Abstract
Background
The diagnosis and treatment of attention deficit hyperactivity disorder (ADHD) comorbid with epilepsy have been insufficiently addressed in China. We conducted a study in China to investigate the current status, diagnosis, and treatment of ADHD in children to further our understanding of ADHD comorbid with epilepsy, strengthen its management, and improve patients’ quality of life.
Methods
We carried out a multicenter cross-sectional survey of children with epilepsy across China between March 2022 and August 2022. We screened all patients for ADHD and compared various demographic and clinical factors between children with and without ADHD, including gender, age, age at epilepsy onset, duration of epilepsy, seizure types, seizure frequency, presence of epileptiform discharges, and treatment status. Our objective was to explore any possible associations between these characteristics and the prevalence of ADHD.
Results
Overall, 395 epilepsy patients aged 6–18 years were enrolled. The age at seizure onset and duration of epilepsy ranged from 0.1–18 to 0.5–15 years, respectively. Focal onset seizures were observed in 212 (53.6%) patients, while 293 (76.3%) patients had epileptiform interictal electroencephalogram (EEG) abnormalities. Among the 370 patients treated with anti-seizure medications, 200 (54.1%) had monotherapy. Although 189 (47.8%) patients had ADHD, only 31 received treatment for it, with the inattentive subtype being the most common. ADHD was more common in children undergoing polytherapy compared to those on monotherapy. Additionally, poor seizure control and the presence of epileptiform interictal EEG abnormalities may be associated with a higher prevalence of ADHD.
Conclusions
While the prevalence of ADHD was higher in children with epilepsy than in normal children, the treatment rate was notably low. This highlights the need to give more importance to the diagnosis and treatment of ADHD in children with epilepsy.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is one of the most common brain disorders characterized by recurrent seizures [1]. The overall prevalence of epilepsy is higher in developing countries than in developed ones [2,3,4], and approximately 70 million people are affected by epilepsy worldwide [5]. Over the years, the knowledge about the diagnosis, etiology, and treatment of epilepsy is constantly evolving. However, the comorbidities associated with epilepsy have not received enough attention during routine diagnosis and treatment, particularly in developing countries, as neurologists tend to prioritize the treatment of seizures. The comorbidities of epilepsy, defined as disorders coexisting with or preceding epilepsy or else compounded or directly attributed to epilepsy or its treatment [6, 7], are broadly divided into physical, neurological, and psychological comorbidities [8]. These comorbidities are often associated with significant social stigma [9], which not only affects the daily lives and overall quality of life of affected individuals but also restricts their opportunities for professional growth [10, 11].
Attention deficit hyperactivity disorder (ADHD) is a common psychological comorbidity for children with epilepsy, often associated with academic and vocational underachievement, depression, and anxiety, which may have a significant impact on people with epilepsy [12, 13]. However, the diagnosis of ADHD has often been overlooked, as clinicians prioritize the diagnosis and treatment of epilepsy. Moreover, attention and behavioral problems may mistakenly be attributed to seizures or the side effects of anti-seizure medication (ASM), contributing to the underdiagnosis of ADHD in children with epilepsy [14]. In addition, most of the children with epilepsy who are diagnosed with ADHD do not receive treatment for it, especially in low and middle-income countries [15].
To strengthen the diagnosis and treatment of ADHD comorbid with epilepsy, the Comorbidity Committee of China Association Against Epilepsy (CC-CAAE) published the “Chinese expert consensus on the diagnosis and treatment of ADHD in children with epilepsy”. Despite this initiative, there are very few reports on ADHD in children with epilepsy in China, with most being single-center studies. Currently, there is a notable absence of large-scale, multi-center studies focusing on ADHD in children with epilepsy in China.
The objective of this study is to assess the prevalence of ADHD among children with epilepsy in China and to investigate potential differences in ADHD prevalence compared to children without epilepsy. We seek to explore the effect of various factors on the prevalence of ADHD, including gender, age of seizure onset, seizure type, frequency of seizures, electroencephalogram (EEG) abnormalities, course of epilepsy, and the efficacy of antiepileptic drugs. In addition, this study will also provide a scientific basis for improving the prognosis of ADHD in children with epilepsy.
Methods
Study design and participants
This study was a cross-sectional study conducted by CC-CAAE across 10 tertiary general or children’s specialized hospitals. Given that children with epilepsy are typically treated in specialized or tertiary hospitals in China, while community hospitals and secondary hospitals are rarely involved in their diagnosis and treatment, only tertiary hospitals were included in this study. These participating hospitals were located across different regions of China, including ethnic minority areas with different levels of economic development and medical care. Therefore, the study provides a more comprehensive and accurate depiction of the diagnosis and treatment status of children with epilepsy and ADHD in China.
Children with an initial diagnosis of epilepsy and those with regular follow-up visits were recruited from the outpatient clinics and wards of the participating hospitals between March 2022 and August 2022. Inclusion criteria comprised age ranging from 6 to 18 years, epilepsy duration of at least 6 months, and parents/legal caregivers capable of answering questionnaire questions independently and clearly. Additionally, patients and their parents/legal caregivers were duly informed about the retrospective analysis of medical records and the assessment of the ADHD scale conducted in this study. Signed informed consent was obtained from those patients and their parents/legal caregivers who agreed to participate. Patients with non-epileptic seizures or any other concomitant mental disorders were excluded.
The study was approved by the ethics committee of West China Hospital, Sichuan University (the leader unit) under protocol number 2021(327), and collaborating research institutes. The research was performed in accordance with the Declaration of Helsinki.
Assessment and data collection
The parents/caregivers of all enrolled patients completed the ADHD Rating Scale V and Conners Parent Rating Scale. These rating scales were used to assess inattention, hyperactivity and impulsivity symptoms, and behavior problems. The results were then utilized by clinicians to make diagnoses related to ADHD and subtypes, in accordance with the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-V-TR) [16].
Demographic and clinical characteristics were collected through a clinical retrospective review, focusing on details such as gender, age of epilepsy onset, duration of epilepsy, seizure types, epilepsy syndromes, seizure frequency, presence of epileptiform discharges, types of ASM, and duration of treatment. The clinical features of all patients were reviewed and confirmed by a child neurologist at the respective hospital. Epileptic seizure types and syndromes were identified by a clinical review of medical records, including demographic data, previous clinical descriptions of epileptic seizures, and EEG features. These data were then classified according to clinical manifestations and the international classification system of the International League Against Epilepsy. The frequency of seizure attacks was categorized into three groups: control (seizure-free for at least 1 year), less than one seizure per 3 months, and more than one seizure per 3 months. Epileptiform abnormalities were defined as the presence of generalized interictal epileptiform discharges, focal epileptiform discharges, and multifocal interictal epileptiform discharges. Types of ASM were categorized as monotherapy, polytherapy, drug withdrawal (defined as prior treatment with ASM that was completely discontinued), or never used ASM.
Statistical methods
As the prevalence of ADHD in children with epilepsy is estimated to be between 30% and 40% [17], the required sample size for this study was at least 369 patients. Continuous and categorical variables were summarized as medians and frequencies, respectively. The demographic and clinical characteristics in children with or without ADHD were compared using Pearson’s Chi-squared test, and a P value of < 0.05 was considered statistically significant. If a group of comparisons was statistically significant, further logistic regression analysis was used to examine the association between demographic and clinical characteristics and ADHD. Odds ratios (OR) and 95% confidence intervals (CI) were reported.
Results
Overall, 395 patients aged 6–18 years with epilepsy were enrolled in our study (Fig. 1), with over half being male (n = 231, 58.5%). The median age of the cohort was 10.75 years. The median age of seizure onset and median duration of epilepsy was 6 years (range: 1 month–18 years) and 4 years (range: 6 months–15 years), respectively. Out of the 395 patients, 48 (12.1%) were diagnosed with epilepsy syndrome, while the rest were classified according to seizure type, including 75 (18.9%) with generalized onset seizures, 212 (53.6%) with focal onset seizures, 41 (10.3%) with generalized and focal onset seizures, and 19 (4.8%) with unclassified seizures. Video-EEG lasting more than 3 hours was performed in 384 (97.2%) patients, including both waking and sleeping periods. Among them, 293 (76.3%) patients had epileptiform interictal EEG and the rest had normal EEG results. Seizure attack was classified as controlled in 154 (38.9%) patients, while 146 (36.9%) patients had a seizure less than once per 3 months, and 36 (9.1%) patients had more than one seizure per 3 months. The seizure frequency could not be determined in 59 (14.9%) patients because of a short duration of epilepsy, incomplete medical history, or poor recall by family members. Overall, 370 (93.6%) patients were treated with ASM, with 200 (54.1%) undergoing monotherapy and 170 (45.9%) receiving polytherapy. Additionally, 18 (4.5%) patients had ASM withdrawal, while 7 (1.8%) had never used ASM.
Flow chart of patient recruitment. “East” included the following one hospital: Children’s Hospital of Fudan University. “West” included the following four hospitals: Lanzhou University Second Hospital; Sichuan Provincial People Hospital; Xijing Hospital, Fourth Military Medical University; Sichuan University West China Hospital. “South” included the following one hospital: The First Affiliated Hospital, Sun Yat-sen University. “North” included the following four hospitals: Peking University First Hospital; The First Medical Center of Chinese PLA General Hospital; Beijing Tiantan Hospital, Captial Medical University; The first hospital of Jilin University. ADHD attention deficit hyperactivity disorder
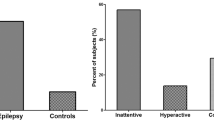
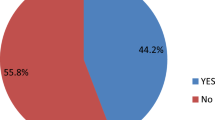
Of the 395 enrolled patients with epilepsy, almost half of them (n = 189, 47.8%) were diagnosed with ADHD based on the DSM-V-TR scale. Among these 189 children with ADHD and epilepsy, the inattentive subtype (ADHD-I) was the most common subtype diagnosed in 95 (50.3%) children, followed by ADHD combined inattentive/hyperactive-impulsive subtype (ADHD-C) in 80 (42.3%) children and hyperactive-impulsive subtype of ADHD (ADHD-H) in 14 (7.4%) children. Notably, only 6 (3.1%) children were receiving or had previously received treatment with methylphenidate, while an additional 25 (13.2%) children had received behavioral therapy for ADHD.
Table 1 presents the prevalence of ADHD in children with epilepsy by various demographic and clinical characteristics. A higher proportion of male children with epilepsy presented with ADHD compared with female children (48.4% vs. 46.9%), but the difference was not statistically significant (P = 0.764). Children aged 6 to 8 years (n = 66, 54.1%) and 9 to 11 years (n = 56, 53.8%) exhibited a significantly higher prevalence (P = 0.019) of ADHD than children aged over 12 years (n = 67, 39.6%). By further logistic regression analysis, children aged over 12 years (OR = 0.557, 95% CI = 0.348–0.893) exhibited decreased odds of developing ADHD compared to those in the younger age groups.
The children were subdivided into four groups based on the age of seizure onset, with the highest prevalence of ADHD observed in those with the first onset age between 3 and 5 years (n = 59, 55.7%), followed by 6 to 8 years (n = 58, 48.3%) (Table 2). The prevalence of ADHD in children with seizure onset aged above 12 years (29.5%) was significantly lower than that in children with seizure onset under 12 years of age (50.1%) (P = 0.033). In general, the prevalence of ADHD gradually decreased with increasing first seizure onset age from 3 to 5 years and beyond. However, no significant difference (P = 0.924) in the prevalence of ADHD was observed when children were grouped according to the duration of epilepsy: under 1 year (n = 12, 44.4%), 1 to 3 years (n = 46, 47.4%), and over 3 years (n = 131, 48.3%). The patients were also grouped according to seizure type and diagnosis of epilepsy syndrome. We found that the prevalence of comorbid ADHD was significantly higher (P = 0.018) in children with generalized onset seizures combined with focal onset seizures (n = 29, 70.7%). All except 11 children had ever undergone EEG testing. Among the children, those with epileptiform interictal EEG abnormalities had a significantly higher prevalence (P = 0.002) of ADHD than those with normal interictal EEG results (52.9% vs. 34.0%). Grouping the patients according to the frequency of seizure attacks showed that the prevalence of ADHD was significantly lower (P < 0.001) in children with seizure control compared to those experiencing seizures less than once per 3 months or more than once per 3 months. Further logistic analysis revealed that seizure onset aged above 12 years (OR = 0.373, 95% CI = 0.167–0.833) decreased the odds of developing ADHD compared with the other three groups. Generalized onset seizures combined with focal onset seizures (OR = 2.914, 95% CI = 1.294–6.564) increased the odds of developing ADHD compared with their counterparts. The odds of developing ADHD among children with normal interictal EEG were found to decrease by 0.460 when compared with children with epileptiform interictal EEG abnormalities (OR = 0.460, 95% CI = 0.282–0.751). Children with a seizure frequency of less than once per 3 months (OR = 1.657, 95% CI = 1.044–2.629) and more than once per 3 months (OR = 5.250, 95% CI = 2.306–11.953) increased the odds of developing ADHD by 1.657 and 5.250, respectively, when compared to children with seizure control (Table 2).
The use of ASM is listed in Table 3. No statistically significant difference (P = 0.660) in the prevalence of ADHD was observed between the children who were treated with ASM and those who were either undergoing withdrawal or never used ASM. However, a significantly higher (P < 0.001) prevalence of comorbid ADHD was observed in children taking polytherapy ASMs (n = 104, 61.1%) compared with those taking monotherapy ASMs (n = 74, 37.0%). Further logistic analysis showed that children taking polytherapy ASMs (OR = 2.683, 95% CI = 1.760–4.089) increased the odds of developing ADHD compared with children taking monotherapy ASMs.
Discussion
Epilepsy is the most common neurological disorder in children. As the most common comorbidity of epilepsy, ADHD may have further negative impacts on children with epilepsy, such as academic and vocational underachievement, depression, and anxiety [12, 13]. To reduce the impact of ADHD on children with epilepsy, an effective and timely diagnosis and treatment of ADHD are needed. Experts recommend that ADHD screening should be performed in patients with epilepsy starting at the age of 6 years or at the time of diagnosis if older than 6 years, with annual reevaluation. Screening for ADHD should also be reassessed after changes in ASM [18]. However, ADHD in children with epilepsy is often underdiagnosed, as clinicians may misinterpret the symptoms of ADHD as epilepsy itself, or may prioritize concerns about the medications for ADHD lowering the seizure threshold [18].
The prevalence of ADHD in children with epilepsy is reported to be between 30% and 40%. In children with refractory epilepsy, the prevalence of ADHD can be as high as 70%, significantly higher than the reported rates of 12.5% to 15% in healthy children without seizures [16, 19,20,21]. In our study, the prevalence of ADHD was found to be 47.8%, slightly higher than that reported in previous studies. This might be because of the inclusion of both non-refractory and refractory cases in our study, with the prevalence rate representing the overall cohort. Furthermore, the hospitals involved in our study were mainly tertiary hospitals in large cities. In China, patients with unsatisfactory epilepsy treatment are more inclined to choose tertiary hospitals for treatment, resulting in a higher proportion of refractory epilepsy cases being managed in these hospitals; this could also be one of the reasons for the slightly higher prevalence rate seen in our study. However, the exact pathogenesis of comorbid ADHD in children with epilepsy was unclear.
According to published literature, male children typically account for the majority of ADHD cases [22]. In our study, however, male children exhibited an equal rate of ADHD (48.4%) compared to female children (47%). No statistically significant difference (P = 0.764) in gender composition was observed between the two groups of children, one with and one without ADHD. This suggests that gender is not associated with the prevalence of ADHD in children with epilepsy. Similarly, most studies revealed no difference between the number of male children with epilepsy and female children with epilepsy [20, 23, 24]. Therefore, it is crucial that children with epilepsy, regardless of gender, receive adequate attention for the diagnosis of ADHD. Screening patients for ADHD should not be overlooked based on the female gender.
The relationship between the prevalence of ADHD and the age of epilepsy onset has presented conflicting views in previous literature [18]. Alfstad et al. showed that early onset of epilepsy increased the risk of psychiatric disorder [25]; however, the risk of ADHD was not specifically mentioned. Kwong et al. also supported this finding and demonstrated that seizure onset at an early age in adolescents with epilepsy was associated with higher rates of ADHD [26]. In contrast, studies by Hermann et al. and Kral et al. observed no significant correlation between the early onset of epilepsy and a higher rate of ADHD [23, 27]. In our study, we grouped the patients according to the age of epilepsy onset and observed that the prevalence of ADHD was statistically significant between different groups using Pearson’s Chi-square test. Furthermore, using logistic regression analysis, we found that those aged ≥ 12 years had a lower prevalence of ADHD than those with an epilepsy onset age < 3 years. The other groups did not show a higher prevalence than the group aged < 3 years. Overall, our study suggested that the onset of epilepsy in adolescence might be associated with a lower prevalence of ADHD. This might be because the neuropsychological development of young children is still maturing, hence seizures are more likely to cause neuropsychological diseases. Therefore, it is important to prioritize the screening of ADHD in young children with epilepsy.
According to the previous studies, there was a negative relationship between the age and the prevalence of ADHD [28]. In our study, we observed a lower prevalence of ADHD in the group of children aged 12 years compared with those aged 6 to 9 years. In addition, the prevalence was comparable between the groups of children aged 6 to 9 years and those aged 9–12 years. This suggests that the prevalence of ADHD decreases during adolescence.
There were few conclusions regarding the association between the duration of epilepsy and the prevalence of ADHD. While we observed that a longer duration of epilepsy was associated with a higher likelihood of comorbid ADHD, the prevalence of ADHD did not increase across the groups with the duration of epilepsy. Many previous studies did not find a correlation between specific epilepsy types and a greater risk of ADHD [20, 23, 24, 27]. Other researchers, however, provided evidence that some epilepsy syndromes or specific types of epilepsy might be associated with increased rates of ADHD or poorer performance on attentional control tests [29, 30]. In the present study, logistic regression analysis suggested that combined generalized and focal epilepsy may have a higher prevalence of ADHD than other types of epilepsy or epilepsy syndrome. While some earlier studies found no significant correlation between the seizure frequency at initial diagnosis in children with newly diagnosed epilepsy [24], the majority of the studies supported an association between higher seizure frequency and a greater risk of ADHD [31, 32]. Our study also supported the association between poor seizure control and a higher prevalence of ADHD. Patients who had seizure attacks more than once per 3 months had a significantly higher risk for ADHD than those with seizure control (OR = 5.250).
Until now, several studies have been conducted to investigate the correlation between epileptiform interictal EEG abnormalities and the risk of ADHD [33,34,35]. However, there is still a lack of convincing evidence for any relationship between interictal EEG abnormalities and ADHD. Our study revealed a higher prevalence of ADHD among individuals with epileptiform interictal EEG compared to those with a normal EEG. This suggests that there may be an association between interictal EEG changes and ADHD in children with epilepsy. This may be because epileptiform interictal EEG abnormalities lead to impaired attention and cognition, thereby increasing the likelihood of comorbidities of ADHD.
To date, only a few studies have focused on the effect of ASMs on the development of ADHD [18]. It had already been reported that benzodiazepines and phenobarbital might lead to attentional deficit [36, 37]. Compared with monotherapy, polytherapy is more likely to be associated with behavioral problems [18]. In our study, none of the patients had ever taken benzodiazepines or phenobarbital as a treatment for epilepsy. No statistically significant difference in the prevalence of ADHD was reported between the treated and untreated groups, whereas the prevalence of ADHD was significantly higher (P < 0.001) in the polytherapy group than in the monotherapy group. More studies are needed to confirm whether polytherapy itself or the underlying refractory epilepsy resulting in polytherapy prescription is associated with ADHD. Previous research claimed that the inattentive subtype was the predominant ADHD type in children with epilepsy [13, 14, 21]. Our findings were consistent with these studies, but there was no significant correlation between the subtype of ADHD and the demographic and clinical characteristics.
Limited data are available on the treatment of ADHD in children with epilepsy, especially the class I study on efficacy and tolerability [18, 38, 39]. The current treatment of ADHD with epilepsy is based on the conventional treatment of ADHD in children, and no specific treatment is recommended [38]. Methylphenidate, a commonly used medication for ADHD, has not been widely used in children with epilepsy and ADHD, due to concerns among clinicians that it may increase seizure frequency, especially in patients who demonstrate epileptiform abnormalities on EEG [18, 38]. Nevertheless, several studies have confirmed the efficacy and tolerability of methylphenidate in children diagnosed with both ADHD and epilepsy. These findings reinforce the hypothesis that ADHD medications do not increase the risk of seizures, even in patients with epilepsy [18, 38]. In China, with the increasing awareness of parents and teachers towards ADHD, the consultation rate of ADHD has gradually increased in recent years. Despite this, the consultation rate for ADHD remains relatively low in China compared to its prevalence. Many parents still assume that ADHD is the sole reason for poor learning and behavioral performance, adopting management methods such as criticism and restraint without recognizing ADHD as a medical condition that requires standardized diagnosis and treatment. Compared with the general population, children with epilepsy have lower consultation and treatment rates for ADHD. Apart from parental factors, clinicians’ insufficient understanding, diagnosis, and treatment of epilepsy with ADHD, along with concerns that the drugs for ADHD may aggravate seizures, are the main reasons for this situation. The results of our study are consistent with the current diagnosis and treatment situation of ADHD in children with epilepsy in China. Only a few patients received attention from clinicians for their ADHD symptoms during routine diagnosis and treatment, and even the children diagnosed with both ADHD and epilepsy were often not recommended for drug treatment or behavioral therapy. There are many factors contributing to the current situation in China. Clinicians tend to focus more on the treatment of epilepsy, often lacking sufficient experience with therapeutic drugs for ADHD in children with epilepsy and harboring concerns that these drugs may lower the seizure threshold. In addition, parents also had limited awareness of ADHD symptoms and did not provide a complete medical history to clinicians thus delaying the diagnosis of ADHD. Furthermore, drugs for ADHD are managed as special drugs, and many hospitals do not stock them, leading to insufficient ADHD treatment rates. Another important reason is that China has a large population and most cases are concentrated in tertiary hospitals. The excessive number of patients results in limited consultation time per capita, making it challenging for clinicians to thoroughly diagnose and treat ADHD. In order to increase clinicians’ awareness of ADHD in children with epilepsy, the “Chinese expert consensus on the diagnosis and treatment of ADHD in children with epilepsy” was revised and published by the CC-CAAE to improve diagnosis and treatment rates of ADHD in children with epilepsy and ultimately improve prognosis.
In conclusion, our study reflects the current situation of ADHD in children with epilepsy across China. We found that children with epilepsy had a higher prevalence of ADHD than healthy children without seizures, with poor seizure control and epileptiform interictal EEG identified as potential risk factors for ADHD in such children. Although ADHD is a common comorbidity in children with epilepsy, the diagnosis and treatment of ADHD are often overlooked by clinicians. The findings from our study have the potential to improve the knowledge of ADHD in children with epilepsy in China and improve patient prognosis by assisting in making more informed diagnostic and treatment decisions. Nonetheless, more studies are needed to confirm the efficacy, tolerability, and safety of ADHD drugs in children with epilepsy.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to potential data breaches that could compromise the privacy of enrolled patients, but are available from the corresponding author on reasonable request.
References
Guidelines for epidemiologic studies on epilepsy. Commission on epidemiology and prognosis, international league against epilepsy. Epilepsia. 1993;34:592–6.
Mac TL, Tran DS, Quet F, Odermatt P, Preux PM, Tan CT. Epidemiology, aetiology, and clinical management of epilepsy in Asia: a systematic review. Lancet Neurol. 2007;6:533–43.
Ba-Diop A, Marin B, Druet-Cabanac M, Ngoungou EB, Newton CR, Preux PM. Epidemiology, causes, and treatment of epilepsy in sub-Saharan Africa. Lancet Neurol. 2014;13:1029–44.
Banerjee PN, Filippi D, Allen HW. The descriptive epidemiology of epilepsy—a review. Epilepsy Res. 2009;85:31–45.
Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia. 2010;51:883–90.
Keezer MR, Sisodiya SM, Sander JW. Comorbidities of epilepsy: current concepts and future perspectives. Lancet Neurol. 2016;15:106–15.
Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7:357–63.
Wei SH, Lee WT. Comorbidity of childhood epilepsy. J Formos Med Assoc. 2015;114:1031–8.
Gaitatzis A, Carroll K, Majeed A, Sander JW. The epidemiology of the comorbidity of epilepsy in the general population. Epilepsia. 2004;45:1613–22.
Pastor PN, Reuben CA, Kobau R, Helmers SL, Lukacs S. Functional difficulties and school limitations of children with epilepsy: findings from the 2009–2010 national survey of children with special health care needs. Disabil Health J. 2015;8:231–9.
Sillanpää M, Helen CJ. The psychosocial impact of epilepsy in childhood. Epilepsy Behav. 2009;15(Suppl 1):S5–10.
Schatz DB, Rostain AL. ADHD with comorbid anxiety: a review of the current literature. J Atten Disord. 2006;10:141–9.
Kwong KL, Lam D, Tsui S, Ngan M, Tsang B, Lai TS, et al. Self-esteem in adolescents with epilepsy: psychosocial and seizure-related correlates. Epilepsy Behav. 2016;63:118–22.
Davis SM, Katusic SK, Barbaresi WJ, Killian J, Weaver AL, Ottman R, et al. Epilepsy in children with attention-deficit/hyperactivity disorder. Pediatr Neurol. 2010;42:325–30.
Muhigwa A, Preux PM, Gérard D, Marin B, Boumediène F, Ntamwira C, et al. Comorbidities of epilepsy in low and middle-income countries: systematic review and meta-analysis. Sci Rep. 2020;110:9015.
Drechsler R, Brem S, Brandeis D, Grünblatt E, Berger G, Walitza S. ADHD: current concepts and treatments in children and adolescents. Neuropediatrics. 2020;51:315–35.
Aaberg KM, Bakken IJ, Lossius MI, Lund Søraas C, Håberg SE, Stoltenberg C, et al. Comorbidity and childhood epilepsy: a nationwide registry study. Pediatrics. 2016;138:e20160921.
Auvin S, Wirrell E, Donald KA, Berl M, Hartmann H, Valente KD, et al. Systematic review of the screening, diagnosis, and management of ADHD in children with epilepsy. Consensus paper of the task force on comorbidities of the ILAE pediatric commission. Epilepsia. 2018;59:1867–80.
Cohen R, Senecky Y, Shuper A, Inbar D, Chodick G, Shalev V, et al. Prevalence of epilepsy and attention-deficit hyperactivity (ADHD) disorder: a population-based study. J Child Neurol. 2013;28:120–3.
Dunn DW, Austin JK, Harezlak J, Ambrosius WT. ADHD and epilepsy in childhood. Dev Med Child Neurol. 2003;45:50–4.
Chou IC, Chang YT, Chin ZN, Muo CH, Sung FC, Kuo HT, et al. Correlation between epilepsy and attention deficit hyperactivity disorder: a population-based cohort study. PLoS One. 2013;8:e57926.
Barkley RA, Murphy KR. Attention-deficit hyperactivity disorder: a clinical workbook. 3rd ed. New York: Guilford Press; 2006.
Hermann B, Jones J, Dabbs K, Allen CA, Sheth R, Fine J, et al. The frequency, complications and aetiology of ADHD in new onset paediatric epilepsy. Brain. 2007;130:3135–48.
Hesdorffer DC, Ludvigsson P, Olafsson E, Gudmundsson G, Kjartansson O, Hauser WA. ADHD as a risk factor for incident unprovoked seizures and epilepsy in children. Arch Gen Psychiatry. 2004;61:731–6.
Alfstad KÅ, Torgersen H, Van Roy B, Hessen E, Hansen BH, Henning O, et al. Psychiatric comorbidity in children and youth with epilepsy: an association with executive dysfunction? Epilepsy Behav. 2016;56:88–94.
Kwong KL, Lam D, Tsui S, Ngan M, Tsang B, Lam SM. Attention deficit hyperactivity disorder in adolescents with epilepsy. Pediatr Neurol. 2016;57:56–63.
Kral MC, Lally MD, Boan AD. Identification of ADHD in youth with epilepsy. J Pediatr Rehabil Med. 2016;9:223–9.
Sherman EMS, Brooks BL, Akdag S, Connolly MB, Wiebe S. Parents report more ADHD symptoms than do teachers in children with epilepsy. Epilepsy Behav. 2010;19:428–35.
Gascoigne MB, Smith ML, Barton B, Webster R, Gill D, Lah S. Attention deficits in children with epilepsy: preliminary findings. Epilepsy Behav. 2017;67:7–12.
Kernan CL, Asarnow R, Siddarth P, Gurbani S, Lanphier EK, Sankar R, et al. Neurocognitive profiles in children with epilepsy. Epilepsia. 2012;53:2156–63.
Bennett-Back O, Keren A, Zelnik N. Attention-deficit hyperactivity disorder in children with benign epilepsy and their siblings. Pediatr Neurol. 2011;44:187–92.
McCusker CG, Kennedy PJ, Anderson J, Hicks EM, Hanrahan D. Adjustment in children with intractable epilepsy: importance of seizure duration and family factors. Dev Med Child Neurol. 2002;44:681–7.
Danhofer P, Pejčochová J, Dušek L, Rektor I, Ošlejšková H. The influence of EEG-detected nocturnal centrotemporal discharges on the expression of core symptoms of ADHD in children with benign childhood epilepsy with centrotemporal spikes (BCECTS): a prospective study in a tertiary referral center. Epilepsy Behav. 2018;79:75–81.
Metz-Lutz MN, Kleitz C, de Saint MA, Massa R, Hirsch E, Marescaux C. Cognitive development in benign focal epilepsies of childhood. Dev Neurosci. 1999;21:182–90.
Wannag E, Eriksson AS, Larsson PG. Attention-deficit hyperactivity disorder and nocturnal epileptiform activity in children with epilepsy admitted to a national epilepsy center. Epilepsy Behav. 2010;18:445–9.
Dunn DW, Kronenberger WG. Childhood epilepsy, attention problems, and ADHD: review and practical considerations. Semin Pediatr Neurol. 2005;12:222–8.
Gallassi R, Morreale A, Di Sarro R, Marra M, Lugaresi E, Baruzzi A. Cognitive effects of antiepileptic drug discontinuation. Epilepsia. 1992;33(Suppl 6):S41–4.
Rheims S, Auvin S. Attention deficit/hyperactivity disorder and epilepsy. Curr Opin Neurol. 2021;34:219–25.
Chatterjee M, Saha S, Sinha S, Mukhopadhyay K. A three-pronged analysis confirms the association of the serotoninergic system with attention deficit hyperactivity disorder. World J Pediatr. 2022;18:825–34.
Acknowledgements
The authors would like to thank the participants and their guardians, the collaborating clinicians, and other clinical staff. We would also like to acknowledge Dr. Ramandeep Singh of Indegene Pvt Ltd. for editorial support.
Funding
None.
Author information
Authors and Affiliations
Contributions
The Comorbidity Committee of China Association Against Epilepsy conceived, designed and supervised the study. PG contributed to investigation and data collection, writing of the original draft, and reviewing and editing. ZSZ contributed to investigation and data collection, and reviewing and editing. HY, WTC, CZY, WXQ, SHB, LYH, WQ, LWH, LJM, and ZYH contributed to investigation and data collection. All authors have read and agreed the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
The study was approved by the Ethics Committee of West China Hospital, Sichuan University (the leader unit) under protocol number 2021(327), and collaborating research institutes, and performed in accordance with the Declaration of Helsinki.
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. And there are no relationships with any manufacturer of antiseizure medication or ADHD drugs. The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pan, G., Han, Y., Wang, TC. et al. Attention deficit hyperactivity disorder in children with epilepsy: a multicenter cross-sectional analysis in China. World J Pediatr (2024). https://doi.org/10.1007/s12519-024-00813-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12519-024-00813-2