Abstract
Background
Obesity is highly prevalent around the world, including in Chile. Although various psychological factors have been previously associated with obesity, there has been less attention on the role of weight stigma as a determinant of obesity in Chile. Therefore, the primary aim of this study was to examine the direct effect of weight stigma on obesity and determine whether chronic stress and unhealthy diet mediate the relationship between weight stigma and obesity.
Methods
Faculty and staff from a Chilean university enrolled in the Chilean Study of Psychological Predictors of Obesity and Metabolic Syndrome and completed anthropometric measurements and measures of weight stigma, chronic stress, and unhealthy diet.
Results
Three-hundred and eighty-three participants (Mage = 45 years old; 58% female) were included in the present analysis. Structural equation model analyses demonstrated a direct effect of weight stigma on obesity, chronic stress, and unhealthy diet. However, chronic stress and unhealthy diet did not mediate the relationship between weight stigma and obesity.
Conclusions
Weight stigma is an important determinant of obesity and is associated with high levels of chronic stress and unhealthy diet in Chilean adults. Our results provide further support for the multifactorial nature of obesity and can inform future interventions aimed promoting weight loss in people with overweight and obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a highly prevalent public health concern around the world, including in Chile. More than half of the adult population in Latin America and the Caribbean is considered to have overweight or obesity. In Chile, 63% of people with higher body weight is 63% [1]. The National Survey of Health in Chile reports that 33.7% of women and 28.6% of men had obesity between 2016 and 2017 [2]. Similarly, 42.1% of women and 38.3% of men had obesity in the USA between 2011 and 2014 (rates are adjusted by age, 40 to 59 years old) [3]. These rates reflect a global rise in obesity [4, 5] that has grave public health consequences, including a significantly elevated risk of chronic conditions like cardiovascular disease, diabetes, and hypertension [6, 7] and substantial economic burden due to the medical cost of obesity [8, 9].
Several determinants and consequences of obesity, such as obesogenic environments [10] and poor health [11], have been previously identified. Various psychological factors have also been associated with obesity, including chronic stress and depressive symptoms [12, 13]. However, the role of weight stigma has received less attention in Chile. Weight stigma is defined as social devaluation and denigration of individuals perceived to carry excess weight, which leads to prejudice, negative stereotyping, and discrimination [14]. Given that overweight and obesity are visible states that can be observed, individuals who carry excess weight can easily become the targets of stigma [15].
Weight stigma has been well studied in several countries, including European nations and the USA [16,17,18,19]. Research consistently demonstrates that weight stigma is common among individuals with obesity [15], has negative effects [20, 21], occurs across varied contexts, including workplace, medical, interpersonal, and family contexts [22], and is detrimental to health [23]. Several studies demonstrate that experiences of weight stigma have consequences such as greater healthcare-related stress, avoidance of healthcare [24], and poor health behaviors [25], such as higher caloric intake [20], tobacco and alcohol use [26], and sedentary behavior [27]. Robust evidence also documents a bidirectional relationship between weight stigma and obesity, such that individuals who experience greater stigma tend to have higher BMIs and waist circumferences [23,24,25], and individuals with higher BMI are more likely to experience weight stigma and weight stigma may promote further weight gain [14, 26]. There are several mechanisms that underlie this relationship [27]. The Cyclic Obesity/Weight-Based Stigma Model [14] posits weight stigma feeds into the cycle of obesity by triggering a series of stressor-related physiological, affective, and behavioral responses [28]. For example, weight stigma activates the HPA axis, which leads to increased cortisol levels and caloric intake, and, ultimately, weight gain [29]. Furthermore, according to the Social Identity Threat Model, the experience of weight stigma threatens social identity and constitutes a stressor that triggers stressor-related physiological, emotional, and behavioral responses [30].
Eating behavior is one mechanism by which weight stigma may influence obesity. An experimental study with women demonstrates that the experience of weight stigma predicts subsequent consumption of high calorie foods [20]. Another experimental study of university students also demonstrates that the experience of weight stigma increases caloric consumption and reduces perceived dietary control among women with overweight [31]. Similarly, diet is directly associated with weight gain [32]. Diets high in saturated fat, sodium, and added sugar are associated with obesity [33] and high consumption of processed foods are associated with weight gain and cardiometabolic health problems [34]. A study conducted in Chile that examined changes in food consumption between 1988 and 1997 documents a 25% increase in overall energy consumption over the study period, including a significant increase in the consumption of foods rich in saturated fats, processed foods, and foods with added sugar and decrease in the consumption of whole grains, legumes, and cereals [35].
Despite the steep rise in rates of overweight and obesity in Chile over the past three decades, there is a paucity of research examining weight stigma. To our knowledge, a single qualitative study of young Chileans demonstrates an association between obesity and both low socioeconomic status and negative attributes, such as laziness, anxiety, and physical unattractiveness. Therefore, people with obesity in Chile may not only be discriminated against because of their physical appearance but also because of perceptions regarding their social class [36].
Nevertheless, no previous research has examined the role of weight stigma on obesity, chronic stress, and unhealthy diet among Chilean adults. Therefore, the primary aim of this study was to examine the direct effect of weight stigma on obesity among Chilean adults and determine whether chronic stress and unhealthy diet mediate the relationship between weight stigma and obesity. Thus, we hypothesized that (1) weight stigma is associated with higher BMI, (2) unhealthy diet mediates this association, and (3) there is a sequential mediation via chronic stress and unhealthy diet.
Method
Participants and Procedures
A convenience sample of 383 participants was enrolled in the Chilean Study of Psychological Predictors of Obesity and Metabolic Syndrome (FONDECYT Iniciación N°11140454). Three longitudinal assessments were obtained every 12 months between 2015 and 2017; however, the current analyses focus on data collected in the third assessment in 2017. In order to be enrolled, participants had to be faculty or staff working for at least 1 year in a public university in the south of Chile. Participants with previous diagnosis of cardiovascular disease, cancer, severe depression, schizophrenia, or inflammatory disease were excluded.
This study was approved by the Scientific Ethics Committee at the Universidad de La Frontera in Temuco, Chile. A trained research assistant contacted all potential participants via email or telephone. Potential participants were informed about the project and study procedures involved. The research assistant verified eligibility and subsequently enrolled those who were eligible and interested in the study. All participants provided informed consent. At each of the three annual visits, participants fasted for at least 8 h before coming into the laboratory and underwent a blood draw (not reported) and anthropometric measurements, including weight, height, waist circumference, and three blood pressure assessments. Participants subsequently completed psychosocial measures online. They were instructed to answer all items. Participants were compensated approximately $15 USD ($10,000 Chilean Pesos) per visit.
Measures
Stigmatizing Situations Inventory (Inventario de Situaciones Estigmatizantes; [37]) is a 10-item measure that assesses how often individuals have experienced weight stigma in the past year. Examples include “Children make fun of me because of my weight” and “I cannot find clothes in my size.” Response options are on an 8-point Likert-type scale (0 = never to 7 = daily). This scale demonstrated excellent internal consistency in this sample (α = .906). The variable weight stigma was measured in wave 2 (2016) and wave 3 (2017). However, data collected in wave 2 (2016) was solely used to validate this measure. Therefore, a reliable, valid measure for weight stigma was only available in wave 3 (2017).
Chronic Stress Burden Scale [38] is a 5-item measure that assesses whether individuals have ever experienced a series of chronic stressors, such as ongoing health problems, job difficulties, and financial strain. Response options are dichotomous (yes = 1, no = 0). A sum score was calculated.
As regards to diet, participants reported the frequency that they consumed different types of food during the last week (0 = none; 7 = all days). This assessment was based on the National Survey of Nutrition in Chile (Encuesta Nacional de Consumo Alimentario) [2]. The current study coded the consumption of sugary drinks, snacks high in sugar or fat, fried food, and fast food, as indicators of an unhealthy diet [39, 40].
Body mass index (BMI) was assessed using the standard calculation (BMI = weight [kilograms]/height [meters2]) as a proxy of obesity.
With a demographics questionnaire, participants self-reported their gender, income, and education. We included these covariates in the model given it well-known association with BMI [41, 42].
Statistical Analysis
Before run the analyses, we did a visual examination for each variable, creating spike plots and box plots, and did not find any outliers. All analyses were conducted using STATA (14.1). Structural equation modeling was used to sequentially test (1) the direct effect of weight stigma on obesity, (2) whether unhealthy diet mediated this association, and (3) if chronic stress and unhealthy diet sequentially mediated the direct effect.
A Confirmatory Factor Analysis (CFA) was conducted to create a latent factor to capture unhealthy diet. P values below .05 were considered significant. Model fit was evaluated according to criteria proposed by Hu and Bentler [43]. The Comparative Fit Index (CFI) is a scaled as a goodness-of-fit index that ranges from 0 to 1, with higher values indicating better model fit. In accordance with the criteria of Hu and Bentler, a value ≥ 0.95 was used as a cutoff score to indicate good model fit. The standardized root mean square residual (SRMR) and root mean square error of approximation (RMSEA) are scaled as badness-of-fit indices that ranges from 0 to 1, with lower values indicating better model fit. In accordance with the criteria of Hu and Bentler, a SRMR value ≤ 0.08 and RMSEA value ≤ 0.06 were used as cutoff scores to indicate good model fit. A nonsignificant χ2 test statistic was also used to determine good model fit.
Results
Sample Characteristics
Participants were on average 45 years old (SD = 8.76) with a slightly higher proportion of women (59%). According to the Adult Treatment Panel III (ATP III) criteria, abdominal obesity is defined as waist size circumference greater than 88 cm for women and 102 for men. Thus, 53% of women and 32% of men meet criteria for abdominal obesity. The average waist circumference was 88.87 cm (SD = 10.05) for women and 99.00 cm (SD = 10.78) for men. The average BMI was 28.05 kg/m2 (SD = 4.49). Twenty-three percent had normal weight, 52% overweight, and 25% obesity. Approximately 45% of participants graduated high school or completed post-secondary education (i.e., vocational/technical or university degrees) and 55% completed a master’s degree or other graduate degree (e.g., doctoral or professional degree). Sixty percent of the sample reported an individual annual income was between US$4488 and $18,000, which is greater than the Chilean minimum wage per year (~ US$3750).
Confirmatory Factor Analysis
Due to the violation of the assumption of normality (Mardias multivariate test p ≤ .001), all analyses were conducted using maximum likelihood estimation with the Satorra-Bentler correction. After performing a CFA for the unhealthy diet factor, all the loadings were greater that .3: consumption of sugary drinks (β = .522, p = .001), snacks high in sugar or fat (β = .424, p = .001), fried foods (β = .453, p = .001), and fast food (β = .451, p = .001); therefore, all the indicators were retained according to the cutoff proposed by Child [44]. In order to optimize the latent factor fit, we added a covariance between snacks high in sugar or fat and fast food, which was statistically significant (β = .278, p = .001). The overall fit indices were good χ2(1) = 1.865, p = .172, CFI = .991, RMSEA = .048 (.000–.153), SRMR = .014.
Hypothesized Model
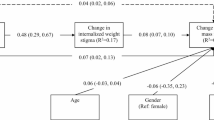
Correlations between all study variables are shown in Table 1. BMI was inversely associated with education (r = − .165, p < .001), income (r = − .011, p < 0.05), and gender (r = − .191, p < .001). Given the strong association between education and income (r = .793, p < 0.01), we chose to include only education as a covariate in the model in order to avoid multicollinearity [45]. Furthermore, we added gender as a covariate. Weight stigma was significantly associated with higher BMI (i.e., β = .379, p = .001) as well as greater chronic stress (β = .179, p = .001) and unhealthy diet (β = .163, p = .050). Similarly, chronic stress was directly associated with unhealthy diet (β = .223, p = .004), and unhealthy diet was associated with higher BMI (β = .200, p = .010). The association between chronic stress and BMI was not significant (β = − .078, p = .140) (see Fig. 1).
The final model demonstrated good overall fit: χ2(16) = 33.993, p = .005, CFI = .926, RMSEA = .056 (.030–.083), SRMR = .041, and explained a proportion of variance in BMI (R2 = .285). Contrary to hypotheses, the relationship between weight stigma and BMI was not explained through the indirect effects of chronic stress and unhealthy diet (β = .008, p = .096), or via unhealthy diet alone (β = .032, p = .106).
Discussion
The primary aim of this study was to examine the effect of weight stigma on BMI in Chilean adults and determine whether chronic stress and unhealthy diet mediate the relationship between weight stigma and BMI. Results demonstrate that weight stigma was associated with greater BMI, chronic stress, and unhealthy diet. Unhealthy diet, in turn, was associated with greater BMI. Contrary to hypotheses, chronic stress did not mediate the relationship between weight stigma and BMI, nor was there evidence of the proposed sequential mediation via chronic stress and unhealthy diet.
Importantly, these results build upon previous research conducted in other countries [14, 15] and, to our knowledge, are the first to examine the relationship between weight stigma and BMI in sample of Chilean adults. Weight stigma and its consequences are particularly relevant for Chileans since Chile currently has the highest rates of overweight and obesity in the world. Almost three quarters of the Chilean population (74.2%) currently have overweight or obesity, compared to 72.5% of the Mexican population and 71.0% of the US population [46]. Therefore, it is crucial to identify psychological factors, such as weight stigma, that may be contributing to this significant increase in overweight and obesity.
Our findings suggest that weight stigma is associated with greater chronic stress, another psychological risk factor. Given that chronic stress predicts greater caloric intake [47] and higher BMI [48], weight stigma in Chilean adults may confer worse health both directly and through its association with greater chronic stress. Given that people with higher body weight commonly experience weight stigma from diverse sources (e.g., family and strangers), it is possible that these experiences directly increase chronic stress and, ultimately, contribute poor mental and physical health across the lifespan. Weight stigma is also associated with unhealthy behaviors, such as lower physical activity and decreased healthcare utilization, which can contribute to the genesis and maintenance of obesity [49, 50]. Therefore, future intervention efforts should consider including behavioral skills training in order to manage stress and negative emotional states associated with weight stigma.
Our hypothesis that the relationship between weight stigma and BMI would be sequentially mediated by chronic stress and unhealthy diet was not supported. Although weight stigma was directly associated with greater chronic stress and unhealthy diet, these variables did not mediate the association between weight stigma and BMI. This null finding contradicts previous research [30, 51, 52] that demonstrates the mediating role of these variables. More research is needed to understand the role of chronic stress and unhealthy diet among Chileans with overweight and obesity. Another potential mechanism that was not included in the current study is weight bias internalization (WBI). Research demonstrates that experience and internalization of weight stigma are associated with greater binge eating, BMI [53], and weight gain [54]. Therefore, future research should examine WBI as a potential underlying mechanism. We also caution against over interpretation of our results as they are based on a single study.
Our results demonstrate that weight stigma was directly associated with an unhealthy diet. This result is consistent with previous research that demonstrates that weight stigma is related to unhealthy behaviors, including poor diet [48,49,50]. Similar to previous studies examining the effect of weight stigma on diet, the current study included self-report measures of diet that assessed the frequency of consumption of food high in sugar or fat over the past week.
The current study has several strengths, including a relatively large sample and the use of structural equation modeling to test a theoretical model that included psychological, behavioral, and anthropometric variables. Furthermore, to our knowledge, this is the first study to examine the role of weight stigma on obesity in Chile. Previous studies examining weight stigma have primarily examined the effects of weight stigma in non-Latino White samples. The primary limitation of this study is the cross-sectional design. Statistical analyses were grounded in a strong theoretical framework that informed hypotheses and interpretation of findings and were consistent with Hayes’s guidelines [55] regarding mediation analyses in cross-sectional designs. Nevertheless, it is important to recognize that causal inference cannot be inferred in this study. Another limitation is the generalizability of our results. Although our sample was relatively large, a convenience sample of university faculty and staff was used. However, we note that the current sample demonstrated a distribution of education and income similar to the general Chilean population.
An important future direction is the use of longitudinal designs to examine how the relationship between weight stigma and obesity unfolds across time and establish temporal precedence. Future studies should also include other potential explanatory variables like physical activity and WBI when examining factors that may explain the relationship between weight stigma and obesity. Future cross-cultural studies will also be important to understanding possible differences between non-Latino Whites, Latinos in the USA, and Latinos in Latin America with respect to weight stigma and its consequences.
Conclusions
In the last decade, there has been a steep increase in individuals carrying excess weight in Chile. The current study highlights that weight stigma, psychological stress, and diet quality are factors that may contribute to the understanding of this phenomenon in an understudied population. Although chronic stress and diet quality did not mediate the association between weight stigma and BMI, findings demonstrated that weight stigma is associated with greater chronic stress and worse diet quality, both of which have been previously linked with BMI. To our knowledge, this is the first study to examine weight stigma and BMI in Chilean adults and builds upon prior studies primarily comprised of non-Latino White samples.
References
United Nations and Pan American Health Organization, Panorama de la seguridad alimentaria y nutricional, 2017.
Ministerio de Salud ENCUESTANACIONALDESALUD. Primeros resultados. 2016-2017:2017.
Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015;219:1–8.
Moreno M. Definición y Clasificación de la Obesidad. Rev Médica Clínica Las Condes. 2012;23(2):124–8.
Williams E, Mesidor M, Winters K, Dubbert P, Wyatt S. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Curr Obes Rep. 2015;4(3):363–70.
Bastien M, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56(4):369–81.
Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on obesity and heart disease from the Obesity Committee of the Council on Nutrition. Physical Circulation. 2006;113(6):898–918.
Dietz W, Douglas C, Brownson R. Chronic disease prevention: tobacco avoidance, physical activity, and nutrition for a healthy start. JAMA. 2016;316(16):1645–6.
Kim DD, Basu A. Estimating the medical care costs of obesity in the United States: systematic review, meta-analysis, and empirical analysis. Value Health. 2016;19(5):602–13.
Azar A, Franetovic G, Santos H. Determinantes individuales, sociales y ambientales del sobrepeso y la obesidad adolescente en Chile. Rev Med Chil. 2015;143(5):598–605.
Hruby A, Manson JE, Qi L, et al. Determinants and consequences of obesity. Am J Public Health. 2016;106(9):1656–62.
Blümel JE, Chedraui P, Aedo S, Fica J, Mezones-Holguín E, Barón G, et al. Obesity and its relation to depressive symptoms and sedentary lifestyle in middle-aged women. Maturitas. 2015;80(1):100–5.
Puterman E, Prather AA, Epel ES, Loharuka S, Adler NE, Laraia B, et al. Exercise mitigates cumulative associations between stress and BMI in girls age 10 to 19. Health Psychol. 2016;35(2):191–4.
Tomiyama AJ. Weight stigma is stressful. A review of evidence for the cyclic obesity/weight-based stigma model. Appetite. 2014;82:8–15.
Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring). 2009;17(5):941–64.
Incollingo Rodriguez AC, Tomiyama AJ, Ward A. What does weight stigma smell like? Cross-modal influence of visual weight cues on olfaction. Int J Obes. 2015;39(6):1030–2.
Latner JD, O’Brien KS, Durso LE, Brinkman LA, MacDonald T. Weighing obesity stigma: the relative strength of different forms of bias. Int J Obes. 2008;32(7):1145–52.
Brewis A, SturtzSreetharan C, Wutich A. Obesity stigma as a globalizing health challenge. Glob Health. 2018;14(1):20.
Emmer C, Bosnjak M, Mata J. The association between weight stigma and mental health: a meta-analysis. Obes Rev. 2020;21(1):1–13.
Schvey NA, Puhl RM, Brownell KD. The impact of weight stigma on caloric consumption. Obesity (Silver Spring). 2011;19(10):1957–62.
Vartanian LR, Novak SA. Internalized societal attitudes moderate the impact of weight stigma on avoidance of exercise. Obesity (Silver Spring). 2011;19(4):757–62.
Latner JD, Puhl RM, Stunkard AJ. Cultural attitudes and biases toward obese persons. In: Akabas SR, Lederman SA, Moore BJ, editors. Textbook of obesity: biological, psychological and cultural influences. 1st ed. United Kingdom, UK: Wiley-Blackwell; 2012. p. 42–57.
Thille P, Friedman M, Setchell J. Weight-related stigma and health policy. CMAJ. 2017;189(6):E223–4.
Jackson SE, Beeken RJ, Wardle J. Perceived weight discrimination and changes in weight, waist circumference, and weight status. Obesity (Silver Spring). 2014;22(12):2485–8.
Seacat JD, Dougal SC, Roy D. A daily diary assessment of female weight stigmatization. J Health Psychol. 2016;21(2):228–40.
Kahan S, Puhl RM. The damaging effects of weight bias internalization. Obesity (Silver Spring). 2017;25(2):280–1.
Hayward LE, Vartanian LR, Pinkus RT. Weight stigma predicts poorer psychological well-being through internalized weight bias and maladaptive coping responses. Obesity (Silver Spring). 2018;26(4):755–61.
Araiza AM, Lobel M. Stress and eating: Definitions, findings, explanations, and implications. Soc Personal Psychol Compass. 2018;12(4):1–13.
Tomiyama AJ, Finch LE, Cummings JR. Did that brownie do its job? Stress, eating, and the biobehavioral effects of comfort food. Emerg Trends Soc Behav Sci. 2015:1–15.
Hunger JM, Major B, Blodorn A, Miller CT. Weighed down by stigma: how weight-based social identity threat contributes to weight gain and poor health. Soc Personal Psychol Compass. 2015;9(6):255–68.
Major B, Hunger JM, Bunyan DP, Miller CT. The ironic effects of weight stigma. J Exp Soc Psychol. 2014;51:74–80.
Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–404.
Tapsell LC, Neale EP, Satija A, Hu FB. Foods, nutrients, and dietary patterns: interconnections and implications for dietary guidelines. Adv Nutr. 2016;7(3):445–54.
Poti JM, Braga B, Qin B. Ultra-processed food intake and obesity: what really matters for health—processing or nutrient content? Curr Obes Rep. 2017;6(4):420–31.
Crovetto M, Uauy R. Changes in household food and nutrient consumption in Metropolitan Santiago 1988-97 by income. Rev Med Chil. 2010;138(9):1091–108.
Energici MA, Acosta E, Borquez F, Huaiquimilla M. Fatness, discrimination and classism: a study in youth from Santiago de Chile. Psicol Soc. 2017;29:1–10.
Ortiz MS, Gómez-Pérez D. Psychometric properties of a brief Spanish version of Stigmatizing Situations Inventory. Mex J Eat Disord. 2019;10(1):1–9.
Bromberger JT, Matthews KA. A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle-aged women. Psychol Aging. 1996;11(2):207–13.
Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Fruit and vegetable intakes, C-reactive protein, and the metabolic syndrome. Am J Clin Nutr. 2006;84(6):1489–97.
Esposito K, Ceriello A, Giugliano D. Diet and the metabolic syndrome. Metab Syndr Relat Disord. 2007;5(4):291–6.
Kim TJ, von dem Knesebeck O. Income and obesity: what is the direction of the relationship? A systematic review and meta-analysis. BMJ Open. 2018;8(1):e019862.
Ohlsson B, Manjer J. Sociodemographic and lifestyle factors in relation to overweight defined by BMI and ‘normal-weight obesity’. J Obes. 2020;2020:2070297.
Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6(1):1–55.
Child D. The essentials of factor analysis. Cassell Educational: New York, NY; 2006.
Vatcheva KP, Lee M, McCormick JB, Rahbar MH. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiology (Sunnyvale). 2016;6(2):227.
Organization for Economic Cooperation and Development. Overweight or obese population (indicator). https://data.oecd.org/healthrisk/overweight-or-obese-population.htm. Accessed June 23, 2020.
Groesz LM, McCoy S, Carl J, Saslow L, Stewart J, Adler N, et al. What is eating you? Stress and the drive to eat. Appetite. 2012;58(2):717–21.
Stepanikova I, Baker EH, Simoni ZR, et al. The role of perceived discrimination in obesity among African Americans. Am J Prev Med. 2017;52(1S1):S77–85.
Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019–28.
Puhl RM, Brownell KD. Ways of coping with obesity stigma: review and conceptual analysis. Eat Behav. 2003;4(1):53–78.
Major B, Tomiyama AJ, Hunger JM. The negative and bidirectional effects of weight stigma on health. In: Major B, Dovidio JF, Link BG, editors. The Oxford handbook of stigma, discrimination and health. New York, NY: Oxford University Press; 2018. p. 499–519.
Vartanian LR, Porter AM. Weight stigma and eating behavior: a review of the literature. Appetite. 2016;102:3–14.
Pearl RL, Puhl RM, Himmelstein MS, Pinto AM, Foster GD. Weight stigma and weight-related health: associations of self-report measures among adults in weight management [published online ahead of print, 2020 Apr 25]. Ann Behav Med. 2020kaaa026.
Puhl RM, Wall MM, Chen C, Bryn Austin S, Eisenberg ME, Neumark-Sztainer D. Experiences of weight teasing in adolescence and weight-related outcomes in adulthood: a 15-year longitudinal study. Prev Med. 2017;100:173–9.
Hayes A. Introduction to mediation, moderation, and conditional process analysis. a regression-based approach. New York, NY: Guilford Press; 2018.
Funding
This study was fully funded by the National Commission for Scientific and Technological Research, Formation of Advanced Human Capital Program/Doctorado Nacional 21150016; and partially by Universidad de La Frontera, Postdoctoral research program UFRO, VRIP19P001; National Fund for Scientific and Technological Development Regular (1180463), National Fund for Scientific and Technological Development Postdoctoral (3180534); and by a Health and Behavior International Collaborative Award sponsored by American Psychosomatic Society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gómez-Pérez, D., Cancino, V., Moreno, P.I. et al. Weight Stigma, Chronic Stress, Unhealthy Diet, and Obesity in Chilean Adults. Int.J. Behav. Med. 28, 292–298 (2021). https://doi.org/10.1007/s12529-020-09917-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-020-09917-1