doi.org/10.1016/j.healthplace.2017.03.002.
Hale L, Troxel W, Buysse DJ. Sleep health: An opportunity for public health to address health equity. Annu Rev Public Health. 2020;41:81–99. https://doi.org/10.1146/annurev-publhealth-040119-094412.
Burchinal M, Vernon-Feagans L, Cox M, Key Family Life Project Investigators. Cumulative social risk, parenting, and infant development in rural low-income communities. Parent Sci Pract. 2008;8(1):41–69. https://doi.org/10.1080/15295190701830672.
Hawkins SS, Takeuchi DT. Social determinants of inadequate sleep in US children and adolescents. Public Health. 2016;138:119–26. https://doi.org/10.1016/j.puhe.2016.03.036.
Williamson AA, Mindell JA. Cumulative socio-demographic risk factors and sleep outcomes in early childhood. Sleep. 2020;43(3):1–13. https://doi.org/10.1093/sleep/zsz233.
El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt IA. Economic adversity and children’s sleep problems: Multiple indicators and moderation effects. Health Psychol. 2013;32(2):849–59. https://doi.org/10.1037/a0030413.
Jarrin DC, McGrath JJ, Quon EC. Objective and subjective socioeconomic gradients exist for sleep in children and adolescents. Health Psychol. 2014;33(3):301–5. https://doi.org/10.1037/a0032924.
Bernier A, Belanger M, Bordeleau S, Carrier J. Mothers, fathers, and toddlers: Parental psychosocial functioning as a context for young children’s sleep. Dev Psychol. 2013;49(7):1375–84. https://doi.org/10.1037/a0030024.
Singh GK, Kenney MK. Rising prevalance and neighborhood, social, and behavioral determinants of sleep problems in US children and adolescents, 2003–2012. Sleep Disorders. 2013;2013:1–15. https://doi.org/10.1155/2013/394320.
Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139(6):1342–96. https://doi.org/10.1037/a0031808.
Hash JB, Oxford ML, Fleming CG, Ward TM, Spieker SJ, Lohr MJ. Impact of a home-visiting program on sleep problems among young children experiencing adversity. Child Abuse Negl. 2019;89:143–54. https://doi.org/10.1016/j.chiabu.2018.12.016.
Alkon A, Boyce WT, Neilands TB, Eskenazi B. Children’s autonomic nervous system reactivity moderates the relations between family adversity and sleep problems in latino 5-year olds in the CHAMACOS study. Front Public Health. 2017;5:155. https://doi.org/10.3389/fpubh.2017.00155.
Bagley EJ, El-Sheikh M. Familial risk moderates the association between sleep and zBMI in Children. J Pediatr Psychol. 2013;38(7):775–84. https://doi.org/10.1093/jpepsy/jst031.
April-Sanders A, Duarte CS, Wang S, et al. Childhood adversity and sleep disturbances: Longitudinal results in puerto rican children. Int J Behav Med. 2021;28:107–15. https://doi.org/10.1007/s12529-020-09873-w.
Gillis B, Shimizu M, Philbrook LE, El-Sheikh M. Racial disparities in adolescent sleep duration: Physical activity as a protective factor. Cult Divers Ethn Minor Psychol. 2020;27(1):118–22. https://doi.org/10.1037/cdp0000422.
Miguez MJ, Bueno D, Perez C. Disparities in sleep health among adolescents: The role of sex, age and migration. Sleep Disorders. 2020:1–6. https://doi.org/10.1155/2020/5316364.
Tomfohr-Madsen L, Cameron EE, Dhillon A, et al. Neighborhood socioeconomic status and child sleep duration: A systematic review and meta-analysis. Sleep Health. 2020;6(5):550–62. https://doi.org/10.1016/j.sleh.2020.02.012.
Lewien C, Genuneit J, Meigen C, Kiess W, Poulain T. Sleep-related difficulties in healthy children and adolescents. BMC Pediatr. 2021;21(1):82. https://doi.org/10.1186/s12887-021-02529-y.
Lin LN, Chang LY, Hurng BS, Wu CC, Yen LL, Chang HY. Sex differences in sleep patterns and changes in 7th to 12th graders: A longitudinal follow-up study in Taiwan. Sleep. 2018;41(3):1–10. https://doi.org/10.1093/sleep/zsx211.
Jiang X, Hardy LL, Baur LA, Ding D, Wang L, Shi H. Sleep duration, schedule and quality among urban chinese children and adolescents: Associations with routine after-school activities. PLoS One. 2015;10(1):e0115326. https://doi.org/10.1371/journal.pone.0115326.
Eaton DK, McKnight-Eily LR, Lowry R, Perry GS, Presley-Cantrell L, Croft JB. Prevalences of insufficient, borderline, and optimal hours of sleep among high school students - United States, 2007. J Adolesc Health. 2010;46(4):399–401. https://doi.org/10.1016/j.jadohealth.2009.10.011.
Gariepy G, Danna S, Gobina I, et al. How are adolescents sleeping? Adolescent sleep patterns and sociodemographic differences in 24 european and north american countries. J Adolesc Health. 2020;66:S81–8. https://doi.org/10.1016/j.jadohealth.2020.03.013.
Amaral O, Pereira C, Veiga N, Coutinho E, Chaves C, Nelas P. Gender and age differences in sleep habits: A cross-sectional study in adolescents. Aten Primaria. 2016;48(1):178–82.
Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep for pediatric populations: A consensus statement of the american academy of sleep medicine. J Clin Sleep Med. 2016;12(6):785–6. https://doi.org/10.5664/jcsm.5866.
James S, Chang AM, Buxton OM, Hale L. Disparities in adolescent sleep health by sex and ethnoracial group. SSM Popul Health. 2020;11(100581):100581. https://doi.org/10.1016/j.ssmph.2020.100581.
Becker SP, Sidol CA, Van Dyk TR, Epstein JN, Beebe DW. Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: A systematic review. Sleep Med Rev. 2017;34:94–121. https://doi.org/10.1016/j.smrv.2016.07.004.
Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8(6):602–12. https://doi.org/10.1016/j.sleep.2006.12.002.
Crowley SJ, Carskadon MA. Modifications to weekend recovery sleep delay circadian phase in older adolescents. Chronobiol Int. 2010;27(7):1469–92. https://doi.org/10.3109/07420528.2010.503293.
Kortesoja L, Vainikainen MP, Hotulainen R, et al. Bidirectional Relationship of Sleep with Emotional and Behavioral Difficulties: A Five-year Follow-up of Finnish Adolescents. J Youth Adolesc. 2020;49(6):1277–91. https://doi.org/10.1007/s10964-020-01203-3.
Lehto JE, Aho O, Eklund M, et al. Circadian preferences and sleep in 15- to 20-year old Finnish students. Sleep Sci. 2016;9(2):78–83. https://doi.org/10.1016/j.slsci.2016.06.003.
Harbard E, Allen NB, Trinder J, Bei B. What’s keeping teenagers up? Prebedtime behaviors and actigraphy-assessed sleep over school and vacation. J Adolesc Health. 2016;58(4):426–32. https://doi.org/10.1016/j.jadohealth.2015.12.011.
Feinberg I, Campbell IG. Sleep EEG changes during adolescence: An index of a fundamental brain reorganization. Brain Cogn. 2010;72(1):56–65. https://doi.org/10.1016/j.bandc.2009.09.008.
Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: Effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123(6):e1005–10. https://doi.org/10.1542/peds.2008-3641.
Chang L-Y, Wu C-C, Yen L-L, Chang H-Y. The effects of family dysfunction trajectories during childhood and early adolescence on sleep quality during late adolescence: Resilience as a mediator. Soc Sci Med. 2019;222:162–70. https://doi.org/10.1016/j.socscimed.2019.01.010.
Hoopes EK, Berube FR, D'Agata MN, et al. Sleep duration regularity, but not sleep duration, is associated with microvascular function in college students. Sleep. 2021;44(2). https://doi.org/10.1093/sleep/zsaa175.
Williamson AA, Milaniak I, Watson B, et al. Early childhood sleep intervention in urban primary care: Caregiver and clinician perspectives. J Pediatr Psychol. 2020;45(8):933–45. https://doi.org/10.1093/jpepsy/jsaa024.
Chaput JP, Janssen I. Sleep duration estimates of Canadian children and adolescents. J Sleep Res. 2016;25(5):541–8. https://doi.org/10.1111/jsr.12410.
Larson K, Russ SA, Crall JJ, Halfon N. Influences on multiple social risks on children’s health. Pediatrics. 2008;121(2):337–44. https://doi.org/10.1542/peds.2007-0447.
Yang AJ, Gromoske AN, Olson MA, Chaffin JG. Single and cumulative relations of social risk factors with children’s dental health and care-utilization within regions of the united states. Matern Child Health J. 2016;20(3):495–506. https://doi.org/10.1007/s10995-015-1847-2.
US Census Bureau. 2018 national survey of children’s health methodology report. 2019. https://www2.census.gov/programs-surveys/nsch/technical-documentation/methodology/2018-NSCH-Methodology-Report.pdf. Accessed Dec 23 2021.
Wheaton AG, Claussen AH. Short sleep duration among infants, children, and adolescents aged 4 months-17 years - united states, 2016–2018. MMWR Morb. Mortal. Wkly. Rep. 2021;70(38):1315–21. https://doi.org/10.15585/mmwr.mm7038a1.
Wang J, Zhang X, Simons SR, Sun J, Shao D, Cao F. Exploring the bi-directional relationship between sleep and resilience in adolescence. Sleep Med. 2020;73:63–9. https://doi.org/10.1016/j.sleep.2020.04.018.
Child and Adolescent Health Measurement Initiative. 2018 national survey of children’s health (NSCH) data query. Data resource center for child and adolescent health supported by the U.S. department of health and human services, health resources and services administration (HRSA), maternal and child health bureau (MCHB). 2018. www.childhealthdata.org. Accessed 2 Aug 2022.
Schlarb A, Gulewitsch M, Weltzer V, Ellert U, Enck P. Sleep duration and sleep problems in a representative sample of german children and adolescents. Health (N. Y.). 2015;07:1397–408. https://doi.org/10.4236/health.2015.711154.
Lee S-M, Kim J-H. Differences of adaptation to school and self-resilience before and after sleep education for adolescent. J Exerc Rehabil. 2016;12(3):176–81. https://doi.org/10.12965/jer.1632588.294.
Funding
Dr. Patterson's work was partially supported by the Centers of Biomedical Research Excellence (COBRE) in cardiovascular health (P20GM113125).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This study was deemed exempt by University of Delaware and Delaware State University Institutional Review Boards. This decision was made in accordance with the ethical stands of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Given the exemption by the University of Delaware and Delaware State University Institutional Review Boards, informed consent was not obtained for completion of this de-identified secondary data analysis.
Statement Regarding the Welfare of Animals
Not Applicable.
Conflict of Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Covington, L.B., Ji, X., Laurenceau, JP. et al. Exploration of Sex and Age as Moderators Between Social Cumulative Risk and Sleep in a Representative Sample of Children and Adolescents Living in the United States. Int.J. Behav. Med. 31, 229–240 (2024). https://doi.org/10.1007/s12529-023-10175-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-023-10175-0